Abstract
Objective
Although the offspring of parents with major depressive disorder (MDD) are at increased risk to develop disruptive behavior disorders (DBD) in addition to MDD, it remains unclear whether this heightened risk is due to MDD or to comorbid DBD in the parents.
Method
In a secondary analysis of longitudinal data from offspring at risk for MDD and panic disorder and comparison children, we stratified 169 children of parents who had been treated for MDD based upon presence (n=50) or absence (n=119) of parental history of DBD (ADHD, oppositional disorder, and conduct disorder) and contrasted them with children of parents with DBD but without MDD (n=19) and children whose parents had neither MDD nor DBD (n=106). The children had been assessed in middle childhood using structured diagnostic interviews.
Results
Offspring of parents with MDD+DBD had significantly higher rates of MDD, DBD in general, and ADHD in particular, compared with offspring of parents with MDD alone. Offspring of parents with MDD+DBD also had higher rates of mania than controls. Both parental MDD and DBD conferred independent risk for MDD and DBD in the offspring. However, only parental DBD conferred independent risk for conduct disorder and ADHD and only parental MDD conferred independent risk for oppositional defiant disorder.
Conclusion
Elevated rates of DBD in the offspring of parents with MDD appear to be due in part to the presence of DBD in the parents. Further studies of samples not selected on the basis of parental panic disorder are needed to confirm these results.
Keywords: Disruptive behavior disorders, major depression, high-risk offspring
Introduction
Numerous top-down high-risk studies have documented that parental major depressive disorder (MDD) confers risk in the offspring for disruptive behavior disorders (DBD). For example, in a study of a high-risk offspring sample, our group found that parental MDD conferred an increased risk for disruptive behavior disorders in children at mean age of 10.1 years (Odds Ratio 2.7, 95% confidence interval: 1.4-5.3, p=.003) (Biederman et al., 2006). Radke-Yarrow and colleagues (1992) also found among children in middle to late childhood that between 22-42% of children with a parent with unipolar depression had a DBD compared to only 3-8% of comparison control children. In a pooled analysis of the data from seven previous studies, Faraone and Biederman (1997) concluded that 12.4% of 475 children of depressed parents had ADHD compared to only 6.6% of 395 children of control parents (X2(1)=6.0, p=.01). Rates of conduct disorder among children of parents with MDD have also been reported to range from 6.5-32% compared with 1.2-8% in offspring of non-depressed controls (Beardslee et al., 1988, Hammen et al., 1990, Weissman et al., 1984).
Bottom-up studies that examine the prevalence of psychiatric disorders in the parents of affected children have also found associations between ADHD and parental MDD. For example, higher rates of major depressive disorder were found among first-degree relatives of boys (Biederman et al., 1991) and girls (Faraone et al., 1991) with DSM-III attention-deficit disorder (ADD) than among relatives of children without ADD. In a large, case-controlled study of boys with ADHD, the first-degree relatives of ADHD probands were at greater risk for MDD compared to relatives of control children without ADHD (Biederman et al., 1992). Similarly, Nigg and Hinshaw (1998) found that boys with ADHD were more likely than control boys without psychiatric disorders to have mothers with a past-year history of MDD or anxiety.
Despite these findings, it is not clear whether associations between parental MDD and DBD in offspring are accounted for by the parental MDD itself, or by the presence of comorbid DBD in the affected parents or their spouses. Major depression is known to be highly comorbid with DBD, in both children and adults. A meta-analysis of child and adolescent community samples (Angold and Costello, 1993) found that among youths with MDD, rates of oppositional defiant disorder or conduct disorder ranged from 22.7%-83.3%, whereas among youths with oppositional defiant or conduct disorder, rates of MDD ranged from 8.5%-45.4%. Similarly, the replication of the National Comorbidity Survey found statistically significant associations between major depression and oppositional defiant disorder (tetrachoric correlation = .48) and ADHD (tetrachoric correlation = .50), but not conduct disorder in adults (Kessler et al., 2005). On the other hand, a population-based twin study found that prior onset of conduct disorder significantly increased the risk for later MDD in adults (Hettema et al., 2003). Thus, the increased risk for DBD in the offspring of parents with MDD may be attributable to the significant comorbidity between MDD and DBD in parents. In addition, parents with MDD may be more likely to partner with spouses with antisocial or disruptive behaviors (Marmorstein et al., 2004, Kim-Cohen et al., 2005), and both parental MDD and antisocial or disruptive behaviors have been shown to be significantly and independently associated with MDD and conduct disorder in offspring (Marmorstein and Iacono, 2005).
