SYNOPSIS
Objectives
Posttraumatic stress disorder (PTSD) results from experiencing or witnessing traumatic, life-threatening events including combat-related experiences. The purpose of this study was to investigate the prevalence of PTSD symptoms and diagnosis, self-reported exposures, and functional health in a large cross-section of the U.S. military.
Methods
This study used baseline Millennium Cohort data (July 2001 to June 2003) of 75,156 U.S. military members to assess the population-based prevalence of PTSD symptoms, self-reported exposures, and functional health as measured by the Medical Outcomes Study Short Form 36-Item Health Survey for Veterans (SF-36V).
Results
PTSD diagnosis without current symptoms was reported by 953 respondents (1.2%, weighted), 1,490 respondents (2.1%, weighted) reported no diagnosis but reported PTSD symptoms, and 287 respondents (0.4%, weighted) reported diagnosis and current symptoms. Self-reported exposure to chemical or biological warfare agents, protective countermeasures, or hearing alarms were associated with PTSD symptoms independent of other combat-like exposures. Physical health was similar among those with PTSD diagnosis and current PTSD symptoms. However, compared with the overall cohort, lower mental health summary means for those reporting current PTSD symptoms (mean = 27.8), current symptoms and diagnosis (mean = 24.6), and diagnosis without current symptoms (mean = 47.5) were found.
Conclusions
Results suggest a 2.0% prevalence of PTSD symptoms without diagnosis and that self-reported threatening exposures were significantly associated with PTSD symptoms. Mental and physical health scores of those with current PTSD symptoms appear diminished, but suggest a return to cohort levels with resolution of PTSD symptoms.
Posttraumatic stress disorder (PTSD) is a psychiatric condition resulting from experiencing or witnessing traumatic events such as military combat,1–10 natural disasters,11 terrorist attacks,12–14 serious accidents,15 death,16 or violent assaults or other physical, sexual, or emotional abuse.17–21 Reported lifetime prevalence of PTSD in an adult U.S. sample of the National Comorbidity Survey was 7.8%, with women (10.4%) twice as likely as men (5.0%) to have PTSD at some point in their lives. Symptoms are likely to persist in at least one-third of those with PTSD.22
Participation in armed conflicts results in a multitude of adverse health outcomes, including emotional and psychological conditions from real and perceived exposures.23 Since the U.S. Civil War, comparable syndromes, illnesses, and conditions have been documented following every conflict, with some minor variations and different naming conventions.24 While acute combat stress reaction has been thought of as an immediate consequence of psychological trauma,25 PTSD, initially called “Post-Vietnam syndrome,” has since been used to describe a condition resulting from both short- and long-term consequences of extreme psychological stress.24,26,27
Although combat experience is an established cause of PTSD symptoms, little is known about other exposures associated with PTSD symptoms. Exposures, such as chemical or biological (chem/bio) agents, medical countermeasures against chem/bio agents, or hearing chemical agent alarms necessitating the wearing of chemical warfare protective gear, may have a profound influence on psychological morbidity and PTSD. Perceived threats may also play a role in developing PTSD symptoms independent of other combat experiences.23,28
This article reports the prevalence of PTSD symptoms and diagnosis in a large, population-based U.S. military cohort and investigates the association with self-reported exposure to chem/bio agents independent of other self-reported military, combat, and combat-related exposures. This article also documents the physical and mental health of those with PTSD symptoms and diagnosis and associated problem drinking and cigarette smoking.
METHODS
Population and data sources
This study included 75,156 baseline consenting participants from the first panel of the Millennium Cohort Study (enrolled July 2001 to June 2003), a 22-year longitudinal study of military personnel health.29 Designed oversampling resulted in a population-based U.S. military sample of more than 25% women and 30% deployed to Southwest Asia, Bosnia, or Kosovo between 1998 and 2000 as of October 1, 2000. This research was conducted in compliance with all applicable federal regulations governing the protection of human subjects in research (Protocol NHRC.2000.007).
In addition to self-reported survey data, demographic and military personnel data were linked to each participant and reflected military status as of October 1, 2000. These data included gender, birth year (pre-1960, 1960–1969, 1970–1979, and 1980 and later), education level (high school or less, some college or a bachelor's degree, more than a bachelor's degree), marital status (married, never married, divorced/other), pay grade (enlisted or officer), race/ethnicity (white non-Hispanic, black non-Hispanic, and other), service component (active duty or Reserve/Guard), service branch (Army, Air Force, Navy/Coast Guard, and Marines), and occupation (combat specialist, health-care specialist, functional and support specialist, or other).
Measures
Examination and diagnosis of PTSD has been debated since first appearing as a formal diagnosis in the Diagnostic and Statistical Manual of Mental Disorders, 3rd ed. (DSM-III), in 1980.30–38 Because traumas associated with PTSD are heterogeneous, defining PTSD and symptom criteria as well as establishing etiologies has been challenging.39–41 Further, the pattern of PTSD symptoms over time, emerging or reemerging long after the original trauma,26,42–48 contributes to the complexity of diagnosing PTSD and the differences in reported prevalence estimates.49
The PTSD Checklist–Civilian Version (PCL-C) is a 17-item self-report measure of PTSD symptoms that requires respondents to rate the severity of each symptom during the past 30 days on a five-point Likert scale ranging from 1 (not at all) to 5 (extremely). Participants were identified as having PTSD symptoms if they reported a moderate or higher level of at least one intrusion symptom, three avoidance symptoms, and two hyperarousal symptoms (criteria established by the DSM-IV),27 and had a score of 50 or more on a scale of 17 to 85.4,50–52 This approach has been shown to have reasonable sensitivity (0.60) and high specificity (0.99).53 Internal consistency of the PCL-C in this cohort, as measured using Cronbach's alpha (α=0.94), indicated an appropriate measurement tool for this population.54
In addition to the PCL-C assessment of PTSD, participants were asked, “Has your doctor or other health professional ever told you that you have any of the following conditions?: PTSD (no, yes). If yes, what year did the problem begin?”
