SYNOPSIS
Objective
We identified maternal, provider, and community predictors among infants for late initiation of immunizations.
Methods
We performed a retrospective cohort study of infants born between January 1, 2002, and December 31, 2004, in Philadelphia, Pennsylvania. Primary outcomes were age in days at first office-based immunization and status as a late starter (i.e., initiating office-based immunizations after 90 days of age). Candidate predictors included sociodemographic and prenatal characteristics, immunization provider practice type and size, and neighborhood factors. We performed hierarchical logistic regression and Cox regression models to identify independent predictors for being a late starter and prolonged time to first immunization.
Results
Of the 65,519 infants from this birth cohort in Philadelphia's immunization registry, 54,429 (88.1%) were included in analysis and 12.6% of these were late starters. Infants whose mothers were younger, received less than five prenatal visits, had less than a high school education, had more than two children, and who smoked cigarettes prenatally were significantly more likely to be late starters. Receiving care at hospital/university-based or public health clinics was also significantly associated with likelihood of being a late starter. Neither distance between infant's residence and practice nor neighborhood socioeconomic indicators was independently associated with the outcomes. Common risk factor profiles based on practice type and four maternal characteristics were found to reliably identify infant risk.
Conclusions
Maternal receipt of fewer prenatal care visits, younger maternal age, higher birth order, and receiving care at public health clinics were the strongest predictors of being a late starter and time to first immunization. Risk factor profiles based on information already collected at birth can be used to identify higher-risk infants. Early intervention and potentially partnering with prenatal care providers may be key strategies for preventing underimmunization.
Despite unprecedented high levels of vaccination coverage rates for children, delays in receipt of vaccines according to the recommended schedule persist, especially in early childhood.1–3 According to 2003 National Immunization Survey (NIS) data, 52% of infants were delayed for at least one immunization by more than six months. Even among those up-to-date by age 2, 23% were under-vaccinated for at least six months.2 This suggests that children who achieve full coverage by age 2 may spend a significant amount of time with incomplete protection and are at risk for developing a vaccine-preventable illness. Immunization delay is also a known predictor of subsequent immunization status. Among children with immunization delay, the risk for continued underimmunization is especially high for late starters (i.e., infants who fail to receive initial two-month office-based immunizations by 3 months of age).4–11
The Philadelphia Department of Public Health Immunization Program (PDPHIP) has identified late starters as an important group to target for immunization outreach initiatives. PDPHIP has estimated that approximately one-quarter of infants do not receive their first set of immunizations by age 3 months.4 Among one Philadelphia academic practice network, late starters were 4.5 times more likely to be not up-to-date at age 2, even after adjusting for demographic and socioeconomic characteristics.5 Late initiation of immunizations is associated with decreased adherence to recommended dose intervals, and infants spend more time underimmunized as they catch up to the recommended schedule.2 Catch-up doses of immunizations can be more costly for immunization programs, especially if the doses are given at inappropriate intervals.1,2 Even more importantly, late initiation of immunizations may be a marker of inadequate receipt of preventative health care in general.7,12,13
An extensive body of literature identifies risk factors for underimmunization, particularly for children who are not up-to-date by ages 19 to 35 months.1,2,7–11,14–25 These studies show higher rates of underimmunization among low-income urban populations and indicate that both individual and provider characteristics play a role in immunization status. Fewer studies focus specifically on risk factors for being a late starter or time to first immunization, and most of these studies are among infants from underserved areas.6,7,10,11,20,21 Late initiation of immunizations has not been systematically evaluated across a larger, more diverse population. In addition, previous studies have also not considered neighborhood characteristics or the potential role of perinatal practices on initiation of immunizations.
This study was designed to describe the geographic distribution and sociodemographic characteristics of late starters in a large metropolitan area, to identify predictors for becoming a late starter, and to identify factors associated with time to first outpatient immunization at the community, provider, and individual level. We assessed neighborhood socioeconomic indicators, immunization provider practice type, birth hospital characteristics, distance from residence to immunization provider, and infant and maternal characteristics in a diverse northeastern urban area to determine risk profiles for late initiation of immunization that will inform subsequent immunization outreach activities and improve age-appropriate vaccination rates.
METHODS
Study design and study subjects
The objectives of this retrospective cohort study were to identify the community, provider, and individual-level factors that best predict an infant's probability of being a late starter and to determine which of these factors are associated with time to first immunization. To be included in the study, an infant must have been born between January 1, 2002, and December 31, 2004, have a valid Philadelphia county residential address, have a state of Pennsylvania birth record, and have at least one immunization record in PDPHIP's immunization registry (KIDS). Each child born in Philadelphia has a record in the KIDS registry and specific demographic and immunization information is populated by provider electronic or billing data, through manual report from practices, or by PDPH staff from data obtained through outreach to families and practice audits. Reporting to the registry is mandated of all Philadelphia medical providers. A PDPHIP study found that 92% of children have an immunization record in KIDS26 and since 2003, PDPHIP regularly performs audits of medical records to increase data accuracy.
