Abstract
Purpose
To compare central corneal thickness measurements obtained by Orbscan II, contact ultrasound pachymetry and the non-contact Artemis-2 scanning ultrasound system.
Methods
The central corneal thickness of 40 eyes (20 normal subjects) was measured using first the Orbscan II, followed by contact ultrasound pachymetry, and finally by the Artemis-2. Results were compared statistically using ANOVA, paired T-tests, and Bland-Altman plots.
Results
One-way ANOVA showed a significant difference between the three different modes of measuring central corneal thickness (F=32.84, p=0.0001). Artemis-2 and the ultrasound pachymeter measurements were highly correlated (R2=0.963, p<0.0001), but with Artemis, on average, measuring central corneal thickness by 11.2±6.6 microns less than the pachymeter. The Artemis-2 and Orbscan II measurements were less well correlated (R2=0.851, p<0.001), with Orbscan measurements on average 7.5±15.7 microns thinner than those obtained with the Artemis-2. In addition, the Orbscan showed a trend towards increasing underestimation of corneal thickness for thinner corneas.
Conclusions
Ultrasound pachymetry and Artemis-2 measurements of central corneal thickness were highly correlated. The 11-micron mean difference between the pachymeter and Artemis measurements may be attributed to decentration, oblique incidence of the probe to the cornea or possibly the effect of topical anesthetic when using contact pachymetry. While Orbscan values only had an average difference of 7.5 microns from Artemis, they were less correlated than contact ultrasound pachymetry with Artemis values and increasing prone to underestimation of corneal thickness for thinner corneas.
BACKGROUND
Accurate measurement of corneal thickness has become increasingly important in management of glaucoma, where corneal thickness must be factored into measurement of intraocular pressure by applanation tonometry, and in refractive surgery, where it is a major factor in pre-and post-operative assessment of the cornea.
The current gold standard for corneal thickness determination is the hand-held ultrasound pachymeter. Ultrasound pachymeters, operating at frequencies of 20 to 50 MHz, emit short acoustic pulses and detect reflections from the anterior and posterior surfaces of the cornea. Corneal thickness is then calculated from the measured time-of-flight between these reflections and the accepted speed of sound in the cornea of 1636–1640 m/s.1
There are a number of potential sources of error in hand-held pachymetry. Accurate measurement of central corneal thickness (CCT) relies on placement of the probe as close as possible to the central cornea. If the probe is placed at a point that is slightly off center, the measurement will be larger than expected. Thicker values will also be obtained if the probe is not placed at 90 degrees to the corneal surface. It is also possible that the thinnest part of the cornea may itself be non-central.
Other devices have been developed to measure corneal thickness including optical coherence tomography2, specular microscopy,3 dual-beam partial coherence interferometry4, confocal microscopy5, scanning slit lamp corneal topography6, ultrasound biomicroscopy7 and ultra-high frequency ultrasound8.
The Orbscan II (Bausch & Lomb, Rochester, NY), a widely-used combined Placido-scanning slit-lamp system, provides topography of both anterior and posterior corneal surfaces and corneal thickness maps. Several studies have been made comparing Orbscan with ultrasound pachymetry for measurement of corneal thickness, some of which are summarized in Table 1.4, ,9,10,11,12,13,14,15,16,17,18,19 From the Table, considerable variability is seen in comparison of mean CCT for groups of normal eyes when comparing ultrasound pachymetry with Orbscan measurements (using the manufacturer’s recommended acoustic correction factor of 0.92), with differences ranging from −21 to 33 µm. For post-LASIK eyes and in keratoconus, Orbscan values for CCT were consistently thicker (30–50 µm) than those obtained by ultrasound pachymetry11,13,14,18,19.
Table 1.
