ABSTRACT
OBJECTIVE
To determine whether lifestyle counseling interventions delivered in primary care settings by primary care providers to their low-risk adult patients are effective in changing factors related to cardiovascular risk.
DATA SOURCES
MEDLINE (PubMed), EMBASE, and CINAHL were searched from January 1985 to December 2007. The reference lists of all articles collected were checked to ensure that all suitable randomized controlled trials (RCTs) had been included.
STUDY SELECTION
We chose RCTs on lifestyle counseling in primary care for primary prevention of cardiovascular disease. The search was limited to English-language articles involving human subjects. Studies had to have been conducted within the context of primary care, and interventions had to have been carried out by primary care providers, such as family physicians or practice nurses. Studies had to have had a control group who were managed with usual care. Outcomes of interest were cardiovascular risk scores, blood pressure, lipid levels, weight or body mass index, and morbidity and mortality.
SYNTHESIS
Seven RCTs were included in the review. Only 4 studies showed any significant positive effect on the outcomes of interest, and only 2 of these showed consistent effects across several outcomes. The main effects were on blood pressure and lipid levels, but the size of these effects, while statistically significant, was small. There was no obvious benefit to one provider doing the intervention over another (eg, physician vs nurse), nor of the focus of the intervention (eg, on diet vs on exercise).
CONCLUSION
Lifestyle counseling interventions delivered by primary care providers in primary care settings to patients at low risk (primary prevention) appeared to be of marginal benefit. Resources and time in primary care might be better spent on patients at higher risk of cardiovascular disease, such as those with existing heart disease or diabetes.
RÉSUMÉ
OBJECTIF
Déterminer si les conseils sur le at de vie donnés par les soignants de première ligne à leurs patients adultes à faible risque sont efficaces pour modifier les facteurs de risque cardiovasculaires.
SOURCES DES DONNÉES
On a consulté MEDLINE (PubMed), EMBASE et CINAHL entre janvier 1985 et décembre 2007. On a vérifié la bibliographie de chaque article pour s’assurer d’inclure tous les essais cliniques randomisés (ECR) pertinents.
CHOIX DES ÉTUDES
Nous avons retenu les ECR portant sur les conseils donnés en première ligne pour la prévention primaire des maladies cardiovasculaires. La recherche était limitée aux articles de langue anglaise comportant des sujets humains. Les études devaient être menées dans un contexte de soins primaires, et les interventions effectuées par des soignants de première ligne, tels que des médecins de famille ou des infirmières praticiennes. Les études devaient inclure un groupe témoin recevant les soins usuels. Les issues principales étaient l’indice de risque cardiovasculaire, la tension artérielle, le niveau des lipides, le poids et l’indice de masse corporelle ainsi que la morbidité et la mortalité.
SYNTHÈSE
La revue a finalement porté sur 7 ECR. Seulement 4 revues ont montré un effet positif significatif sur les issues principales et seulement 2 d’entreelles montraient des effets positifs réguliers sur plus d’une issue. Les principaux effets concernaient la tension artérielle et le taux des lipides, mais l’amplitude de ces effets, quoique statistiquement significative, était faible. Il n’y avait pas d’avantage évident associé à un type d’intervenant (p. ex. médecin vs infirmière) ou à un type d’intervention (p. ex. régime ou exercice).
CONCLUSION
Les conseils sur le mode de vie donnés aux patients à faible risque par les intervenants de première ligne (prévention primaire) semblaient avoir peu d’effets bénéfiques. Dans un contexte de soins primaires, les ressources et le temps pourraient être mieux utilisés en ciblant les patients à risque plus élevé de maladie cardiovasculaire, comme ceux souffrant déjà d’une maladie cardiaque ou de diabète.
Elements of lifestyle, such as exercise, diet, smoking, and stress, are known to affect health and risk of cardiovascular disease. Various studies have identified relationships between lifestyle and health status, health care use, and costs to the health care system.1–4 Interventions aimed at improving patients’ lifestyles have resulted in improvements in health outcomes.5–7 The best known study of these interventions was conducted by the Diabetes Prevention Program research group.6 They found that lifestyle interventions prevented progression to diabetes in patients with pre-diabetes. Most of these interventions, however, involved intense exercise and diet programs delivered by exercise physiologists and dietitians.
