National and international pandemic influenza planning has been stimulated by concerns about an unprecedented panzootic of highly pathogenic avian influenza H5N1 virus, fatal to 245 humans as of September 10, 2008.1 In these planning efforts, public health officials have looked to previous influenza pandemics for information about prevention measures adopted and their proven or perceived efficacy. After the isolation of influenza A virus in 1930, and its serologic identification2 as the cause of the 1918–1919 influenza pandemic,3 vaccines were developed and used for seasonal influenza and in the subsequent pandemics of 1957 and 1968. Antiviral medications were used in the last two of these pandemics as well. Before these important advances, however, the principal countermeasure against pandemic influenza had been the application of sound public health practice based predominantly upon what has lately been called “community mitigation.”4
A 2007 review of historical information from 43 American cities during the 1918–1919 pandemic, the most explosive and fatal on record, suggests to some that standard public health measures might be beneficial in a future pandemic.4 Thus, it is of interest to consider expert consensus opinion about pandemic influenza prevention at the time of the 1918–1919 pandemic. This article examines one such report (based largely upon European and American experiences) from the principal international public health agency of the time, and compares it to modern prevention/mitigation recommendations.
BACKGROUND
Shortly after the 1918 influenza pandemic, the Paris-based Office internationale d'hygiène publique (OIHP), an international health organization established in 1907, published a report that included recommendations about community pandemic mitigation.5 This report appears to reflect contemporary conventional wisdom about influenza prevention and control, as expressed in many other public health documents from various nations (data not shown). In February 2007, the U.S. Centers for Disease Control and Prevention (CDC) released a comprehensive and well-articulated document outlining options and recommendations for community mitigation based on stratification of the severity of a potential influenza pandemic.6 The 2007 recommendations consider the 1918 pandemic, the most deadly in recorded history, as a “worst case scenario.”
COMPARISON OF 1921 AND 2007 GUIDELINES
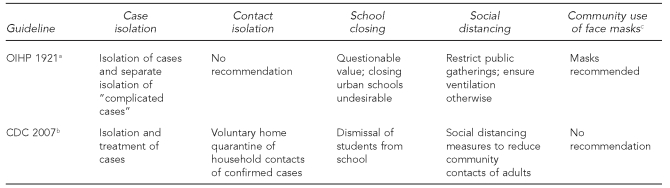
A side-by-side comparison of some of the issues addressed in these two documents—and the recommendations rendered—underscores the relevance of public health principles considered to be sound over a period spanning more than 90 years.
The 2007 CDC document is organized into four major categories of mitigation strategies that cover most of the major prevention topics found in the 1921 document (Figure 1). For example, although written nine years before the viral cause of influenza was identified, the 1921 document is consonant with today's understanding of influenza transmission in noting the importance of both aerosol droplets and hands soiled with “secretion-contaminated fomites.”5
Figure 1. Comparison of guidelines for community mitigation of pandemic influenza published in 1921a and 2007b.
aPottevin H. Rapport sur la pandémie grippale de 1918–1919 présenté au comité permanent de l'Office internationale d'hygiène publique. Bulletin de l'Office internationale d'hygiène publique 1921;13:125-81.
bCenters for Disease Control and Prevention (US). Interim pre-pandemic planning guidance: community strategy for pandemic influenza mitigation in the United States—early, targeted, layered use of nonpharmaceutical interventions. February 2007 [cited 2008 Oct 15]. Available from: URL: http://www.pandemicflu.gov/plan/community/community_mitigation.pdf
cThe four main mitigation categories addressed in the 2007 CDC guidelines do not include community-wide use of face masks, but do include contact isolation.
OIHP = Office internationale d'hygiène publique
CDC = Centers for Disease Control and Prevention
The OIHP guidelines also concur with those of CDC that isolation of ill individuals is “strictly necessary,” but add that it is also important to separately isolate complicated cases as early as possible after complications develop. This further recommendation apparently addresses the high rate of influenza, pneumonia, and other complications from transmissible secondary bacterial infections in 1918, which were associated with most of the influenza mortality then.7–9 Unlike CDC in 2007, voluntary home quarantine of people in contact with infected individuals was not recommended by the OIHP in 1921, probably because of uncertainty in that era about the period of influenza communicability and whether infection could be transmitted before onset of symptoms or in the absence of symptoms.8
Then, as now, the value of dismissing children from school was controversial. The OIHP document states, “A universal principle cannot be arrived at, seeing that it is a matter of different solutions according to local circumstances,” but adds that in urban locations, closing elementary schools seems undesirable because it places children at greater risk of contagion. Questions about closing schools during the 1918 pandemic arose in part because data regarding the efficacy of this strategy were lacking, as they remain today. Although not addressed in the OIHP report, an oft-repeated argument in favor of keeping schools open in 1918 was to provide an opportunity for responsible individuals such as school physicians, nurses, or teachers to diagnose and send home or care for ill children who might not otherwise have medical or first aid attention.
