Summary
Background
The treatment of perinatal depression is a public-health priority because of its high prevalence and association with disability and poor infant development. We integrated a cognitive behaviour therapy-based intervention into the routine work of community-based primary health workers in rural Pakistan and assessed the effect of this intervention on maternal depression and infant outcomes.
Methods
We randomly assigned 40 Union Council clusters in rural Rawalpindi, Pakistan, in equal numbers to intervention or control. Married women (aged 16–45 years) in their third trimester of pregnancy with perinatal depression were eligible to participate. In the intervention group, primary health workers were trained to deliver the psychological intervention, whereas in the control group untrained health workers made an equal number of visits to the depressed mothers. The primary outcomes were infant weight and height at 6 months and 12 months, and secondary outcome was maternal depression. The interviewers were unaware of what group the participants were assigned to. Analysis was by intention to treat. The study is registered as ISRCTN65316374.
Findings
The number of clusters per group was 20, with 463 mothers in the intervention group and 440 in the control group. At 6 months, 97 (23%) of 418 and 211 (53%) of 400 mothers in the intervention and control groups, respectively, met the criteria for major depression (adjusted odds ratio (OR) 0·22, 95% CI 0·14 to 0·36, p<0·0001). These effects were sustained at 12 months (111/412 [27%] vs 226/386 [59%], adjusted OR 0·23, 95% CI 0·15 to 0·36, p<0·0001). The differences in weight-for-age and height-for-age Z scores for infants in the two groups were not significant at 6 months (−0·83 vs −0·86, p=0·7 and −2·03 vs −2·16, p=0·3, respectively) or 12 months (−0·64 vs −0·8, p=0·3 and −1·10 vs −1·36, p=0·07, respectively).
Interpretation
This psychological intervention delivered by community-based primary health workers has the potential to be integrated into health systems in resource-poor settings.
Funding
Wellcome Trust.
Introduction
Depression is the fourth leading cause of disease burden and the largest cause of non-fatal burden, accounting for almost 12% of years lived with disability worldwide.1 A systematic review suggests an overall mean prevalence of 33% in the Pakistani population, with women at a greater risk than are men.2 In a previous study of rural Pakistani women, we reported a prevalence of 25% during pregnancy and 28% in the postnatal period.3 Perinatal depression was associated with high rates of disability, infant malnutrition, increased rates of infant diarrhoea, and reduced uptake of immunisation.4,5
Evidence from high-income countries shows that psychotherapeutic approaches, such as cognitive behaviour therapy, interpersonal therapy, or problem-solving, are effective treatments for depression.6 Randomised trials from low-income and middle-income countries resulted in similar findings.7,8 However, the overall difficulty in these countries remains the scarcity of mental-health professionals to deliver such interventions to underprivileged communities.9 The challenge is to adapt these interventions so that they can be delivered by ordinary health workers without previous training in mental health. Furthermore, policy makers in low-income countries need to be convinced of the public health importance of treating mental disorders so that they integrate such interventions into existing health systems.10
With a population of more than 130 million, Pakistan is the world's sixth most populous country. It is a low-income country, with an income per person of less than US$500 per year, and 33% of the population live below the poverty line.11 The literacy rate among women and girls is 35%. The infant mortality rate is about 80 per 1000 livebirths and more than a third of children aged less than 5 years show stunted growth.12 The proportion of the yearly budget spent on health was 0·7% in 2000–01; no figures are available for the amount spent on mental health. About 350 psychiatrists and 3000 psychiatric beds are concentrated in the major cities, without any specialist mental health services in the rural areas where 67% of Pakistan's population resides.11
From earlier quantitative and qualitative studies done in a rural sub-district of Pakistan, we developed an intervention based on principles of cognitive behaviour therapy, which could be delivered by ordinary village-based primary health workers.3,13 We used a manual (with step by step instructions for each session) to train the health workers and for them to keep for reference. The intervention, called the Thinking Healthy Programme, used cognitive behaviour therapy techniques of active listening, collaboration with the family, guided discovery (ie, style of questioning to both gently probe for family's health beliefs and to stimulate alternative ideas), and homework (ie, trying things out between sessions, putting what has been learned into practice), and applied these to health workers' routine practice of maternal and child health education. The intervention was integrated into existing health systems in a rural sub-district of Pakistan, and pilot studies showed that both health workers and depressed mothers reported the programme to be relevant and useful; further details of the intervention process are described elsewhere.13
Our aims were to assess the effect of the intervention on perinatal depression in women, and to test the hypothesis that treatment of perinatal depression would lead to improved nutrition and other health outcomes in the infant.