Although these studies support the hypothesis that the association between parental MDD and DBD in offspring may be attributable in part to a history of DBD in the parents, research on this question has been scarce. Kim-Cohen and colleagues (2005) found that a parental history of antisocial behavior accounted for approximately one-third of the association between maternal MDD and antisocial behavior in children (age seven), although maternal MDD was an independent predictor as well. These researchers also found that compared to children of mothers with MDD alone, children of mothers with MDD and antisocial behavior had higher rates of both antisocial behavior and DSM-IV conduct disorder (Kim-Cohen et al., 2006). However, these studies were limited by including only symptom counts of parents’ antisocial behavior and not a full assessment of parents’ life histories of disruptive behavior disorders including childhood disorders such as ADHD and oppositional defiant disorder.
This question has important scientific and public health implications. DBDs can be very debilitating to children, impeding their academic, social and familial functioning (Greene et al., 2002, Blackman et al., 2005). Understanding which familial factors put children at heightened risk for these disorders could enable the development of appropriate preventive interventions aimed at mitigating them. Thus, identifying a particular subgroup of children at highest risk (i.e. the offspring of parents with MDD with comorbid DBD) would enable that group to be targeted both for preventive intervention and for focused longitudinal studies to elucidate the etiological trajectory and behavioral, temperamental, neural, and genetic substrates of disruptive behavior disorders.
The main aim of the present study, therefore, was to assess whether the association between parental MDD and DBD in the offspring was accounted for by parental MDD, parental DBD, or both. To this end, we conducted a secondary analysis of data from a longitudinal sample of offspring of parents with MDD, with and without comorbid panic disorder, and controls without mood or anxiety disorders (Biederman et al., 2006), in which parental depression was found to be associated with childhood disruptive behavior disorders. We hypothesized that the increased rates of DBD in the offspring of depressed parents would be associated with DBD in their parents.
Method
Overview of Study
This study is a secondary analysis of data from a longitudinal study of a case controlled high-risk sample of over 300 children originally recruited between 1993-1998. As described in an earlier report (Biederman et al., 2001), we had recruited offspring of parents with panic disorder (with or without major depression), major depression without panic disorder, and comparison offspring whose parents were free of mood or major anxiety disorders. Both parents in each family had been assessed via structured clinical interviews at baseline, and children had been assessed diagnostically via structured clinical interviews at baseline and at five-year follow-up (Biederman et al., 2006).
Subjects
The present analysis included four groups of children: 1) children from 47 families with parents without DBD and without MDD (Controls, N=106; these included offspring of the original control parents recruited for the study, who did not have any mood or major anxiety disorders as well as a small group of offspring of parents with panic disorder alone without major depression), 2) children from 10 families with parents with DBD and without MDD (DBD, N=19), 3) children from 60 families with parents with MDD and without DBD (MDD, N=119), and 4) children from 30 families with parents with DBD and MDD (MD+DBD, N=50). DBDs in the parents were defined to include childhood history of attention-deficit hyperactivity disorder (ADHD), oppositional disorder, and/or conduct disorder. Specifically, among the 10 families in the DBD only group, four parents had a history of conduct disorder only, two had ADHD only, two had oppositional disorder only, one had oppositional plus conduct disorder and one had all three disorders. In the families from the MDD+DBD group, ten parents had a history of ADHD only, seven had oppositional disorder only, five had conduct disorder only, four had ADHD plus oppositional disorder, and one each had oppositional plus conduct, ADHD plus conduct, or all three disorders. Eleven of the 30 MDD+DBD families (comprising 22 children) were defined by MDD in one parent and DBD in the other; the other 19 families (comprising 28 children) had a parent with the comorbid condition. Parents with bipolar disorder were excluded from the analysis.
Subject Ascertainment
Parents with MDD had been recruited from hospital outpatient and HMO settings and advertisements and were included if they met full DSM–III–R criteria for MDD on the Structured Clinical Interview for DSM-III-R (Spitzer et al., 1990) (SCID). To ensure “caseness” of MDD, we included them in the present analysis only if they had been treated for MDD (with pharmacotherapy and/or psychotherapy). Parents who were acutely psychotic or suicidal had been excluded from the study. Comparison parents were recruited through advertisements to hospital personnel and in the community and were included only if both parents did not meet DSM–III–R criteria on the SCID for any major anxiety or mood disorders and had never received psychiatric treatment. The institutional review board at the Massachusetts General Hospital approved all study protocols. At baseline and follow-up, after complete description of the study to the subjects, written informed consent was obtained. All parents signed written consent for themselves and their children. Children assented to study procedures, with those 7 and older signing written assent forms which were read to them.