Functional health was measured by the Medical Outcomes Study Short Form 36-Item Health Survey for Veterans (SF-36V).55–57 The SF-36V assesses eight health concepts55,58 that make up the physical component summary (PCS) and mental component summary (MCS).59,60 MCS and PCS scores were calculated using 1998 general U.S. population norm-based scoring algorithms, where a score of 50 and a standard deviation of 10 reflect the 1998 U.S. population. The scales are constructed such that higher scores reflect better functional health.55 If the respondent answered at least half of the questions in a scale, imputed values were used for the missing questions to reflect the mean of the score for the complete portion of that scale.55,58
Self-reported exposures
The Millennium Cohort questionnaire includes an occupational exposure section that asks, “Have you ever been exposed to the following?”, with allowable answers of “no,” “yes—one time,” and “yes—more than one time.” It also asks the year of exposure. Within this section are three items regarding exposures to chem/bio warfare or countermeasures for these weapons: (1) chem/bio warfare agents, (2) other medical countermeasures for chem/bio warfare agent exposure, and (3) alarms necessitating wearing chem/bio warfare protective gear. Within the chem/bio variable, if a cohort member reported exposure one or more times to (2) or (3) and not (1), they were designated as having reported exposure to medical countermeasures or alarms necessitating wearing protective gear for chem/bio warfare agents. If a cohort member reported exposure one or more times to (1), the individual was designated as reporting exposure to chem/bio warfare agents.
For the purposes of investigating the association between chem/bio exposure and PTSD independently of other combat-type exposures, questions about combat-type exposures addressing “Witnessing a person's death due to war, disaster, or tragic event,” “Knowledge of or witnessing instances of physical abuse (torture, beating, rape),” “Dead and/or decomposing bodies,” “Maimed soldiers/civilians,” and “Prisoners of war/refugees” were grouped into a single “combat-like exposure” variable.
Smoking cigarettes and drinking alcohol
Current smoking was assessed based on responses to the following questions: “In your lifetime, have you smoked at least 100 cigarettes (five packs)?”, “In the past year, have you used cigarettes?”, and “Have you ever tried to quit smoking?” Problem drinking was assessed using the CAGE questionnaire.61
Statistical analyses
We conducted descriptive and univariate comparisons of cohort members' exposures, functional health, demographics, and military characteristics, stratified by self-report of (1) no PTSD symptoms, (2) being told by a health-care professional that they had PTSD without current PTSD symptoms based on the PCL-C (PTSD diagnosis without symptoms), (3) PTSD symptoms based on the PCL-C without diagnosis (PTSD symptoms without diagnosis), and (4) being told by a health-care professional that they had PTSD with current PTSD symptoms based on the PCL-C (PTSD diagnosis and current PTSD symptoms).
Univariate analyses and adjusted odds ratios were weighted based on response differences from the proportion of 2000 U.S. military for gender, birth year, education, marital status, race/ethnicity, military rank, and military component (active duty or Reserve/Guard).
Variables examined included gender, age, education, marital status, and race/ethnicity; deployment to the 1991 Gulf War (GW), Southwest Asia (SWA), Bosnia (BOS), or Kosovo (KOS) (none, 1991 GW only, 1991 GW and BOS/KOS/SWA, or BOS/KOS/SWA only); other combat-like exposures (no/yes); rank, service branch, component, occupational category, smoking (no, past, current); and problem drinking (no/yes).
An initial analysis was completed to assess multicollinearity, significant associations, and possible confounding, while simultaneously adjusting for all other variables in the model. Confounding was investigated using a manual backward removal technique of variables that were not contributing significantly to the model, at α≤0.05, while potentially distorting the measure of effect by more than 15%.
Multivariate polychotomous logistic regression with response weights was used to investigate the adjusted association of self-reported exposures to chem/bio warfare agents, protective countermeasures for these agents, or hearing alarms due to these agents, with PTSD symptoms or self-reported health-care provider-indicated PTSD. Data management and statistical analyses were performed using SAS®.62
RESULTS
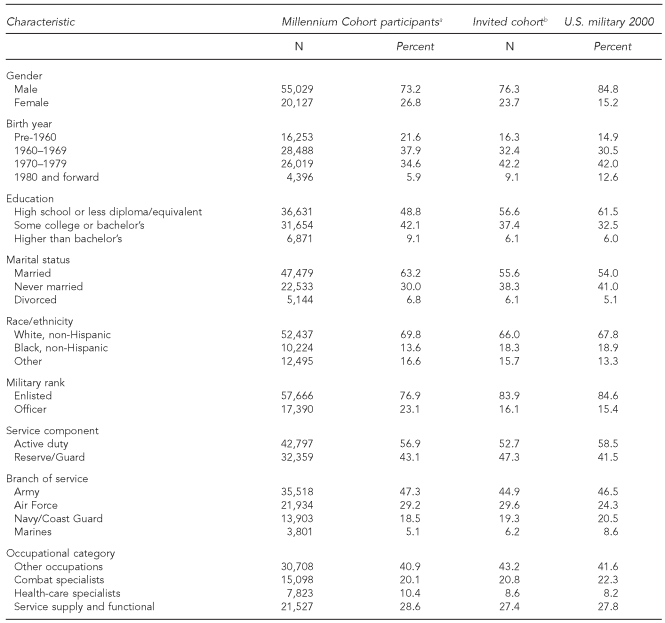
Complete military, demographic, PTSD, and MCS and PCS scores were available for 75,156 (about 98%) Millennium Cohort participants. Differences in characteristic proportions among the cohort, the invited sample, and the U.S. military in 2000 are reported in Table 1. The majority of the study population consisted of men who were born between 1960 and 1979, married, and enlisted members serving on active duty; other demographic features are shown in Table 1. In this cohort, 42% reported current or past smoking and 19% reporting problem drinking. Nearly 15% reported chem/bio alarms or countermeasures and 5% reported exposures to chem/bio warfare agents, while more than 40% reported other combat-like exposures (data not shown).
Table 1. Characteristics of Millennium Cohort participants, invited participants, and U.S. military in 2000.
aIncludes those with complete demographic, military, and self-reported data for these analyses.
bIncludes invited members who were contacted by U.S. Postal Service mail at least one time and had complete demographic data, with the exception of length of service.