Methods
Study area and participants
The study was done in two rural areas (ie, Gujar Khan and Kallar Syedan, with a combined population of 600 000), located 65 km southeast of Rawalpindi city. Most families in the area depend on subsistence farming, supplemented by one or more of the men serving in the armed forces or working as government employees, or as semi-skilled or unskilled labourers in the cities.14 Primary health care is delivered through a network of Basic Health Units, each providing care to about 15 000–20 000 people. Each unit is staffed by a doctor, midwife, vaccinator, and 15–20 village-based community health workers called Lady Health Workers. These women have completed secondary school, and are trained to provide mainly preventive maternal and child health care, and education in the community. Each Lady Health Worker is responsible for about 100 households in her village. About 96 000 health workers in the Lady Health Worker programme provide coverage to more than 80% of Pakistan's rural population (some inaccessible areas, including some of the tribal areas are not covered).15
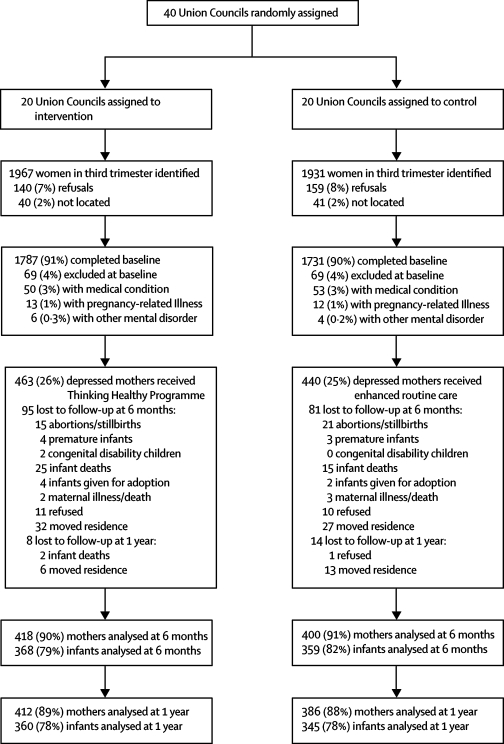
The smallest administrative unit in Pakistan is the Union Council, which has a population of around 15 000–20 000. This unit was chosen as the cluster unit of randomisation. Normally one Basic Health Unit provides primary health care for one Union Council and all affiliated Lady Health Workers work in villages within that Union Council only. Supervision of health workers takes place in the Union Council. Thus the risk of contamination of the control group with the intervention is negligible. There were 40 Union Councils in the two subdistricts of the study area. These subdistricts were geographically contiguous and ethnically, culturally, and socioeconomically homogeneous. All the units were eligible for randomisation, which was done by an independent trial centre in Islamabad, before recruitment of participants (figure 1). These administrative units were assigned by random allocation with a table of random numbers by a researcher who was not involved in the study and who was unaware of the identity of the Union Councils. Lady Health Workers from each Union Council were enrolled to participate in the study before randomisation.
Figure 1.
Trial profile
Participants were women in the 40 Union Councils who were aged 16–45 years, married, and in their third trimester of pregnancy. They were enrolled from April, 2005, to March, 2006. Lists of participants were compiled from official registers kept with the Lady Health Workers. To ensure full coverage, we did an additional door-to-door survey to identify women not registered. We excluded women with a diagnosed serious medical condition requiring inpatient or outpatient treatment, pregnancy-related illness (except for common conditions, such as anaemia), substantial physical or learning disability, and postpartum or other form of psychosis (figure 1).
We did baseline (ie, at the third trimester of pregnancy) assessments after the women had been identified in each Union Council. The assessments were done by experienced psychiatrists (AM and SS) who were trained to administer the structured clinical interview for Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV diagnosis,16 which is a semi-structured diagnostic interview that has been widely used in cross-cultural epidemiological and treatment studies of prenatal and postnatal depression.17 We translated and culturally adapted the section for major depressive episode into Urdu with a rigorous procedure developed in Pakistan for previous studies.18 We established inter-rater reliability before starting the study—both interviewers independently assessed 20 women (ten had clinical depression) and agreed on the diagnosis of 19 (κ=0·90). All women who fulfilled the criteria for a DSM-IV major depressive episode were recruited into the trial (figure 1). The interviewers assessed depressed women at baseline with the Hamilton Depression Rating Scale,19 a measure of depressive symptoms that has 17 items and a total score from 0 to 54 (with higher scores indicating increased severity of depression). The interviewers were unaware of the allocation status of the Union Councils (because they had no contact with the team that did the randomisation), and we took care to ensure they remained so; none of the interviewers resided in the study area, and throughout the duration of the study they had no contact with the Lady Health Workers or any other health personnel in the study area. Mothers were asked not to tell the interviewers anything about their sessions with Lady Health Workers.