Diagnostic Assessments
Both parents from each family were assessed at baseline using the SCID-III-R, amended to include modules from the Kiddie Schedule for Affective Disorders and Schizophrenia, Epidemiologic Version (K-SADS-E) for DSM-III-R (Puig-Antich and Ryan, 1986) assessing childhood ADHD, oppositional disorder, and conduct disorder. Children who reached the age of 5 by the end of the first five-year grant period were assessed during the first wave of the study, based upon interviews with the mother using the DSM-III-R-based K-SADS-E. Interviewers were blind to ascertainment group and to all diagnostic information about the parents. The children were a mean age of 6.8 years at the initial diagnostic assessment. Socioeconomic status (SES) was assessed using the Hollingshead Four-Factor Index (Hollingshead, 1975).
Follow-up assessments were done a median of five years after baseline diagnostic assessments (mean 4.5 years, SD 1.5) by interviewers blind to all previous information about the child and family. Because some younger siblings were assessed for the first time at this wave, the children assessed had a mean age of 10.1 years. Assessments of the children at this wave relied on the DSM-IV based K-SADS-E (Orvaschel and Puig-Antich, 1987). We interviewed the mothers for all subjects and directly interviewed subjects older than 12 years. We considered a disorder positive if diagnostic criteria were unequivocally met in either the parent or child interview.
Diagnostic interviewers had bachelor’s or master’s degrees in psychology and were trained to high levels of inter-rater reliability. All interviews were presented for review to a committee of board-certified child and adult psychiatrists and licensed psychologists who were blind to the subject’s ascertainment status, referral source, and all other data, to resolve diagnostic uncertainties. Diagnoses were considered positive only if a consensus was achieved that criteria were met to a degree that would be considered clinically meaningful. We computed kappa coefficients of agreement for all diagnoses by having experienced, board certified child and adult psychiatrists and licensed clinical psychologists diagnose subjects from audiotaped interviews made by the assessment staff. Based on 500 assessments from interviews of children and adults, the median kappa coefficient was .98 with excellent agreement for ADHD (0.88), conduct disorder (CD;1.0), oppositional defiant disorder (ODD; .90), major depression (1.0), mania (0.95).
In the present analysis, we included all children for whom follow-up diagnostic assessments were available, and supplemented the lifetime diagnoses reported in these interviews with lifetime disorders that had been reported at the initial diagnostic interview.
Data Analysis
Analyses were conducted using STATA (Stata, 2005). We first compared the four groups of offspring on demographic characteristics and other parental psychiatric disorders (panic disorder). Logistic regression, linear regression, or ordinal logistic regression was used depending on the distribution of the outcome. We then compared rates of mood and disruptive behavior disorders in offspring from the four groups using logistic regression, covarying any potential demographic confounds. Pairwise comparisons were conducted if the four group omnibus test was statistically significant. To account for non-independence of siblings, we used Huber correction to produce robust variances. Finally, in order to examine the degree to which parental MDD, independently from parental DBD, or parental DBD, independently from parental MDD, predicted child disorders, we conducted logistic regression analyses in which both presence or absence of MDD in a parent and presence or absence of DBD in a parent were included in the equation, and we examined the odds ratios for each parental disorder predicting each child outcome independently of the other. All tests were two-tailed with alpha set at 0.05.
Results
Table 1 shows the demographic characteristics of the sample. All three groups of high-risk offspring differed from controls on SES, and the offspring of depressed parents differed from control offspring on rates of parental panic disorder. Therefore SES and parental panic disorder were covaried in all subsequent analyses.
Table 1.
Demographic Characteristics of the Four Offspring Groups
| Offspring of Controls (N=106) | Offspring of Parents with DBD (N=19) | Offspring of Parents with MDD (N=119) | Offspring of Parents with MDD+DBD (N=50) | Test Statistic | p-value | |
|---|---|---|---|---|---|---|
| Mean±SD or n (%) | Mean±SD or n (%) | Mean±SD or n (%) | Mean±SD or n (%) | |||
| Age | 10.0 ± 3.4 | 10.6 ± 2.8 | 10.3 ± 4.1 | 11.0 ± 5.6 | F(3,146)=0.39 | 0.76 |
| Gender (Male) | 54 (51) | 15 (79) | 64 (54) | 26 (52) | χ2 (3)=5.48 | 0.14 |
| Family SES | 1.7 ± 0.9 | 2.3 ± 1.0 a* | 2.5 ± 1.1 a*** | 2.4 ± 0.9 a** | χ2 (3)=17.10 | <0.001 |
| Parent with Panic Disorder | 19 (18) | 8 (42) | 85 (71) a*** | 37 (74) a*** | χ2 (3)=28.38 | <0.001 |
=vs. Controls;
=vs. DBD;
=vs. MDD;
p≤0.05;
p≤0.01;
p≤0.001.