The objective of this study was to determine whether lifestyle interventions delivered in primary care settings by primary care providers to their adult patients were effective in changing factors related to cardiovascular risk. Only patients without known cardiovascular disease or diabetes were included in the study (primary prevention situations only). Lifestyle interventions were limited to those related to exercise and diet. Outcomes of interest were cardiovascular risk scores, blood pressure, lipid levels, weight or body mass index, and morbidity and mortality.
DATA SOURCES
Literature search
We searched MEDLINE (PubMed), EMBASE, and CINAHL from January 1985 to December 2007 for all randomized controlled trials (RCTs) and systematic reviews of lifestyle counseling in primary care for primary prevention of cardiovascular disease. Search terms used included lifestyle counseling, dietary advice, exercise, physical activity, lifestyle intervention, behaviour modification, primary care, general or family practice, and primary prevention. The reference lists of all articles retrieved were checked to ensure that all suitable RCTs had been included. The search was limited to English-language articles involving human subjects.
Study selection
We considered only RCTs that reported on outcomes at 12 months or longer of patients who did not have pre-existing cardiovascular disease or diabetes. Study participants had to be 18 years or older and could be of either sex. Trials involving drug treatment in combination with lifestyle counseling were excluded.
Interventions had to be lifestyle orientated and focused on healthy eating or increased physical activity. Smoking could not be a main focus of the trial. Trials must have been conducted within the context of primary care and carried out by primary care providers, such as family physicians or practice nurses. Trials had to have had control groups who were managed with usual care. Usual care could include distribution of basic lifestyle messages, such as the literature on healthy living typically handed out by health professionals.
Both authors reviewed the articles independently using the criteria outlined in the users guides by Guyatt et al.8 Criteria used to assess the validity of the articles included randomization, accountability and follow-up after the study, intention-to-treat analysis, blinding and concealment, homogeneity, similarity of study and control groups, and evidence of contamination or simultaneous interventions. The reviewers were not blinded to the authors of the articles nor to the citation sources, but it turns out they were not familiar with any of the authors of the articles included. Reviewers considered both overall study validity and applicability to general practice. Overall assessment included details of studies’ methodology, patient populations, interventions and controls, and clinical aspects. Agreement as to whether an article would be included was settled by consensus after the independent reviews.
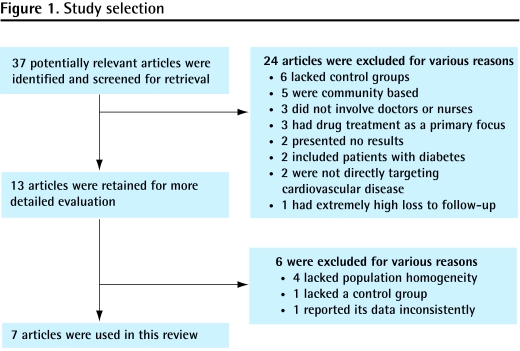
As shown in the flow diagram (Figure 1), our initial literature search identified 37 articles of which 24 were excluded. The remaining 13 articles9–21 were reviewed in more detail. Among these 13 articles, 4 were excluded because the study populations lacked homogeneity9–12 (eg, they included primary and secondary prevention patients), 1 was excluded because it lacked a control group,13 and another because of a lack of consistency in data reporting.14 In the end, 7 studies were included in the review (Table 1).15–21
Figure 1.
Study selection
Table 1.