We used questionnaires that we had translated and adapted in our previous studies for the other baseline assessments.3,20 These assessments included the brief disability questionnaire,21 an eight-item questionnaire that rates present difficulties in doing daily activities on a scale of 0 (not at all) to 2 (definitely), with a maximum score of 16; global assessment of functioning scale,22 a 100-point scale reporting the clinician's assessment of the patient's overall psychological, social, and occupational functioning on a hypothetical continuum (with a higher score indicating better functioning); and the multidimensional scale for perceived social support,23 a 12-item Likert scale measuring the subjective assessment of adequacy of social support from family, friends, and partners (higher score indicating greater social support). We gathered data for socioeconomic status and demographic characteristics.
We obtained informed verbal and written consent from the participants. Ethical approval for the study was granted by committees of the University of Manchester, UK, and the Institute of Psychiatry, Rawalpindi, Pakistan.
Intervention and control groups
Mothers in the intervention clusters received the Thinking Healthy Programme through 40 specially trained Lady Health Workers (ie, two for each Union Council cluster). Participants only knew that they were receiving one of two types of visits from the health workers. The intervention consisted of a session every week for 4 weeks in the last month of pregnancy, three sessions in the first postnatal month, and nine 1-monthly sessions thereafter.13 Mothers in the control clusters received an equal number of visits in exactly the same way as those in the intervention group, but by routinely trained Lady Health Workers (two for each Union Council). These health workers in both groups received monthly supervision, and were monitored by the research team to ensure that they were attending the scheduled visits. In practice, the Lady Health Workers seldom provide such structured and monitored care in the community. The control group thus received what would be regarded as ideal care, which we called enhanced routine care.
Outcome assessments at follow-up
Infants who were aborted, stillborn, born premature or congenitally disabled, given up for adoption, or died in the first year were excluded from the study (figure 1). Mothers, who became seriously ill, died, or moved residence were excluded (figure 1). Mothers in both the intervention and control groups were re-interviewed by the same psychiatrists at 6 months and 12 months postnatally. Infants in both groups were weighed and measured with standard techniques.24 Growth data were converted into SDs (Z scores) for weight and length with Epi Info 2002 (version 3.4.1).
Additionally, at 6 months, mothers were asked if they were exclusively breastfeeding. At 12 months, the number of diarrhoeal episodes in the infants in the 2 weeks before interview was recorded with a questionnaire used in previous studies;5 diarrhoea was defined as three or more unformed stools passed in 24 h, and a diarrhoeal episode was defined as being separated from another episode by at least 3 diarrhoea-free days. Records of immunisation were assessed at 12 months for all infants in the study, and infants were classified as those with or without up-to-date immunisation status. At 12 months, mothers were asked if they were using any form of contraception, and both parents were asked if they set aside time everyday to play with their infant. All infant outcomes were assessed by researchers unaware of the psychiatric status of the mother.
Statistical analysis
Because we wanted to study the effect of the intervention on infant outcomes, we did our sample-size calculations with infant nutrition as the primary outcome. On the basis of previous observational work,4 we estimated a difference of 0·62 SD in infant weight-for-age Z score between intervention and control groups. The unit of randomisation was the Union Council. With 20 Union Councils in each group, 18 mothers per Union Council, and assuming an intra-cluster correlation coefficient of 0·05, a sample size of 360 in each group would give more than 95% power to detect the effect size at a significance level of 0·05. The same sample size would give us a power of more than 80% to detect a difference of 0·3 SD with maternal depression as the secondary outcome.
The Manchester centre, under the supervision of the trial statistician (CR), independently undertook the analysis. We based the statistical analysis on a random-effects model with random effects for Union Council and mother.25 For outcomes, we included covariates in the model for baseline value of the outcome, and mother's age, education, parity, infant sex, and socioeconomic status. We checked distributional assumptions with normal probability plots of patient and Union Council residuals. We analysed binary and ordinal outcomes with a random-effects logistic regression model with the same covariates, and did statistical analyses with STATA 9 (version 9.0). In the intervention group, we compared weight and height of the infants born to mothers whose depressive disorder had and had not resolved.
The study is registered as ISRCTN65316374.
Role of the funding source
The sponsor of the study had no role in the design, data analysis, data interpretation, writing of the report, or in the decision to submit the report for publication. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
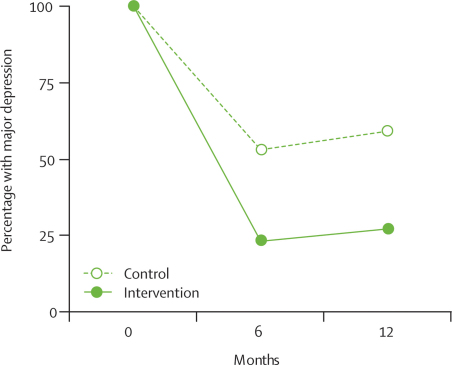
Figure 1 shows the trial profile. At birth, 226 (51%) of 440 infants in the intervention group and 223 (48%) of 463 in the control group were boys. Table 1 shows the baseline characteristics. Table 2 and figure 2 show the prevalence of DSM-IV major depressive episodes in the two groups at 6 months and 12 months. At both time points, the prevalence was much higher in the control group than in the intervention group. The cluster-adjusted odds ratio (OR) for major depression among women in the control clusters compared with those in the intervention clusters was highly significant and remained so after adjustment for covariates.
