Abstract
Previous studies of the phenotype of developmental coordination disorder (DCD) have largely concentrated on population-based samples. The present study reports on an in-depth examination of a large Canadian family with eight children, after three children who were suspected to have DCD were referred for evaluation. Subsequently, five of the six children whose motor impairments could be measured, and the mother, met the diagnostic criteria for DCD as per the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders – fourth edition. The family members diagnosed with DCD showed remarkably similar profiles of motor difficulties. Additionally, the five children diagnosed with DCD had current speech articulation difficulties, with four of them having visited speech/language pathologists; the mother had a lateral lisp. More in-depth testing for three children revealed intact intellectual, academic and language comprehension skills. Three of the children diagnosed with DCD were obese. The present report highlights familial clustering of DCD and the presence of comorbid conditions in the affected children.
Keywords: Children, Comorbid developmental disorders, Developmental coordination disorder, Familial clustering
Abstract
Les études précédentes sur le phénotype du trouble d’acquisition de la coordination (TAC) ont surtout porté sur des échantillons en population. La présente étude fait état de l’examen approfondi d’une grande famille canadienne de huit enfants, après qu’on eut aiguillé trois enfants chez qui on présumait une TAC en vue de les faire évaluer. Par la suite, on a établi que cinq des six enfants chez qui on pouvait mesurer les atteintes motrices, ainsi que la mère, respectaient les critères diagnostiques de TAC conformément au Manuel diagnostique et statistique des troubles mentaux de l’American Psychiatric Association. Les membres de la famille chez qui on avait diagnostiqué le TAC présentaient des profils remarquablement similaires de troubles moteurs. De plus, les cinq enfants ayant un diagnostic de TAC présentaient des troubles de l’articulation du langage, et quatre avaient consulté un orthophoniste, tandis que la mère présentait un sigmatisme latéral. Des tests plus approfondis de trois enfants ont révélé des aptitudes intellectuelles, scolaires et de compréhension du langage intactes. Trois des enfants ayant un TAC diagnostiqué étaient obèses. Le présent rapport démontre le regroupement familial du TAC et la présence de troubles comorbides chez les enfants touchés.
Developmental coordination disorder (DCD) is a significant, pervasive neurodevelopmental disorder that negatively affects motor coordination in 5% to 6% of children, despite sufficient intelligence, motivation and education (1). In severe cases, this disabling condition can lead to academic, emotional, behavioural and health problems (2). The manifestations of DCD, as with other neurodevelopmental disorders, change with age. This is most likely due to neurological maturity, increased practice and experience, as well as the individual’s ability to compensate for his or her difficulties. DCD shows a high prevalence rate of comorbid childhood disorders, including learning disabilities (3), speech and language impairments (4,5), and high-blood pressure/attentional difficulties (6,7). The etiology of DCD is unknown; however, it is most likely multifactorial, with a genetic contribution similar to that for other childhood developmental disorders.
The phenotype of DCD has been studied infrequently, and results have often been confounded by the presence of other conditions that may be genetically linked, including attention-deficit hyperactivity disorders (ADHDs) and learning disabilities (8). To the extent of the authors’ knowledge, there have been two studies (6,9) of twins, but none looking directly at familial clustering of DCD. The likelihood of DCD occurring in more than one family member, and the resulting phenotypic profiles, has not previously been explored. The present study reports on an in-depth examination of a large Canadian family with eight children. Three of the eight children were referred for motor assessment because of suspected DCD. Permission was sought from the family to participate in a follow-up study that would examine the potential for familial clustering of DCD. The purpose of the present paper is to report the results of the additional medical and clinical investigations conducted with this family.
METHOD
Participants
The present family first came to the attention of the researchers through their participation in a research project designed to educate physicians about DCD (10). Ethical approval was provided by the research ethics board of the Children’s Hospital of Eastern Ontario (Ottawa, Ontario), and the family provided informed consent to take part in the investigations described below.
Procedure
Diagnosis of DCD
According to the Diagnostic and Statistical Manual of Mental Disorders – fourth edition (1), a diagnosis of DCD is appropriate when motor coordination difficulties are substantially below one’s given age and intelligence (criterion A); these difficulties impact negatively on daily living activities and/or academic achievement (criterion B); the difficulties are not due to a known medical condition nor a pervasive developmental disorder (criterion C); and if a mental retardation is evident, the motor coordination difficulties are in excess to those associated with mental retardation (criterion D). A more detailed review of the procedures involved in diagnosing DCD can be found in the article by Missiuna et al (11).