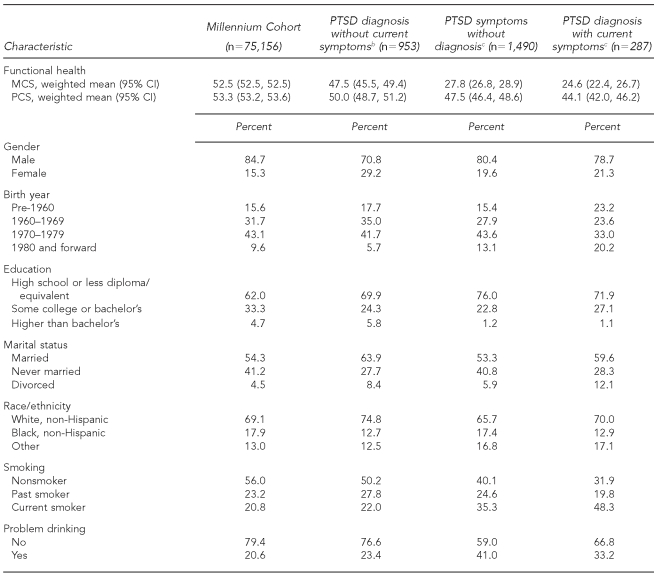
Table 2 compares the weighted demographic and behavioral characteristics after stratification by PTSD symptom and diagnosis status. As shown, 953 (1.2%, weighted) reported PTSD diagnosis without current symptoms, 1,490 (2.1%, weighted) reported PTSD symptoms without reporting a diagnosis, and 287 (0.4%, weighted) reported PTSD diagnosis along with reporting current symptoms. Those reporting PTSD diagnosis without symptoms, current PTSD symptoms, or PTSD diagnosis with current PTSD symptoms were significantly more likely to be women, less educated, and report current smoking and problem drinking behaviors. Those with no diagnosis of PTSD and current symptoms, or diagnosis of PTSD and current symptoms, had significantly less favorable PCS and MCS scores, while those with PTSD diagnosis and no current symptoms had lower scores that appeared closer in magnitude to the overall cohort means.
Table 2. Weighteda measures of demographic and behavioral characteristics by PTSD diagnosis and symptom status (2001–2003).
aWeighted for response differences in gender, birth year, education, marital status, race/ethnicity, military rank, and military component. Only participants with complete data were included.
bIncludes participants told they had PTSD by a health-care professional without current symptoms based on the PTSD Patient Checklist (PCL-C).
cPTSD symptoms at baseline enrollment determined using the PCL-C.
PTSD = posttraumatic stress disorder
MCS = mental component summary
PCS = physical component summary
CI = confidence interval
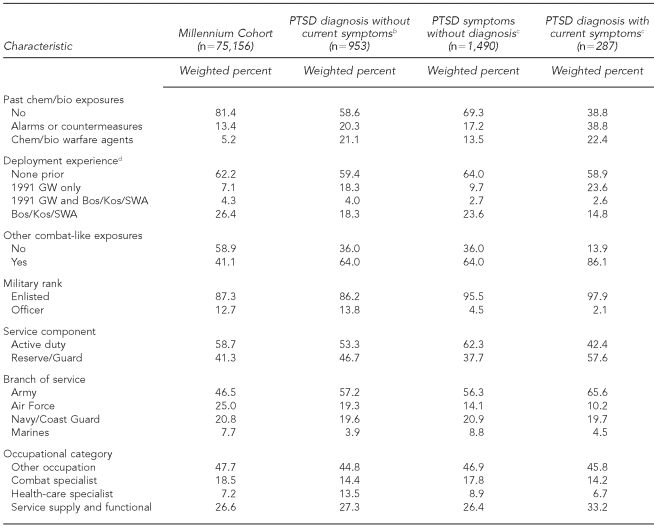
Table 3 compares the weighted military characteristics after stratification by PTSD symptom and diagnosis status. Those reporting PTSD diagnosis only, current PTSD symptoms only, or PTSD diagnosis with current PTSD symptoms were also more likely to report chem/bio exposure to alarms or countermeasures or chem/bio warfare agents and other combat exposures, and to have been deployed to the 1991 GW, enlisted, and Army personnel. Active-duty members were more likely to report current symptoms without a PTSD diagnosis. In contrast, Reserve/Guard members were more likely to report a diagnosis of PTSD with and without symptoms. Health-care specialists were also more likely to report a diagnosis of PTSD without symptoms.
Table 3. Weighteda measures of military characteristics by PTSD diagnosis and symptom status (2001–2003).
aWeighted for response differences in gender, birth year, education, marital status, race/ethnicity, military rank, and military component. Only participants with complete data were included.
bIncludes participants told they had PTSD by a health-care professional without current symptoms based on the PTSD Patient Checklist (PCL-C).
cPTSD symptoms at baseline enrollment determined using the PCL-C
dDeployment to SWA/Bos/Kos anytime from January 1, 1998, to September 30, 2000
PTSD = posttraumatic stress disorder
Chem/bio = self-reported exposure to chemical or biological warfare agents, protective countermeasures for these agents, or hearing alarms due to these agents
GW = Gulf War
Bos = Bosnia
Kos = Kosovo
SWA = Southwest Asia
Investigation of multicollinearity, using variance inflation factors of greater than four to establish multicollinearity, showed there were no variables in Table 1 exhibiting noteworthy multicollinearity.
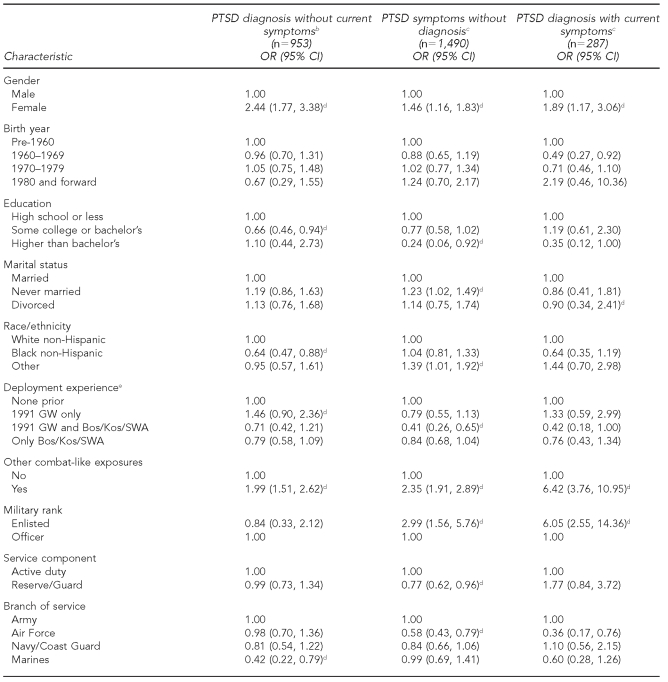
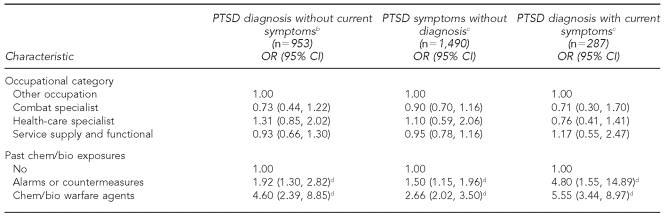
Weighted multivariate polychotomous logistic regression results for demographic and military characteristics are presented in Table 4. Those reporting chem/bio agent alarms or countermeasure exposure or other combat-like exposures were significantly more likely to also report PTSD diagnosis with and without current symptoms as well as current PTSD symptoms without diagnosis when compared with those with no PTSD symptoms or diagnosis.