Table 1.
Demographics and baseline characteristics of participants in intervention and control clusters
| Intervention (N=463) | Control (N=440) | ||
|---|---|---|---|
| Participants | |||
| Age (years) | |||
| <20 | 30 (6%) | 21 (5%) | |
| 20–24 | 138 (30%) | 122 (28%) | |
| 25–29 | 154 (33%) | 150 (34%) | |
| 30–34 | 90 (19%) | 87 (20%) | |
| >35 | 51 (11%) | 60 (14%) | |
| Mean age | 26·5 (5·2) | 27·0 (5·1) | |
| Schooling (years) | |||
| 0 | 184 (40%) | 190 (43%) | |
| 1–6 (primary) | 147 (32%) | 128 (29%) | |
| 7–10 (secondary) | 116 (25%) | 105 (24%) | |
| >10 | 16 (3%) | 17 (4%) | |
| Mean schooling | 4·2 (4·0) | 3·9 (3·9) | |
| Body-mass index | 23·3 (4·1) | 23·1 (4·1) | |
| Financially empowered | 238 (51%) | 240 (55%) | |
| Mean depression score* | 14·8 (4·2) | 14·4 (4·0) | |
| Mean disability score† | 8·1 (2·7) | 8·3 (2·7) | |
| Family | |||
| Extended/joint family | 250 (54%) | 280 (64%) | |
| Illiterate husband | 87 (19%) | 78 (18%) | |
| Number of children | |||
| 0 | 89 (19%) | 82 (19%) | |
| 1–2 | 191 (41%) | 171 (39%) | |
| 3–4 | 133 (29%) | 137 (31%) | |
| >5 | 50 (11%) | 50 (11%) | |
| Mean number | 2·2 (1·8) | 2·3 (1·8) | |
| Socioeconomic status | |||
| Health workers' rating | |||
| 1 (richest) | 6 (1%) | 6 (1%) | |
| 2 | 43 (9%) | 38 (9%) | |
| 3 | 173 (37%) | 170 (39%) | |
| 4 | 142 (31%) | 128 (29%) | |
| 5 (poorest) | 99 (21%) | 98 (22%) | |
| In debt | 266 (57%) | 235 (53%) | |
| Rated below 3 and in debt | 169 (37%) | 158 (36%) | |
| Ownership of assets and amenities | |||
| Own land | 242 (52%) | 238 (54%) | |
| Electricity | 442 (95%) | 412 (94%) | |
| Television | 278 (60%) | 263 (60%) | |
| Refrigerator | 169 (37%) | 151 (34%) | |
| Source of drinking water | |||
| Well without pump | 178 (38%) | 178 (40%) | |
| Well with pump | 158 (34%) | 141 (32%) | |
| Piped onto residence or property | 30 (6%) | 26 (6%) | |
| Other | 97 (21%) | 95 (22%) | |
| Type of toilet facility | |||
| Field | 253 (55%) | 251 (57%) | |
| Flush toilet | 126 (27%) | 109 (25%) | |
| Other (pit, bucket) | 84 (18%) | 80 (18%) | |
Data are number (%) or mean (SD).
Hamilton Depression Rating Scale.
Brief Disability Questionnaire.
Table 2.
Comparison of changes in rates of diagnosable major depression after intervention at 6 months and 12 months postnatally
| Intervention | Control | ICC | Adjusted odds ratio (95% CI)* | p value | |
|---|---|---|---|---|---|
| 6 months | 97/418 (23%) | 211/400 (53%) | 0·047 | 0·22 (0·14–0·36) | <0·0001 |
| 12 months | 111/412 (27%) | 226/386 (59%) | 0·037 | 0·23 (0·15–0·36) | <0·0001 |
Data are number (%), unless otherwise indicated. Diagnosis of major depression based on Diagnostic and Statistical Manual of Mental Disorders-IV criteria. ICC=intra-cluster correlation coefficient.
Adjusted for baseline depression score, mothers' age, parity, education, socioeconomic status, and infant sex with a logistic regression model with random effect for Union Council.
Figure 2.
Rates of depression in women in the control and intervention groups at 6 months and 12 months
Mothers in the intervention group had lower depression scores and lower disability scores at both time points than did mothers in the control group (table 3). Similarly, mothers in the intervention group had better overall functioning and perception of social support (table 3). The differences remained significant when adjusted for baseline scores of each measure, mother's age, education, parity, infant sex, and socioeconomic status (table 3).
Table 3.
