Abstract
Poor marital quality is a reliable correlate of internalizing problems, but the etiology of this association has yet to be examined. Marital distress may exert its influence by acting as a stressor that enables the expression of latent genetic risk for internalizing psychopathology. We examined this question using 379 twin pairs concordant for marriage who were assessed for marital quality, symptoms of major depression (MD), generalized anxiety disorder (GAD), panic attacks (PA), and neuroticism (N). First, we conducted a phenotypic factor analysis to confirm that one factor best accounted for the variance shared between MD, GAD, PA, and N. After accounting for genetic influences on the general internalizing factor, there were residual genetic influences on neuroticism but no specific genetic influences on any other individual internalizing syndrome. We then investigated the overlap between genetic and environmental influences on both marital quality and the internalizing spectrum, and found genetic influences common to both phenotypes. Finally, biometrical moderation models revealed that genetic effects on the internalizing factor decreased from low (h2=.29) to high (h2=.05) levels of marital quality, suggesting that those with a genetic predisposition to internalizing syndromes may be more likely to express this predisposition in the context of a dissatisfying marriage.
Keywords: depression, anxiety, neuroticism, factor
Extensive comorbidity among the mood and anxiety disorders has led to the theoretical and empirical conceptualization of an “internalizing” spectrum characterized by a latent liability to general distress and worry (e.g., Krueger & Markon, 2006; Watson, 2005) that is also etiologically coherent (Hettema, Neale, Myers, Prescott, & Kendler, 2006; Kendler, Prescott, Myers, & Neale, 2003), with genetic and environmental influences that parallel the phenotypic structure. Internalizing syndromes often co-occur with difficulties in social and interpersonal functioning. For instance, relationship distress has long been linked with mood and anxiety disorders and neuroticism both concurrently and longitudinally (for a review, see Whisman & Uebelacker, 2003). Only recently has research emerged studying the relationship between mental health and marital quality within a genetically informative design (Spotts et al., 2004a). A next logical step in the study of etiological links between internalizing syndromes and marital quality is the idea that genetic and environmental influences on internalizing syndromes may vary as a function of levels of marital quality. This is a question of gene × environment (G×E) interaction, also defined as genetic susceptibility to environmental risk. It may be that there are certain people whose inherited liabilities increase their sensitivity to symptoms of depression or anxiety as a result of being in a marriage that is unsatisfying or conflict-laden.
Evidence for the Existence and Coherent Etiology of the Internalizing Spectrum
Researchers have theorized that the mood and anxiety disorders represent different manifestations of psychopathology within a single coherent spectrum. Underlying all of the disorders is a general dimension of negative affect, while (low) positive affect is a component of mood disorders and social phobia, and physiological hyperarousal is common to panic disorder and post-traumatic stress disorder (Clark & Watson, 1991; Mineka, Watson, & Clark, 1998; Watson, 2005; Watson, Clark, & Carey, 1988). Research has shown that the comorbidity among mood and anxiety disorders can largely be accounted for by the personality trait of neuroticism (Battaglia, Przybeck, Bellodi, & Cloninger, 1996; Bienvenu et al., 2001; Clark, Waston, & Mineka, 1994; Khan, Jacobson, Gardner, Prescott, & Kendler, 2005). Empirical evidence from several large scale studies that collected diagnostic data across the range of Axis I syndrome disorders provide evidence that the phenotypic structure is best captured with a two factor model involving Externalizing and Internalizing spectrums (Krueger, 1999; Krueger, Caspi, Moffitt, & Silva, 1998; Slade & Watson, 2006; Vollebergh et al., 2001). Krueger and Markon (2006) conducted a meta-analysis of multivariate comorbidity studies and confirmed that a higher-order Internalizing spectrum split into two, highly correlated lower order factors of Distress (major depression, dysthymia, GAD), and Fear (panic disorder, agoraphobia, social phobia, specific phobia).
Findings from behavior genetic modeling of comorbidity suggest that the internalizing spectrum is etiologically coherent, providing further support in favor of a liability-spectrum model. Bivariate biometrical studies of the genetic and environmental influences common to specific combinations of internalizing syndromes (i.e., depression and generalized anxiety, neuroticism and depression) have been universal in concluding that the genetic influences common to depression and anxiety are so great as to make the disorders virtually indistinguishable at the genetic level (see Middledorp, Cath, Van Dyck, & Boomsma, 2005, for a recent review). Research has also shown that the structure of the genetic and environmental influences on psychopathology across the internalizing spectrum parallels the phenotypic structure (Kendler et al., 2003). Hettema et al. (2006) explicitly modeled the comorbidity between neuroticism and seven internalizing disorders using 9,000 twin pairs from the Virginia Twin Registry. They found that similar genetic factors underlie neuroticism and the latent liability to the internalizing spectrum, but environmental factors were largely uncorrelated. Neuroticism largely accounted for the comorbidity among the internalizing disorders, but there were genetic risk factors common to major depression, generalized anxiety disorder, and panic disorder not shared with neuroticism. Internalizing psychopathology is most likely a continuously distributed spectrum of liability to a certain type of pathology, and the specific constellation of symptoms that define a disorder result from this general overarching liability as well as disorder-specific influences (Krueger & Piasecki, 2002). Despite the strong evidence for a genetically coherent factor of internalizing, little research has examined the etiological connections between an internalizing phenotype and key environmental risk factors.
Marital Quality and Internalizing Spectrum Syndromes
As one of the most significant social forces in a person’s life, marriage has an important contextual role in the etiology and maintenance of psychopathology (Beach, Fincham, & Katz, 1998). Partners in conflict-laden marriages often exhibit behaviors like criticism, contempt, and defensiveness (Gottman, 1994), behaviors which are hallmarks of expressed emotion, a measure of family atmosphere that strongly predicts psychiatric relapse and poor response to treatment (Hooley, 2004). Following from the diathesis-stress model of psychopathology, there is theoretical and empirical evidence to suggest that conflict laden or unsatisfying marriages may act as an environmental stressor leading to the development of mental illness in vulnerable individuals (e.g., Beach, Katz, Kim, & Brody, 2003). However, others have suggested that marital distress is subsequent to, and a consequence of, psychopathology (Coyne, 1976). It is likely that both models are equally valid, although the direction of causality may differ by type of pathology.
Research strongly supports the phenotypic association between marital satisfaction and psychiatric disorders, particularly mood and anxiety disorders (Whisman & Uebelacker, 2003). Both large-scale epidemiological surveys (Goering, Lin, Campbell, Boyle, & Offord, 1996; Whisman, 1999; Whisman, 2007; Whisman, Sheldon, & Goering, 2000) and studies examining specific disorders (e.g., Markowitz, Weissman, Ouelette, Lish, & Klerman, 1989; McLeod, 1994; Whisman, 2001) show a clear and substantial link between psychiatric disorders and marital distress. Marital discord is also associated with subclinical levels of depression and anxiety and overall psychological distress (e.g., Barnett, Raudenbush, Brennan, Pleck, & Marshall, 1995; Fincham, Beach, Harold, & Osborne, 1997; Horowitz, McLaughlin, & White, 1998; Whisman, Uebelacker, & Weinstock, 2004). Finally, neuroticism is one of the strongest intrapersonal predictors of poor marital relationship quality and stability (see Karney & Bradbury, 1995, for a review).
Only recently have researchers begun to study marital quality, and the relationship between marital quality and other psychological phenomena, using genetically informative designs. Behavior genetics is an important area in which the analysis of relationship patterns, particularly marital quality, may aid in understanding the nosology and etiology of psychiatric dysfunction (Wamboldt & Reiss, 2006). In line with other work that finds moderate to substantial heritability of putatively “environmental” variables (Kendler & Baker, 2007; Rowe, 1981, 1983), Spotts and colleagues found moderate heritability of marital quality in both Swedish (Spotts et al., 2004b) and American (Spotts, Prescott, & Kendler, 2006) samples. Spotts et al. (2005a) showed that 32% of the total variance in wives’ marital satisfaction was shared in common with a personality composite of optimism and aggression, suggesting that genetically-influenced personality traits affect the establishment and maintenance of long-term romantic relationships. Spotts and colleagues have also found shared genetic influences between marital quality and well-being (Spotts et al., 2005b), and marital satisfaction and self-reported symptoms of depression (Spotts et al., 2004a).