Table 4. Weighteda and adjusted odds of reporting PTSD symptoms when compared with reporting of no PTSD symptoms (n=72,225) using multivariate polychotomous logistic regression with various military and demographic characteristics (2001–2003).
aWeighted for response differences in gender, birth year, education, marital status, race/ethnicity, military rank, and military component. Only participants with complete data were included in this table.
bIncludes participants told they had PTSD by a health-care professional without current symptoms based on the PTSD Patient Checklist, PCL-C.
cPTSD symptoms at baseline enrollment were determined using the PCL-C.
dStatistically significant at α<0.05
eDeployment to Southwest Asia, Bosnia, or Kosovo anytime from January 1, 1998, to September 30, 2000
PTSD = posttraumatic stress disorder
OR = odds ratio
CI = confidence interval
Chem/bio = self-reported exposure to chemical or biological warfare agents, protective countermeasures for these agents, or hearing alarms due to these agents
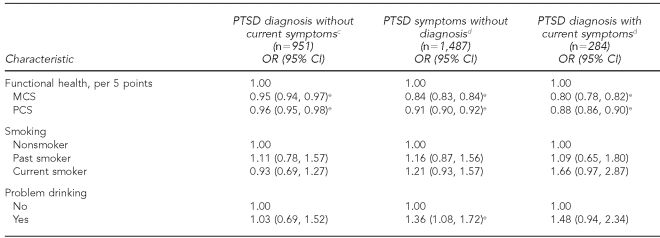
Weighted multivariate polychotomous logistic regression results for possible comorbidities are shown in Table 5. Those with more favorable MCS and PCS scores were significantly less likely to report PTSD diagnosis or current PTSD symptoms when compared with those with no PTSD symptoms or diagnosis. Those reporting signs of problem drinking were 1.36 times more likely to report PTSD symptoms without diagnosis when compared with those without signs of problem drinking (95% confidence interval 1.08, 1.72).
Table 5. Weighteda and adjustedb odds of reporting PTSD symptoms when compared with reporting of no PTSD symptoms (n=72,225) using multivariate polychotomous logistic regression for potential comorbidities (2001–2003).
aWeighted for response differences in gender, birth year, education, marital status, race/ethnicity, military rank, and military component. Only participants with complete data were included in this table. Adjusted for past chem/bio exposures, sex, birth year, education, marital status, race/ethnicity, deployment experience, other combat-like exposures, military rank, service component, branch of service, and occupational category.
bAdjusted for sex, age, education, marital status, race/ethnicity, chem/bio exposure, previous deployment, other combat-like exposures, rank, component, service branch, and occupation
cIncludes participants previously told they had PTSD by a health-care professional without current symptoms based on the PTSD Patient Checklist (PCL-C).
dPTSD symptoms at baseline enrollment determined using the PTSD PCL-C.
eStatistically significant at α<0.05
PTSD = posttraumatic stress disorder
OR = odds ratio
CI = confidence interval
MCS = mental component summary
PCS = physical component summary
DISCUSSION
PTSD affects physical and mental health and is associated with numerous comorbidities. In this study, the combined weighted prevalence of diagnosed and undiagnosed PTSD symptoms was 3.7%. The majority of these individuals (2.0%) were those with PTSD symptoms without a diagnosis of PTSD; a little more than 1.0% reported being told in their lifetime by a health-care professional that they had PTSD but did not exhibit current symptoms as defined by the PCL-C. Differences in the amount of self-reported PTSD in U.S. military found in these analyses as compared with that reported elsewhere were likely due to variations in the populations studied and time period of assessment.4
This article also documented the self-reported stressful experiences of exposure to chem/bio warfare agents, protective countermeasures, or hearing alarms due to these agents as being significantly associated with PTSD diagnosis and current PTSD symptoms independent of other combat and combat-like exposures. We found a strong association between current PTSD symptoms and decreased mental and physical health, as well as a tendency toward levels in the general cohort of mental and physical health with the apparent resolution of PTSD symptoms.
Finding a significant association between reporting PTSD symptoms or diagnosis and reporting an experience related to chem/bio warfare, independent of reporting other combat-like exposures, is interesting. There is no evidence that chemical warfare nerve agents were used during the 1991 GW.23 Therefore, increased exposure reporting may be related to combat stress63 and may also result in increased symptom reporting. Alternatively, although evidence of exposure to chem/bio warfare agents during the 1991 GW has not been shown, the perception of a chem/bio exposure significantly increased the odds for reporting of PTSD symptoms among those with both diagnosis and current symptoms. This type of self-reported exposure, while difficult to validate, may be used as a surrogate for unmeasurable stressful or life-threatening exposures that may be experienced in combat situations and may result in an important cause of post-combat morbidity.
Diminished physical and mental health in association with current PTSD symptoms confirms previous findings.64,65 It is noteworthy, however, that those with past PTSD diagnoses demonstrating apparently resolved symptoms had physical and mental functioning similar to the general cohort. The mental health of those with current symptoms was surprisingly low in the context of the magnitude of the PCS and may reflect a population that appears physically fit for duty but that may be vulnerable to stress induced from deployment to combat areas. While the 2.0% who reported PTSD symptoms without a diagnosis may be indicative of those without the disorder, these individuals may also represent a population without knowledge, understanding, or acceptance of the disorder. These individuals appear physically fit and may not display noticeable signs of lower functioning to health-care providers or superiors. Enhanced and standardized screening for PTSD symptoms, along with coordinated controlled trials to investigate effectiveness of treatment methods, may benefit those with undiagnosed PTSD symptoms.