Articles included in this review
| STUDY | DESIGN | SAMPLE | INTERVENTION GROUP | CONTROL GROUP | OUTCOMES MEASURED |
|---|---|---|---|---|---|
| Baron et al,15 1990 | RCT with 12-mo follow-up at a single general practice | 368 subjects (189 men, 179 women) aged 25–60 y were recruited in England. Mean age for the intervention group was 41.2 y (SD 1.0 y) for men and 41.1 y (SD 1.0 y) for women, and for the control group was 41.6 y (SD 1.0 y) for men and 41.9 y (SD 1.1 y) for women | 97 men and 90 women were given dietary advice and guidelines by a practice nurse in 30-min group or individual sessions. Subjects were given a diet booklet containing advice and recipes. There was a brief follow-up at 1 and 3 mo. Advice was to decrease intake of total fat and increase intake of polyunsaturated fatty acids and fibre. Retention rate was 89% | 92 men and 89 were given usual care with no dietary advice. Retention rate was 93% | TC and LDL and HDL levels were assessed at 1-yr follow-up |
| OXCHECK study group,16 1995 | RCT with 36-mo follow-up at 5 general practices | 4121 subjects aged 35–64 y were recruited in the United Kingdom | 2205 subjects received lifestyle advice from a practice nurse at 45– to 60-min health checkups with 10- to 20-min follow-ups. Advice was tailored to individual patients’ risk factors. 1100 subjects received annual checkups, and 1105 did not. Retention rate was 81.7% | 1916 subjects received usual care. Retention rate was 81.3% | TC, BP, and BMI were assessed at 3-y follow- up |
| Elley et al,17 2003 | Cluster RCT with 12-mo follow-up at 23 intervention and 19 control practices | 878 subjects (296 men, 582 women) aged 40–79 y were recruited from general practices in New Zealand. Mean age for the intervention group was 57.2 y (SD 10.8 y) and for the control group was 58.6 y (SD 11.5 y). Only subjects considered “less active” (< 30 min of physical activity 5 d/wk) were enrolled | 451 subjects (150 men, 301 women) received counseling on physical activity from a GP or practice nurse. Clinicians counseled verbally then gave out written advice on home-based exercise. Written advice and patient information were forwarded to exercise specialists who made 3, 10- to 20-min follow-up calls. Retention rate was 85% | 427 subjects (146 men, 281 women) received usual care. Retention rate was 85% | Cardiovascular risk score, BP, and BMI were assessed at 1-y follow-up |
| Kastarinen et al,18 2002 | Open RCT with 24-mo follow-up at 10 primary care centres | 341 subjects (48% male in intervention group and 46% male in control group) aged 25–74 y with primary hypertension were recruited in primary care in Finland. Mean age was 54.4 y (SD 10.1 y) in the intervention group and 54.2 y (SD 9.9 y) in the control group | 175 subjects in a no-drug treatment group were given lifestyle counseling (less sodium, alcohol, and saturated fat; weight reduction; physical activity) based on individual risk factors by practice nurses with visits at 1, 3, 6, 9, 15, 18, and 21 mo. Two 2-h group sessions on salt and weight reduction were held at 6 and 18 mo. Retention rate was 84% | 166 subjects received usual care. Retention rate was 80% | BP was assessed at 2-y follow- up |
| Roderick et al,19 1997 | RCT with 12-mo follow-up at 8 general practices | 956 subjects (48% male in intervention group and 52% male in control group) 30–59 y were recruited from general practices in the United Kingdom. Spouses were encouraged to enrol. Mean age was 47.2 y in the intervention group and 47.4 y in the control group | 473 subjects were given dietary advice based on negotiated change and healthy living literature by a practice nurse at an initial session. Nurses negotiated up to 5 diet changes based on a food- frequency questionnaire interpreted for individual cases. Overweight patients were given special diet plans with calorie- restricted diets. Retention rate was 80% overall | 483 subjects received usual care with standard healthy living literature and annual follow-up. Retention rate was 80% overall | TC, BMI, and BP were assessed at 1-y follow- up |
| Salkeld et al,20 1997 | RCT with 12-mo follow-up at 75 general practices | 755 subjects (387 men, 368 women) 18–69 y with ≥ 1 modifiable risk factors for CVD were recruited from general practices in Australia. Mean age in the group shown the video was 51 y for men and 52 y for women. Mean age in the group shown the video and given self-help materials was 50 y for men and 51 y for women. Mean age in the control group was 53 y for men and 56 y for women | 2 separate interventions were conducted by physicians: 269 subjects were shown a video on lifestyle, and 231 subjects were shown the video and also given written self-help materials. The interventions targeted healthy eating, physical activity, and smoking cessation. Retention rate for the video group was 74%; retention rate for the video and self-help materials group was 67% | 255 subjects received usual care. Retention rate was 51% | BP (diastolic only), TC, and BMI were assessed at 1-y follow-up |
| Steptoe et al,21 1999 | Cluster RCT with 12-mo follow-up at 20 general practices | 883 subjects (406 men, 477 women) with a mean age of 46.7 y (SE 0.4) were recruited from general practices in the United Kingdom. Subjects had ≥ 1 modifiable risk factor for CVD, such as high serum cholesterol or a high BMI | 316 subjects received behavioural counseling in 2–3, 20-min sessions conducted by a practice nurse targeted at healthy eating (low-fat, high fruit and vegetable intake), physical activity (increased to 12 moderately intense sessions/mo), and smoking cessation. The intervention operated on a “stages of change” model where counseling is tailored to individual readiness to change behaviour. Nurses telephoned subjects to reinforce counseling between sessions. Retention rate was 53% | 567 subjects received usual care. Retention rate was 62% | TC, BMI, and BP were assessed at 1-y follow-up |
BP—blood pressure, BMI—body mass index, CVD—cardiovascular disease, HDL—high-density lipoprotein, LDL—low-density lipoprotein, RCT—randomized controlled trial, SD—standard deviation, SE—standard error, TC—total cholesterol.