Effect of intervention on depression, disability, functioning, and perceived social support scores
| Intervention | Control | ICC | Adjusted mean difference (95% CI)* | p value | |
|---|---|---|---|---|---|
| Depression score† | |||||
| Baseline | 463 (14·8, 4·2) | 440 (14·4, 4·0) | n/a | n/a | n/a |
| 6 months | 418 (4·5, 6·0) | 400 (8·7, 7·4) | 0·090 | −5·86 (−7·92 to −3·80)‡ | <0·0001 |
| 12 months | 412 (5·4, 6·5) | 386 (10·7, 8·1) | 0·056 | −6·65 (−8·56 to −4·74)‡ | <0·0001 |
| Disability score§ | |||||
| Baseline | 440 (8·1, 2·7) | 440 (8·3, 2·7) | n/a | n/a | n/a |
| 6 months | 418 (2·3, 3·1) | 400 (4·2, 3·9) | 0·061 | −1·80 (−2·48 to −1·12) | <0·0001 |
| 12 months | 412 (2·2, 3·3) | 386 (5·2, 4·5) | 0·060 | −2·88 (−3·66 to −2·10) | <0·0001 |
| Function score¶ | |||||
| Baseline | 440 (62, 5·1) | 440 (62, 5·3) | n/a | n/a | n/a |
| 6 months | 418 (79, 9·9) | 400 (72, 11·9) | 0·060 | 6·85 (4·73 to 8·96) | <0·0001 |
| 12 months | 412 (78, 9·9) | 386 (69, 12·0) | 0·047 | 8·27 (6·23 to 10·31) | <0·0001 |
| Perceived social support score‖ | |||||
| Baseline | 440 (46, 16·6) | 440 (44·5, 16·3) | n/a | n/a | n/a |
| 6 months | 418 (50·8, 15·3) | 400 (43·7, 15·7) | 0·043 | 6·71 (3·93 to 9·48) | <0·0001 |
| 12 months | 412 (51·0, 12·1) | 386 (42·5, 13·8) | 0·059 | 7·85 (5·43 to 10·27) | <0·0001 |
Data are number (mean, SD), unless otherwise indicated. ICC=intra-cluster correlation coefficient. n/a=not applicable.
Adjusted for baseline scores, mother's age, parity, education, infant sex, and socioeconomic status with random effect for Union Council.
Hamilton Depression Rating Scale19 (maximum score 54; higher score indicating greater severity).
Random-effect Tobit regression due to number of zero scores.
Brief Disability Questionnaire21 (maximum score 16; higher score indicating greater disability).
Global Assessment of Functioning Scale22 (maximum score 100, higher score indicating improved functioning).
Multidimensional scale for perceived social support23 (maximum score 84; higher score indicating better perceived social support).
The differences between the intervention and control groups in weight-for-age Z scores or height-for-age Z scores at 6 months or 12 months were not significant, although at 12 months the number of stunted infants in the intervention arm was less than that in the control arm (table 4). Further analysis of the intervention group showed that infants whose mothers were still depressed at 6 months had significantly lower Z scores at both 6 months (weight-for-age −1·2 vs −0·73, p=0·0003; height-for-age −0·94 vs −0·55, p=0·0033) and 12 months (weight-for-age −2·2 vs −1·95, p=0·0149; height-for-age −1·5 vs −0·98, p<0·0001) than did infants whose mothers had recovered. The associations remained significant after we controlled for all sociodemographics listed in table 1 with multivariate analysis, indicating that untreated maternal depression contributed to infant undernutrition substantially and independently even in the intervention group.
Table 4.
Effect of intervention on infant growth
| Intervention | Control | ICC | Adjusted mean difference (95% CI)* | p value | ||
|---|---|---|---|---|---|---|
| 6 months | 0·07 (−0·09 to 0·23) | 0·38 | ||||
| Stunted† | 32/368 (9%) | 32/359 (9%) | ||||
| HAZ | −0·64 (1·04) | −0·8 (1·01) | 0·019 | |||
| 12 months | 0·17 (−0·02 to 0·35) | 0·07 | ||||
| Stunted* | 66/360 (18%) | 81/345 (23%) | ||||
| HAZ | −1·10 (1·02) | −1·36 (1·17) | 0·032 | |||
| 6 months | −0·02 (−0·18 to 0·14) | 0·76 | ||||
| Underweight* | 43/368 (12%) | 43/359 (12%) | ||||
| WAZ | −0·83 (1·06) | −0·86 (1·00) | 0·017 | |||
| 12 months | 0·07 (−0·08 to 0·22) | 0·37 | ||||
| Underweight* | 215/360 (60%) | 223/345 (65%) | ||||
| WAZ | −2·03 (1·01) | −2·16 (1·03) | 0·004 | |||
Data are n/N (%) or mean (SD), unless otherwise indicated. HAZ=height-for-age Z score. WAZ=weight-for-age Z score. ICC=intra-cluster correlation coefficient.