DBD=disruptive behavior disorders (includes history of ADHD, oppositional disorder, and/or conduct disorder). MDD=major depressive disorder. SES=Socioeconimic status.
Although offspring of parents with MDD, irrespective of comorbidity with DBD, had higher rates of DBD than offspring of comparison parents without MDD or DBD, the rates of DBD were significantly higher among offspring of parents with MDD+DBD than among offspring of parents with MDD alone (z=2.36, p=.02). Similarly, ADHD was significantly elevated in the offspring of parents with MDD+DBD compared with the offspring of parents with MDD only (z=2.08, p=.04). In addition, the rate of MDD was significantly higher in the offspring of parents with MDD+DBD compared with those of parents with MDD alone (z=2.00, p=.04). Oppositional defiant disorder and MDD were both significantly higher in both the MDD+DBD and MDD groups compared with controls without MDD or DBD. In contrast, conduct disorder and mania were significantly elevated (versus offspring of unaffected controls) only among the offspring of parents with MDD+DBD.
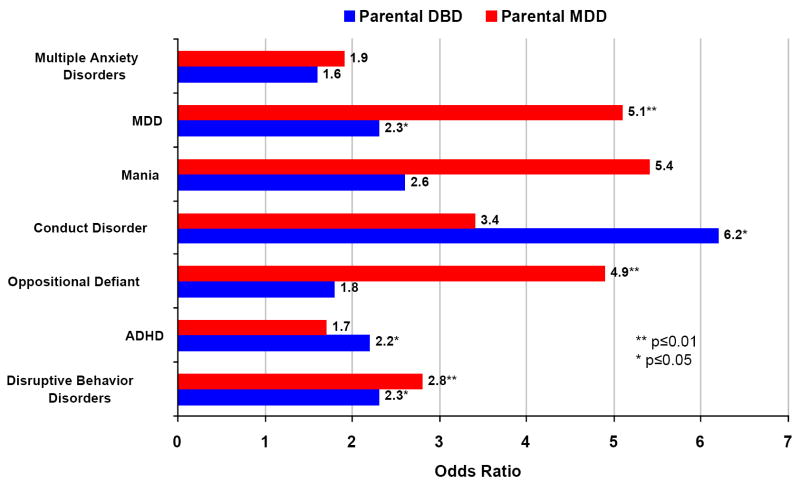
Figure 1 shows the risk for psychiatric disorders in offspring conferred by parental DBD versus no parental DBD and parental MDD versus no parental MDD, independent of the presence or absence of the other parental diagnosis (MDD or DBD, respectively). As can be seen, both parental MDD and parental DBD conferred independent risk for MDD and DBD in the offspring. However, only parental DBD conferred independent risk for conduct disorder and ADHD, and only parental MDD conferred independent risk for oppositional defiant disorder in the offspring.
Figure 1.
Risk for psychiatric disorders in offspring conferred by parental disruptive behavior disorders (DBD) and parental major depression (MDD)
To examine whether the association between parental and child DBDs might have been accounted for by overall severity of parental psychopathology among parents in the MDD+DBD group, indexed by total number of lifetime comorbid disorders, we examined whether children from the four parental groups differed on total lifetime disorders in both parents, added together, including MDD, mania, dysthymia, panic disorder, agoraphobia, GAD, OCD, specific and social phobias, PTSD, alcohol and substance abuse and dependence, anorexia, bulimia, and adult antisocial disorder. We excluded the childhood DBDs, on the basis of which the groups had been constructed. We found that the groups did differ, with means of 2.5 (SD 1.8) for the controls, 3.7 (SD 3.2) for the offspring of DBD, 5.9 (SD 2.8) for the offspring of MDD, and 8.2 (SD 3.8) for the offspring of MDD+DBD. The MDD group differed significantly from controls, and the MDD+DBD group differed significantly from all other groups (χ2 (3)=33.99, p<.0010). Additionally, the number of disorders in the children themselves (total number of DBDs, mood, and anxiety disorders) increased from group to group (mean=1.0, [SD=1.5]; 1.4 [1.8]; 2.0 [2.1]; 3.3 [2.4], respectively, χ2 (3)=15.85, p<.001, with the MDD+DBD group differing significantly from all others).