Because data were reported in various ways in the studies and because some information was missing (eg, no standard deviations, percentages without numbers), we could not adequately conduct a meta-analysis. We report outcome data in Table 2.15–21 In addition to determining the statistical significance of the outcomes, we assessed the relevance or importance of differences, when they were found, using the definitions shown in Table 3.
Table 2.
Summaries of outcome data in the 7 articles included in this study
| STUDY | OUTCOME | INTERVENTION GROUP | CONTROL GROUP | P VALUE | COMMENTS | EFFECT SIZE* |
|---|---|---|---|---|---|---|
| Baron et al,15 1990 | Mean TC (SE) men/women, mmol/L | 4.52 (0.08)/4.80 (0.11) | 4.50 (0.08)/4.84 (0.11) | NS | No significant effect for women or men. | None |
| Mean LDL levels (SE) men/ women, mmol/L | 2.36 (0.07)/2.71 (0.09) | 2.31 (0.08)/2.73 (0.10) | NS | Small sample size might account for this | None | |
| Mean HDL levels (SE) men/ women, mmol/L | 1.41 (0.03)/1.49 (0.03) | 1.48 (0.03)/1.53 (0.03) | NS | None | ||
| OXCHECK study group,16 1995 | Mean TC (SD) attenders/all, mmol/L | 5.93 (1.06)/5.99 (1.10) | 6.18 (1.17) | <.05 | A large sample size can show statistical significance even when the absolute difference is small | Small |
| Mean diastolic BP (SD) attenders/all, mm Hg | 126.8 (19.6)/126.5 (19.3) | 129.0 (20.4) | <.05 | Small | ||
| Mean systolic BP (SD) attenders/all, mm Hg | 75.7 (11.5)/75.7 (11.6) | 77.2 (11.7) | <.05 | Small | ||
| Mean BMI (SD) attenders/all, kg/m2 | 25.89 (4.14)/25.88 (4.21) | 26.26 (4.31) | <.05 | Small | ||
| Elley et al,17 2003 | Mean change (95% CI) in systolic BP, mm Hg | −2.58 (−4.02 to −1.13) | −1.21 (−2.57 to 0.15) | NS | No effect despite reasonable sample size and follow up by exercise specialists | None |
| Mean change (95% CI) in diastolic BP, mm Hg | −2.62 (−3.62 to −1.61) | −0.81 (−1.77 to 0.16) | NS | None | ||
| 4-y cardiovascular risk score (95% CI) | 0.42 (0.23 to 0.6) | 0.52 (0.32 to 0.72) | NS | None | ||
| Mean change (95% CI) in BMI, kg/m2 | −0.11 (−.25 to 0.02) | −0.05 (−0.18 to 0.07) | NS | None | ||
| Kastarinen et al,18 2002 | Mean change (95% CI) in systolic BP, mm Hg | −2.0 (−3.7 to −0.3) | −0.4 (−1.3 to 2.0) | <.05 | Small | |
| Mean change (95% CI) in diastolic BP, mm Hg | −2.4 (−3.4 to −1.4) | −0.4 (−1.4 to 0.8) | <.05 | Small | ||
| Roderick et al,19 1997 | Mean differences† (95% CI) in TC, mmol/L | −0.20 (−0.38 to −0.03) | <.05 | Use of practice nurses for dietary counseling to decrease cardiovascular risk scores was ineffective in a low-risk population | None | |
| Mean differences† (95% CI) in BMI, kg/m2 | −0.12 (−0.03 to 0.05) | NS | None | |||