One possibility that has not been extensively researched is that people with a genetic predisposition to internalizing psychopathology (i.e., a higher loading on the spectrum) will express that pathology in the face of difficult or troubling circumstances in their lives. This is a question of gene × environment interaction (G×E), also known as biometrical moderation, or genetic susceptibility to environmental stressors. In one example of this type of model, Heath, Eaves, and Martin (1998) found smaller effects of genetic influence on depression in married vs. unmarried women. Using a sample of female Australian twin pairs, they divided the sample into pairs concordant for a marriage-like partnership, concordant for no relationship, and discordant. The proportion of total variance in depression due to genetic influences increased from 29% in married twins to 51% in unmarried twins over 31 years of age. Marriage, therefore, acted as a protective factor by reducing the genetic liability to depressive symptoms. Surprisingly, there have been no studies since Heath et al. (1998) to expand on this interesting notion of the marital relationship as a protective factor in diminishing genetic influences.
Current Study
In the current study, we examine whether the comorbidity between symptoms of major depressive episode, generalized anxiety, panic attack, and ratings of neuroticism can be explained by a continuous underlying spectrum that is genetically influenced. Further, we were interested in whether this common internalizing spectrum could account for all genetic influences shared between the syndromes, or whether there would be genetic effects specific to each disorder. We then estimated the degree of genetic and environmental overlap between the internalizing spectrum and marital quality. Finally, we examined whether marital quality moderates the genetic and environmental influences on the internalizing spectrum. Evidence of significant moderation would suggest that the marital relationship may act as an environmental stressor that allows for the expression of a genetic predisposition to internalizing spectrum syndromes.
Method
Participants
Participants in the current study were drawn from the MacArthur Foundation Survey of Midlife Development in the United States (MIDUS), a nationally representative survey of persons age 25–74 years in the noninstitutionalized civilian population of the continental United States. The MIDUS study used telephone and mail questionnaires to assess variables related to physical health, psychological well-being, and social responsibilities. A subset of the larger MIDUS sample consists of 998 twin pairs (Kessler, Gilman, Thornton, & Kendler, 2004). To collect this twin sample, approximately 50,000 households were screened through telephone surveys to determine if any members of the household, or a relative, was a member of a twin pair. Respondents who agreed and met eligibility criteria were referred to the MIDUS recruitment process (see Kendler, Thornton, Gilman, & Kessler, 2000). All participants: 1) were administered a computer-assisted telephone interview that lasted approximately 45 minutes; and 2) completed two questionnaire booklets that they received in the mail which required an average of 1.5 hours to complete. Data collection procedures began in 1994 and lasted approximately 13 months, concluding in 1995.
The base MIDUS twin sample consists of 998 pairs. Zygosity was determined using self-report questions regarding information such as similarity of eye and hair color and degree to which others were confused as to their identity during childhood. Such techniques are generally more than 90% accurate (Lykken, Bouchard, McGue, & Tellegen, 1990); however, 16 pairs in this sample were not considered classifiable due to missing or indeterminate zygosity information. We also excluded 263 opposite-sex pairs from the full MIDUS twin sample, resulting in a sample of 719 pairs. Of the base sample of 1438 respondents (719 pairs), 69.75% were married, comparable to the percentage of married persons in the MIDUS main (non-twin) sample (see Marks, Bumpass, & Hun, 2004). We studied twin pairs who were concordant for being married at the time of data collection because marital quality was the focus of this research. This eliminated 435 individual respondents who were not married. We then eliminated 254 individuals for whom co-twin data was not available because of discordant marital status. This resulted in a final sample of 379 twin pairs: 99 monozygotic (MZ) male pairs, 102 MZ female pairs, 82 dizygotic (DZ) male pairs, and 96 DZ female pairs. The mean age of the sample was 45.8 (SD=12.03, range 25–74). Participants had been married an average of 23 years (SD=13, range=0–56).
Measures
Assessment of internalizing disorders
All diagnoses in the MIDUS study were based on a phone interview that used the Composite International Diagnostic Interview Short Form scales (CIDI-SF; Kessler, Andrews, Mroczek, Ustun, & Wittchen, 1998). The CIDI-SF is a fully structured diagnostic interview that assesses the 12-month prevalence of mental disorders based on DSM-III-R criteria (American Psychiatric Association, 1987). The CIDI-SF scales were developed based on analysis of the Composite International Diagnostic Interview questions in the National Comorbidity Survey. The MIDUS study assesses for the symptoms of three disorders included in the internalizing spectrum: major depressive episode (MD), generalized anxiety disorder (GAD), and panic disorder (PD). The CIDI-SF MDD, GAD, and PD assessments have good total classification accuracy (percentage of respondents whose CIDI-SF classification is the same as their classification of the full CIDI), with percentages of 93%, 99%, and 98%, respectively (Kessler et al., 1998a) and, in turn, the full CIDI instrument has good agreement with clinical diagnoses (Kessler et al., 1998b; Wittchen, 1994).
The CIDI-SF uses a stem-branch logic in which a small number of initial diagnostic stem questions are used in each section to skip-out people who are least likely to be cases before they are asked further symptom questions. For major depressive episode, participants meet the stem requirement by endorsing two weeks of depressed mood, at least most of the day, for at least almost every day, or endorsing two weeks of anhedonia, at least most of the day, for at least almost every day. If the participant endorses either of these stems, they are queried about additional depression symptoms, including feeling tired, change in weight, trouble with sleep, trouble concentrating, feeling down, and thoughts about death. The persons’s MDE score (0–7) is then calculated as the sum of the positive responses to each of these questions. The diagnostic stem requirement for generalized anxiety is met when the participant reports a period of feeling worried, tense, or anxious that lasted at least six months. The CIDI-SF also assesses for panic attacks, not panic disorder per se, because the time-frame for the interview could not specifically evaluate the DSM-III-R criteria that either four panic attacks occur within a 4-week period or that one or more panic attacks are followed by a 4-week period of persistent fear of having another panic attack.
Assessment of neuroticism
The MIDUS survey’s self-administered mailed questionnaire included a personality measure based on the Five Factor Model (FFM) of personality (Lachman & Weaver, 1997). For the current study, we make use of the Neuroticism scale (α = .75). Respondents were asked to rate themselves on four adjectives: ‘moody,’ ‘worrying,’ ‘nervous,’ and ‘calm’ (reverse scored). Adjectives were rated on a scale of 1–4 indicating “how well each of the following describes you: a lot, some, a little, not at all,” with 1 signifying “a lot.” The neuroticism scale was constructed by calculating the mean across these items.
Assessment of marital quality
The current study used an overall marital quality score that was based on items which assessed the quality of the marital relationship in different areas. Two items used in a large national survey (National Survey of Families and Households) assessed the risk for separation or divorce (e.g., During the past year, how often have you thought your relationship might be in trouble?). Three items commonly used in national surveys (e.g. National Survey of Families and Households; National Longitudinal Survey of Labor Market Experiences) measured the level of disagreement between the participant and her or his spouse regarding money matters, household tasks, and leisure time activities (e.g., How much do your and your spouse disagree on money matters, such as how much to spend, save or invest?). The amount of empathy and level of criticism the respondent received from his or her spouse were each measured by six items adapted from Schuster, Kessler, and Aseltine (1990) (e.g., How much does your spouse really care about you?, How often does your spouse make too many demands on you?). Finally, four items assessed the quality of decision making between the participant and his or her spouse (e.g., My partner and I are a team when it comes to making decisions). Items were summed to create a total quality score, with higher scores indicating higher relationship quality. The internal reliability of this overall scale was excellent (α=.94). For more information on the construction of these items, their reliability, and validity, see Bookwala (2005) and Grzywacz and Marks (2000).
Biometric Analysis
Biometric modeling was utilized to evaluate the genetic and environmental moderation of internalizing pathology by marital quality. This type of modeling makes use of twin methodology and structural equation modeling to estimate how much of the variance in a trait (phenotype) is due to additive genetic effects (A), common environmental influences (C), and unique environmental influences (E). The standard univariate “ACE” model assumes that the A, C, and E components are fixed over the entire population from which the sample is drawn. In other words, there is no provision for the association between the genetic and environmental influences on internalizing pathology and any other trait.