Infants who received one or more outpatient immunizations with diphtheria, tetanus, acellular pertussis (DTaP), inactivated polio vaccine (IPV), Haemophilus influenzae type b (Hib), or pneumococcal vaccine (PCV) between 42 and 90 days of age were classified as on time, and infants who received these antigens for the first time after 90 days of age were classified as late starters. As outpatient immunizations, with the exception of hepatitis B vaccine (HBV), are recommended to begin no earlier than at 6 weeks of age, immunization with DTaP, IPV, Hib, or PCV given before age 42 days were considered invalid and the subsequent vaccine date was used to classify the infant. We did not consider HBV when classifying infants, as birth hospital audits performed in 2005 demonstrated that 98% of infants received HBV1 at birth in Philadelphia (Personal communication, Barbara Watson, MD, Immunization Program at PDPHIP, September 2007). Infants were not required to receive all recommended vaccines at the time of their first visit to be identified as on time. Our results exclude infants with age at first immunization greater than 365 days (1 year of age). These infants may have been born or received immunizations at a practice outside of the city and would therefore be incorrectly identified as late starters.
The candidate maternal and infant independent variables were infant's race/ethnicity, maternal age, maternal education level, number of prenatal visits, birth order of infant, prenatal use of cigarettes, and Women, Infants, and Children (WIC) status (for the 2004 birth cohort) obtained from the birth record database. Infant race/ethnicity data were taken from KIDS, if available. If race/ethnicity data were missing, we used self-reported maternal and paternal race from the birth record to determine the infant's race. Any infant whose mother's and father's reported races were not the same was classified as other/unknown.
Provider independent variables were immunization provider practice type (private pediatric, public health clinic, family practice, hospital/university facility, federally qualified health center [FQHC], or other), practice size, and infant's birth hospital. The provider assignment was based on the practice where infants received their first outpatient immunization after age 42 days. Practice and birth hospital data were obtained from KIDS and the Vaccines for Children (VFC) program database. The latter database includes information on all practices that participate in the VFC program (i.e., all but one pediatric practice in Philadelphia). Lastly, candidate community predictor variables were median income of census tract, proportion of females with more than a high school education, and distance between residence and provider. We used ArcView 9.127 to assign residential census tract and calculate distance. Socioeconomic indicators for each census tract were based on 2000 U.S. Census data.28 We mapped the location of late starters to determine whether or not there was geographic clustering of cases by neighborhood and to calculate whether or not distance from immunization provider was a factor.
The protocol was approved by the Institutional Review Boards at the University of Pennsylvania School of Medicine and PDPH.
Statistical analysis
For all analyses, time to first immunization and immunization incidence were evaluated first among all infants and then among the late starters. We utilized Chi-square analyses and Fisher's exact test to compare proportions of late starters among risk factor groups. We utilized Kruskal-Wallis analyses to compare median age in days at first immunization. We constructed Kaplan-Meier curves for each exposure to identify possible outliers, to identify which variables had a linear relationship with the outcome, and to identify whether proportional hazards assumptions were reasonable.
For multivariable analyses, we used logistic regression to evaluate associations with late-starter status and Cox Proportional Hazards (PH) models to evaluate associations with time to immunization among late starters.16 Best-subsets' algorithms were used to identify a set of independent variables that were strongly associated with the outcomes. Plausible two-way interactions were evaluated one at a time for statistical significance: maternal education and prenatal care, maternal education and race, age and prenatal care, birth order and prenatal care, cigarette use and prenatal care, and maternal education and census tract median income. We retained immunization provider method of entry to the KIDS registry as a potential confounder because mode of entry has been found to be associated with completeness of immunization data reporting and up-to-date rates in Philadelphia.26
To adjust standard errors for clustering within practice, birth hospital, and residential census tract, we evaluated the effect of a hierarchical generalized estimating equation for logistic regression and a sandwich covariance estimator for Cox PH models.29,30 If standard errors did not change by more than 10% in the general estimating equation model, then clustering effects were ignored in the final model. An alpha level of 0.01 was used for all analyses. Subjects with missing values for any of the predictor variables included in the model, with the exception of infant race/ethnicity, were excluded from analysis. All remaining missing values for infant race/ethnicity (approximately 10% of the study sample) were recoded as other/unknown.
We present both odds ratios for status as a late starter and hazard ratios for time to first immunization among the late starters. Hazard ratios <1.0 represent a lower incidence of first immunization (i.e., fewer children receiving their first immunization and/or longer time until first immunization). We also present risk profiles, or combinations of risk factors, for the probability of becoming a late starter. We selected combinations representing at least 2% of our sample. These probabilities were determined from the parameter estimates derived from the logistic multivariable model.