We therefore repeated all analyses covarying the number of parental disorders. Although the odds ratios for all significant comparisons in Table 2 remained over 2.0, the comparisons between the offspring of MDD+DBDs versus those of MDD alone dropped to trend or near-trend significance for DBD (OR=2.1 [0.97,4,6], z=2.13, p=0.06), ADHD (2.2 [0.9,5.6], z=2.21, p=0.10), and MDD (2.3 [0.8,6.3], z=2.25, p=0.12) due to diminished statistical power. For the binary predictor analysis (Figure 1), the odds ratios for the prediction of child DBDs (OR=1.9, p=0.052), of child ADHD (OR=2.0, p=0.07), and of child MDD (OR=2.1, p=0.11) by parental DBDs remained in the same 2.0-range, but dropped to trend or near-trend significance. All other comparisons remained significant. Finally, we compared rates of parental comorbid disorders between children with and without DBDs, separately within the offspring of MDD and within the offspring of MDD+DBD. In both cases, the number of parental comorbid disorders did not differ between children with and without DBDs (offspring of MDD: OR= 1.1[.97-1.3], z=1.49, p=.14; offspring of MDD+DBD: OR=1.1 [.91-1.2], z=0.74, p=.46).
Table 2.
Rates of Disorders in the Four Offspring Groups
| Offspring of Controls (N=106) | Offspring of Parents with DBD (N=19) | Offspring of Parents with MDD (N=119) | Offspring of Parents with MDD+DBD (N=50) | Test Statistic | p-value | |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |||
| DBD | 17 (16) | 5 (26) | 43 (36) a** | 29 (58) a*** c* | χ2 (3)=16.48 | <0.001 |
| ADHD | 13 (12) | 4 (21) | 26 (22) | 20 (40) a* c* | χ2 (3)=8.18 | 0.04 |
| ODD | 6 (6) | 1 (5) | 26 (22) a** | 18 (36) a*** | χ2 (3)=14.20 | 0.003 |
| CD | 0 (0) | 1 (5) | 3 (3) | 4 (8) a** | Fisher’s Exact | 0.02 |
| BPD | 1 (1) | 0 (0) | 3 (3) | 5 (10) a* | Fisher’s Exact | 0.05 |
| MDD | 3 (3) | 1 (5) | 17 (14) a* | 14 (28) a** c* | χ2 (3)=13.07 | 0.004 |
| Multiple Anxiety Disorders (≥2) | 17 (16) | 3 (16) | 40 (34) | 26 (52) | χ2 (3)=5.72 | 0.13 |
=vs. Controls;
=vs. DBD;
=vs. MDD;
p≤0.05;
p≤0.01;
p≤0.001.
DBD=disruptive behavior disorders (includes history of ADHD, oppositional disorder, and/or conduct disorder). MDD=major depressive disorder. ADHD=attention deficit-hyperactivity disorder, ODD=oppositional defiant disorder, CD=conduct disorder, BPD=Bipolar disorder.
Discussion
This study investigated whether the association between parental major depressive disorder (MDD) and elevated risk for disruptive behavior disorders (DBD) in the offspring is accounted for by parental MDD, parental DBD, or both. We found that the offspring of parents with MDD plus DBD had significantly higher rates of DBD in general, and ADHD in particular, than those of parents with MDD alone. Analysis of the unique risk contributed by parental MDD and parental DBD, respectively, revealed that both parental MDD and DBD conferred independent risk for MDD and DBD in the offspring, whereas only parental DBD conferred independent risk for conduct disorder and ADHD, and only parental MDD conferred independent risk for oppositional defiant disorder. These findings support the study hypothesis and suggest that the elevated rates of DBD in the offspring of parents with MDD may be due in part to the presence of DBD in the parents themselves.
Our findings confirm and extend results by other groups suggesting that some of the elevated DBD among offspring of depressed mothers are accounted for by antisocial behaviors in the mothers or fathers (Kim-Cohen et al., 2005, 2006, Marmorstein et al., 2004). Our study extends these findings by demonstrating that childhood parental history of disruptive behavior disorders (including ADHD and oppositional disorder as well as conduct disorder) contribute to this increased risk.
The specific association between parental DBD and childhood conduct disorder and ADHD in our study is consistent with studies documenting the heritability of conduct disorder (Gelhorn et al., 2006) and ADHD (Faraone et al., 2005). The specific association between parental MDD and childhood oppositional defiant disorder is interesting given the frequent comorbidity between oppositional defiant disorder and mood disorders (Kessler et al., 2005) and the similarities in affective dysregulation between the two disorders (Greene and Doyle, 1999). Additional work is needed to clarify whether symptoms of oppositional defiant disorder are an early characteristic of or marker of risk for major depression. One hypothesis is that the negative affect reactivity and ease to anger found among children with ODD may represent, in some cases, subthreshhold presentations of irritable depression.