To test our hypothesis that the genetic and environmental influences on internalizing pathology differ as a function of marital quality, we needed to utilize a model that allowed the variance components of internalizing to vary as a function of marital quality. This type of analysis has been referred to as a test of “gene-environment interaction,” or the notion that different environments can lead to different genetic expression of a phenotype. However, this term does not completely describe the nature of the effects we examined. In the current study, neither the moderator variable, marital quality, nor the dependent variable, internalizing pathology, are wholly “environmental” or wholly “genetic.” The advantage of the model that we utilize is that it is possible to decompose the moderator variable into its genetic and environmental variance components, and test for gene-environment interaction in the presence of gene-environment correlation (Purcell, 2002). A genetic correlation is the amount of overlap in the genetic influences on two phenotypes and ranges from −1 to +1; similar types of correlations (i.e., overlap) can occur for shared and nonshared environmental influences. Therefore, we will use the more accurate term “biometrical moderation” to refer to the analyses conducted in these studies; this term better captures the goal of this study—to determine whether the magnitude of genetic and environmental influences on internalizing pathology depends on marital quality (gene-environment interaction), and the extent to which influences acting on internalizing pathology also exerted influences on marital quality (gene-environment correlation).
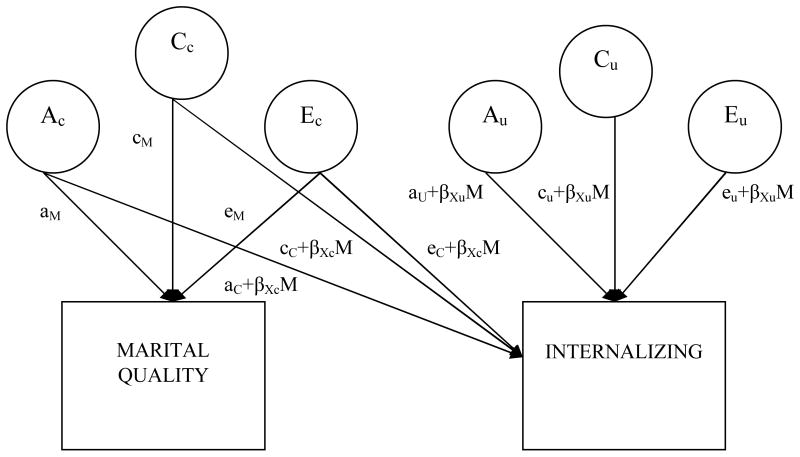
Figure 1 presents a path model of the biometric moderation model used in this study. This model is an extension of the bivariate (Cholesky) decomposition model, which is used to compute the genetic and environmental influences that are shared between two variables. In the moderation model, the variable being moderated (here, internalizing pathology) is the downstream variable in the model. There are two sets of paths contributing genetic and environmental influences: those common to internalizing and the moderator (marital quality), and those unique to internalizing. The paths from the moderator (M) variable to the dependent variable are linear functions of the form a + βM, where a is the parameter for genetic influence on the variable, β is a regression coefficient, and M is the level of the moderator variable. The total phenotypic variance in Internalizing can be calculated by squaring and summing all of the paths leading to it: P2= (aC+βXcM)2 + (aU+βXuM) 2 + (cC+βXcM)2 + (cU+βXuM)2 + (eC+βXcM) 2 + (eU+βXuM) 2.
Figure 1.
Path diagram of a biometrical moderation model with Marital Quality moderating the genetic and environmental influences on a general Internalizing factor (model is shown for only one member of the twin pair). The latent variables Ac, Cc, and Ec represent the additive genetic, shared (common) environmental, and non-shared (unique) environmental variance in Marital Quality and any of the variance that is shared between Quality and Internalizing. Variables Au, Cu, and Eu represent any residual variance in Internalizing after accounting for Quality. Each of the paths impacting Internalizing is a linear function that combines 1) an overall coefficient separate from the moderator variable (e.g., ac) that indicates the magnitude of each effect of A, C, or E on Internalizing, and 2) the product of a coefficient that indexes the moderation of Internalizing by Quality (βXc) multiplied by the level of the moderator (Quality). The total phenotypic variance in Internalizing can be calculated by squaring and summing all of the paths leading to it: P2= (aC+βXcM)2 + (aU+βXuM)2 + (cC+βXcM)2 + (cU+βXuM)2 + (eC+βXcM) 2 +(eU+βXuM) 2.
Biometric models were fit to the raw data using the Mx software system (Neale, Boker, Xie, & Maes, 2003). For ease of interpretation, the Internalizing variable was reversed to be positively correlated with the marital quality scale (with higher scores corresponding to greater Quality). To correct for potential biases in model fitting, the internalizing and marital relationship scales were adjusted for effects of age and gender (McGue & Bouchard, 1984). Each scale was regressed on age, age2, age × gender, and age2 × gender, and the standardized residuals from these regressions were used in subsequent analyses. Because not all participants had both internalizing and relationship data, we used full-information maximum-likelihood with the raw data, a procedure that was also necessary for the moderated biometric models we were using. Fit of the moderation models were judged relative to the fit of a bivariate “no moderation” model in which the six moderation parameters (βXc and βXu for A, C, and E) were fixed at zero (so that aC+βXcM became aC + (0*M) = aC).
Two indices were used to evaluate model fit: (1) the likelihood-ratio test (LRT; distributed as χ2, and computed as the difference in the −2 log-likelihood values for the two models); and (2) the Akaike Information Criterion (AIC; Akaike, 1987). The LRT is used as a goodness-of-fit index, representing the degree of fit between model expectations and observed data. Improvements in the model’s fit, from adding or omitting parameters, can be assessed by a statistically significant change in LRT. Akaike’s Information Criterion (AIC; Akaike, 1987) is also conventionally used to compare the fit of alternative models. The AIC statistic considers goodness of fit while penalizing over-parameterization. Because the aim of model fitting is to explain the data as parsimoniously as possible, the model with the lowest AIC value is generally considered best (Markon & Krueger, 2004).
Results
Structure of the Internalizing Spectrum
We first conducted a confirmatory factor analysis in Mplus (Muthén & Muthén, 2004) to determine whether the phenotypic structure of the internalizing spectrum disorders could be accounted for by one latent factor. Raw data, in the form of symptom counts for depression, generalized anxiety, and panic attacks, and the scale score for neuroticism, were fit to a one-factor model using a weighted least squares estimator with a mean- and variance-adjusted chi-square test statistic (WLSMV) to account for the non-normality of the data. No participants were missing data on the symptom count variables. For neuroticism, 36 participants were missing data; these missing values were handled by substituting the mean of the variable in SPSS before conducting the factor analysis in Mplus. The metric of the factor was defined by setting the loading for depression symptoms to 1.0. The factor loadings for the remaining indicators, the error variances, and the factor variance were all freely estimated, and all error covariances were fixed to 0.
The χ2 (2) for the one-factor model was 7.48, p = .02. However, because evaluation of nested models with chi-square values was not relevant to the analyses, overall goodness of fit of the model was evaluated using root mean square error of approximation (RMSEA), comparative fit index (CFI), the Tucker-Lewis index (TLI), and the weighted root mean residual (WRMR). According to Hu and Bentler (1999), acceptable model fit was defined by: RMSEA ≤.06, CFI ≥ .95, and TLI ≥.95 or greater. For our one-factor solution, RMSEA was .06 and CFI was .97, indicating reasonably good fit. The TLI of .91 was somewhat low, but still in the range indicative of acceptable model fit (Bentler, 1990). The WRMR was .98, less than the cut-off value of 1.0 which has previously been shown to provide an acceptable error rate (Yu, 2002). The overall fit of the one-factor model was also supported by an absence of any localized areas of strain. None of the standardized residuals from the model were larger than 1.0 (as these are roughly equivalent to z-scores, a value of 1.96 is often used as a marker of statistical significance at p<.05). Standardized factor loadings of each of the individual internalizing syndromes are given in Table 1. All freely estimated unstandardized factor loadings were statistically significant (ps < .001). As shown, generalized anxiety had the strongest loading on the internalizing factor, followed by depression, panic attack, and neuroticism. Factor scores were extracted from Mplus and used in the biometrical analyses described below. The total Marital Quality score was significantly associated with the Internalizing factor score (r = −0.28, p < .01).
Table 1.