RESULTS
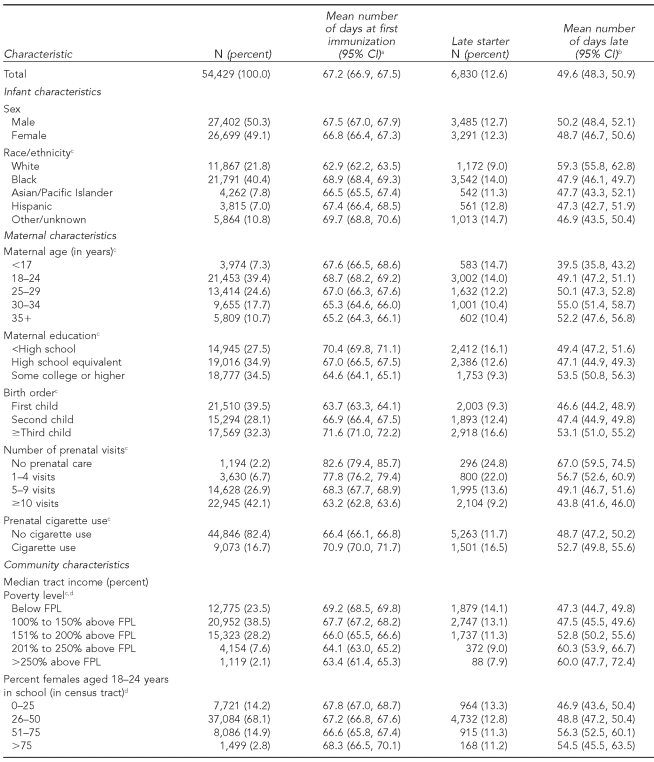
Of the 65,519 infants with a KIDS record, 62,138 (94.8%) had a Philadelphia address and of these, 55,801 (89.8%) had a matching birth record. One thousand forty-five (1.7%) infants were excluded for their first documented immunization at age >356 days, and 327 (0.6%) infants were excluded if they received DTaP, Hib, IPV, or PCV at <42 days of age, leaving 54,429 (83.1% of the total sample) who met full criteria for analysis. Of these infants, 50.6% were male, 46.5% were identified as black, 23.5% lived in census tracts with median income below the federal poverty level (FPL), 28.3% were born to mothers with less than a high school education, and 11.4% were born to mothers who received no or fewer than five prenatal care visits (Table 1). The majority of infants (72.3%) were followed in private pediatric or hospital/university-based clinics. Thirteen percent of infants in the study population were late starters.
Table 1. Infant and maternal characteristics, status as a late starter, and age in days at first immunization.
aAmong all infants
bAmong late starters
cp<0.01, based on Chi-square analysis for proportion of late starters and Kruskal-Wallis for number of days late
dFor a family of four as per U.S. Census data
CI = confidence interval
FPL = federal poverty level
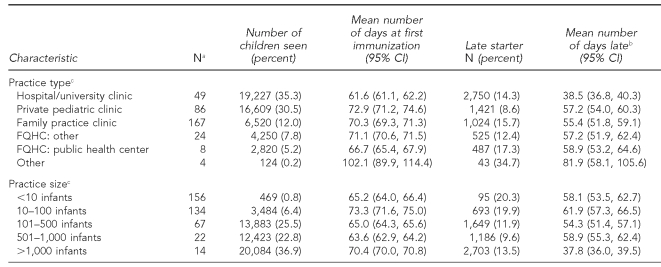
There was significant variation in the likelihood of being a late starter and mean age at first immunization among late starters across all candidate predictor variables except infant's gender and birth hospital size (Tables 1 and 2). The highest proportions of late starters were seen among infants with younger mothers, mothers who had less than a high school education, mothers with no prenatal care visits, and among infants whose birth order was third or higher. Also, infants receiving care at public health, family practice, and university-based clinics, and infants residing in census tracts with median income at or below 150% FPL (for a family of four) and tracts with lower proportions of 18- to 24-year-old females in school, had higher proportions of late starters. When evaluating late starters, longer time to first immunization was seen among white infants, infants whose mothers had at least some college education, whose mothers were older, and among infants who resided within census tracts with higher median incomes and higher proportions of 18- to 24-year-old females in school. Fewer prenatal care visits and infant birth order of third or higher were also associated with longer time to first immunization.
Table 2. Initial provider characteristics, status as late starter, and age in days at first immunization.
aNumber of practices
bAmong late starters
cp<0.01, based on Chi-square analysis for proportion of late starters and Kruskal-Wallis for number of days late
CI = confidence interval
FPL = federal poverty level
FQHC = federally qualified health center
Figure 1 illustrates the location of primary care practices and the prevalence of late starters by census tract. Overall, the map indicates that immunization providers are distributed throughout the city of Philadelphia and many areas with a higher prevalence of late starters contain at least one immunization provider. Direct measurement of distance between infant residence and immunization provider showed no significant association with likelihood of being a late starter (mean distance of 2.72 miles for the total population vs. 2.24 miles for late starters, p=0.15).
Figure 1. Prevalence of late starters for immunization by census tract, Philadelphia County, 2002–2004.
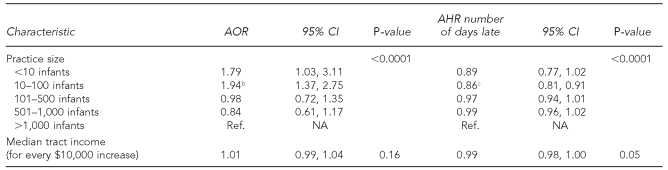
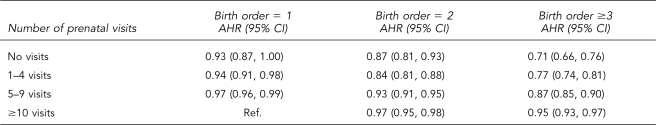
For the adjusted analyses (Table 3), birth hospital size, census tract female educational attainment, and distance between residence and provider were not included in the final model. The highest likelihood of being a late starter and longest time to first immunization occurred among mothers receiving no or less than five prenatal care visits, younger mothers, and among infants whose birth order was third or higher. Of the interactions we assessed, only prenatal care and birth order showed a significant interaction for the Cox PH regression and was included in the final Cox model (Table 4). The effect of fewer prenatal care visits on immunization delay was greatest for late starters whose mothers had three or more children. Late starters whose birth order was third or higher and whose mothers had received no prenatal care—the highest-risk combination—had the lowest incidence of immunization (adjusted hazard ratio [AHR] = 0.71 [0.64, 0.77], referent = first-born infant and ≥10 prenatal care visits). Mothers with less than a high school education were more likely to have an infant who was a late starter, but maternal education was not significantly associated with time to first immunization. Practice type was also independently associated with the likelihood of being a late starter: public health and university/hospital-based clinics were more likely to have late starters compared with private pediatricians' offices.