Findings of studies comparing ultrasound pachymetry with Orbscan II in determinations of central corneal thickness.
| Investigator | Study Population | N Eyes | US±SD µm | Orbscan±SD µm | US-Orbscan µm |
|---|---|---|---|---|---|
| Doughty9 | Normals | 50 | 523±37 | 544±40 | −21 |
| Fernandez10 | Normals | 92 | 551.2±43.8 | 559.9±35.8 | −9 |
| Gherghel11 | Normals | 137 | 550.5±37.2 | 546.4±48.1 | 4 |
| Gonzalez-Meijome12 | Normals | 24 | 545±40 | 515±45 | 30 |
| Iskander13 | Normals* | 906 | 532.6±30.0 | 514.2±33.0 | 18 |
| Kawana14 | Normals | 203 | 478.8±41.9 | 445.6±60.0 | 33 |
| Lackner15 | Normals | 30 | 552.0±31.7 | 530.0±33.9 | 22 |
| McLaren16 | Normal | 24 | 554±28 | 540±35 | 14 |
| Rainer4 | Normal | 40 | 543.4±34.8 | 523.6±36.2 | 20 |
| Suzuki30 | Normal | 216 | 548.1±33.0 | 546.9±35.4 | 1 |
| Radford17 | Glaucoma | 66 | 558.4±34.6 | 564.9±36.5 | 7 |
| Iskander13 | Post-LASIK | 183 | 482.8±40.0 | 432.7±44.0 | 50 |
| Kawana14 | Post-LASIK | 203 | 478.8±41.9 | 445.6±60.0 | 33 |
| Ho18 | Post-LASIK | 103 | 438.2±41.2 | 435.2±49.6** | 3** |
| Gherghel11 | Keratoconus | 64 | 502.8±52.5 | 458.8±62.5 | 44 |
| Kawana19 | Keratoconus | 22 | 485.0±29.3 | 449.5±43.2 | 35 |
Pre-LASIK
Acoustic correction factor = 0.89
The variability of ultrasound pachymetry is largely related to decentration, oblique incidence and possibly corneal compression by the probe. The Artemis-2 system20 (ArcScan, Inc., Morrison, CO) is a high-frequency (35 MHz) ultrasound system is largely unaffected by these factors. In the Artemis-2, the cornea is offset from the probe by a normal-saline immersion medium. During scanning, the probe is moved in an arc-shaped trajectory that is matched approximately to the corneal curvature, enabling near-normal incidence at all positions. The device incorporates a fixation light and optical camera for visualization of the eye to assure centration.
The purpose of this study was to determine how well CCT measurements taken with the handheld ultrasound pachymeter, Orbscan II, and the Artemis-2 correlate.
METHODS
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of the Weill Cornell Medical College of (WCMC).
Central corneal thickness was determined with three different modalities: Orbscan II, ultrasound pachymetry (SP-2000; Tomey, Erlangen, Germany); and the Artemis-2 ultrasound system. The same investigator performed all measurements on subjects using each modality. Twenty healthy subjects were recruited (40 eyes). All subjects had healthy eyes and no corneal pathology.
Informed consent was obtained from each volunteer. Subjects’ ages ranged from 25–60 (average 31.5 years). Fourteen volunteers were female, while six were male. None of the subjects had prior corneal surgery or pathology. Contact lens wearers were included in this study, but were required to have not worn their contact lenses for 24 hours before measurements were taken. Two subjects (4 eyes) were soft contact lens wearers. Each subject's cornea was measured at the same time of day.
For Orbscan measurements, the subject’s chin was placed on the chin rest and the forehead was pressed against the forehead strap. The subject was asked to look at the blinking fixation target, and the images were captured. The system software automatically detects the anterior and posterior corneal surfaces on the acquired images and calculates the corneal diameter over the whole surface. An acoustic equivalent correction factor of 0.92 was used for consistency with the ultrasonic evaluation, as recommended by the manufacturer. From these measurements, the thinnest value is automatically selected as CCT.
CCT was then measured using a handheld ultrasound pachymeter (SP-2000; Tomey, Erlangen, Germany) calibrated by the manufacturer. The subject’s eye was anesthetized with topical 1% proparacaine, and the pachymeter probe was brought in light contact with the cornea centrally and perpendicularly. CCT was recorded as the minimum of three individual acquisitions. The measurements were made with the ultrasound velocity (acoustic index) set to 1640 m/s.