Finally, social distancing was directly addressed by the OIHP, as it is by CDC, particularly with respect to municipal bans, enacted by many cities, on public gatherings such as meetings, church services (Figure 2), and theater performances. When such meetings must take place, the OIHP report suggested that good ventilation was necessary to mitigate the risk of suspended infectious particles. The importance of good ventilation was undoubtedly of great concern in 1921 because many homes and buildings were poorly ventilated, especially in the winter when doors and windows were kept closed, and because of the generally low humidity in homes and buildings, which was believed to facilitate influenza transmission.
Figure 2. Sunday church services in San Francisco, 1918–1919.
Sunday church services were often held outdoors during the 1918–1919 influenza pandemic, as shown here in San Francisco. (Photograph from the California Historical Society, FN-30852)
Unlike the 2007 CDC guidelines, in 1921 the OIHP recommended use of “special preventive measures” such as community-wide face mask use, largely on the grounds that they had been deemed effective in hospital use, and perhaps also because many cities had concluded (without compelling data) that their use inhibited influenza spread. Despite these recommendations, however, the OIHP echoed prevailing scientific opinion of the time10 in its pessimism about the ability of community mitigation strategies to prevent or significantly inhibit pandemic progression. Despite a caveat that “taken together,” preventive measures might diminish epidemic spread somewhat, the report concluded that “preventive measures against influenza did not seem to exert much influence on the progression of the pandemic.”
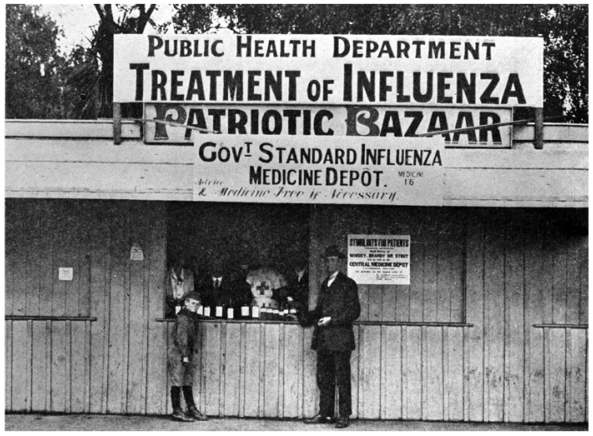
In addition to the OIHP report, many other professional societies, governments, and official entities made influenza prevention recommendations during or after the pandemic, including the American Public Health Association and various state health departments.11,12 Although they are too numerous to summarize here, these recommendations were generally similar to those of the OIHP, but varied in their comprehensiveness. They tended to rely upon standard public health measures considered effective in response to epidemics of other diseases (e.g., sanitation, hygiene, and separating the ill from the well) that had stood the test of time, and which are still considered useful today. We chose to discuss only the OIHP report in this comparison because it represents the only such document of which we are aware that appears to have reflected international consensus on influenza prevention. In retrospect, it is not clear that nearly a century of subsequent research has diminished the perceived relative importance of these measures in influenza control (Figures 2 and 3).
Figure 3. Health department clinic in Christchurch, New Zealand, 1918–1919.
Health department clinics such as this one (the medicine depot in Cathedral Square) in Christchurch, New Zealand, dispensed medicines, disinfectants, and, sometimes, crude antibacterial vaccines during the 1918–1919 influenza pandemic. The cause of influenza was unknown at the time. Most believed it was a bacterial disease caused either by Pfeiffer's bacillus (Haemophilus influenzae), or by several other bacteria. Those who believed it was caused by an unknown “filter-passing agent”—i.e., a virus—nevertheless agreed that most influenza deaths were associated with secondary bacterial pneumonias against which antibacterial vaccines might be effective. (Photograph from the Christchurch City Libraries)
CONCLUSIONS
Comparison of 1921 and 2007 influenza community prevention guidelines suggests that optional prevention and mitigation strategies for pandemic influenza are perceived as being as important today as they were nearly 90 years ago. Much has been accomplished in the interim, especially with regard to understanding the molecular virology of influenza viruses and the availability of vaccines and influenza antiviral medications. However, vaccine availability will probably be limited in the early phases of a pandemic, and antiviral medications are of unproven ability to inhibit community spread. Because influenza pandemics cannot be predicted as to timing and antigenic type,13 community mitigation strategies will remain a key component of influenza pandemic responses insofar as they attempt to counter known mechanisms of transmission and can be broadly applied by ordinary citizens without specialized medical knowledge.