| Mean differences† (95% CI) in systolic BP, mm Hg | −0.59 (−2.43 to 1.24) | NS | None | |||
| Mean differences (95% CI) in diastolic BP, mm Hg | 0.09 (−4.9 to 5.0) | NS | None | |||
| Salkeld et al,20 1997 | Mean change (95% CI) in diastolic BP‡ men/women, mm Hg | −4.0 (−6.02 to −1.97)/ −0.9 (−3.1 to 1.3) | −1.5 (−3.34 to 0.73)/ −4.0 (−6.37 to −1.7) | <.05/<.05 | Appears to be helpful only in improving diastolic BP in men | Moderate/ Negative |
| Mean change (95% CI) in TC‡ men/women, mmol/L | −0.46 (−0.75 to −0.13)/ −0.83 (−1.15 to −0.51) | −0.58 (−0.88 to −0.27)/ −0.58 (−0.81 to −0.35) | NS | None | ||
| Mean change (95% CI) in BMI‡ men/women, kg/m2 | 0.1 (−0.57 to 0.38)/ −0.03(−0.6 to 0.53) | −0.6 (−1.23 to −0.001)/ −0.3 (−0.48 to −0.15) | NS | None | ||
| Steptoe et al,21 1999 | Mean change (95% CI) in TC, mmol/L | −0.31 (−0.46 to −0.21) | −0.33 (−0.48 to −0.15) | NS | Appears to be helpful only in improving diastolic BP in men | None |
| Mean change (95% CI) in BMI, kg/m2 | 0.23 (−0.6 to 0.12) | −0.07 (−0.3 to 0.14) | NS | None | ||
| Mean change (95% CI) in systolic BP, mm Hg | −4.3 (−7.0 to −2.3) | −1.8 (−4.1 to 0.5) | NS | None | ||
| Mean change (95% CI) in diastolic BP, mm Hg | −0.7 (−0.31 to 1.6) | −1.0 (−2.0 to 0.01) | NS | None |
BP—blood pressure, BMI—body mass index, HDL—high-density lipoprotein, LDL—low-density lipoprotein, NS—not significant, SD—standard deviation, SE—standard error, TC—total cholesterol.
See Table 3.
Between intervention and control groups.
Video and self-help materials group.
Table 3.
Definitions of effect size for each outcome
| OUTCOME | NONE | SMALL | MODERATE | LARGE |
|---|---|---|---|---|
| Cholesterol levels (TC, LDL, HDL) | P ≥ .05 | P < .05 and < 5% decrease in mean level compared with control group | P < .05 and 5%–10% decrease in mean level compared with control group | P < .05 and > 10% decrease in mean level compared with control group |
| Systolic BP | P ≥ .05 | P < .05 and < 4 mm Hg decrease in mean BP compared with control group | P < .05 and 4–7 mm Hg decrease in mean BP compared with control group | P < .05 and > 7 mm Hg decrease in mean BP compared with control group |
| Diastolic BP | P ≥ .05 | P < .05 and < 2 mm Hg decrease in mean BP compared with control group | P < .05 and 2–4 mm Hg decrease in mean BP compared with control group | P < .05 and > 4 mm Hg decrease in mean BP compared with control group |
| Weight or BMI | P ≥ .05 | P < .05 and < 5% decrease in mean weight compared with control group | P < .05 and 5%–10% decrease in mean weight compared with control group | P < .05 and > 10% decrease in mean weight compared with control group |
BMI—body mass index, BP—blood pressure, HDL—high-density lipoprotein, LDL—low-density lipoprotein, TC—total cholesterol.