CCT was then measured using the Artemis-2. The subject was placed in a seated position before the instrument, leaned forward and looked with one eye through an aperture surrounded by a disposable eyepiece consisting of a 1-cm thick viscoelastic ring with a central optically and acoustically transparent membrane. No anesthetic eyedrops were used. Sterile normal saline solution was then introduced into the eyepiece to form an acoustic coupling medium between the eye and the transparent membrane. The ultrasound transducer and scan mechanism are submerged in degassed water within the body of the scanner and separated from the eye by the transparent membrane. Behind the transducer is an optical system including a beam-splitter, a blinking fixation light and a digital infrared camera. With the subject directing gaze at the fixation light, the scan axis was centrated by moving the scan mechanism with a joystick until a crosshair representing the ultrasound axis was centered within the pupil. When proper alignment was achieved, the range of the transducer to the cornea was adjusted to place the cornea in the acoustic focal plane. When alignment and range adjustments were complete, we acquired three vertical and three horizontal scans.
Artemis scans were then analyzed with software (ArtPro) developed in our laboratory. Digital signal processing (deconvolution and determination of the signal envelope by analytic signal magnitude detection) was used to detect corneal tissue interfaces.8 The corneal sound velocity setting used for analysis of Artemis-2 data was 1636 M/sec. The minimum measurement of the CCT was recorded for comparison with Orbscan and ultrasound pachymeter measurements.
ANOVA , paired T-test (2-tailed), and Bland-Altman analyses were used to examine differences in CCT determinations between the three measurement techniques.
RESULTS
One-way ANOVA (correlated samples) showed a significant difference between the three different modes of measuring CCT (F=32.84, p=0.0001).
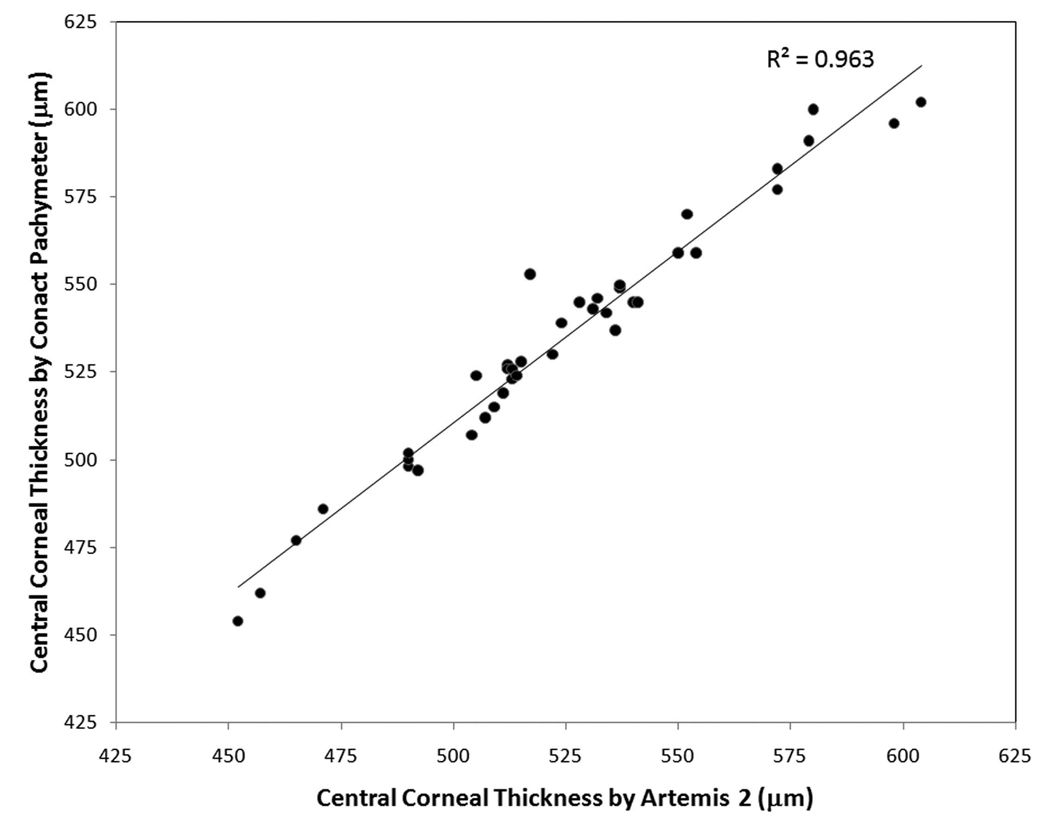
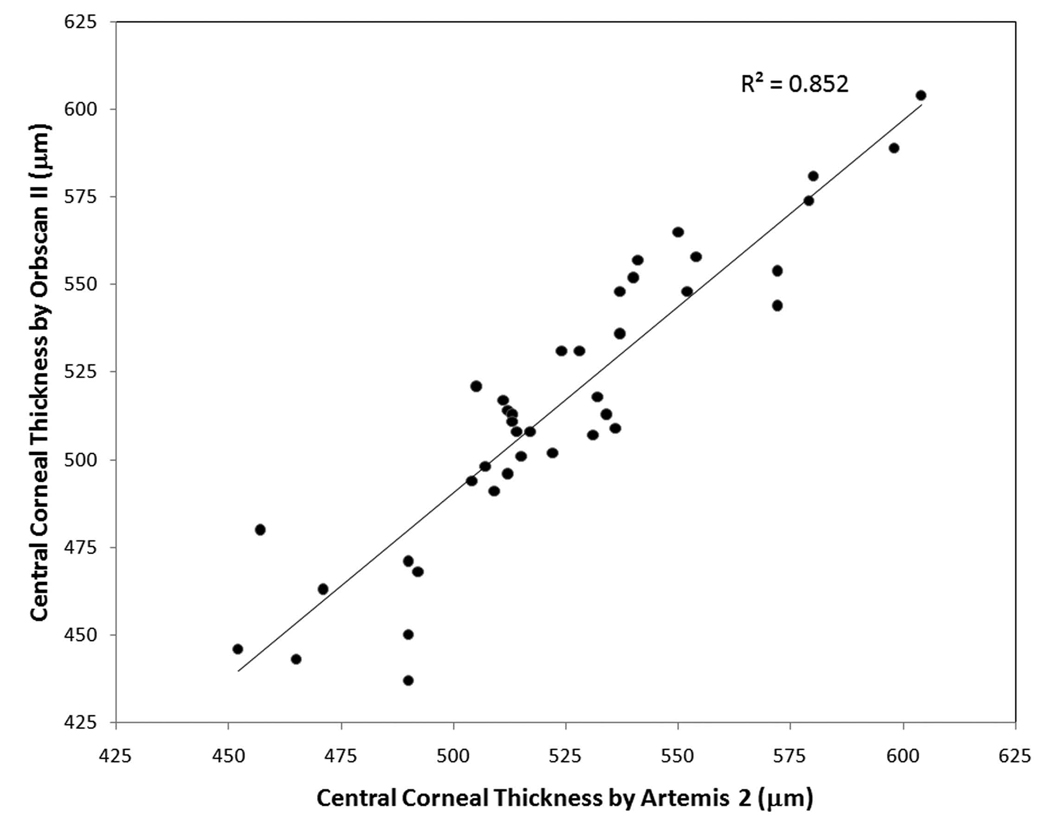
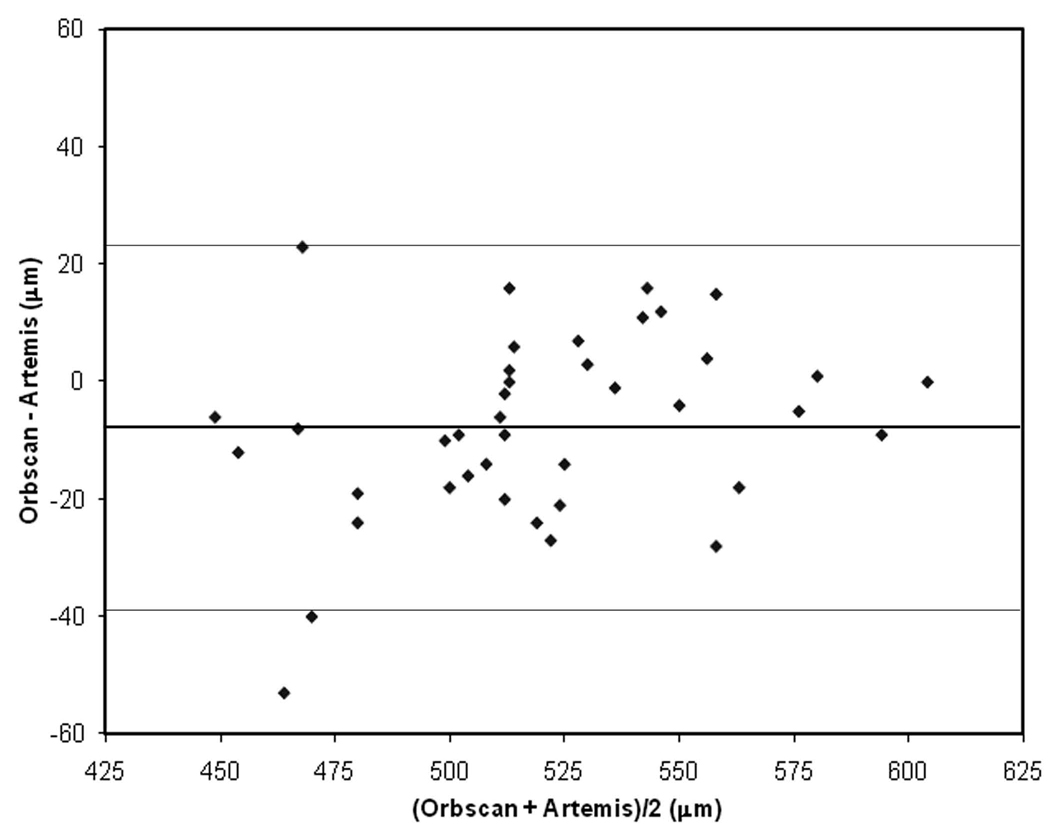
Measurements taken with the Artemis-2 and the ultrasound pachymeter were highly correlated (R2=0.963, p<0.0001, see Figure 1a). However, as seen in the Bland-Altman plot (Figure 1b), the Artemis-2 values for CCT were thinner than those provided by the US pachymeter by an average of 11.2-µm, a statistically significant difference (T=−9.38, p<.0001). Artemis-2 and Orbscan measurements were less highly correlated (R2=0.851, p<0.001, see Figure 2a) and Orbscan values averaged of 7.5-µm less than Artemis values (T=3.04, p=.0036). While this difference is less than that between handheld pachymetry and Artemis, the variability of Orbscan relative to Artemis was much greater (SD=15.7) than that between the ultrasound pachymeter and Artemis (SD=6.6). Furthermore, the Bland-Altman plot (Figure 2b) shows a trend towards underestimation of CCT compared to Artemis for thinner corneas.
Figure 1.
Figure 1a. Contact ultrasound pachymeter versus Artemis-2 measurements of central corneal thickness.
Figure 1b. Bland-Altman plot of the handheld US pachymeter compared with the Artemis-2. The horizontal lines represent mean difference with 95% confidence bounds.
Figure 2.
Figure 2a. Orbscan II versus Artemis-2 measurements of central corneal thickness.
Figure 2b. Bland-Altman plot of the Orbscan II compared with the Artemis-2. The horizontal lines represent mean difference with 95% confidence bounds.