Table 3. Logistic and Cox regression analyses of predictors for likelihood of being a late starter and time to first immunizationa.
aAmong late starters
bp<0.001 compared to reference group
cp<0.0001 compared to reference group
dp<0.01 compared to reference group
eBecause of the interaction between prenatal care and birth order, adjusted hazard ratios were unable to be calculated for these two variables separately.
AOR = adjusted odds ratio
CI = confidence interval
AHR = adjusted hazard ratio
Ref. = reference group
NA = not applicable
FQHC = federally qualified health center
Table 4. Interaction between prenatal care and birth order: incidence of late starters for immunization between infants with and without prenatal care across birth order.
AHR = adjusted hazard ratio
CI = confidence interval
Ref. = reference group
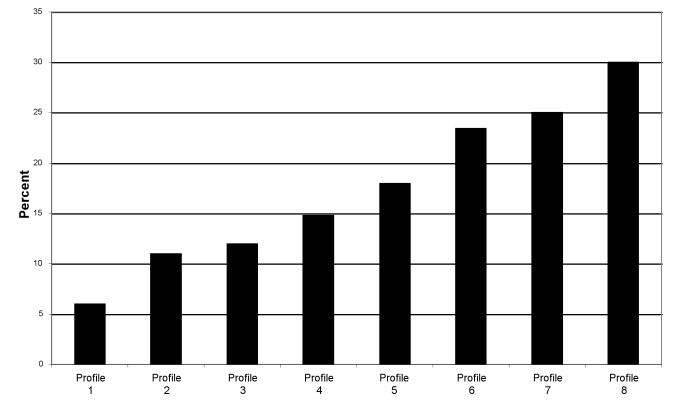
We also determined combinations of risk factors associated with becoming a late starter (Figure 2). According to these results, the lowest risk (5%) was among infants who were first or second born and whose mothers had at least five prenatal care visits. The highest risk (30%) was among infants who received care in a public health clinic and whose mothers received less than five prenatal care visits, had no more than a high school education, were younger than age 24, and already had at least one child.
Figure 2. Probability of becoming a late startera for immunizations for selected risk factor profiles.
aLate starters are infants who fail to initiate two-month office-based immunizations by 3 months of age.
Profile 1: Infants whose mothers had ≥5 prenatal care visits and were first or second in birth order
Profile 2: Infants whose mothers had 0–4 prenatal care visits and were ≥3 in birth order
Profile 3: Infants whose mothers had 0–4 prenatal care visits, were ≥2 in birth order, and received care at a hospital or university-based clinic
Profile 4: Infants whose mothers had 0–4 prenatal care visits, were ≥2 in birth order, and received care at a public health clinic
Profile 5: Infants whose mothers had 0–4 prenatal care visits, were ≥2 in birth order, received care at a hospital or university-based clinic, and whose maternal age was <24 years
Profile 6: Infants whose mothers had 0–4 prenatal care visits, were ≥2 in birth order, received care at a public health clinic, and whose maternal age was <24 years
Profile 7: Infants whose mothers had 0–4 prenatal care visits, were ≥2 in birth order, received care at a hospital or university-based clinic, whose maternal age was <24 years, and maternal education was ≤high school
Profile 8: Infants whose mothers had 0–4 prenatal care visits, were ≥2 in birth order, received care at a public health clinic, whose maternal age was <24 years, and maternal education was ≤high school
As a subset analysis of the 2004 birth cohort, we also assessed WIC status as a candidate risk factor for our outcomes (data not shown). Of the 17,821 infants in this cohort, 62.4% of their mothers received WIC. Non-WIC infants were significantly more likely than WIC infants to be late starters in both unadjusted and adjusted analyses (adjusted odds ratio [AOR] = 1.26 [1.08, 1.46]) and had a longer time to first immunization (AHR=0.92 [0.88, 0.96]).
DISCUSSION
This study is the largest to date to investigate multiple levels of potential risk factors for late initiation of immunization and time to first immunization. Almost 13% of the 2002–2004 Philadelphia birth cohort were late starters. This is a smaller percentage than previously estimated by the PDPHIP4 but represents a large number of infants likely to be at increased risk for developing vaccine-preventable infections. We found that maternal receipt of fewer prenatal care visits, younger maternal age, infants having birth order of third or higher, and receiving care at public health clinics were the strongest predictors for likelihood of being a late starter and of time to first immunization, suggesting that early intervention may be a key strategy to prevent underimmunization.