The use of alcohol and cigarettes was evident in those with current PTSD symptoms. However, the prevalence of both problem drinking and current smoking seemed to approach general cohort levels in those reporting PTSD diagnosis without current symptoms based on the PCL-C. This, in itself, may be a marker for those who never had PTSD symptoms or perhaps a marker for those with resolution of symptoms. If associated with resolution of PTSD symptoms, it would be a positive outcome and suggest that effective treatment of individuals, returning them to non-symptomatic levels of PTSD, may reduce the risk of adverse health behaviors such as problem drinking and smoking.
Limitations
Limitations to these analyses should be considered. First, although 71% participated in follow-up surveying between June 2004 and February 2006, the initial response to the invitation for participation was 36%.29 The generalizability of results based on data from this cohort to all U.S. military has been examined by investigating potential reporting biases among Millennium Cohort participants. These analyses have shown no differences in responder health with respect to medical encounters in the year prior to enrollment,66 strong test-retest reliability,54 reliable vaccination reporting,67,68 occupation reporting,69 and deployment reporting,70 and little difference between participants choosing Web submission vs. paper submission.71
Differential response rates that are influenced by PTSD symptoms are particularly concerning. Further, it is possible that those who were ill may have believed that inclusion in a study of this type might be of benefit to them, resulting in a possible overestimation of the true prevalence of PTSD. Conversely, those who may have been physically or mentally ill, specifically those who may have PTSD, may have found the survey distressing and chosen not to respond; this would potentially underestimate the true prevalence of PTSD.
Further analyses of potential response bias to continued follow-up are ongoing. Self-report of exposures and outcome data used to represent the true exposure and disease prevalence in this cohort may be limited. Studies have shown that increased exposure and symptom reporting occur among personnel seeking medical compensation.72 However, compensation is not offered to Millennium Cohort participants, and this fact may mitigate this bias. Still, differential reporting of either exposures or symptoms would bias these results and may result in incorrect inferences based on PTSD symptom and exposure reporting.
Further, it was not possible to discern those exposures that were truly unique to military service from those that could be encountered through other occupational or nonoccupational activities. Lastly, although the PCL-C has undergone thorough testing and has been found to correlate well with a physician's assessment of PTSD, the use of a survey instrument as a surrogate for PTSD diagnosis is imperfect and can only measure PTSD symptoms in a population. However, PTSD is often underreported in health-care databases due to the stigma associated with mental health illness, making self-reported instruments essential tools for identifying this disorder in populations not readily submitting for care for mental disorders.
Strengths
There were also many strengths in these analyses. Although self-reported data were inherently limited, they were also invaluable for the information provided that was not accessible elsewhere. Further, the use of a standard instrument allowed for comparison with other populations, such as the U.S. population in general and other military populations. Additionally, the large sample, including a large proportion of women, allowed for robust estimation of prevalence and associations.
CONCLUSION
We documented a 2.0% prevalence of current PTSD symptoms without diagnosis and an almost 0.5% prevalence of current PTSD symptoms with a health-care provider diagnosis. Rising concern regarding deployment-related exposures as well as the decreased physical and mental health associated with PTSD in returning deployed personnel have prompted many investigations into the etiologies of PTSD and associated comorbidities. In addition to describing the prevalence of diagnosis and current PTSD symptoms in a large U.S. military cohort, we investigated how PTSD was associated with self-reported stressful exposures.
Findings suggested that real or perceived exposures to chem/bio warfare agents, protective countermeasures for these agents, or hearing alarms due to these agents were associated with a twofold increased risk for diagnosis or current PTSD symptoms. Those with a PTSD diagnosis with no current PTSD symptoms had significantly better physical and mental health when compared with those with current PTSD symptoms, possibly suggesting overreporting of PTSD diagnosis or resolved symptomology. More research is necessary to prospectively evaluate the risk for development of PTSD after significant combat deployments and to identify the types of combat exposures most predictive of PTSD onset. The Millennium Cohort, a prospective 22-year study, will soon meet this important research need.
Acknowledgments
The authors thank all Millennium Cohort Study participants: Scott L. Seggerman and Greg D. Boyd from the Management Information Division, Defense Manpower Data Center in Seaside, California; Gina Creaven, MBA; James Davies; Syke Endara, MPH; Lacy Farnell; Nisara Granado, MPH, PhD; Gia Gumbs, MPH; Molly Kelton, MS; Cynthia LeardMann, MPH; Travis Leleu; Jamie McGrew; Robert Reed, MS; Katherine Snell; Steven Spiegel; Kari Welch, MA; Martin White, MPH; James Whitmer; Charlene Wong, MPH; and Lauren Zimmermann, MPH, from the Department of Defense (DoD) Center for Deployment Health Research, Naval Health Research Center, San Diego, California; and Michelle Stoia, also from the Naval Health Research Center. The authors also thank the professionals from the U.S. Army Medical Research and Material Command, especially those from the Military Operational Medicine Research Program in Fort Detrick, Maryland. And the authors appreciate the support of the Henry M. Jackson Foundation for the Advancement of Military Medicine in Rockville, Maryland.
Footnotes
In addition to the authors, the Millennium Cohort Study Team includes Paul J. Amoroso, MD, MPH, of the Madigan Army Medical Center in Tacoma, Washington; Edward J. Boyko, MD, MPH, of the Seattle Epidemiologic Research and Information Center, Department of Veterans Affairs Puget Sound Healthcare System in Seattle, Washington; Gary D. Gackstetter, PhD, DVM, MPH, of the Department of Preventive Medicine and Biometrics, Uniformed Services University of the Health Sciences in Bethesda, Maryland, and Analytic Services, Inc., in Arlington, Virginia; Gregory C. Gray, MD, MPH, of the College of Public Health, University of Iowa in Iowa City, Iowa; Tomoko I. Hooper, MD, MPH, of the Department of Preventive Medicine and Biometrics, Uniformed Services University of the Health Sciences; James R. Riddle, DVM, MPH, of the Air Force Research Laboratory at Wright-Patterson Air Force Base in Dayton, Ohio; Besa Smith, MPH, of the DoD Center for Deployment Health Research at the Naval Health Research Center in San Diego, and the Division of Epidemiology, Department of Family and Preventive Medicine at the University of California San Diego in La Jolla, California; and Timothy S. Wells, DVM, MPH, PhD, of the Air Force Research Laboratory at Wright-Patterson Air Force Base.