Adjusted for maternal height and weight, parity, education, infant sex, baseline depression, disability, and perceived social support scores with regression model with random effect for Union Council.
A child is considered stunted or underweight if the growth is less than the anthropometric cutoff of −2 SD below the median WAZ and HAZ scores of the National Center for Health Statistics/WHO international references.26
The rate of stunting and underweight rose sharply from 6 months to 12 months in both intervention and control groups (table 4). This rise is a recognised occurrence in infants because the risk of malnutrition begins to increase after 6 months of age when most children stop breastfeeding and begin relying on solid foods. However, the overall rate of underweight in the two groups was higher than the overall rate at this age reported for Pakistan (42%),12 and was probably the effect of untreated maternal depression in both groups (table 4).
Infants in the intervention group were less likely to have had a diarrhoeal episode in the 2 weeks preceding the 12-month assessment and were more likely to have completed their scheduled immunisation (table 5). Contraceptive use by mothers in the intervention group was significantly higher than in the control group (table 5). The rate of exclusive breastfeeding was higher in the intervention group, although not significant (table 5). Both parents in the intervention group reported spending more time everyday on play-related activities with the infant than did parents in the control group (table 5).
Table 5.
Effect of intervention on activities affecting infant health
| Intervention | Control | ICC | Adjusted odds ratio(95% CI)* | p value | |
|---|---|---|---|---|---|
| Health outcome | |||||
| Diarrhoea episodes at 12 months† | 116/360 (32%) | 149/345 (43%) | 0·056 | 0·6 (0·39–0·98) | 0·04 |
| Complete immunisation at 12 months | 339/360 (94%) | 294/345 (85%) | 0·013 | 2·5 (1·47–4·72) | 0·001 |
| Contraceptive use at 12 months | 253/406 (62%) | 205/385 (53%) | 0·003 | 1·6 (1·20–2·27) | 0·002 |
| Exclusive breastfeeding at 6 months | 63/368 (17%) | 40/359 (11%) | 0·070 | 1·6 (0·79–3·18) | 0·20 |
| Play frequency with infant at 12 months‡ | |||||
| Mother | 247/360 (69%) | 149/345 (43%) | 0·005 | 2·4 (2·07–4·01) | <0·0001 |
| Father | 191/302 (63%) | 119/285 (42%) | 0·058 | 1·9 (1·59–4·15) | 0·0001 |
Data are n/N (%), unless otherwise indicated. ICC=intra-cluster correlation coefficient.
Adjusted for parity, education, infant sex, socioeconomic status, baseline depression, disability, and perceived social support with a random effect for Union Council.
One or more in 2 weeks before assessment.
Once or more every day.
Discussion
The intervention did not produce any significant change in infant growth indices but had other benefits—ie, infants had less episodes of diarrhoea and were more likely to be immunised than those in the control group; mothers were more likely to use contraception (birth spacing is an important factor in reducing infant morbidity), and both parents reported spending more time playing with their infants. In a poor rural community with little access to mental health care, integration of a cognitive behaviour therapy-based intervention into the routine work of community health workers more than halved the rate of depression in prenatally depressed women compared with those receiving enhanced routine care. In addition to symptomatic relief, the women receiving the intervention had less disability and better overall and social functioning, and these effects were sustained after 1 year.
This community-based trial had a high response and follow-up rate. Assessments were done by trained and experienced researchers who were from the same cultural background as the depressed women, and all instruments were culturally adapted. The cluster design ensured that the risk of contamination was negligible. Although cluster-randomised trials are susceptible to bias, the baseline characteristics in the two groups were similar, and efforts were made to ensure that the assessors remained unaware of the allocation. The trial did not capture mothers who were not depressed in pregnancy and developed a depressive episode postnatally. However, our previous study in the same area showed that in more than 90% of the women, postnatal depression was a continuation of a depressive episode during pregnancy3 and therefore targeting women for intervention during pregnancy was the correct strategy.
The rate of stunting in infants in the intervention group was non-significantly less than that in the control group. Height for age is more responsive to repeated or longer term adverse conditions (such as maternal depression) than is weight for age, which responds to acute adversity.27 Growth is likely to be affected by complex interactions between maternal, child, and environmental variables. The benefits of improved maternal mental health on infant nutrition, possibly mediated through improved stimulation, care, and responsive feeding are likely to be cumulative and develop during time. A longer follow-up might have shown significant effects of the intervention. The finding that infants whose mothers did not respond to treatment had poor growth, even after controlling for sociodemographic factors, strengthens the argument for an important role of maternal depression in infant undernutrition. Thus, earlier interventions (before depression becomes chronic), and development of secondary-care and tertiary-care facilities for depressed women who do not respond to primary care, might be necessary.