Another possibility is that DBDs in the children and parents may be a reflection of a temperamental factor which may be a precursor to MDD. For example, emotionality or negative affectivity, especially in the absence of positive affectivity, has been associated with risk for MDD (Lonigan et al., 2003), and high emotionality (in particular expressions of anger) in early childhood has been found also to predict onset of disruptive behavior symptoms (Rydell et al., 2003). Additionally, our group has found that motivational behavioral disinhibition, defined as the reactive tendency to exhibit boldness, heightened exploration, and talkativeness in unfamiliar settings, measured in the preschool years predicts elevated risk for disruptive behavior disorders and comorbid mood disorders in early and middle childhood (Hirshfeld-Becker et al., 2004, 2007). Therefore, DBDs may be indexing a temperamental precursor to MDD, which puts the child at risk for a trajectory consisting of behavioral disinhibition in toddlerhood or preschool years, disruptive behavior disorders in childhood, and MDD later in childhood, adolescence or adulthood. Longitudinal studies following disinhibited children over time are needed to further examine this possibility.
The elevated rate of mania among the offspring of parents with MDD+DBD is noteworthy. Although we excluded offspring whose parents had met full criteria for mania, and although we assessed all parents carefully with the SCID, it is possible that some of the parents from the MDD+DBD group might have had undetected bipolar spectrum illness. Family studies have shown that among offspring of parents with bipolar disorder, the rate of ADHD is approximately three times higher than among offspring of normal controls, and that bipolar disorder is twice as common among relatives of ADHD probands compared to relatives of normal control probands (Faraone et al., 1997). However, since only approximately 20% of the first-degree relatives of patients with bipolar disorder have bipolar disorder themselves, and since it is very common for these relatives to have unipolar depression and disruptive behavior disorders (e.g. Chang et al., 2003; Joyce et al., 2004), it is equally plausible that parental unipolar depression and comorbid parental DBDs confer additive risk for bipolar disorder.
The strengths of this study include the complete assessment of both parents in each family with standardized, well-validated diagnostic instruments that evaluated childhood as well as adulthood psychiatric disorders; the blind assessments of children with structured diagnostic interviews; and the large sample size.
However, our results should be considered in light of several limitations. First, parental DBDs were assessed based upon retrospective reports by parents using structured diagnostic interviews and, with the exception of some parents who still met criteria for ADHD, were not observed directly. Second, because parents with MDD+DBD also had more comorbid disorders and had children with higher numbers of comorbid disorders, we cannot be sure whether the associations we observed represent a specific relationship between parental and child DBDs, or a case of greater severity in parents breeding greater severity in children. When we covaried parental comorbidity in our analyses, only the specific associations between parental DBD and child conduct disorder and between parental MDD and child DBD, ODD, and MDD remained. However, the odds ratios for all previously significant associations remained at or close to 2.0, and the significances for most remained at trend level, suggesting that the loss in significance may have been due to reduced power. Moreover, if it was parental comorbid disorders and not parental DBDs that were conferring risk for child DBDs, we would expect that within the group of offspring of MDD and within the group of offspring of MDD+DBD, presence of child DBDs would be associated with higher numbers of parental comorbid disorders. However, this was clearly not the case. In further support of a specific association between parental and child DBDs is the fact that parental MDD+DBD conferred increased risk only for the DBDs (DBDs in general, ADHD, and conduct disorder) and not for all disorders in general (e.g. the anxiety disorders), as would be expected if the effect were simply of severity in parents conferring increased severity in children. Similarly, some disorders (e.g. ADHD) did not show a step-wise increase across groups as would be expected if they were linked to increasing parental comorbidity. This issue needs further study in larger samples.
Third, since our analysis was conducted on a sample of offspring of parents with panic disorder, many affected parents also had comorbid panic disorder. Therefore it is not known how results would generalize to samples of offspring of parents with MDD and DBD alone. Third, the group of offspring of parents with DBD without MDD was very small, and the size of this group may have reduced the study’s power to detect differences, particularly in four-group comparisons. Fourth, assessments of children 12 and under relied on parental report. Future study waves, in which all the children will be old enough to be directly interviewed about their lifetime symptoms, will enable us to further assess the risk conferred by parental MDD and DBD. Finally, whereas our analysis covaried SES, other environmental factors, including exposure to parents’ symptoms of affective or behavioral dysregulation, might also influence the associations noted.