Descriptives, Factor Analysis Loadings for Internalizing Syndromes, Twin Correlations, and Standardized Variance Components for Internalizing Syndromes
| Descriptives
|
Internalizing Factor Loading
|
Twin Correlations
|
||||
|---|---|---|---|---|---|---|
| Variable | M | SD | Range | MZ | DZ | |
| Marital Quality | 80.27 | 11.79 | 24–97 | -- | .29** | .02 |
| Internalizing | .04 | .39 | −.50–1.57 | -- | .37** | .27** |
|
|
|
|||||
|
Raw Scores
|
Residual Scores
|
|||||
| Depression | .61 | 1.69 | 0–7 | .65 | .11 | .05 |
| Generalized Anxiety | .06 | .55 | 0–9 | .77 | −.06 | .03 |
| Panic Disorder | .29 | .98 | 0–6 | .59 | −.05 | −.15* |
| Neuroticism | 2.20 | .65 | 1–4 | .39 | .23** | .04 |
Note. N=758.
p<.01,
p<.001. Residuals=Twin correlations for Depression, Generalized Anxiety, Panic Disorder, and Neuroticism after regressing out Internalizing factor score.
Genetic and Environmental Influences on Specific Internalizing Syndromes
We next turned to examining the specific genetic and environmental influences on each of the internalizing syndromes to determine which etiological factors contribute to differences between the observed phenotypes. We constructed a residual score from a regression equation predicting each of the individual syndromes from the total internalizing factor score (e.g., the residual of a regression equation predicting depression from internalizing). We then examined the MZ and DZ twin correlations for each of these four residual scores (see Table 1). Of note, almost all twin correlations were small and non-significant (MZ correlations were .11, −.06, and −.05 for depression, generalized anxiety, and panic attack, respectively; corresponding DZ correlations were .05, .03, −.15). These findings suggest strong etiologic overlap among the symptoms of these disorders, and argue against any familial (genetic or shared environmental) influences specific to each of the individual syndromes. The unique variance in the symptoms of each disorder were largely due to non-shared environmental effects or error in the psychometric sense (i.e., unique idiosyncratic variation in a variable that does not correlate with other variables). The only significant correlations were the residual scores for neuroticism net of internalizing; MZ correlations were .23, while DZ correlations were .04. This indicates that there are genetic effects on neuroticism that are unique to the trait and not shared in common with the overall internalizing factor.
Bivariate Biometrical Modeling of the Internalizing Spectrum and Marital Quality
Having established an etiologically coherent internalizing factor, we examined whether there was overlap in the genetic and environmental influences on this factor and marital relationship quality. The MZ twin correlation for Internalizing was .37, more than the DZ correlation of .27 but still less than twice as much (see Table 1). This indicates that genetic influences are important in the variance of Internalizing, but also implicates shared environmental effects. We ran a bivariate decomposition (Cholesky) model for marital quality and internalizing. As shown in Table 2, the heritability (proportion of total variance due to genetic effects) of internalizing was 24%, while proportion of variance due to shared family environment was 13% and the amount attributable to non-shared environmental effects was 62%. The genetic correlation between Marital Quality and Internalizing was 1.00, indicating that the genetic contributions to Marital Quality perfectly overlap with the genetic influences on the Internalizing spectrum. (Shared environmental factors (C) are not a substantial contributor to the etiology of Marital Quality, so the rC correlations of 1.0 are not useful to interpret, as they represent correlations between trivial variance components. These are presented simply for the sake of completeness). The non-shared environmental correlation between Marital Quality and Internalizing was −.02; thus, even though unique environmental influences weigh heavily in the etiology of both Marital Quality and Internalizing, the environmental influences important for each phenotype do not overlap.
Table 2.
Estimates of Unstandardized and Standardized Variance Components and Genetic and Environmental Correlations between Internalizing and Marital Quality
| Variance components | Total Phenotypic Variance | Proportions of variance | Correlations | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | C | E | A(%) | C(%) | E(%) | rA | rC | rE | |||
| Bivariate Decomposition (Cholesky) | |||||||||||
| Marital Adjustment | .22 | .01 | .68 | .91 | .25 | .01 | .75 | -- | -- | -- | |
| Internalizing | .24 | .13 | .62 | 1.00 | .24 | .13 | .62 | 1.00 | 1.00 | −.02 | |
| No Moderation Model | |||||||||||
| Marital Adjustment | .23 | .01 | .68 | .92 | .25 | .01 | .74 | -- | -- | -- | |
| Internalizing | .22 | .19 | .61 | 1.01 | .21 | .19 | .60 | 1.00 | 1.00 | .00 | |
| Moderation Model | |||||||||||
| Marital Adjustment | .23 | .01 | .68 | .92 | .26 | .01 | .74 | -- | -- | -- | |
| Internalizing at Level of Marital Score | −2 | .45 | .05 | 1.05 | 1.55 | .29 | .03 | .68 | 1.00 | 1.00 | −.08 |
| −1 | .30 | .11 | .80 | 1.21 | .25 | .09 | .66 | 1.00 | 1.00 | −.04 | |
| 0 | .18 | .20 | .58 | .97 | .19 | .21 | .60 | 1.00 | 1.00 | .01 | |
| 1 | .10 | .32 | .40 | .82 | .12 | .39 | .49 | 1.00 | 1.00 | .08 | |
| 2 | .04 | .46 | .26 | .76 | .05 | .61 | .34 | 1.00 | 1.00 | .18 | |
Note. A=unstandardized genetic variance component; C=unstandardized shared environmental variance component; E=unstandardized nonshared environmental variance component; A(%)=standardized genetic variance proportion; C(%)=standardized shared environmental variance proportion, E(%)=unstandardized shared environmental variance proportion; rA=genetic correlation, rC=shared environmental correlation; rE=non-shared environmental correlation.
Biometric Moderation Analysis
We next tested whether Marital Quality moderated the genetic and environmental influences on Internalizing pathology. Ultimately, our goal was to test the full moderation model with all moderation paths freely estimated, as shown in Figure 1. As a baseline model of the etiological influences common to Marital Quality and Internalizing, we ran a no-moderation model in which the moderation parameters were fixed to 0 (−2lnL=3761.34, df=1377, AIC=1007.34). Variance components and genetic and environmental correlations from this no-moderation model are presented in Table 2. Of note, the no-moderation model is essentially equivalent to a bivariate decomposition (Cholesky) model, but differs in the degrees of freedom and −2 log likelihood due to the data entry method required for the moderation model (the moderator variable is entered twice). From the baseline, no-moderation model, we added each of the six moderation paths (the path common to both Marital Quality and Internalizing, and the path unique to Internalizing, for genetic, shared environmental, and unique environmental influences) one at a time. For five of the six moderation parameters, the model with the moderation parameter provided a significantly better fit than the baseline, no-moderation model, as shown in the difference in log likelihood value and smaller AIC values (see Table 3). Concurrently, the confidence intervals around the moderation parameter were significant for the same five models (see Table 4). Only the moderation parameter on the common E path was not a significant improvement over the no-moderation model.
Table 3.
Fit Statistics From the Biometrical Moderation Models of Marital Quality and Internalizing Psychopathology
| Model | −2lnL | df | Δχ2 | Δdf | p | AIC |
|---|---|---|---|---|---|---|
| No Moderation | 3761.34 | 1377 | 1007.34 | |||
| Only A common Moderation | 3754.25 | 1376 | 7.09 | 1 | .008 | 1002.25 |
| Only A unique Moderation | 3752.57 | 1376 | 8.77 | 1 | .003 | 1000.57 |
| Only C common Moderation | 3753.33 | 1376 | 8.00 | 1 | .005 | 1001.33 |
| Only C unique Moderation | 3754.24 | 1376 | 7.09 | 1 | .008 | 1002.24 |
| Only E common Moderation | 3760.84 | 1376 | 0.49 | 1 | .483 | 1008.84 |
| Only E unique Moderation | 3741.41 | 1376 | 19.93 | 1 | .000 | 989.41 |
| Five Parameter Moderation (all but E common) | 3739.78 | 1372 | 21.55 | 5 | .001 | 995.78 |
| ACE Full Moderation | 3738.92 | 1371 | 22.42 | 6 | .001 | 996.92 |
Note. −2lnL = −2 log likelihood; df = degrees of freedom; AIC = Akaike’s Information Criterion.
Table 4.