SYNTHESIS
Overall, the studies found little benefit from lifestyle- orientated interventions compared with usual care. Three of the 6 studies that assessed blood pressure as an outcome found a small but significant benefit to lifestyle counseling versus usual care.16,18,20 Two of the 5 studies that assessed cholesterol levels as an outcome found a small but significant benefit of lifestyle counseling.16,19 Only 1 of the 5 studies that assessed body mass index showed significant benefit of counseling, but again the effect was small.16 Only 1 of the 7 studies included in this review measured cardiovascular risk scores as an outcome; it showed no significant improvement in risk between intervention and control groups.17 None of the articles included in this review measured mortality or morbidity as an outcome.
The studies used a variety of lifestyle interventions. Two used dietary interventions only.15,19 One study was strictly oriented toward physical activity.17 The remaining 4 studies16,18,20,21 used a combination of healthy-eating and staying-active messages. The interventions varied in duration from 1 to 9 months. There was also variation in who delivered the advice. In 1 study20 it was physicians only, in 2 others17,18 it was a combination of nurses and physicians, and in 4 studies15,16,19,21 it was nurses only. Details of the studies are shown in Tables 1 and 2.15–21
DISCUSSION
Usefulness of lifestyle interventions
This review allows us to answer, or at least get insight into, specific questions about the usefulness of lifestyle counseling interventions delivered in primary care settings.
Were outcomes affected by which primary care provider (physician or practice nurse) delivered the intervention?
Among the 4 studies15,16,19,21 in which a nurse alone delivered the intervention, only 1 showed a consistent positive benefit.16 The benefit was small, however, and the achievement of statistical significance was helped by a large sample size. The 1 study20 in which a primary care physician alone delivered the intervention showed the intervention was not effective at lowering cholesterol or body mass index, but did have a positive effect on diastolic blood pressure in men only. The intervention in this study was, however, complex and not easily generalizable to most practices. The 2 studies in which both physicians and nurses were involved17,18 showed little positive effect of the intervention. One study showed no benefit on any of the outcomes measured; the other looked at blood pressure only and showed a small but significant reduction. It does not appear to matter which primary care provider delivers the intervention. The results are generally not impressive.
Did adding external supports to the provider-delivered intervention improve outcomes?
Two studies17,20 used additional services with the primary care providers’ intervention. One study had exercise specialists follow up patients after initial counseling by physicians and nurses. The other had experts providing physicians with extra training. Neither of these studies showed benefit of the intervention except for a moderate improvement in diastolic blood pressure in men only.
Were overall cardiovascular risk scores affected by the lifestyle interventions?
The 1 study17 that looked at cardiovascular risk scores showed no benefit from the intervention, even though there was a reasonable sample size (N = 878), and the intervention was delivered by physicians and nurses with follow-up by exercise specialists.
Were specific components of risk (blood pressure, weight, lipid levels) affected by the lifestyle interventions?
Only 416,18–20 of the 7 studies in this review showed any positive effect of lifestyle interventions. The main effects were on blood pressure and to a lesser degree on lipids. In general, effects were small.
Were morbidity and mortality affected by the lifestyle interventions?
These outcomes were not measured in any of the 7 studies included in the review.
Limitations
The main limitation of this review was the inability to conduct a meta-analysis because the study populations were not homogeneous and the presentation of results was done in a variety of ways. Since a meta-analysis was not done, we could not assess the likelihood of a negative result bias because we could not construct a funnel plot. We did not search non-English literature; it is possible that valid articles on the topic exist in other languages. We searched the 2 major medical databases (MEDLINE and EMBASE) and the major allied health database (CINAHL). It is unlikely that there is much primary care or family practice literature that has not been captured by the 3 databases we searched.
Future research
More sustained intensive programs of lifestyle counseling, delivered by health educators with backgrounds in nutrition and exercise, might be more effective. This has been shown to be the case outside the primary care setting in the Diabetes Prevention Program7 study. A randomized controlled trial (the PROACTIVE study22) is currently under way in Canada, funded by the Canadian Institutes for Health Research, looking at the use of an intensive program of lifestyle counseling delivered during many visits over a 2-year period. The intervention is being delivered in primary care settings, but by providers referred to as health educators with backgrounds in exercise and health promotion. We await the results of this trial to know whether outcomes will be improved using this approach in primary care.