Of note, our comparisons were not between intervention and treatment as usual but intervention and enhanced routine care. The rate of recovery from depression in the control group at 6 months (47%) was greater than the rate of spontaneous remission without treatment we reported in our previous observational study in the same area (24%).28 We did not assess whether the Lady Health Workers in the control group took action to treat the mothers' depression (other than monitoring their visits). Even regular, monitored visits by experienced health workers could have had therapeutic benefits, which could have diluted the effects of our intervention on our primary outcome. Such treatment effects with control groups have been reported in other trials in developing countries.29
Even in high-income countries, more than 50% of people in the community with major depression are not treated because access to mental health care is absent.30 In low-income countries, this value is 70–100%.31 This intervention has the potential of providing mental health care at the doorstep to a very high proportion of women with this highly prevalent and disabling mental disorder in Pakistan and other low-income countries. This programme is not vertical (ie, focusing solely on depression); it is dependent on a separate mental-health workforce. On the contrary, the integrated cognitive behaviour therapy-approach eases the routine work of health workers with women who are otherwise socially excluded and difficult to access, and has added benefits, such as improvement of infant health outcomes. Indeed, the intervention led to an increased rate of immunisation and uptake of contraception, the two key tasks for Lady Health Workers. These effects, combined with the high prevalence of maternal depression, should make this intervention of interest to policy makers.
The intervention was designed to be integrated into the routine work of the Lady Health Workers, and feedback from the 40 trained women showed that almost all of them thought it was relevant to their day-to-day work and none of them considered it an extra burden.13 The training was short (2 days followed by a 1 day refresher after 4 months) and therefore feasible on a large scale. However, an important component of the training process was the monthly half-day group supervision, which, for this study, was provided by experienced members of the research team.13 Regular and reliable training and supervision are essential for the success of community health worker-based programmes.32 Working with depressed individuals and their families in very poor settings can be stressful for the health workers; therefore, strong supervisory mechanisms need to be in place when scaling up a programme of this nature. This supervision could be in the form of peer groups in which health workers from each locality meet on a regular basis to discuss the families they are caring for. In our experience, such meetings in which health workers brainstorm for solutions and discuss their successes and failures in a supportive environment can be a sustainable model for supervision in places without resources to employ trained supervisors.13 Guidelines for such peer supervision would need to be incorporated into training.
Worldwide, the importance of mental health in achieving developmental goals, such as those endorsed by the UN's Millennium Development project has received increased recognition.33 However, this recognition is not matched by the development of an evidence-base for cost-effective interventions that can be scaled up in resource-poor settings. We believe this study suggests directions such interventions could take to make mental health an important component of public-health programmes.
Acknowledgments
The study was funded by the Wellcome Trust, UK, through a career development fellowship in tropical medicine awarded to AR. The fellowship was awarded through the Wellcome Trust Tropical Centre at the Liverpool School of Tropical Medicine and hosted by the University of Manchester and the Institute of Psychiatry, Rawalpindi. We would like to thank the Human Development Research Foundation, Islamabad for logistic assistance; the Ministry of Health, Government of Punjab, for their permission to do this study; Fareed Minhas at Rawalpindi for his unflinching support and encouragement; and Zaeem Haq for assistance with the development of training materials and supervision of the Lady Health Workers.
Contributors
AR conceived the study, developed the research design and wrote the first draft of the report. AR and FC supervised all aspects of study. AM and SS assisted with development of instruments and training material, and gathered data. CR analysed the data and tabulated the results. All authors helped to interpret findings and review the report. All authors have seen and approved the final version of the report to be published.
Conflict of interest statement
We declare that we have no conflict of interest.