DISCUSSION
Central corneal thickness is one of the most important factors for patient selection in kerato-refractive surgery. The most frequently utilized method for CCT determination remains handheld ultrasound pachymetry. Miglior et al. reported an average interobserver standard deviation of 12 microns and variability of less than 2% for this technique.1 There are several potential sources of variation in handheld pachymetry. A study by Asensio et al found a variation of more than ±10-µm after instillation of topical anaesthetic.21 A similar study conducted with proparacaine found corneal thickness measurements were larger when two drops of proparacaine were instilled into the eye.22 The thicker measurements obtained after the instillation of proparacaine were likely the result of epithelial edema from the topical anaesthetic. Another variable that may lead to inaccuracy is compression of the cornea by the probe23 and displacement of the tear film which leads to thinner measurements. In addition, significant variability in CCT measurements has been observed when more than one person takes the measurements, when the same person takes the CCT measurements and when different handheld pachymeters are used to measure the same patient’s corneal thickness.24,25,26 One final factor that may influence the accuracy of pachymeter readings is the speed of sound in corneal tissue. The pachymeter operates on the assumption that all corneal tissue conducts sound at the same speed, but in reality there are slight variations of the speed of sound in healthy versus diseased tissue which also can add a degree of uncertainty to ultrasound pachymetry.27
CCT determinations by handheld ultrasound pachymetry and uncorrected Orbscan do not agree well, with the Orbscan tending to overestimate CCT.28,29 However, with the acoustic correction factor of 0.92 applied to Orbscan measurements, several studies have shown good agreement between handheld pachymetry measurements and the Orbscan.11,29,30,31 It has been reported that Orbscan underestimates corneal thickness in post-LASIK eyes compared to ultrasound pachymetry6,28,32, although a recent report by Ho et al. found the difference to be negligible.18 The difference between the uncorrected Orbscan and ultrasound pachymeter may be attributed to the problem of correcting for optical refraction by the curved corneal surfaces in scanning slit methods, displacement of the tear film by contract pachymeters, and possibly differences in definition of the posterior surface.29
The Artemis-2 uses high frequency ultrasound, but unlike handhelds, includes an optical subsystem for centration, uses an arc scan geometry to maintain normal incidence, does not compress the cornea, and acquires a series of two-dimensional cross-sections of the cornea. This allows determination of the thickness profile across the full width of the cornea as well as the thickness of internal layers (epithelium, and flap and residual stroma in post-LASIK eyes). The thinnest part of the cornea can be located and measured from a series of scans.
We compared corneal measurements taken with the ultrasound pachymeter, the Orbscan II, and the Artemis-2. Bland-Altman plots showed the handheld ultrasound consistently measured CCT thicker than the Artemis-2 (on average 11.2 micrometers). The Orbscan measurements were less highly correlated with Artemis-2 than those obtained with handheld pachymetry. While the average difference was only 7.5-µm, the variability was higher and a trend towards underestimation of CCT by Orbscan relative to Artemis-2 was seen for thinner corneas. The results of this study follow what has generally been reported in the literature: namely, that Orbscan measurements do not correlate well with the hand-held ultrasound. In contrast, the handheld ultrasound pachymeter and Artemis-2 correlated well, though the pachymeter measured (on average) CCT 11 microns thicker than Artemis-2.
This study demonstrated that while contact ultrasound pachymetry is highly correlated with non-contact, optically aligned Artemis-2 ultrasound measurements of CCT, the handheld pachymeter tended to produce slightly higher measurements of CCT than Artemis. This may be attributed to lack of centration, oblique incidence or even the effect of the topical anesthetic in handheld pachymetry. While the mean CCT of the study population determined by Orbscan was close to that of the Artemis, the variability of Orbscan values relative to the Artemis was much greater.