Despite these limitations, this study suggests that elevated rates of disruptive behavior disorders (DBD) in the offspring of parents with major depressive disorder (MDD) may be due in part to increased presence of DBD in the parents themselves. Further studies of samples not selected on the basis of parental panic disorder are needed to confirm these results. Clinically, our findings suggest that offspring of parents with MDD with DBD are at particularly elevated risk for DBD themselves, and that they should be targeted for preventive interventions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Angold A, Costello EJ. Depressive comorbidity in children and adolescents: Empirical, theoretical and methodological issues. Am J Psychiatry. 1993;150:1779–1791. doi: 10.1176/ajp.150.12.1779. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Keller MB, Lavori PW, Klerman GK, Dorer DJ, Samuelson H. Psychiatric disorder in adolescent offspring of parents with affective disorder in a non-referred sample. J Affect Disord. 1988;15:313–322. doi: 10.1016/0165-0327(88)90028-6. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone S, Hirshfeld-Becker D, Friedman D, Robin J, Rosenbaum J. Patterns of psychopathology and dysfunction in a large sample of high-risk children of parents with panic disorder and major depression: A controlled study. Am J Psychiatry. 2001;158:49–57. doi: 10.1176/appi.ajp.158.1.49. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Keenan K, Benjamin J, Krifcher B, Moore C, Sprich S, Ugaglia K, Jellinek MS, Steingard R, Spencer T, Norman D, Kolodny R, Kraus I, Perrin J, Keller MB, Tsuang MT. Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder (ADHD): Patterns of comorbidity in probands and relatives in psychiatrically and pediatrically referred samples. Arch Gen Psychiatry. 1992;49:728–738. doi: 10.1001/archpsyc.1992.01820090056010. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Keenan K, Tsuang MT. Evidence of familial association between attention deficit disorder and major affective disorders. Arch Gen Psychiatry. 1991;48:633–642. doi: 10.1001/archpsyc.1991.01810310051009. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty C, Hirshfeld-Becker DR, Henin A, Faraone SV, Dang D, Jakubowski A, Rosenbaum JF. A controlled longitudinal five year follow-up study of children at high and low risk for panic disorder and major depression. Psychol Med. 2006 doi: 10.1017/S0033291706007781. in press. [DOI] [PubMed] [Google Scholar]
- Blackman GL, Ostrander R, Herman KC. Children with ADHD and depression: a multisource, multimethod assessment of clinical, social, and academic functioning. J Atten Disord. 2005;8:195–207. doi: 10.1177/1087054705278777. [DOI] [PubMed] [Google Scholar]
- Chang K, Steiner H, Ketter T. Studies of offspring of parents with bipolar disorder. Am J Med Genet C Semin Med Genet. 2003;123:26–35. doi: 10.1002/ajmg.c.20011. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J. Do attention deficit hyperactivity disorder and major depression share familial risk factors? J Nervous Mental Diseases. 1997;185:533–541. doi: 10.1097/00005053-199709000-00001. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Keenan K, Tsuang MT. A family-genetic study of girls with DSM-III attention deficit disorder. Am J Psychiatry. 1991;148:112–117. doi: 10.1176/ajp.148.1.112. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Mennin D, Wozniak J, Spencer T. Attention-deficit hyperactivity disorder with bipolar disorder: a familial subtype? J Am Acad Child Adolesc Psychiatry. 1997;36:1378–1390. doi: 10.1097/00004583-199710000-00020. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, Sklar P. Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005;57:1313–23. doi: 10.1016/j.biopsych.2004.11.024. [DOI] [PubMed] [Google Scholar]
- Gelhorn H, Stallings M, Young S, Corley R, Rhee SH, Hewitt J. Genetic and environmental influences on conduct disorder: symptom domain and full-scale analyses. J Child Psychol Psychiat. 2006;46:580–591. doi: 10.1111/j.1469-7610.2004.00373.x. [DOI] [PubMed] [Google Scholar]
- Greene RW, Biederman J, Zerwas S, Monuteaux MC, Goring JC, Faraone S. Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. Am J Psychiatry. 2002;159:1214–1224. doi: 10.1176/appi.ajp.159.7.1214. [DOI] [PubMed] [Google Scholar]
- Greene RW, Doyle AE. Toward a transactional conceptualization of oppositional defiant disorder: Implications for assessment and treatment. Clinical Child and Family Psychology Review. 1999;2:129–148. doi: 10.1023/a:1021850921476. [DOI] [PubMed] [Google Scholar]