This article represents Naval Health Research Center report 07-040, supported by the DoD, under work unit no. 60002. The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of the Army, Department of the Air Force, DoD, Department of Veterans Affairs, the U.S. Government, or the University of California San Diego.
REFERENCES
- 1.Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, et al. Trauma and the Vietnam War generation: report of findings from the National Vietnam Veterans Readjustment Study. New York: Brunner/Mazel; 1990. [Google Scholar]
- 2.Kang HK, Hyams KC. Mental health care needs among recent war veterans. N Engl J Med. 2005;352:1289. doi: 10.1056/NEJMp058024. [DOI] [PubMed] [Google Scholar]
- 3.Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157:141–8. doi: 10.1093/aje/kwf187. [DOI] [PubMed] [Google Scholar]
- 4.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 5.Bremner JD, Southwick SM, Darnell A, Charney DS. Chronic PTSD in Vietnam combat veterans: course of illness and substance abuse. Am J Psychiatry. 1996;153:369–75. doi: 10.1176/ajp.153.3.369. [DOI] [PubMed] [Google Scholar]
- 6.Orr SP, Pitman RK, Lasko NB, Herz LR. Psychophysiological assessment of posttraumatic stress disorder imagery in World War II and Korean combat veterans. J Abnorm Psychol. 1993;102:152–9. doi: 10.1037//0021-843x.102.1.152. [DOI] [PubMed] [Google Scholar]
- 7.Friedman MJ. Veterans' mental health in the wake of war. N Engl J Med. 2005;352:1287–90. doi: 10.1056/NEJMp058028. [DOI] [PubMed] [Google Scholar]
- 8.Card JJ. Epidemiology of PTSD in a national cohort of Vietnam veterans. J Clin Phychol. 1987;43:6–17. doi: 10.1002/1097-4679(198701)43:1<6::aid-jclp2270430103>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 9.Foy DW, Sipprelle RC, Rueger DB, Carroll EM. Etiology of posttraumatic stress disorder in Vietnam veterans: analysis of premilitary, military, and combat exposure influences. J Consult Clin Psychol. 1984;52:79–87. doi: 10.1037//0022-006x.52.1.79. [DOI] [PubMed] [Google Scholar]
- 10.Smith TC, Ryan MA, Wingard DL, Slymen DJ, Sallis JF, Kritz-Silverstein D. New onset and persistent symptoms of post-traumatic stress disorder self-reported after deployment and combat exposures: prospective population-based U.S. military cohort study. BMJ. 2008;336:366–71. doi: 10.1136/bmj.39430.638241.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goenjian AK, Steinberg AM, Najarian LM, Fairbanks LA, Tashjian M, Pynoos RS. Prospective study of posttraumatic stress, anxiety, and depressive reactions after earthquake and political violence. Am J Psychiatry. 2000;157:911–6. doi: 10.1176/appi.ajp.157.6.911. [DOI] [PubMed] [Google Scholar]
- 12.Verger P, Dab W, Lamping DL, Loze JY, Deschaseaux-Voinet C, Abenhaim L, et al. The psychological impact of terrorism: an epidemiologic study of posttraumatic stress disorder and associated factors in victims of the 1995–1996 bombings in France. Am J Psychiatry. 2004;161:1384–9. doi: 10.1176/appi.ajp.161.8.1384. [DOI] [PubMed] [Google Scholar]
- 13.Lating JM, Sherman MF, Everly GS, Jr, Lowry JL, Peragine TF. PTSD reactions and functioning of American Airlines flight attendants in the wake of September 11. J Nerv Ment Dis. 2004;192:435–41. doi: 10.1097/01.nmd.0000126732.00555.4b. [DOI] [PubMed] [Google Scholar]
- 14.Rosenheck R, Fontana A. Use of mental health services by veterans with PTSD after the terrorist attacks of September 11. Am J Psychiatry. 2003;160:1684–90. doi: 10.1176/appi.ajp.160.9.1684. [DOI] [PubMed] [Google Scholar]
- 15.Maes M, Mylle J, Delmeire L, Janca A. Pre- and post-disaster negative life events in relation to the incidence and severity of post-traumatic stress disorder. Psychiatry Res. 2001;105:1–12. doi: 10.1016/s0165-1781(01)00325-0. [DOI] [PubMed] [Google Scholar]
- 16.Ursano RJ, Fullerton CS, Kao TC, Bhartiya VR. Longitudinal assessment of posttraumatic stress disorder and depression after exposure to traumatic death. J Nerv Ment Dis. 1995;183:36–42. doi: 10.1097/00005053-199501000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Nishith P, Mechanic MB, Resick PA. Prior interpersonal trauma: the contribution to current PTSD symptoms in female rape victims. J Abnorm Psychol. 2000;109:20–5. [PMC free article] [PubMed] [Google Scholar]
- 18.Dahl S. Acute response to rape—a PTSD variant. Acta Psychiatr Neurol Scand. 1989;355:56–62. doi: 10.1111/j.1600-0447.1989.tb05254.x. [DOI] [PubMed] [Google Scholar]
- 19.Bownes IT, O'Gorman EC, Sayers A. Assault characteristics and posttraumatic stress disorder in rape victims. Acta Psychiatr Neurol Scand. 1991;83:27–30. doi: 10.1111/j.1600-0447.1991.tb05507.x. [DOI] [PubMed] [Google Scholar]
- 20.Roth S, Newman E, Pelcovitz D, van der Kolk B, Mandel FS. Complex PTSD in victims exposed to sexual and physical abuse: results from the DSM-IV Field Trial for Posttraumatic Stress Disorder. J Trauma Stress. 1997;10:539–55. doi: 10.1023/a:1024837617768. [DOI] [PubMed] [Google Scholar]
- 21.Street AE, Arias I. Psychological abuse and posttraumatic stress disorder in battered women: examining the roles of shame and guilt. Violence Vict. 2001;16:65–78. [PubMed] [Google Scholar]
- 22.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 23.Riddle JR, Brown M, Smith TC, Ritchie EC, Brix KA, Romano J. Chemical warfare and the Gulf War: a review of the impact on Gulf veterans' health. Mil Med. 2003;168:606–13. [PubMed] [Google Scholar]