Today, nearly a century after the historic 1918 influenza pandemic, its mysteries remain largely unexplained.14 Much work remains to be done, by scientists as well as historians and other scholars, with regard to many unanswered questions. In facing an inevitable future influenza pandemic, a robust and broad research effort should include a careful examination of existing scientific and historical scholarship—spanning 90 years and in numerous languages—to look for evidence from previous eras that might be helpful in moderating pandemics today.4,15–17 Even though questions about the efficacy of some of the measures remain, the fact that the 2007 CDC community mitigation guidelines6 closely echo those of an earlier era5 underscores the timeless and universal importance of public health.
REFERENCES
- 1.World Health Organization. Cumulative number of confirmed human cases of avian influenza A/(H5N1) reported to WHO. 2008. Sep 10, [cited 2008 Oct 15]. Available from: URL: http://www.who.int/csr/disease/avian_influenza/country/cases_table_2008_09_10/en/index.html.
- 2.Shope RE. The incidence of neutralizing antibodies for swine influenza virus in the sera of human beings of different ages. J Exp Med. 1936;63:669–84. doi: 10.1084/jem.63.5.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barry JM. The great influenza: the epic story of the deadliest plague in history. New York: Viking Press; 2004. [Google Scholar]
- 4.Markel H, Lipman HB, Navarro JA, Sloan A, Michalsen JR, Stern AM, et al. Nonpharmaceutical interventions implemented by US cities during the 1918–1919 influenza pandemic. JAMA. 2007;298:644–54. doi: 10.1001/jama.298.6.644. [published erratum appears in JAMA 2007;298:2264] [DOI] [PubMed] [Google Scholar]
- 5.Pottevin H. Rapport sur la pandémie grippale de 1918–1919 présenté au comité permanent de l'Office internationale d'hygiène publique. Bulletin de l'Office internationale d'hygiène publique. 1921;13:125–81. [Google Scholar]
- 6.Centers for Disease Control and Prevention (US) Interim pre-pandemic planning guidance: community strategy for pandemic influenza mitigation in the United States—early, targeted, layered use of nonpharmaceutical interventions. 2007. Feb, [cited 2008 Oct. 15]. Available from: URL: http://www.pandemicflu.gov/plan/community/community_mitigation.pdf.
- 7.Opie EL, Blake FG, Small JC, Rivers TM. Epidemic respiratory disease: the pneumonias and other infections of the respiratory tract accompanying influenza and measles. St. Louis: C.V. Mosby Co.; 1921. [Google Scholar]
- 8.Anonymous. Quarantine and isolation in influenza [editorial] J Am Med Assoc. 1918;71:1220. [Google Scholar]
- 9.Morens DM, Taubenberger JK, Fauci AS. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis. 2008;198:962–70. doi: 10.1086/591708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kellogg WH. A consideration of the methods used in the control of influenza. Cal State J Med. 1919;17:228–31. [PMC free article] [PubMed] [Google Scholar]
- 11.American Public Health Association. Influenza: report of a special committee of the American Public Health Association. J Am Med Assoc. 1918;71:2068–73. [Google Scholar]
- 12.Feezer LW. A comparative study of state regulations for the control of influenza. Public Health Rep. 1920;35:2155–61. [Google Scholar]
- 13.Taubenberger JK, Morens DM, Fauci AS. The next influenza pandemic: can it be predicted? JAMA. 2007;297:2025–7. doi: 10.1001/jama.297.18.2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morens DM, Fauci AS. The 1918 influenza pandemic: insights for the 21st century. J Infect Dis. 2007;195:1018–28. doi: 10.1086/511989. [DOI] [PubMed] [Google Scholar]
- 15.Markel H, Stern AM, Navarro JA, Michalsen JR, Monto AS, DiGiovanni C. Nonpharmaceutical influenza mitigation strategies, US communities, 1918–1920 pandemic. Emerg Infect Dis. 2006;12:1961–4. doi: 10.3201/eid1212.060506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bootsma MC, Ferguson NM. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proc Natl Acad Sci USA. 2007;104:7588–93. doi: 10.1073/pnas.0611071104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hatchett RJ, Mecher CE, Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc Natl Acad Sci USA. 2007;104:7582–7. doi: 10.1073/pnas.0610941104. [DOI] [PMC free article] [PubMed] [Google Scholar]