The association between late initiation of immunizations and maternal prenatal care is consistent with previous studies. Maternal prenatal care could be a marker of self-efficacy or health literacy and has been strongly associated with both infant immunization status and the likelihood of receiving well-child visits.7,8,10,12,20,22,24 We found that lower maternal education was a predictor for likelihood of being a late starter, but did not have a significant effect on actual time to first immunization among late starters. This suggests that the effect of maternal education is complex. Lower educational attainment may have a strong association with health-care-seeking behavior and health-care access. Both of these factors are likely to be associated with being a late starter. Other studies show that less-educated parents are less likely to support compulsory vaccination, have higher levels of concern regarding vaccine safety, or perceive that they have enough information regarding vaccines.31–35 On the other hand, research suggests that mothers with hesitancy toward vaccines tend to have more knowledge regarding vaccines and seek out information from a variety of sources to make their decisions.36 Our finding that maternal education was weakly associated with time to first immunization may reflect a subset of infants for whom parents with more vaccine knowledge have made a choice to delay immunizations. This combination of findings suggests that quantifying the degree to which these attitudes affect actual vaccine receipt warrants further investigation. Maternal education may not provide the best way for practitioners and immunization programs to assess the effect of knowledge on attitudes toward vaccination.
Our finding that birth order was strongly associated with late initiation of immunizations is also consistent with results from previous studies.6–8,10,24,25 However, the association that we found between younger maternal age and late initiation of immunization has not been consistent in previous studies.7,8,12,22,23,25 A wide body of literature describes an association between adolescent pregnancy and adverse birth outcomes, even when adjusting for socioeconomic factors.37 Previous research also suggests that young maternal age can result in negative health outcomes for their children.38,39 These studies indicate that younger mothers are more likely to come from economically disadvantaged backgrounds, have fewer social supports, engage in health-risk behaviors, and receive less prenatal care. However, young maternal age remained independently associated in our study even after adjusting for some of these factors.
While our findings suggest that maternal characteristics are the most important predictors for late initiation of immunizations, community characteristics are often utilized to identify areas with at-risk populations or to target outreach activities. Area-level socioeconomic measures have been found to correlate fairly well with individual socioeconomic markers and are used increasingly both as proxy measures and to measure the effect of neighborhood context on health outcomes.40,41 Median tract income was not significantly associated with our outcomes in adjusted analyses. There may be collinearity between median household income and some of our other predictors. Also, tract income may not be a good proxy measure for individual household income in this population.
We found that proximity to an immunization provider was not associated with being a late starter. However, there was significant variation in prevalence of late starters across census tracts, and we found a high prevalence of late starters in some census tracts with higher median incomes. Though these neighborhoods may be considered lower risk due to higher density of resources, our findings suggest that there may be pockets of high-risk families in these neighborhoods who have difficulty accessing available services or who are not being reached by outreach initiatives. Increasing amounts of research assess the relationship between individual and area-level socioeconomic indicators on health outcomes.40–42 This phenomenon could be applicable to outcomes such as immunization status and represents an area of future research.
The last category of risk factors that we assessed was provider characteristics. Our results showed significant variation in time to first immunization and prevalence of late starters across individual practices. Our findings also suggest that smaller practices and public health and hospital/university-based clinics were associated with increased likelihood of being a late starter. An association with public clinics has been noted in other studies investigating risk factors for underimmunization and receipt of well-child services.1,2,12,16,43 These clinics are more likely to serve uninsured and publicly insured children. Some of these families may be at higher risk for irregular access to care, and being uninsured has been shown to be associated with underimmunization.44,45 Families who seek care at a public health clinic may also be less likely to use the clinic as a medical home and previous work has indicated that the identification of a medical home increases the likelihood of being up-to-date with immunizations.45,46 We were not able to determine from our data sources whether or not infants within our cohort had a medical home; this would be a valuable area for future study.
We assessed birth hospital size based upon the hypothesis that larger hospitals are more likely to have staff and infrastructure to implement perinatal guidelines and give anticipatory guidance regarding well-infant care to mothers before they leave the hospital. Previous studies suggest that birth hospitals' administration of the hepatitis B birth dose can increase the likelihood of being up-to-date for subsequent immunizations.47–49 Birth hospital size was not a significant factor in our results but may not have been a good proxy measure for birth hospital practices. Also, during the study period, Philadelphia had only eight dedicated birth hospitals, and we therefore had limited statistical power to identify subtle patterns among hospitals.
Limitations
Our work did have limitations. Overall, there was likely residual confounding that was not adjusted for in our model. Therefore, we cannot definitively establish cause and effect between the predictors that we identified and our outcomes. Control of confounding and determination of causality are important if an intervention is to be directed at changing the risk factor itself. If, on the other hand, these results will be used to predict late-starter status, then demonstrating causality is not required. Another consideration is the use of an immunization registry. Registries have resulted in significant improvements in immunization coverage, but they have also been difficult to fully implement.50,51 The KIDS registry represents approximately 95% of children in Philadelphia, but does require reporting from providers, which is subject to potential inaccuracy depending upon the method of reporting.26 However, reporting method was included in our models as a confounder and did not significantly affect our results.
Interpretation of our findings was also subject to several caveats. First, though the study population included infants from a wide range of socioeconomic backgrounds and practice types, the results may not be applicable to suburban or rural settings. Second, we did not take into account the potential effect of medical diagnoses, such as prematurity, that influence the timeliness and recommended schedule of immunizations, because this information was not reliably available in the KIDS registry or birth record database. However, given the large sample size, we anticipated that there was a small proportion unable to receive vaccines and excluded infants who had not received any vaccines by 1 year of age from the analysis. Lastly, there was a small amount of missing data (approximately 10%) for infant racial/ethnicity, even after utilizing birth record data. We did not impute missing racial/ethnicity data and counted these infants as other/unknown race. However, because nearly 7,000 infants were included in the other/unknown category, it is difficult to interpret the variability in immunization status that we did find among race/ethnicity.