- Hammen C, Burge D, Burney E, Adrian C. Longitudinal study of diagnoses in children of women with unipolar and bipolar affective disorder. Arch Gen Psychiatry. 1990;47:1112–1117. doi: 10.1001/archpsyc.1990.01810240032006. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Prescott CA, Kendler KS. The effects of anxiety, substance use and conduct disorders on risk of major depressive disorder. Psychol Med. 2003;33:1423–32. doi: 10.1017/s0033291703008365. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker DR, Biederman J, Faraone SV, Violette H, Wrightsman J, Rosenbaum JF. Temperamental correlates of disruptive behavior disorders in young children: Preliminary findings. Biol Psychiatry. 2002;51:563–574. doi: 10.1016/s0006-3223(01)01299-9. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker DR, Biederman J, Henin A, Faraone SV, Micco JA, van Grondelle A, Henry B, Rosenbaum JF. Clinical outcomes of laboratory-observed preschool behavioral disinhibition at five-year follow-up. Biol Psychiatry. 2007 doi: 10.1016/j.biopsych.2006.10.021. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Position. Yale University; New Haven: 1975. [Google Scholar]
- Joyce PR, Doughty CJ, Wells JE, Walsh AE, Admiraal A, Lill M, Olds RJ. Affective disorders in the first-degree relatives of bipolar probands: results from the South Island Bipolar Study. Compr Psychiat. 2004;45:168–74. doi: 10.1016/j.comppsych.2004.02.005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demier O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Rutter M, Tomas MP, Moffitt TE. The caregiving environments provided to children by depressed mothers with or without an antisocial history. Am J Psychiatry. 2006;163:1009–18. doi: 10.1176/ajp.2006.163.6.1009. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Moffitt TE, Taylor A, Pawlby SJ, Caspi A. Maternal depression and children’s antisocial behavior: nature and nurture effects. Arch Gen Psychiatry. 2005;62:173–181. doi: 10.1001/archpsyc.62.2.173. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Phillips BM, Hooe ES. Relations of positive and negative affectivity to anxiety and depression in children: evidence from a latent variable longitudinal study. J Couns Clin Psychology. 2003;71:465–481. doi: 10.1037/0022-006x.71.3.465. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG. Longitudinal follow-up of adolescents with late-onset antisocial behavior: a pathological yet overlooked group. J Am Acad Child Adolesc Psychiatry. 2005;44:1284–91. doi: 10.1097/01.chi.0000181039.75842.85. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Malone SM, Iacono WG. Psychiatric disorders among offspring of depressed mothers: Associations with paternal psychopathology. Am J Psychiatry. 2004;161:1588–94. doi: 10.1176/appi.ajp.161.9.1588. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Hinshaw SP. Parent personality traits and psychopathology associated with antisocial behaviors in childhood attention-deficit hyperactivity disorder. J Child Psychol Psychiat. 1998;39:145–159. [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J. Schedule for Affective Disorder and Schizophrenia for School-Age Children-Epidemiologic 4th version. Nova University, Center for Psychological Study; Ft. Lauderdale: 1987. [Google Scholar]
- Puig-Antich J, Ryan ND. Schedule of affective disorders and schizophrenia for school-aged children (Kiddie-SADS) Western Psychiatric Institute and Clinic; Pittsburgh, PA: 1986. [Google Scholar]
- Radke-Yarrow M, Nottelman E, Martinez P, Fox MB, Belmont B. Young children of affectively ill parents: A longitudinal study of psychosocial development. J Am Acad Child Adolesc Psychiatry. 1992;31:68–77. doi: 10.1097/00004583-199201000-00011. [DOI] [PubMed] [Google Scholar]
- Rydell AM, Berlin L, Bohlin G. Emotionality, emotion regulation, and adaptation among 5- to 8-year-old children. Emotion. 2003;3:30–47. doi: 10.1037/1528-3542.3.1.30. [DOI] [PubMed] [Google Scholar]
- Spitzer R, WIlliams J, Gibbon M, First M. Structured Clinical Interview for DSM-III-R-Non-Patient Edition (SCID-NP, Version 1.0) American Psychiatric Press; Wash., DC: 1990. [Google Scholar]
- Stata . Stata User’s Guide: Release 9. Stata Corp LP; College Station, TX: 2005. [Google Scholar]
- Weissman MM, Prusoff BA, Gammon GD, Merikangas KR, Leckman JF, Kidd KK. Psychopathology in the children (ages 6-18) of depressed and normal parents. J Am Acad Child Adolesc Psychiatry. 1984;23:78–84. doi: 10.1097/00004583-198401000-00011. [DOI] [PubMed] [Google Scholar]