Acknowledgments
Supported in part by NIH grant EB000238, the Dyson Foundation, New York, NY and Research to Prevent Blindness, New York, NY.
Biography

Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meetings: Preliminary data was presented at ARVO (Advanced Research in Vision and Ophthalmology) April 2007, Fort Lauderdale, Florida, USA
Commercial Interests: Drs. Coleman and Silverman have a commercial interest in ArcScan, Inc.
References
- 1.Miglior S, Albe E, Guareschi M, et al. Intraobserver and interobserver reproducibility of ultrasonic pachymetry measurements of central corneal thickness. Br J Ophthalmol. 2004;88:174–177. doi: 10.1136/bjo.2003.023416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bechman M, Thiel MJ, Neubauer AS, et al. Central corneal thickness measurements with a retinal optical coherence tomography device versus standard ultrasonic pachymetry. Cornea. 2001;20:50–54. doi: 10.1097/00003226-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Bovelle R, Kaufman SC, Thompson HW, et al. Corneal thickness measurements with the Topcon SP-2000p specular microscope and an ultrasound pachymeter. Arch Ophthalmol. 1999;117:868–870. doi: 10.1001/archopht.117.7.868. [DOI] [PubMed] [Google Scholar]
- 4.Rainer G, Findl O, Petternel V, et al. Central corneal thickness measurements with partial coherence interferometry, ultrasound, and the Orbscan System. Ophthalmology. 2004;111:875–879. doi: 10.1016/j.ophtha.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 5.Li HF, Petroll WM, Møller-Pederson T, et al. Epithelial and corneal thickness measurements by in vivo confocal microscopy through focusing (CMTF) Curr Eye Res. 1997;16:214–221. doi: 10.1076/ceyr.16.3.214.15412. [DOI] [PubMed] [Google Scholar]
- 6.Yaylali V, Kaufman SC, Thompson HW. Corneal thickness measurements with the Orbscan topography system and ultrasound pachymetry. J Cataract Refract Surg. 1997;23:1345–1350. doi: 10.1016/s0886-3350(97)80113-7. [DOI] [PubMed] [Google Scholar]
- 7.Tam ES, Rootman DS. Comparison of central corneal thickness measurements by specular microscopy, ultrasound pachymetry, and ultrasound biomicroscopy. J Cataract Refract Surg. 2003;29:1179–1184. doi: 10.1016/s0886-3350(02)01921-1. [DOI] [PubMed] [Google Scholar]
- 8.Reinstein DZ, Silverman RH, Sutton HF, et al. Arc-scanning very high-frequency digital ultrasound for 3D pachymetric mapping of the corneal epithelium and stroma in laser in situ keratomileusis. J Refract Surg. 2000;16:414–430. doi: 10.3928/1081-597X-20000701-04. [DOI] [PubMed] [Google Scholar]
- 9.Doughty MJ, Jonuscheit S. Effect of central corneal thickness on Goldmann applanation tonometry measures – a different result with different pachymeters. Graefe’s Arch Clin Exp Ophthalmol. 2007;245:1603–1610. doi: 10.1007/s00417-007-0601-x. [DOI] [PubMed] [Google Scholar]
- 10.Fernandez MJG, Rey AD, Cervino A, Yebra-Pimental E. A comparison of two achymetric systems: slit-scanning and ultrasonic. CLAO J. 2002;221:223. doi: 10.1097/01.ICL.0000034556.15901.CC. [DOI] [PubMed] [Google Scholar]
- 11.Ghergel D, Hosking SL, Mantry S, et al. Corneal pachymetry in normal and keratoconic eyes: Orbscan II versus ultrasound. J Cat Refract Surg. 2004;30:1272–1277. doi: 10.1016/j.jcrs.2003.11.049. [DOI] [PubMed] [Google Scholar]
- 12.Gonzalez-Meijome JM, Cervino A, Yebra-Pimentel E, Parafita MA. Central and peripheral corneal thickness measurement with Orbscan II and topographical ultrasound pachymetry. J Cat Refr Surg. 2003;29:125–132. doi: 10.1016/s0886-3350(02)01815-1. [DOI] [PubMed] [Google Scholar]
- 13.Iskander NG, Penno EA, Peters NT, Gimbel HV, Ferensowicz M. Accuracy of Orbscan pachymetry measurements and DHG ultrasound pachymetry in primary laser in situ keratomileusis and LASIK enhancement procedures. J Cat Refr Surg. 2001;27:681–685. doi: 10.1016/s0886-3350(01)00820-3. [DOI] [PubMed] [Google Scholar]
- 14.Kawana K, Tokunaga T, Okamoto F, Kiuchi T, Oshika T. Comparison of corneal thickness measurements using Orbscan II, non-contact specular microscopy, and ultrasonic pachymetry in eyes after laser in situ keratomileusis. Br J Ophthalmol. 2004;88:466–468. doi: 10.1136/bjo.2003.030361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lackner B, Schmidinger G, Pieh S, Funovics MA, Skorpik C. Repeatability and reproducibility of central corneal thickness measurement with Pentacam, Orbscan, and ultrasound. Optom Vis Sci. 2005;82:892–899. doi: 10.1097/01.opx.0000180817.46312.0a. [DOI] [PubMed] [Google Scholar]