CONCLUSIONS
Despite these limitations, our findings provide a rich assessment of risk factors for late initiation of immunizations, taking into account the important individual, provider, and community characteristics that work together to affect the receipt of vaccinations. Although our findings support the work of previous studies, the strength of association with maternal risk factors emphasizes the importance of targeting at-risk mothers early, even prenatally. This early outreach has not been a focus of many immunization programs and can potentially be applied in similar settings. In Philadelphia, efforts are underway to use these results to inform the immunization outreach activities conducted by the PDPHIP. Specifically, partnerships with maternal and child health services and obstetric practices at three Philadelphia academic medical centers have been initiated to begin vaccine education and promote prenatal pediatric visits as an integral part of prenatal care. Previous work shows that prenatal pediatric visits, which have been previously recommended by the American Academy of Pediatrics, can positively impact some health-care outcomes.52
The PDPHIP will also use registry data to begin outreach to infants delayed at 3 months of age. Pediatric practices can outreach within their patient populations and implement more targeted reminder/recall initiatives or establish new strategies to partner with prenatal health-care providers to ensure that newborns receive timely preventive care. Birth hospitals can use birth certificate information to identify which infants match the risk profiles for becoming a late starter to ensure that timely follow-up with a pediatric provider is carefully planned. Investing in early prevention can ensure that children are up-to-date and fully protected throughout their infancy and childhood.
Footnotes
All data extraction, management, and analysis took place at the Philadelphia Department of Public Health (PDPH) Division of Disease Control. Statistical support was provided by the PDPH Epidemiology Unit, Division of Disease Control, and the University of Pennsylvania School of Medicine Center for Clinical Epidemiology and Biostatistics statistical consulting services.
Dr. Feemster was supported by the Robert Wood Johnson Clinical Scholars Program at the University of Pennsylvania School of Medicine
REFERENCES
- 1.Luman ET, Barker LE, McCauley MM, Drews-Botsch C. Timeliness of childhood immunizations: a state-specific analysis. Am J Public Health. 2005;95:1367–74. doi: 10.2105/AJPH.2004.046284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luman ET, Barker LE, Shaw KM, McCauley MM, Buehler JW, Pickering LK. Timeliness of childhood vaccinations in the United States: days undervaccinated and number of vaccines delayed. JAMA. 2005;293:1204–11. doi: 10.1001/jama.293.10.1204. [DOI] [PubMed] [Google Scholar]
- 3.Dombkowski KJ, Lantz PM, Freed GL. The need for surveillance of delay in age-appropriate immunization. Am J Prev Med. 2002;23:36–42. doi: 10.1016/s0749-3797(02)00442-7. [DOI] [PubMed] [Google Scholar]
- 4.Chilkatowsky AP. Philadelphia Immunization Coalition Meeting. Philadelphia: Philadelphia Department of Public Health Division of Disease Control; 2005. Immunization coverage levels among Philadelphia children 19–35 months of age. [Google Scholar]
- 5.Fiks AG, Alessandrini EA, Luberti AA, Ostapenko S, Zhang X, Silber JH. Identifying factors predicting immunization delay for children followed in an urban primary care network using an electronic health record. Pediatrics. 2006;118:e1680–6. doi: 10.1542/peds.2005-2349. [DOI] [PubMed] [Google Scholar]
- 6.Bardenheier BH, Yusuf HR, Rosenthal J, Santoli JM, Shefer AM, Rickert DL, et al. Factors associated with underimmunization at 3 months of age in four medically underserved areas. Public Health Rep. 2004;119:479–85. doi: 10.1016/j.phr.2004.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brenner RA, Simons-Morton BG, Bhaskar B, Das A, Clemens JD. Prevalence and predictors of immunization among inner-city infants: a birth cohort study. Pediatrics. 2001;108:661–70. doi: 10.1542/peds.108.3.661. [DOI] [PubMed] [Google Scholar]
- 8.Bates AS, Wolinsky FD. Personal, financial and structural barriers to immunization in socioeconomically disadvantaged urban children. Pediatrics. 1998;101(4 Pt 1):591–6. doi: 10.1542/peds.101.4.591. [DOI] [PubMed] [Google Scholar]