In the present study, a physician and occupational therapist collaborated in establishing whether the criteria for DCD were met in the six oldest children. The two youngest children, 20 months and six weeks of age, were too young to be assessed for motor impairment and motor skill delay. The criteria for DCD were clinically operationalized using standardized measures, and a diagnosis of DCD was given by the physician when all four criteria were met (for a detailed review of the specific procedures and information about the reliability and validity of the standardized measures, please refer to the article by Missiuna et al [12]). In an interview, the mother described herself as a ‘bull in a china shop’ and reported many of the characteristics commonly noted in individuals with DCD including difficulty learning to ride a bicycle and learning to drive, avoidance of physical activity and continuing challenges with everyday activities, such as climbing stairs or walking on uneven surfaces. Motor assessment was subsequently conducted with the mother, and a further investigation of the criteria needed for a diagnosis of DCD was completed. The interview with the father revealed no reported evidence of motor difficulties.
Assessment of comorbid conditions
The diagnosis of DCD concentrates on the individual’s motor coordination difficulties, in the absence of other medical explanations for them. It is well-accepted, however, that DCD is often accompanied by other developmental disorders (13). Speech and/or language impairment issues, attentional difficulties and learning disabilities are frequently reported (13). Due to the common occurrence of comorbid disorders, the present study provided additional assessment(s) by a speech/language pathologist (four children – III-2, III-4, III-5 and III-6) and a psychologist (three children – III-2, III-4 and III-5). Pertinent developmental histories for all of the children in this family were compiled through interviews with both parents and through a review of the physician’s medical record. The physician had cared for the children since birth, and was also the mother’s physician during her childhood. Height and weight measures were also collected for the seven eldest children to determine their body mass index (BMI) – a reliable indicator of weight status in children and adolescents (14). A majority of children with a BMI greater than the 95th percentile for their age are considered to be obese.
RESULTS
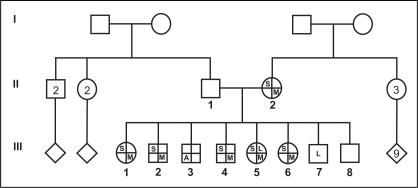
The family is comprised of two married parents and eight children (five males and three females), ranging in age from six weeks to 14 years. They are of English, Irish and French descent. The family structure and presence or absence of DCD and other comorbid conditions are summarized in Figure 1.
Figure 1).
Pedigree of family. Individual third generation (III)-8 was too young to be assessed, and individual III-7 demonstrated signs of early language delay. Squares denote males, circles denote females and diamonds denote either sex. The numbers in the symbols refer to the number of females, males or either sex. Roman numerals indicate generation and Arabic numerals indicate the individual within a generation. I First generation; II Second generation; A Attention-deficit disorder; L Current language delay; M Developmental coordination disorder; S Current speech articulation difficulties
Developmental information
Birth and medical history
All eight children were born by Caesarian section – one emergency procedure (child III-1), one complicated by intrauterine growth restriction and premature birth (child III-3, birthweight 4 lbs 5 oz), one believed to be secondary to placenta problems (child III-4) and one birth during which the mother was dangerously compromised (child III-7). Children III-1, III-5 and III-6 have histories of fractures after falls (child III-1, right foot and left wrist; child III-5, greenstick fracture of radius twice and child III-6, fracture of radius). All eight children are in good health, and medical issues are absent. The physical examination was unremarkable for minor malformations or facial dysmorphism. Chromosome analysis for III-2 was normal at the 550 to 650 band level, suggesting that a chromosomal abnormality is not contributing to the clinical expression of motor difficulties in the family.
Early motor and speech/language milestones:
Table 1 presents information concerning some of the major developmental milestones for the seven eldest children. Information concerning the youngest child, an infant, was not collected. Five of seven children did not crawl and their milestones for independent walking were on the late end of normal. Three children were reported to be late talkers, who also presented with preschool speech (articulation) delays severe enough to have warranted referral to a speech/language pathologist.
TABLE 1.
Developmental history of children
| Developmental history | Child III-1 | Child III-2 | Child III-3 | Child III-4 | Child III-5 | Child III-6 | Child III-7 | Child III-8 |
|---|---|---|---|---|---|---|---|---|
| Crawling | DNC | DNC | C | DNC | DNC | DNC | C | – |
| Independent walking age | 14 m | 16 m | 16 m | 22 m | 14 m | 18 m | 10 m | – |
| Late talker? | No | No | No | Yes | No | Yes | Yes | – |
| Preschool speech delay? | Yes | No | No | Yes | Yes | Yes | – | – |
Late talker – at two years of age, child had fewer than 50 expressive words and was not producing two-word combinations; preschool speech delay – speech delay identified by a speech/language pathologist, when the child was three to five years of age. III Third generation; C Crawled before walking; DNC Did not crawl
Diagnosis of DCD
Table 2 illustrates the results of assessments conducted with the individual members of the family, and indicates whether sufficient evidence was present to diagnose DCD. Five of the six children whose motor impairments were able to be measured, plus the mother were found to meet the Diagnostic and Statistical Manual of Mental Disorders – fourth edition criteria for a diagnosis of DCD (1). One non-DCD child (III-3) was well-coordinated, but has previously been diagnosed with ADHD.