Path Estimates and 95% Confidence Intervals for the Moderation Models of Internalizing Pathology by Marital Quality
| Am | Ac | Au | Amc | Amu | Cm | Cc | Cu | Cmc | Cmu | Em | Ec | Eu | Emc | Emu | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No Moderation | .48 | .46 | .00 | -- | -- | .09 | .43 | .00 | -- | -- | .82 | .00 | .78 | -- | -- |
| 95% CI | .23, .60 | .11, .70 | −.49, .49 | −.38, .38 | −.63, .63 | −.50, .50 | .76, .90 | −.09, .10 | .71, .85 | ||||||
| Only A common Moderation | .38 | .49 | .00 | −.15 | -- | .24 | .27 | .28 | -- | -- | .85 | −.03 | .76 | -- | -- |
| 95% CI | −.03, .58 | .12, .71 | −.46, .46 | −.03, −.36 | −.48, .48 | −.60, .60 | −.49, .49 | .77, .93 | −.13, .12 | .70, .83 | |||||
| Only A unique Moderation | .46 | .37 | −.26 | -- | .23 | .14 | .43 | .00 | -- | -- | .83 | .03 | .75 | -- | -- |
| 95% CI | .17, .59 | −.03, .63 | −.51, ’−.02 | .08, .38 | −.40, .40 | −.62, .62 | −.48, .48 | .76, .90 | −.07, .14 | .69, .82 | |||||
| Only C common Moderation | .47 | .44 | .00 | -- | -- | .12 | .28 | .32 | −.21 | -- | .83 | .00 | .76 | -- | -- |
| 95% CI | .27, .59 | .10, .64 | −.49, .49 | −.08, .34 | −.02, .62 | −.50, .50 | −.37, −.05 | .76, .90 | −.10, .10 | .69, .84 | |||||
| Only C unique Moderation | .47 | .42 | .00 | -- | -- | .11 | .41 | −.19 | -- | .23 | .83 | .02 | .76 | -- | -- |
| 95% CI | .21, .59 | .01, .66 | −.47, .47 | −.38, .38 | −.62, .62 | −.50, .06 | .05, .38 | .76, .90 | −.08, .13 | .69, .83 | |||||
| Only E common Moderation | .48 | .48 | .00 | -- | -- | .09 | .43 | .00 | -- | -- | .82 | .01 | .78 | .02 | -- |
| 95% CI | .25, .60 | .13, .71 | −.49, .49 | −.38, .38 | −.62, .62 | −.50, .50 | .76, .90 | −.09, .12 | .71, .85 | −.04, .08 | |||||
| Only E unique Moderation | .48 | .42 | .00 | -- | -- | .10 | .47 | .00 | -- | -- | .83 | .02 | .77 | -- | −.13 |
| 95% CI | .22, .60 | .05, .67 | −.49, .49 | −.39, .39 | −.64, .64 | −.53, .53 | .76, .90 | −.08, .12 | .71, .84 | −.20, −.07 | |||||
| Five Parameter Moderation (all but E common) | .47 | .41 | .00 | −.06 | .00 | .11 | .44 | .14 | .04 | .13 | .83 | .01 | .76 | -- | −.14 |
| 95% CI | .17, .59 | .02, .66 | −.48, .48 | −.23, .15 | −.31, .31 | −.40, .40 | −.63, .63 | −.51, .51 | −.32, .32 | −.34, .34 | .76, .90 | −.10, .12 | .69, .84 | −.22, −.06 | |
| ACE Full Moderation | .48 | .43 | .00 | −.12 | .00 | .09 | .45 | .00 | .12 | .00 | .82 | .01 | .76 | .04 | −.13 |
| 95% CI | .20, .60 | .05, .66 | −.47, .47 | −.28, .12 | −.29, .29 | −.40, .40 | −.63, .63 | −.51, .51 | −.31, 31 | −.32, .32 | .76, .90 | −.09, .11 | .69, .83 | −.05, .13 | −.21, −.05 |
Note. Am=genetic path estimate for marital quality; Ac=genetic path estimate from marital quality to internalizing; Au=genetic path estimate unique to internalizing; Amc=moderator of genetic path from marital quality to internalizing; Amu=moderator of genetic path to internalizing; Cm=shared environmental path estimate for marital quality; Cc=shared environmental path estimate from marital quality to internalizing; Cu=shared environmental path estimate unique to internalizing; Cmc=moderator of shared environmental path from marital quality to internalizing; Cmu=moderator of shared environmental path to internalizing; Em=non-shared environmental path estimate for marital quality; Ec=non-shared environmental path estimate from marital quality to internalizing; Eu=non-shared environmental path estimate unique to internalizing; Emc=moderator of non-shared environmental path from marital quality to internalizing; Emu=moderator of non-shared environmental path to internalizing.
We then compared the full moderation model with all parameters freely estimated (−2 log likelihood = 3738.92, AIC = 996.92, df=1371), and a moderation model with the five significant moderation paths (−2 log likelihood = 3739.78, AIC = 995.78, df=1372), to the no-moderation model. When compared to the no-moderation model, both moderation models resulted in significantly better fit. The full moderation model resulted in a slightly better −2 log likelihood value, while the five parameter moderation model had a slightly better AIC value. Thus, given the almost equal fit of the two models, we chose the full moderation for its ability to provide the fullest picture of the change in the etiology of Internalizing as a function of the level of Marital Quality. Of note, in the final model, the confidence intervals around five of the six moderation parameters included zero, and were thus not statistically significant in the p-value sense (see Table 4). Nevertheless, as a set, these parameters are important to include in the model, because the full moderation model fit better than a model with no moderation (No Moderation AIC=1007.34, whereas Moderation AIC = 996.92).
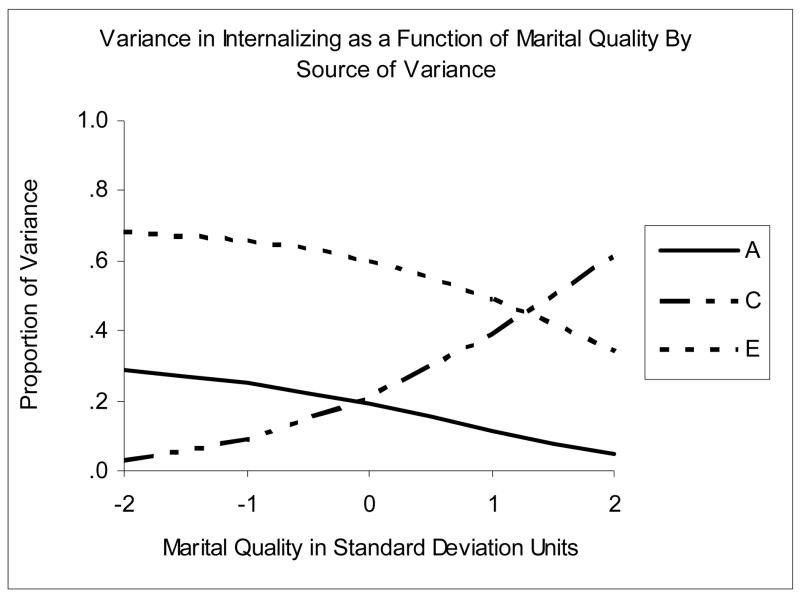
Figure 2 illustrates the change in the standardized variance components for Internalizing from the full moderation model with Marital Quality. As shown, the standardized variance components for Internalizing vary as functions of Marital Quality (shown as z-scores from −2 to +2). As Marital Quality increased, genetic effects and non-shared environmental effects decreased in importance in the etiology of Internalizing, whereas shared environmental effects increased in importance.
Figure 2.
Proportions of Variance in Internalizing as a function of Marital Quality total score. A=standardized genetic variance, C=standardized shared environmental variance, E=standardized nonshared environmental variance.