- 9.Williams IT, Milton JD, Farrell JB, Graham NM. Interaction of socioeconomic status and provider practices as predictors of immunization coverage in Virginia children. Pediatrics. 1995;96(3 Pt 1):439–46. [PubMed] [Google Scholar]
- 10.Wood D, Donald-Sherbourne C, Halfon N, Tucker MB, Ortiz V, Hamlin JS, et al. Factors related to immunization status among inner-city Latino and African-American preschoolers. Pediatrics. 1995;96(2 Pt 1):295–301. [PubMed] [Google Scholar]
- 11.Guyer B, Hughart N, Holt E, Ross A, Stanton B, Keane V, et al. Immunization coverage and its relationship to preventive health care visits among inner-city children in Baltimore. Pediatrics. 1994;94:53–8. [PubMed] [Google Scholar]
- 12.Freed GL, Clark SJ, Pathman DE, Schectman R. Influences on the receipt of well-child visits in the first two years of life. Pediatrics. 1999;103:864–9. [PubMed] [Google Scholar]
- 13.Hambidge SJ, Davidson AJ, Phibbs SL, Chandramouli V, Zerbe G, LeBaron CW, et al. Strategies to improve immunization rates and well-child care in a disadvantaged population: a cluster randomized control trial. Arch Pediatr Adolesc Med. 2004;158:162–9. doi: 10.1001/archpedi.158.2.162. [DOI] [PubMed] [Google Scholar]
- 14.Meyerhoff AS, Jacobs RJ. Do too many shots lead to missed vaccination opportunities? Does it matter? Prev Med. 2005;41:540–4. doi: 10.1016/j.ypmed.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Daniels D, Jiles RB, Klevens RM, Herrera GA. Undervaccinated African-American preschoolers: a case of missed opportunities. Am J Prev Med. 2001;20(4 Suppl):S61–8. doi: 10.1016/s0749-3797(01)00278-1. [DOI] [PubMed] [Google Scholar]
- 16.Dayan GH, Shaw KM, Baughman AL, Orellana LC, Forlenza R, Ellis A, et al. Assessment of delay in age-appropriate vaccination using survival analysis. Am J Epidemiol. 2006;163:561–70. doi: 10.1093/aje/kwj074. [DOI] [PubMed] [Google Scholar]
- 17.Hambidge SJ, Phibbs SL, Davison AJ, LeBaron CW, Chandramouli V, Fairclough DL, et al. Individually significant risk factors do not provide an accurate clinical prediction rule for infant underimmunization in one disadvantaged urban area. Ambul Pediatr. 2006;6:165–72. doi: 10.1016/j.ambp.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Taylor JA, Darden PM, Slora E, Hasemeier CM, Asmussen L, Wasserman R. The influence of provider behavior, parental characteristics and a public policy initiative on the immunization status of children followed by private pediatricians: a study from pediatric research office settings. Pediatrics. 1997;99:209–15. [PubMed] [Google Scholar]
- 19.Steyer TE, Mainous AG, III, Geesey ME. The effect of race and residence on the receipt of childhood immunizations: 1993–2001. Vaccine. 2005;23:1464–70. doi: 10.1016/j.vaccine.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 20.Bates AS, Fitzgerald JF, Dittus RS, Wolinsky FD. Risk factors for underimmunization in poor urban infants. JAMA. 1994;272:1105–10. [PubMed] [Google Scholar]
- 21.Ross A, Kennedy AB, Holt E, Guyer B, Hou W, Hughart N. Initiating the first DTP vaccination age-appropriately: a model for understanding vaccination coverage. Pediatrics. 1998;101:970–4. doi: 10.1542/peds.101.6.970. [DOI] [PubMed] [Google Scholar]
- 22.Kogan MD, Alexander GR, Jack BW, Allen MC. The association between adequacy of prenatal care utilization and subsequent pediatric care utilization in the United States. Pediatrics. 1998;102:25–30. doi: 10.1542/peds.102.1.25. [DOI] [PubMed] [Google Scholar]
- 23.Strobino D, Keane V, Holt E, Hughart N, Guyer B. Parental attitudes do not explain underimmunization. Pediatrics. 1996;98(6 Pt 1):1076–83. [PubMed] [Google Scholar]
- 24.Wiecha J, Gann P. Does maternal prenatal care use predict infant immunization delay? Fam Med. 1994;26:172–8. [PubMed] [Google Scholar]
- 25.Luman ET, McCauley MM, Shefer A, Chu SY. Maternal characteristics associated with vaccination of young children. Pediatrics. 2003;111(5 Pt 2):1215–8. [PubMed] [Google Scholar]
- 26.Kolasa MS, Chilkatowsky AP, Clarke KR, Lutz JP. How complete are immunization registries? The Philadelphia story. Ambul Pediatr. 2006;6:21–4. doi: 10.1016/j.ambp.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 27.ESRI, Inc. ArcView, ArcMap: Version 9.1. Redlands (CA): ESRI, Inc.; 2006. [Google Scholar]
- 28.Census Bureau (US) U.S. Census 2000. [cited 2008 Aug 18]. Available from: URL: http://www.census.gov.