- 24.Hyams KC, Wignall FS, Roswell R. War syndromes and their evaluation: from the U.S. Civil War to the Persian Gulf War. Ann Intern Med. 1996;125:398–405. doi: 10.7326/0003-4819-125-5-199609010-00007. [DOI] [PubMed] [Google Scholar]
- 25.Kentsmith DK. Principles of battlefield psychiatry. Mil Med. 1986;151:89–96. [PubMed] [Google Scholar]
- 26.The Centers for Disease Control Vietnam Experience Study. Health status of Vietnam veterans. I. Psychosocial characteristics. JAMA. 1988;259:2701–7. [PubMed] [Google Scholar]
- 27.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. DSM-IV. Washington: American Psychiatric Association; 1994. [Google Scholar]
- 28.Bendor A, Gelkopf M, Sigal M. Insanity and war: the Gulf War and a psychiatric institution. Am J Psychother. 1993;47:424–42. doi: 10.1176/appi.psychotherapy.1993.47.3.424. [DOI] [PubMed] [Google Scholar]
- 29.Ryan MA, Smith TC, Smith B, Amoroso P, Boyko EJ, Gray GC, et al. Millennium Cohort: enrollment begins a 21-year contribution to understanding the impact of military service. J Clin Epidemiol. 2007;60:181–91. doi: 10.1016/j.jclinepi.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 30.Turnbull GJ. A review of post-traumatic stress disorder. Part I: historical development and classification. Injury. 1998;29:87–91. doi: 10.1016/s0020-1383(97)00131-9. [DOI] [PubMed] [Google Scholar]
- 31.Turnbull GJ. A review of post-traumatic stress disorder. Part II: treatment. Injury. 1998;29:169–75. doi: 10.1016/s0020-1383(97)00132-0. [DOI] [PubMed] [Google Scholar]
- 32.Jones E, Hodgins-Vermaas R, McCartney H, Everitt B, Beech C, Poynter D, et al. Post-combat syndromes from the Boer War to the Gulf War: a cluster analysis of their nature and attribution. BMJ. 2002;324:321–4. doi: 10.1136/bmj.324.7333.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jones E, Vermaas RH, McCartney H, Beech C, Palmer I, Hyams K, et al. Flashbacks and post-traumatic stress disorder: the genesis of a 20th-century diagnosis. Br J Psychiatry. 2003;182:158–63. doi: 10.1192/bjp.182.2.158. [DOI] [PubMed] [Google Scholar]
- 34.Davidson J, Smith R, Kudler H. Validity and reliability of the DSM-III criteria for posttraumatic stress disorder. Experience with a structured interview. J Nerv Ment Dis. 1989;177:336–41. doi: 10.1097/00005053-198906000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Kuhne A, Baraga E, Czekala J. Completeness and internal consistency of DSM-III criteria for post-traumatic stress disorder. J Clin Psychol. 1988;44:717–22. doi: 10.1002/1097-4679(198809)44:5<717::aid-jclp2270440508>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 36.Brett EA, Spitzer RL, Williams JB. DSM-III-R criteria for posttraumatic stress disorder. Am J Psychiatry. 1988;145:1232–6. doi: 10.1176/ajp.145.10.1232. [DOI] [PubMed] [Google Scholar]
- 37.Feinstein A. Posttraumatic stress disorder: a descriptive study supporting DSM-III-R criteria. Am J Psychiatry. 1989;146:665–6. doi: 10.1176/ajp.146.5.665. [DOI] [PubMed] [Google Scholar]
- 38.Solomon SD, Canino GJ. Appropriateness of DSM-III-R criteria for posttraumatic stress disorder. Compr Psychiatry. 1990;31:227–37. doi: 10.1016/0010-440x(90)90006-e. [DOI] [PubMed] [Google Scholar]
- 39.Maes M, Delmeire L, Schotte C, Janca A, Creten T, Mylle J, et al. Epidemiologic and phenomenological aspects of post-traumatic stress disorder: DSM-III-R diagnosis and diagnostic criteria not validated. Psychiatry Res. 1998;81:179–93. doi: 10.1016/s0165-1781(98)00095-x. [DOI] [PubMed] [Google Scholar]
- 40.Kinzie JD, Goetz RR. A century of controversy surrounding posttraumatic stress-spectrum syndromes: the impact on DSM-III and DSM-IV. J Trauma Stress. 1996;9:159–79. doi: 10.1007/BF02110653. [DOI] [PubMed] [Google Scholar]
- 41.Wessely S. Risk, psychiatry and the military. Br J Psychiatry. 2005;186:459–66. doi: 10.1192/bjp.186.6.459. [DOI] [PubMed] [Google Scholar]
- 42.King DW, King LA, Erickson DJ, Huang MT, Sharkansky EJ, Wolfe J. Posttraumatic stress disorder and retrospectively reported stressor exposure: a longitudinal prediction model. J Abnorm Psychol. 2000;109:624–33. doi: 10.1037//0021-843x.109.4.624. [DOI] [PubMed] [Google Scholar]
- 43.Engdahl BE, Speed N, Eberly RE, Schwartz J. Comorbidity of psychiatric disorders and personality profiles of American World War II prisoners of war. J Nerv Ment Dis. 1991;179:181–7. doi: 10.1097/00005053-199104000-00001. [DOI] [PubMed] [Google Scholar]
- 44.McFarlane AC. The longitudinal course of posttraumatic morbidity. The range of outcomes and their predictors. J Nerv Ment Dis. 1988;176:30–9. doi: 10.1097/00005053-198801000-00004. [DOI] [PubMed] [Google Scholar]
- 45.McFarlane AC. The prevalence and longitudinal course of PTSD. Implications for the neurobiological models of PTSD. Ann N Y Acad Sci. 1997;821:10–23. doi: 10.1111/j.1749-6632.1997.tb48265.x. [DOI] [PubMed] [Google Scholar]
- 46.Solomon Z, Mikulincer M, Waysman M. Delayed and immediate onset posttraumatic stress disorder. II. The role of battle experiences and personal resources. Soc Psychiatry Psychiatr Epidemiol. 1991;26:8–13. doi: 10.1007/BF00783574. [DOI] [PubMed] [Google Scholar]
- 47.Solomon Z, Mikulincer M, Waysman M, Marlowe DH. Delayed and immediate onset posttraumatic stress disorder. I. Differential clinical characteristics. Soc Psychiatry Psychiatr Epidemiol. 1991;26:1–7. doi: 10.1007/BF00783573. [DOI] [PubMed] [Google Scholar]