- 16.McLaren JW, Nau CB, Erie JC, Bourne WM. Corneal thickness measurement by confocal microscopy, ultrasound, and scanning slit methods. Am J Ophthalmol. 2004;137:1011–1020. doi: 10.1016/j.ajo.2004.01.049. [DOI] [PubMed] [Google Scholar]
- 17.Radford SW, Lim R, Salmon JF. Comparison of Orbscan and ultrasound pachymeter in the measurement of central corneal thickness. Eye. 2004;18:434–436. doi: 10.1038/sj.eye.6700669. [DOI] [PubMed] [Google Scholar]
- 18.Ho T, Cheng ACK, Rao SK, et al. Central corneal thickness measurements using Orbscan II, Visante, ultrasound and Pentacam pachymetry after laser in situ keratomileusis for myopia. J Cat. Refr. Surg. 2007;33:1177–1182. doi: 10.1016/j.jcrs.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 19.Kawana K, Miyata K, Tokungawa T, et al. Central corneal thickness measurements using Orbscan II scanning slit topography, noncontact specular microscopy, and ultrasonic pachymetry in eyes with keratoconus. Cornea. 2005;24:967–971. doi: 10.1097/01.ico.0000159733.37554.ba. [DOI] [PubMed] [Google Scholar]
- 20.Reinstein DZ, Archer T, Silverman RH. Very high frequency digital ultrasound: Artemis 2 scanning in corneal refractive surgery. In: Vinciguerra P, editor. Refractive Surface Ablation: PRK, Lasek, Epi-Lasik, Custom, PTK and Retreatment. Thorofare, NJ: Slack, Inc.; 2006. pp. 315–330. [Google Scholar]
- 21.Asensio I, Rahhal SM, Alonso L, et al. Corneal thickness values before and after oxybuprocaine 0.4% eye drops. Cornea. 2003;22:527–532. doi: 10.1097/00003226-200308000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Herse O, Siu A. Short-term effects of proparacaine on human corneal thickness. Acta Ophthalmol. 1992;70:740–744. doi: 10.1111/j.1755-3768.1992.tb04879.x. [DOI] [PubMed] [Google Scholar]
- 23.Solomon OD. Corneal indentation during ultrasonic pachymetry. Cornea. 1999;18:214–215. doi: 10.1097/00003226-199903000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Marsich MW, Bullimore M. The repeatability of corneal thickness measures. Cornea. 2000;19:792–795. doi: 10.1097/00003226-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Giasson C, Forthomme D. Comparison of central corneal thickness measurements between optical and ultrasound pachymeters. Optom Vis Sci. 1992;69:236–241. doi: 10.1097/00006324-199203000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Wheeler NC, Morantes CM, Kristensen RM, et al. Reliability coefficients of three corneal pachymeters. Am J Ophthalmol. 1992;113:645–651. doi: 10.1016/s0002-9394(14)74788-9. [DOI] [PubMed] [Google Scholar]
- 27.Nemeth G, Tsorbatzoglou A, Kertesz K, et al. Comparison of central corneal thickness measurements with a new optical device and a standard ultrasonic pachymeter. J Cataract Refract Surg. 2006;32:460–463. doi: 10.1016/j.jcrs.2005.12.138. [DOI] [PubMed] [Google Scholar]
- 28.Prisant O, Calderon N, Chastang P, et al. Reliability of Pachymetric Measurements using Orbscan after Excimer Refractive Surgery. Ophthalmology. 2003;110:511–515. doi: 10.1016/S0161-6420(02)01298-8. [DOI] [PubMed] [Google Scholar]
- 29.Amano S, Honda N, Amano Y, et al. Comparison of central corneal thickness measurements by rotating scheimpflug camera, ultrasonic pachymetry, and scanning-slit corneal topography. Ophthalmology. 2006;113:937–941. doi: 10.1016/j.ophtha.2006.01.063. [DOI] [PubMed] [Google Scholar]
- 30.Suzuki S, Oshika T, Oki K, et al. Corneal thickness measurements: scanning-slit corneal topography and noncontact specular microscopy versus ultrasonic pachymetry. J Cataract Refract Surg. 2003;29:1313–1318. doi: 10.1016/s0886-3350(03)00123-8. [DOI] [PubMed] [Google Scholar]
- 31.Fakhry MA, Artola A, Belda JI, et al. Comparison of corneal pachymetry using ultrasound and Orbscan II. J Cataract Refract Surg. 2002;28:248–252. doi: 10.1016/s0886-3350(01)01277-9. [DOI] [PubMed] [Google Scholar]
- 32.Cheng ACK, Rao SK, Tang E, Lam DSC. Pachymetry assessment with Orbscan II in postoperative patients with myopic LASIK. J Refract Surg. 2006;22:363–366. doi: 10.3928/1081-597X-20060401-12. [DOI] [PubMed] [Google Scholar]