- 29.Austin PC, Goel V, van Walraven C. An introduction to multilevel regression models. Can J Public Health. 2001;92:150–4. doi: 10.1007/BF03404950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yau KK. Multilevel models for survival analysis with random effects. Biometrics. 2001;57:96–102. doi: 10.1111/j.0006-341x.2001.00096.x. [DOI] [PubMed] [Google Scholar]
- 31.Shui IM, Weintraub ES, Gust DA. Parents concerned about vaccine safety: differences in race/ethnicity and attitudes. Am J Prev Med. 2006;31:244–51. doi: 10.1016/j.amepre.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 32.Gust DA, Kennedy A, Shui I, Smith PJ, Nowak G, Pickering LK. Parent attitude toward immunizations and healthcare providers: the role of information. Am J Prev Med. 2005;29:105–12. doi: 10.1016/j.amepre.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 33.Gust DA, Strine TW, Maurice E, Smith P, Yusuf H, Wilkinson M, et al. Underimmunization among children: effects of vaccine safety concerns on immunization status. Pediatrics. 2004;114:e16–22. doi: 10.1542/peds.114.1.e16. [DOI] [PubMed] [Google Scholar]
- 34.Kennedy AM, Brown CJ, Gust DA. Vaccine beliefs of parents who oppose compulsury vaccination. Public Health Rep. 2005;120:252–8. doi: 10.1177/003335490512000306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mills EJ, Montori VM, Ross CP, Shea B, Wilson K, Guyatt GH. Systematically reviewing qualitative studies complements survey design: an exploratory study of barriers to paediatric immunisations. J Clin Epidemiol. 2005;58:1101–8. doi: 10.1016/j.jclinepi.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 36.Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers' decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117:1532–41. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- 37.Chen XK, Wen SW, Fleming N, Demissie K, Rhoads GG, Walker M. Teenage pregnancy and adverse birth outcomes: a large population-based retrospective cohort study. Int J Epidemiol. 2007;26:368–73. doi: 10.1093/ije/dyl284. [DOI] [PubMed] [Google Scholar]
- 38.Klein JD American Academy of Pediatrics Committee on Adolescence. Adolescent pregnancy: current trends and issues. Pediatrics. 2005;116:281–6. doi: 10.1542/peds.2005-0999. [DOI] [PubMed] [Google Scholar]
- 39.Morrow AL, Rosenthal J, Lakkis HD, Bowers JC, Butterfoss FD, Crews RC, et al. A population-based study of access to immunization among urban Virginia children served by public, private, and military health care systems. Pediatrics. 1998;101:e5. doi: 10.1542/peds.101.2.e5. [DOI] [PubMed] [Google Scholar]
- 40.Diez-Roux AV, Kiefe CI, Jacobs DR, Jr, Haan M, Jackson SA, Nieto FJ, et al. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Ann Epidemiol. 2001;11:395–405. doi: 10.1016/s1047-2797(01)00221-6. [DOI] [PubMed] [Google Scholar]
- 41.Subramanian SV, Chen JT, Rehkopf DH, Waterman PD, Krieger N. Comparing individual- and area-based socioeconomic measures for the surveillance of health disparities: a multilevel analysis of Massachusetts births, 1989–1991. Am J Epidemiol. 2006;164:823–34. doi: 10.1093/aje/kwj313. [DOI] [PubMed] [Google Scholar]
- 42.Winkleby M, Cubbin C, Ahn D. Low individual socioeconomic status, neighborhood socioeconomic status, and adult mortality. Am J Public Health. 2006;96:1–9. doi: 10.2105/AJPH.2004.060970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Santoli JM, Barker LE, Lyons BH, Gandhi NB, Phillips C, Rodewald LE. Health department clinics as pediatric immunization providers: a national survey. Am J Prev Med. 2001;20:266–71. doi: 10.1016/s0749-3797(01)00299-9. [DOI] [PubMed] [Google Scholar]
- 44.Smith PJ, Stevenson J, Chu SY. Associations between childhood vaccination coverage, insurance type, and breaks in health insurance coverage. Pediatrics. 2006;117:1972–8. doi: 10.1542/peds.2005-2414. [DOI] [PubMed] [Google Scholar]
- 45.Allred NJ, Wooten KG, Kong Y. The association of health insurance and continuous primary care in the medical home on vaccination coverage for 19- to 35- month-old children. Pediatrics. 2007;119(Suppl 1):S4–11. doi: 10.1542/peds.2006-2089C. [DOI] [PubMed] [Google Scholar]
- 46.Smith PJ, Santoli JM, Chu SY, Ochoa DQ, Rodewald LE. The association between having a medical home and vaccination coverage among children eligible for the Vaccines for Children program. Pediatrics. 2005;116:130–9. doi: 10.1542/peds.2004-1058. [DOI] [PubMed] [Google Scholar]
- 47.Lauderdale DS, Oram RJ, Goldstein KP, Daum RS. Hepatitis B vaccination among children in inner-city public housing, 1991–1997. JAMA. 1999;282:1725–30. doi: 10.1001/jama.282.18.1725. [DOI] [PubMed] [Google Scholar]
- 48.Seal JB, Daum RS. What happened to primum non nocere? Pediatrics. 2001;107:1177–8. doi: 10.1542/peds.107.5.1177. [DOI] [PubMed] [Google Scholar]
- 49.Shete PB, Daum RS. Real versus theoretical: assessing the risks and benefits of postponing the hepatitis B vaccine birth dose. Pediatrics. 2002;109:701–3. doi: 10.1542/peds.109.4.701. [DOI] [PubMed] [Google Scholar]
- 50.Freeman VA, DeFriese GH. The challenge of potential of childhood immunization registries. Annu Rev Public Health. 2003;24:227–46. doi: 10.1146/annurev.publhealth.24.100901.140831. [DOI] [PubMed] [Google Scholar]
- 51.Bartlett DL, Molinari NA, Ortega-Sanchez IR, Urquhart GA. Economics of immunization information systems in the United States: assessing costs and efficiency. Cost Eff Resour Alloc. 2006;4:15. doi: 10.1186/1478-7547-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Serwint JR, Wilson ME, Vogelhut JW, Repke JT, Seidel HM. A randomized controlled trial of prenatal pediatric visits for urban, low-income families. Pediatrics. 1996;98(6 Pt 1):1069–75. [PubMed] [Google Scholar]