References
- 1.Lopez A, Mathers C, Ezzati M, Jamison D, Murray C. Global burden of disease and risk factors. World Bank; Washington: 2006. [PubMed] [Google Scholar]
- 2.Mirza I, Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: systematic review. BMJ. 2004;328:794. doi: 10.1136/bmj.328.7443.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rahman A, Iqbal Z, Harrington R. Life events, social support and depression in childbirth: perspectives from a rural community in the developing world. Psychol Med. 2003;33:1161–1167. doi: 10.1017/s0033291703008286. [DOI] [PubMed] [Google Scholar]
- 4.Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R. Impact of maternal depression on infant nutritional status and illness: a cohort study. Arch Gen Psychiatry. 2004;61:946–952. doi: 10.1001/archpsyc.61.9.946. [DOI] [PubMed] [Google Scholar]
- 5.Rahman A, Bunn J, Lovel H, Creed F. Maternal depression increases infant risk of diarrhoeal illness—a cohort study. Arch Dis Child. 2007;92:24–28. doi: 10.1136/adc.2005.086579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Churchill R, Hunot V, Corney R. A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression. Health Technol Assess. 2001;5:1–173. doi: 10.3310/hta5350. [DOI] [PubMed] [Google Scholar]
- 7.Patel V, Araya R, Chatterjee S. Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet. 2007;370:991–1005. doi: 10.1016/S0140-6736(07)61240-9. [DOI] [PubMed] [Google Scholar]
- 8.Rojas G, Fritsch R, Solis J. Treatment of postnatal depression in low-income mothers in primary-care clinics in Santiago, Chile: a randomised controlled trial. Lancet. 2007;370:1629–1637. doi: 10.1016/S0140-6736(07)61685-7. [DOI] [PubMed] [Google Scholar]
- 9.Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370:878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- 10.Prince M, Patel V, Saxena S. No health without mental health. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 11.Karim S, Saeed K, Rana MH, Mubbashar M, Jenkins R. Pakistan mental health country profile. Int Rev Psychiatry. 2004;16:83–92. doi: 10.1080/09540260310001635131. [DOI] [PubMed] [Google Scholar]
- 12.Bhutta ZA, Thaver D, Akram DS, Khan M. A situation and program analysis of malnutrition among women and children in Pakistan: Can we break the time warp? In: Bhutta ZA, editor. Maternal and child health in Pakistan: challenges and opportunities. Oxford University Press; Oxford: 2004. pp. 151–172. [Google Scholar]
- 13.Rahman A. Challenges and opportunities in developing a psychological intervention for perinatal depression in rural Pakistan: a multi-method study. Arch Womens Ment Health. 2007;10:211–219. doi: 10.1007/s00737-007-0193-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Government of Pakistan . District Census Report of Rawalpindi: 1998. Population Census Organization, Government of Pakistan; Islamabad: 1999. [Google Scholar]
- 15.Ministry of Health, Government of Pakistan . National Programme for Family Planning and Primary Health Care. Ministry of Health, Government of Pakistan; 2007. [Google Scholar]
- 16.First MB, Spitzer RL, Gibbon M. Structured Clinical Interview for Axis I DSM-IV Disorders. Biometrics Research; NewYork: 1994. [Google Scholar]
- 17.Gorman LL, O'Hara MW, Figueiredo B. Adaptation of the structured clinical interview for DSM-IV disorders for assessing depression in women during pregnancy and post-partum across countries and cultures. Br J Psychiatry. 2004;46(suppl):s17–s23. doi: 10.1192/bjp.184.46.s17. [DOI] [PubMed] [Google Scholar]
- 18.Rahman A, Iqbal Z, Waheed W, Hussain N. Translation and cultural adaptation of health questionnaires. J Pak Med Assoc. 2003;53:142–147. [PubMed] [Google Scholar]
- 19.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Husain N, Bevc I, Husain M, Chaudhry IB, Atif N, Rahman A. Prevalence and social correlates of postnatal depression in a low income country. Arch Womens Ment Health. 2006;9:197–202. doi: 10.1007/s00737-006-0129-9. [DOI] [PubMed] [Google Scholar]
- 21.VonKorff M, Ustun TB, Ormel J, Kaplan I, Simon G. Self-report disability in an international primary care study of psychological illness. J Clin Epidemiol. 1996;49:297–303. doi: 10.1016/0895-4356(95)00512-9. [DOI] [PubMed] [Google Scholar]
- 22.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4th edn. APA; Washington, DC: 1994. [Google Scholar]
- 23.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52:30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 24.WHO . Physical status: the use and interpretation of anthropometry. Technical report series number 854. World Health Organization; Geneva: 1995. [PubMed] [Google Scholar]
- 25.Donner A, Klar N. Design and analysis of cluster randomization trials in health research. Hodder Arnold; London: 2000. [Google Scholar]
- 26.WHO Use and interpretation of anthropometric indicators of nutritional status. Bull World Health Organ. 1986;64:929–941. [PMC free article] [PubMed] [Google Scholar]
- 27.Gorstein J, Sullivan K, Yip R. Issues in the assessment of nutritional status using anthropometry. Bull World Health Organ. 1994;72:273–283. [PMC free article] [PubMed] [Google Scholar]
- 28.Rahman A, Creed F. Outcome of prenatal depression and risk factors associated with persistence in the first postnatal year: prospective study from Rawalpindi, Pakistan. J Affect Disord. 2007;100:115–121. doi: 10.1016/j.jad.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bolton P, Bass J, Neugebauer R. Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. JAMA. 2003;289:3117–3124. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- 30.Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82:866. [PMC free article] [PubMed] [Google Scholar]
- 31.Jacob KS, Sharan P, Mirza I. Mental health systems in countries: where are we now? Lancet. 2007;370:1061–1077. doi: 10.1016/S0140-6736(07)61241-0. [DOI] [PubMed] [Google Scholar]
- 32.WHO . Community health workers: what do we know about them? World Health Organization; Geneva: 2007. [Google Scholar]
- 33.Chisholm D, Flisher AJ, Lund C. Scale up services for mental disorders: a call for action. Lancet. 2007;370:1241–1252. doi: 10.1016/S0140-6736(07)61242-2. [DOI] [PubMed] [Google Scholar]