Table 2 presents the variance components of Internalizing at five different discrete levels, scaled in standard deviation units (z-scored): −2, −1, 0, 1, and 2 standard deviations away from the mean of the moderator. The unstandardized genetic component of variance decreased from low to high levels of Quality; because the total phenotypic variance in Internalizing also decreased from low to high levels of Quality, the heritability of Internalizing was greatest when Quality was lowest. At the extreme low end of Quality, the proportion of variance in Internalizing due to genetic effects was 29%, while there were essentially no genetic effects on Internalizing at high levels of Quality (h2=5%). Similarly, non-shared environmental effects were strongest at low levels of Quality (e2=68%) and decreased as relationship quality became more positive. In contrast, shared environmental influences were weakest at low levels of Quality (c2=3%) and increased linearly with level of Quality, until, at the highest levels of Quality, a majority of the variance in Internalizing was due to shared environmental influences (c2=61%). Examination of the genetic correlations between Internalizing and Marital Quality showed perfect overlap (ra=1.0) across the level of Quality. The genetic influences on the Internalizing spectrum were the same genetic influences on Marital Quality at every level of Quality. There was an increasing association between the non-shared environmental influences on Marital Quality and Internalizing from low to high levels of Quality (see rE in Table 2). The non-shared environmental correlation between Quality and Internalizing increased from rE = −0.08 at low levels of Quality to rE = 0.18 at high levels of Quality.
Discussion
Internalizing syndromes often co-occur with social and interpersonal difficulties, particularly poor marital quality. In the current study, we examined possible mechanisms behind the frequent co-occurrence of poor relationship quality and internalizing syndromes. Specifically, we evaluated whether the genetic and environmental influences on an internalizing factor score vary as functions of the level of marital quality. Findings from the current study support the existence of an etiologically coherent, moderately heritable internalizing spectrum that accounts for the phenotypic co-occurrence among the internalizing syndromes. After accounting for the general internalizing factor, there were no disorder-specific genetic influences, suggesting that phenotypic internalizing disorders (e.g., depression) are all possible expressions of the same genetically-influenced latent liability, with specific manifestation dependent on environmental stressors.
In line with previous research (Spotts et al., 2004a; Spotts et al., 2005b), we found overlap between the genetic influences on marital quality and mental health, represented here by a factor of internalizing pathology. This finding may support a directional link in which internalizing pathology leads to disrupted marital relations. Conversely, it might indicate that an underlying personality dimension or temperament, perhaps of high negative affectivity, influences both internalizing pathology and the quality of the marital relationship. For instance, a person with a predisposition toward higher levels of negative affect or neuroticism may evoke negative reactions from his or her spouse, which may then trigger an internalizing syndrome disorder. In contrast to research that found overlapping non-shared environmental influences shared between marital quality and well-being and depression (Spotts et al., 2004a; Spotts et al., 2005b), we found virtually no unique environmental influences common to marital quality and internalizing pathology. The finding that these two variables are connected solely through genetic influences common to both is strong support for the influence of a distress- and worry-prone personality that contributes to disrupted marital relationship and an internalizing disorder.
When we examined biometrical moderation of internalizing psychopathology by marital quality, a more complex picture emerged, detailing the contribution of genetic and environmental influences on internalizing as functions of marital relationship quality. Specifically, genetic influences were of greater importance in the etiology of the internalizing spectrum where levels of marital quality were low. These results suggest that adults with a genetic liability to internalizing spectrum syndromes may be at greater risk of developing symptoms when they are in an unsatisfying marriage. Considering only the static parameter estimates from a no-moderation bivariate model, the etiology of internalizing appeared largely to be due to substantial non-shared environmental influences and similar modest contributions from genetic and shared environmental factors. From the moderation models, we see that people at the extreme low end of marital quality reported a level of internalizing that reflects a genetic sensitivity to pathology. Both the total phenotypic variance and the heritability of internalizing were generally highest at low levels of Quality. Thus, it seems that being low in positive relationship quality allows for the expression of a genetic predisposition to internalizing symptoms.
One intriguing finding from this study that deserves further discussion is the substantial influence of shared environmental effects on the internalizing spectrum. Common environmental influences, particularly in adult samples, have been notoriously difficult to document (Turkheimer, 2000). Standard biometrical modeling on most psychological phenotypes of interest finds that eliminating shared environmental effects from the model does not appreciably decrease model fit. Yet, we found moderate common environmental influences even in the standard, no-moderation model; the biometrical moderation models found an even greater impact of shared environment at the extreme high end of quality. For those with the most positive marital relationships, the majority of the variance in the internalizing spectrum is due to environmental factors shared in common with family members. A possible interpretation of this finding is that a person who develops an internalizing syndrome, even in the context of a fulfilling and satisfying marriage, may have developed poor problem-solving and stress-reducing habits in the context of the childhood home they shared with their siblings – habits that continue into adulthood.
Limitations
There are several potential limitations of this study that may affect the interpretation and generalizability of our findings. First, all information came from the self-report of the participant, which is subject to mood-state distortions; it is possible that elevated feelings of negative affect or negative feelings toward one’s spouse biased the participants responses to the measures. It will be important to replicate these findings with spouse, observer, or laboratory based measures of marital quality and informant or clinician report of pathology. We must suggest that, given the notable confidence intervals around the moderation parameters in the final model, these results should be replicated in future studies.
Our findings in this study should also be interpreted in light of the specific measures used to assess for the constructs of interest. Symptoms of the three psychiatric syndromes assessed in the MIDUS study, MDD, GAD, and PD, were measured with the CIDI-SF (Kessler et al., 1998). This is a well-validated measure that shows good sensitivity and specificity in comparison to the full Composite International Diagnostic Interview (Kessler et al., 1998). It is, however, a lay-administered diagnostic interview that may not adequately capture the presence of absence of a symptom in the same way that a clinician or more extensive inventory might. Further, the stem-branch structure of the interview may result in failing to capture the presence of associated symptoms in the absence of depressed mood or anhedonia. However, given that the stem questions—which must be endorsed to trigger assessment of the other symptoms—are the defining features of the disorders (i.e., DSM requires depress mood or anhedonia for a diagnosis of depressive episode), the CIDI-SF is most likely capturing the true variation in the internalizing syndromes as they exist in nature. Finally, the diagnostic interview only assessed for 12-month, not lifetime, prevalence, and thus may have failed to adequately capture the full extent of pathology in this sample.
Another possible limitation in the current study is the assessment of the personality trait of neuroticism. Even though the measure of neuroticism utilized here is based on several well-known trait scales (e.g., Goldberg, 1992; John, 1990; Trapnell & Wiggins, 1990), it consisted of only four single-word adjectives, and may not only underrepresent the construct of neuroticism but also be prone to mood-state distortion. We are confident, however, that there are several reasons why this is unlikely to be the case. First, it has been suggested that different measurement formats of the FFM (e.g., adjectives vs. full statements) are basically equivalent (John, 1990). Second, the particular FFM measure has been used successfully in other MIDUS research (e.g., Plant, Markus, & Lachman, 2002; Staudinger, Fleeson, & Baltes, 1999). Third, neuroticism as a structurally and etiologically coherent structure was clearly revealed in phenotypic and genetic factor analyses using the same base twin sample as used in the current study (Johnson & Krueger, 2004).
Finally, we must make note of limitations to the data analysis of this study. With the availability of only four indicators, the current analyses offered a relatively weaker test of the latent structure of the internalizing disorders. Specifically, the measurement model was over-identified by only two degrees of freedom, and without additional indicators of a possible, second factor (e.g., Hettema et al., 2006), viable alternative models could not be pursued. Further, because of the specifics of the biometric moderation model that we utilized in this study, we did not make use of opposite-sex twin pairs or twin pairs where one of the two twins was missing data on the moderator variable. Hopefully, future improvements in this model will eliminate these reductions in sample size.
Summary
The results of the current study mesh well with previous genetically informative research on marital satisfaction. We replicated previous work that found moderate estimates of heritability for marital quality (Spotts et al., 2004b; Spotts et al., 2006). In many ways, it is not surprising that there are genetic effects on an “environmental” variable. There are now numerous studies that document genetic influences on measures of family environment (see Kendler & Baker, 2007, for a recent review). One hypothesis that has been substantiated in several studies is that genetic effects on environmental variables are due to personality traits (Chipuer, Plomin, Pedersen, McClearn, & Nesselroade, 1993; Krueger, Markon, & Bouchard, 2003; South, Krueger, Johnson, & Iacono, 2007). In the only study to examine genetic and environmental overlap between marital quality and personality, there were significant genetic correlations between marital satisfaction and a personality composite of optimism and aggression (Spotts et al., 2005a). Here we extend this work to show that genetic effects on marital quality are shared in common with the internalizing spectrum, which includes a neurotic personality style. Hopefully this will stimulate future research into how marital relationships, and other interpersonal relationships, can act as an environmental stressor that allows for the expression of psychopathology for those with an inherited vulnerability.