Conclusion
This review looked at lifestyle counseling interventions delivered by primary care providers in primary care settings to patients at low risk of cardiovascular disease (primary prevention). The effects of the interventions were far from striking. Only 2 of the 7 studies showed consistently positive results, and these were primarily around improvements in blood pressure. The improvements were small, in the range of 2 mm Hg difference between intervention and control groups. While we did not formally look at high-risk patients, several of the studies we encountered looked at both high- and low-risk patients. It appears that patients at higher risk (those with pre-existing ischemic heart disease or diabetes) might benefit more from lifestyle counseling than the low-risk patients we studied. In general, while it is difficult to suggest that primary care providers not counsel all their patients on healthy lifestyles, their time might be better spent focusing on those at higher risk. It is possible that more sustained intensive programs of lifestyle counseling, delivered by health educators with backgrounds in nutrition and exercise, are more effective.
EDITOR’S KEY POINTS
This systematic review was conducted to determine whether lifestyle interventions delivered in primary care settings by primary care providers to their adult patients were effective in changing factors related to cardiovascular risk.
Overall, for cardiovascular risk scores, blood pressure, lipid levels, weight or body mass index, morbidity, and mortality outcomes, the studies found little benefit from lifestyle-orientated interventions compared with usual care.
While it is difficult to suggest that primary care providers not counsel all their patients on how to lead healthy lives, their time might be better spent focusing on those patients at higher risk.
POINTS DE REPÈRE DU RÉDACTEUR
Cette revue systématique voulait déterminer si les interventions des soignants de première ligne auprès de leurs patients adultes concernant leur mode de vie étaient efficaces pour modifier les facteurs de risque cardiovasculaires.
Dans l’ensemble, les études ont montré que par rapport aux soins habituels, les interventions visant le mode de vie avaient peu d’effet bénéfique sur l’indice de risque cardiovasculaire, la tension artérielle, le niveau des lipides, le poids et l’indice de masse corporelle, la morbidité et la mortalité.
Même si on peut difficilement suggérer aux intervenants de première ligne de ne pas renseigner leurs patients sur un mode de vie sain, il pourrait être plus avantageux pour eux de consacrer davantage de temps aux patients à haut risque.
Footnotes
This article has been peer reviewed.
Competing interests
None declared
Contributors
Mr Fleming and Dr Godwin contributed to concept and design of the study; data gathering, analysis, and interpretation; and preparing the article for submission.
References
- 1.Kohl H., 3 Physical activity and cardiovascular disease: evidence for a dose response. Med Sci Sports Exerc. 2001;33(6 Suppl):S472–83. doi: 10.1097/00005768-200106001-00017. discussion S493–4. [DOI] [PubMed] [Google Scholar]
- 2.Pope CR. Lifes-styles, health status and medical care utilization. Med Care. 1982;20(4):402–13. doi: 10.1097/00005650-198204000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Tucker LA, Clegg AG. Differences in health care costs and utilization among adults with selected lifestyle-related risk factors. Am J Health Promot. 2002;16(4):225–33. doi: 10.4278/0890-1171-16.4.225. [DOI] [PubMed] [Google Scholar]
- 4.Wang F, McDonald T, Reffitt B, Edington DW. BMI, physical activity, and health care utilization/costs among medicare retirees. Obes Res. 2005;13(8):1450–7. doi: 10.1038/oby.2005.175. [DOI] [PubMed] [Google Scholar]
- 5.Johansson SE, Sundquist J. Change in lifestyle factors and their influence on health status and all-cause mortality. Int J Epidemiol. 1999;28:1073–80. doi: 10.1093/ije/28.6.1073. [DOI] [PubMed] [Google Scholar]
- 6.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–40. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V Indian Diabetes Prevention Programme (IDPP) The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1) Diabetologia. 2006;49(2):289–97. doi: 10.1007/s00125-005-0097-z. [DOI] [PubMed] [Google Scholar]