- 48.Port CL, Engdahl B, Frazier P. A longitudinal and retrospective study of PTSD among older prisoners of war. Am J Psychiatry. 2001;158:1474–9. doi: 10.1176/appi.ajp.158.9.1474. [DOI] [PubMed] [Google Scholar]
- 49.Thompson WW, Gottesman II, Zalewski C. Reconciling disparate prevalence rates of PTSD in large samples of U.S. male Vietnam veterans and their controls. BMC Psychiatry. 2006;6:19. doi: 10.1186/1471-244X-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. Paper presented at the Annual Meeting of International Society for Traumatic Stress Studies; 1993 Oct 6–10; San Antonio, Texas. [cited 2006 Jul 10]. Also available from: URL: http://www.pdhealth.mil/library/downloads/PCL_sychometrics.doc. [Google Scholar]
- 51.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34:669–73. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 52.Wright KM, Huffman AH, Adler AB, Castro CA. Psychological screening program overview. Mil Med. 2002;167:853–61. [PubMed] [Google Scholar]
- 53.Brewin CR. Systematic review of screening instruments for adults at risk of PTSD. J Trauma Stress. 2005;18:53–62. doi: 10.1002/jts.20007. [DOI] [PubMed] [Google Scholar]
- 54.Smith TC, Smith B, Jacobson IG, Corbeil TE, Ryan MA. Reliability of standard health assessment instruments in a large, population-based cohort study. Ann Epidemiol. 2007;17:525–32. doi: 10.1016/j.annepidem.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 55.Ware JE, Kosinski M, Gandek B. SF-36 health survey: manual and interpretation guide. Lincoln (RI): Quality Metric Inc.; 2000. [Google Scholar]
- 56.Ware JE, Jr, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 57.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 58.Ware JE, Davies AR, Brook RH. Conceptualization and measurement of health for adults in the Health Insurance Study. Volume VI: analysis of relationships among health status measures. Santa Monica (CA): The Rand Corporation; 1980. [Google Scholar]
- 59.Ware JE, Kosinski M, Keller SD. SF-36 physical and mental health summary scales: a user's manual. Boston: Health Assessment Lab; 1994. [Google Scholar]
- 60.Perlin J, Kazis LE, Skinner K, Ren XS, Lee A, Rogers WH, et al. Health status and outcomes of veterans: physical and mental component summary scores, Veterans SF-36, 1999 Large Health Survey of Veteran Enrollees. Washington: Department of Veterans Affairs, Veteran's Health Administration, Office of Quality and Performance (US); 2000. Executive report. [Google Scholar]
- 61.Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;252:1905–7. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 62.SAS Institute Inc. SAS: Version 9.1.3. Cary (NC): SAS Institute Inc.; 2004. [Google Scholar]
- 63.Stuart JA, Ursano RJ, Fullerton CS, Wessely S. Belief in exposure to chemical and biological agents in Persian Gulf War soldiers. J Nerv Ment Dis. 2008;196:122–7. doi: 10.1097/NMD.0b013e318162aad3. [DOI] [PubMed] [Google Scholar]
- 64.Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, Bradley KA. Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment. Arch Intern Med. 2004;164:394–400. doi: 10.1001/archinte.164.4.394. [DOI] [PubMed] [Google Scholar]
- 65.Magruder KM, Frueh BC, Knapp RG, Johnson MR, Vaughan JA, 3rd, Carson TC, et al. PTSD symptoms, demographic characteristics, and functional status among veterans treated in VA primary care clinics. J Trauma Stress. 2004;17:293–301. doi: 10.1023/B:JOTS.0000038477.47249.c8. [DOI] [PubMed] [Google Scholar]
- 66.Wells TS, Jacobson IG, Smith TC, Spooner CN, Smith B, Reed RJ, et al. Prior health care utilization as a potential determinant of enrollment in a 21-year prospective study, the Millennium Cohort Study. Eur J Epidemiol. 2008;23:79–87. doi: 10.1007/s10654-007-9216-0. [DOI] [PubMed] [Google Scholar]
- 67.Smith B, Leard CA, Smith TC, Reed RJ, Ryan MA. Anthrax vaccination in the Millennium Cohort; validation and measures of health. Am J Prev Med. 2007;32:347–53. doi: 10.1016/j.amepre.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 68.LeardMann CA, Smith B, Smith TC, Wells TS, Ryan MA. Smallpox vaccination: comparison of self-reported and electronic vaccine records in the Millennium Cohort Study. Hum Vaccin. 2007;3:245–51. doi: 10.4161/hv.4589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Smith TC, Jacobson IG, Smith B, Hooper TI, Ryan MA, Team FT. The occupational role of women in military service: validation of occupation and prevalence of exposures in the Millennium Cohort Study. Int J Environ Health Res. 2007;17:271–84. doi: 10.1080/09603120701372243. [DOI] [PubMed] [Google Scholar]
- 70.Smith B, Wingard DL, Ryan MA, Macera CA, Patterson TL, Slymen DJ. U.S. military deployment during 2001–2006: comparison of subjective and objective data sources in a large prospective health study. Ann Epidemiol. 2007;17:976–82. doi: 10.1016/j.annepidem.2007.07.102. [DOI] [PubMed] [Google Scholar]
- 71.Smith B, Smith TC, Gray GC, Ryan MA. When epidemiology meets the Internet: Web-based surveys in the Millennium Cohort Study. Am J Epidemiol. 2007;166:1345–54. doi: 10.1093/aje/kwm212. [DOI] [PubMed] [Google Scholar]
- 72.Frueh BC, Elhai JD, Grubaugh AL, Monnier J, Kashdan TB, Sauvageot JA, et al. Documented combat exposure of U.S. veterans seeking treatment for combat-related post-traumatic stress disorder. Br J Psychiatry. 2005;186:467–72. doi: 10.1192/bjp.186.6.467. [DOI] [PubMed] [Google Scholar]