Acknowledgments
This research was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development and by a grant from the National Institute on Aging (#AG20166).
Footnotes
It is reasonable to wonder about the direction of this effect. Certainly the causal direction between marital satisfaction and psychopathology at the phenotypic level is not clear, with evidence that poor relationship quality precedes the onset and exacerbation of major mental illness (Beach & O’Leary, 1993; Whisman, 1999) and that psychopathology precedes marital dysfunction (Whisman et al., 2004). It is possible that the internalizing spectrum also moderates the genetic and environmental influences on marital quality. We examined this question by reversing our models to determine if the genetic and environmental influences on marital quality would change as functions of levels of internalizing. For total Marital Quality, the moderation model was a significant improvement in fit over the no-moderation model (χ2=16.60, df=6, p<.05, ΔAIC=4.60). Genetic influences on marital quality were greater at high levels of internalizing, common environmental influences increased at low levels of internalizing, and unique environmental influences were fairly static across the level of internalizing. That moderation was significant in both directions for marital quality and internalizing suggests mutually reinforcing effects between positive relationship quality and the internalizing spectrum.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at http://www.apa.org/journals/abn/
References
- Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. Washington, D.C.: American Psychiatric Press; 1987. [Google Scholar]
- Barnett RC, Raudenbush SW, Brennan RT, Pleck JH, Marshall NL. Change in job and marital experiences and change in psychological distress: A longitudinal study of dual-earner couples. Journal of Personality and Social Psychology. 1995;69:839–850. doi: 10.1037//0022-3514.69.5.839. [DOI] [PubMed] [Google Scholar]
- Battaglia M, Przybeck TR, Bellodi L, Cloninger RC. Temperament dimensions explain the comorbidity of psychiatric disorders. Comprehensive Psychiatry. 1996;37:292–298. doi: 10.1016/s0010-440x(96)90008-5. [DOI] [PubMed] [Google Scholar]
- Beach SRH, Fincham FD, Katz J. Marital therapy in the treatment of depression: Toward a third generation of therapy and research. Clinical Psychology Review. 1998;18:635–661. doi: 10.1016/s0272-7358(98)00023-3. [DOI] [PubMed] [Google Scholar]
- Beach SRH, Katz J, Kim S, Brody G. Prospective effects of marital satisfaction on depressive symptoms in established marriages: A dyadic model. Journal of Social and Personal Relationships. 2003;20:355–371. [Google Scholar]
- Beach SR, O’Leary KD. Marital discord and dysphoria: For whom does the marital relationship predict depressive symptomatology? Journal of Social and Personal Relationships. 1993;10:405–420. [Google Scholar]
- Bentler PM. Comparative fit indices in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bienvenu OJ, Brown C, Samuels JF, Liang KY, Costa PT, Eaton WW, Nestadt G. Normal personality traits and comorbidity among phobic, panic, and major depressive disorders. Psychiatry Research. 2001;102:73–85. doi: 10.1016/s0165-1781(01)00228-1. [DOI] [PubMed] [Google Scholar]
- Bookwala J. The role of marital quality in physical health during the mature years. Journal of Aging and Health. 2005;17:85–104. doi: 10.1177/0898264304272794. [DOI] [PubMed] [Google Scholar]
- Chipuer HM, Plomin R, Pedersen NL, McClearn GE, Nesselroade JR. Genetic influence on family environment: The role of personality. Developmental Psychology. 1993;29:110–118. [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D, Mineka S. Temperament, personality and the mood and anxiety disorders. Journal of Abnormal Psychology. 1994;103:103–116. [PubMed] [Google Scholar]
- Coyne JC. Toward an interactional description of depression. Psychiatry: Journal for the Study of Interpersonal Processes. 1976;39:28–40. doi: 10.1080/00332747.1976.11023874. [DOI] [PubMed] [Google Scholar]
- Farone SV, Tsuang MT, Tsuang DW. Genetics of mental disorders. New York: The Guilford Press; 1999. [Google Scholar]
- Fincham FD, Beach SRH, Harold GT, Osborne LN. Marital satisfaction and depression: Different causal relationships for men and women? Psychological Science. 1997;8:351–357. [Google Scholar]
- Goering P, Lin E, Campbell D, Boyle MH, Offord DR. Psychiatric disability in Ontario. Canadian Journal of Psychiatry. 1996;41:564–571. [PubMed] [Google Scholar]
- Goldberg LR. The development of markers for the Big-Five structure. Psychological Assessment. 1992;4:26–42. [Google Scholar]
- Gottman JM. What predicts divorce? The relationship between marital processes and marital outcomes. Hillsdale, NJ: Lawrence Erlbaum; 1994. [Google Scholar]
- Grzywacz JG, Marks NF. Reconceptualizing the work-family interface: An ecological perspective on the correlates of positive and negative spillover between work and family. Journal of Occupational Health Psychology. 2000;5:111–126. doi: 10.1037//1076-8998.5.1.111. [DOI] [PubMed] [Google Scholar]
- Heath AC, Eaves LJ, Martin NG. Interaction of marital status and genetic risk for symptoms of depression. Twin Research. 1998;1:119–122. doi: 10.1375/136905298320566249. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Myers JM, Prescott C, Kendler KS. A population-based twin study of the relationship between neuroticism and internalizing disorders. American Journal of Psychiatry. 2006;163:857–864. doi: 10.1176/ajp.2006.163.5.857. [DOI] [PubMed] [Google Scholar]
- Hooley J. Do psychiatric patients do better clinically if they live with certain kinds of families? Current Directions in Psychological Science. 2004;13:202–205. [Google Scholar]
- Horowitz AV, McLaughlin J, White HR. How the negative and positive aspects of partner relationships affect the mental health of young married people. Journal of Health and Social Behavior. 1998;39:124–136. [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- John OP. The Big Five factor taxonomy: Dimensions of personality in the natural language and in questionnaires. In: Pervin LA, editor. Handbook of personality: Theory and research. New York: Guilford Press; 1990. pp. 66–100. [Google Scholar]
- Johnson W, Krueger RF. Genetic and environmental structure of adjectives describing the domains of the Big Five Model of personality: A nationwide US twin study. Journal of Research in Personality. 2004;38:448–472. [Google Scholar]
- Karney B, Bradbury TN. The longitudinal course of marital quality and stability: A review of theory, methods, and research. Psychological Bulletin. 1995;118:3–34. doi: 10.1037/0033-2909.118.1.3. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Baker JH. Genetic influences on measures of the environment: A systematic review. Psychological Medicine. 2007;37:615–626. doi: 10.1017/S0033291706009524. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Walters EE, Neale MC, Kessler RC, Heath AC, Eaves LJ. The structure of the genetic and environmental risk factors for six major psychiatric disorders in women. Archives of General Psychiatry. 1995;52:374–383. doi: 10.1001/archpsyc.1995.03950170048007. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, Gilman SE, Kessler RC. Sexual orientation in a national sample of twin and sibling pairs. American Journal of Psychiatry. 2000;157:1843–1846. doi: 10.1176/appi.ajp.157.11.1843. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen HU. The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF) International Journal of Methods in Psychiatric Research. 1998a;7:171–185. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Gilman SE, Thornton LM, Kendler KS. Health, wellbeing, and social responsibility in the MIDUS twin and sibling subsamples. In: Brim OG, Ryff CD, Kessler RC, editors. How healthy are we? A national study of wellbeing at midlife. Chicago: University of Chicago Press; 2004. pp. 124–152. [Google Scholar]
- Kessler RC, Wittchen HU, Abelson JM, Kendler KS, Knauper B, McGonagle KA, Schwarz N, Zhao S. Methodological studies of the composite international diagnostic interview (CIDI) in the US national comorbidity survey. International Journal of Methods in Psychiatric Research. 1998b;7:33– 55. [Google Scholar]
- Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. British Journal of Psychiatry. 2005;186:190–196. doi: 10.1192/bjp.186.3.190. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM–III–R): A longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Bouchard TJ. The extended genotype: The heritability of personality accounts for the heritability of recalled family environments in twins reared apart. Journal of Personality. 2003;71:809–833. doi: 10.1111/1467-6494.7105005. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Krueger RF, Piasecki TM. Toward a dimensional and psychometrically informed approach to conceptualizing psychopathology. Behavior Research and Therapy. 2002;40:485–500. doi: 10.1016/s0005-7967(02)00016-5. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Weaver SL. The Midlife Development Inventory (MIDI) personality scales: Scale construction and scoring. Waltham, MA: 1997. [Google Scholar]
- Lykken DT, Bouchard TJ, McGue M, Tellegen A. The Minnesota Twin Family Registry: Some initial findings. Acta Genetica Medica Gemellol. 1990;39:35–70. doi: 10.1017/s0001566000005572. [DOI] [PubMed] [Google Scholar]
- Markon K, Krueger RF. An empirical comparison of information-theoretic selection criteria for multivariate behavior genetic models. Behavior Genetics. 2004;34:593–610. doi: 10.1007/s10519-004-5587-0. [DOI] [PubMed] [Google Scholar]
- Markowitz JS, Weissman MM, Ouellette R, Lish JD, Klerman GL. Quality of life in panic disorder. Archives of General Psychiatry. 1989;46:984–992. doi: 10.1001/archpsyc.1989.01810110026004. [DOI] [PubMed] [Google Scholar]
- Marks NF, Bumpass LL, Jun H. Family roles and well-being during the middle life course. In: Brim OG, Ryff CD, Kessler RC, editors. How healthy are we? A national study of well-being at midlife. Chicago, IL: The University of Chicago Press; 2004. [Google Scholar]
- McGue M, Bouchard TJ. Quality of twin data for the effects of age and sex. Behavior Genetics. 1984;14:325–343. doi: 10.1007/BF01080045. [DOI] [PubMed] [Google Scholar]
- McLeod JD. Anxiety disorders and marital quality. Journal of Abnormal Psychology. 1994;103:767–776. doi: 10.1037//0021-843x.103.4.767. [DOI] [PubMed] [Google Scholar]
- Middeldorp CM, Cath DC, Van Dyck R, Boomsma DI. The co-morbidity of anxiety and depression in the perspective of genetic epidemiology: a review of twin and family studies. Psychological Medicine. 2005;35:611–24. doi: 10.1017/s003329170400412x. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles, CA: Author; 2004. [Google Scholar]
- Neale MC, Boker SM, Xie G, Maes HH. Mx: Statistical Modeling. 6 VCU Box 900126, Richmond, VA 23298: Department of Psychiatry; 2003. [Google Scholar]
- Plant VC, Markus HR, Lachman ME. Place matters: Consensual features and regional variation in American well-being and self. Journal of Personality and Social Psychology. 2002;83:160–184. [PubMed] [Google Scholar]
- Purcell S. Variance components models for gene-environment interaction in twin analysis. Twin Research. 2002;5:554–571. doi: 10.1375/136905202762342026. [DOI] [PubMed] [Google Scholar]
- Rowe DC. Environmental and genetic influences on dimensions of perceived parenting: A twin study. Developmental Psychology. 1981;17:203–208. [Google Scholar]
- Rowe DC. A biometrical analysis of perceptions of family environment: A study of twin and singleton sibling kinships. Child Development. 1983;54:416–423. [PubMed] [Google Scholar]
- Schuster TL, Kessler RC, Aseltine RH. Supportive interactions, negative interactions, and depressed mood. American Journal of Community Psychology. 1990;18:423–438. doi: 10.1007/BF00938116. [DOI] [PubMed] [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- South SC, Krueger RF, Johnson W, Iacono WG. Adolescent personality moderates genetic and environmental influences on perceived relationships with parents. 2007. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spotts EL, Lichtenstein P, Pedersen N, Neiderhiser JM, Hansson K, Cederblad M, Reiss D. Personality and marital satisfaction: A behavioural genetic analysis. European Journal of Personality. 2005a;19:205–227. [Google Scholar]
- Spotts EL, Neiderhiser JM, Ganiban J, Reiss D, Lichtenstein P, Hansson K, Cederblad M, Pedersen NL. Accounting for depressive symptoms in women: A twin study of associations with interpersonal relationships. Journal of Affective Disorders. 2004a;82:101–111. doi: 10.1016/j.jad.2003.10.005. [DOI] [PubMed] [Google Scholar]
- Spotts EL, Neiderhiser JM, Towers H, Hansson K, Lichtenstein P, Cederblad M, Pederson NL, Reiss D. Genetic and environmental influences on marital relationships. Journal of Family Psychology. 2004b;18:107–119. doi: 10.1037/0893-3200.18.1.107. [DOI] [PubMed] [Google Scholar]
- Spotts EL, Pedersen NL, Neiderhiser JM, Reiss D, Lichtenstein P, Hansson K, Cederblad M. Genetic effects on women’s positive mental health: Do marital relationships and social support matter? Journal of Family Psychology. 2005b;19:339–349. doi: 10.1037/0893-3200.19.3.339. [DOI] [PubMed] [Google Scholar]
- Spotts EL, Prescott C, Kendler KS. Examining the origins of gender differences in marital quality: A behavior genetic analysis. Journal of Family Psychology. 2006;20:605–613. doi: 10.1037/0893-3200.20.4.605. [DOI] [PubMed] [Google Scholar]
- Staudinger UM, Fleeson W, Baltes PB. Predictors of subjective physical health and global well-being: Similarities and differences between the United States and Germany. Journal of Personality and Social Psychology. 1999;76:305–319. [Google Scholar]
- Trapnell PD, Wiggins JS. Extension of the interpersonal adjective scales to include the Big Five dimensions of personality. Journal of Personality and Social Psychology. 1990;59:781–790. [Google Scholar]
- Turkheimer E. Three laws of behavior genetics and what they mean. Current Directions in Psychological Science. 2000;9:160–164. [Google Scholar]
- Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: The NEMESIS Study. Archives of General Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- Wamboldt MZ, Reiss D. Genetic strategies for clarifying a nosology of relational Distress. Journal of Family Psychology. 2006;20:378–385. doi: 10.1037/0893-3200.20.3.378. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. Journal of Abnormal Psychology. 1988;97:346–353. doi: 10.1037//0021-843x.97.3.346. [DOI] [PubMed] [Google Scholar]
- Watson D, Gamez W, Simms L. Basic dimensions of temperament and their relation to anxiety and depression: A symptom-based perspective. Journal of Research in Personality. 2005;39:46–66. [Google Scholar]
- Whisman MA. Marital dissatisfaction and psychiatric disorders: Results from the National Comorbidity Survey. Journal of Abnormal Psychology. 1999;108:701–706. doi: 10.1037//0021-843x.108.4.701. [DOI] [PubMed] [Google Scholar]
- Whisman MA. Marital distress and DSM-IV psychiatric disorders in a population-based national survey. Journal of Abnormal Psychology. 2007;116:638–643. doi: 10.1037/0021-843X.116.3.638. [DOI] [PubMed] [Google Scholar]
- Whisman MA. The association between depression and marital dissatisfaction. In: Beach SRH, editor. Marital and family processes in depression: A scientific foundation for clinical practice. Washington, DC: American Psychological Association; 2001. pp. 3–24. [Google Scholar]
- Whisman MA, Sheldon CT, Goering P. Psychiatric disorders and dissatisfaction with social relationships: Does type of relationship matter? Journal of Abnormal Psychology. 2000;109:803–808. doi: 10.1037//0021-843x.109.4.803. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA. Comorbidity of relationship distress and mental and physical health problems. In: Snyder DK, Whisman MA, editors. Treating difficult couples: Helping clients with coexisting mental and relationship distress. New York: Guilford; 2003. [Google Scholar]
- Whisman MA, Uebelacker LA, Weinstock LM. Psychopathology and marital satisfaction: The importance of evaluating both partners. Journal of Consulting and Clinical Psychology. 2004;72:830–838. doi: 10.1037/0022-006X.72.5.830. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Clark LA. Toward DSM-V and the classification of psychopathology. Psychological Bulletin. 2000;126:946–963. doi: 10.1037/0033-2909.126.6.946. [DOI] [PubMed] [Google Scholar]
- Wittchen HU. Reliability and validity studies of the WHO composite international diagnostic interview (CIDI): A critical review. Journal of Psychiatric Research. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Yu CY. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes. University of California; Los Angeles: 2002. Doctoral dissertation. [Google Scholar]