- 8.Guyatt GH, Sackett D, Cook DJ Evidence Based Medicine Working Group. Users guides to the medical literature. II: How to use an article about therapy or prevention. A. Are the results of the study valid? JAMA. 1993;270(21):2598–601. doi: 10.1001/jama.270.21.2598. [DOI] [PubMed] [Google Scholar]
- 9.Jalkanen L. The effect of a weight reduction program on cardiovascular risk factors among overweight hypertensives in primary health care. Scand J Soc Med. 1991;19(1):66–71. doi: 10.1177/140349489101900112. [DOI] [PubMed] [Google Scholar]
- 10.Ketola E, Makela M, Klockars M. Individualised multifactorial lifestyle intervention trial for high-risk cardiovascular patients in primary care. Br J Gen Pract. 2001;51(465):291–4. [PMC free article] [PubMed] [Google Scholar]
- 11.Korhonen M, Kastarinen M, Uusitupa M, Puska P, Nissinen A. The effect of intensified diet counseling on the diet of hypertensive subjects in primary health care: a 2-year open randomized controlled trial of lifestyle intervention against hypertension in eastern Finland. Prev Med. 2003;36(1):8–16. doi: 10.1006/pmed.2002.1120. [DOI] [PubMed] [Google Scholar]
- 12.Eriksson KM, Westborg CJ, Eliasson MC. A randomized trial of lifestyle intervention in primary healthcare for the modification of cardiovascular risk factors. Scand J Public Health. 2006;34(5):453–61. doi: 10.1080/14034940500489826. [DOI] [PubMed] [Google Scholar]
- 13.Willaing I, Ladelund S, Jorgensen T, Simonsen T, Nielsen LM. Nutritional counselling in primary health care: a randomized comparison of an intervention by general practitioner or dietitian. Eur J Cardiovasc Prev Rehabil. 2004;11(6):513–20. doi: 10.1097/01.hjr.0000152244.58950.5f. [DOI] [PubMed] [Google Scholar]
- 14.Randomised controlled trial evaluating cardiovascular screening and intervention in general practice: principal results of the British family heart study. Family Heart Study Group. BMJ. 1994;308(6924):313–20. [PMC free article] [PubMed] [Google Scholar]
- 15.Baron JA, Gleason R, Crowe B, Mann JI. Preliminary trial of the effect of general practice based nutritional advice. Br J Gen Pract. 1990;40(333):137–41. [PMC free article] [PubMed] [Google Scholar]
- 16.Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. Imperial cancer research fund OXCHECK study group. BMJ. 1995;310(6987):1099–104. [PMC free article] [PubMed] [Google Scholar]
- 17.Elley CR, Kerse N, Arroll B, Robinson E. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial [abstract] BMJ. 2003;326(7393):793. doi: 10.1136/bmj.326.7393.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kastarinen MJ, Puska PM, Korhonen MH, Mustonen JN, Salomaa VV, Sundvall JE, et al. Non-pharmacological treatment of hypertension in primary health care: a 2-year open randomized controlled trial of lifestyle intervention against hypertension in eastern Finland. J Hypertens. 2002;20(12):2505–12. doi: 10.1097/00004872-200212000-00031. [DOI] [PubMed] [Google Scholar]
- 19.Roderick P, Ruddock V, Hunt P, Miller G. A randomized trial to evaluate the effectiveness of dietary advice by practice nurses in lowering diet-related coronary heart disease risk. Br J Gen Pract. 1997;47(414):7–12. [PMC free article] [PubMed] [Google Scholar]
- 20.Salkeld G, Phongsavan P, Oldenburg B, Johannesson M, Convery P, Graham-Clarke P, et al. The cost-effectiveness of a cardiovascular risk reduction program in general practice. Health Policy. 1997;41(2):105–19. doi: 10.1016/s0168-8510(97)00015-8. [DOI] [PubMed] [Google Scholar]
- 21.Steptoe A, Doherty S, Rink E, Kerry S, Kendrick T, Hilton S. Behavioural counselling in general practice for the promotion of healthy behaviour among adults at increased risk of coronary heart disease: randomised trial. BMJ. 1999;319(7215):943–7. doi: 10.1136/bmj.319.7215.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Institute of Nutrition, Metabolism, and Diabetes. Prevention and reduction of obesity through active living (PROACTIVE): an effectiveness trial. Ottawa, ON: Canadian Institute of Health Research; 2004. [Accessed 14 October 2008]. Available from: www.cihrirsc.gc.ca/e/24556.html. [Google Scholar]