TABLE 2.
Presence of Diagnostic and Statistical Manual of Mental Disorders – fourth edition diagnostic criteria across family members
| Age at testing (years) | Sex | Criterion A: Presence of motor impairment | Criterion B: Motor impairment impacts on academic and/or self-care areas* | Criterion C: Other medical explanations ruled out | Criterion D: Motor impairment not attributable to mental retardation | Meets all criteria for DCD? | Given DCD diagnosis? | |
|---|---|---|---|---|---|---|---|---|
| Mother | ||||||||
| II-2 | 41 | Female | <5th percentile BOT† | Yes | Yes | College diploma | Yes | Yes |
| Father | ||||||||
| II-1 | 41 | Male | No data | No difficulties | N/A | University degree | No | No |
| Children | ||||||||
| III-1 | 13 | Female | 10th percentile‡ | Yes | Yes | 75th percentile§ | Yes | Yes |
| III-2 | 11 | Male | <1st percentile‡ | Yes | Yes | 77th percentile§ | Yes | Yes |
| III-3 | 9 | Male | 45th percentile‡ | No difficulties | Yes | 75th percentile¶ | No | No |
| III-4 | 8 | Male | <1st percentile‡ | Yes | Yes | 68th percentile§ | Yes | Yes |
| III-5 | 5 | Female | 1st percentile‡ | Yes | Yes | 53rd percentile§ | Yes | Yes |
| III-6 | 4 | Female | 9th percentile‡ | Yes | Yes | 87th percentile§ | Yes | Yes |
As reported during clinical interview questions (30);
Percentile achieved on Bruininks-Oseretsky Test (BOT) II (motor test with adult norms) (31);
Percentile on Movement Assessment Battery for Children (motor test with norms for children four to 12 years of age) (32);
Kaufman Brief Intelligence Test – second edition (KBIT2) IQ composite score (33);
KBIT2-verbal IQ score (33). II Second generation; III Third generation; DCD Developmental coordination disorder
Assessment of comorbid conditions
Speech/language profiles
As shown earlier in Table 1, four of the five children who were diagnosed with DCD had positive histories for being late talkers (vocabulary of fewer than 50 words and no evidence of two-word combinations at two years of age) and/or displayed articulation concerns in the preschool period, as diagnosed by a speech/language pathologist. All four of these children received services from speech/language pathologists in the preschool and early school years. Child III-7 showed an early profile for being a late talker, with an expressive vocabulary of only five words at 20 months of age.
Table 3 presents the results of the standardized measures administered with the four children who were referred for further speech/language assessment. Current assessments of speech/language skills indicate low average articulation skills for child III-4 and child III-6, a moderate phonological impairment for child III-2, and a moderate phonological impairment with difficulties with rapid automatic naming for child III-5. The mother also reported a history of preschool speech and language delay, and today has a mild lateral lisp. There is no evidence of language comprehension difficulties in this family.
TABLE 3.
Standardized scores of interdisciplinary assessments of speech/language, adaptive, academic and cognitive functioning in child III-2, III-4, III-5 and III-6
| III-2 | III-4 | III-5 | III-6 | |
|---|---|---|---|---|
| Speech and language | ||||
| GFTA-2*, percentiles | 2 | 18 | 6 | 20 |
| CELF-4, core language | 126 | 114 | 96 | 102 |
| CTOPP, phonological awareness | 97 | 112 | 104 | CNS† |
| CTOPP, phonological memory | 109 | 94 | 85 | CNS† |
| CTOPP, rapid naming | 100 | 94 | 52 | CNS† |
| TEWL-2, basic | 110 | 117 | 112 | CNS† |
| TEWL-2, contextual | 124 | 97 | 114 | CNS† |
| Academic achievement (WIAT-II) | ||||
| Word reading | 81 | 89 | 99 | – |
| Reading comprehension | 111 | 109 | – | – |
| Numerical operations | 100 | 97 | 77 | – |
| Math reasoning | 114 | – | 88 | – |
| Adaptive functioning (ABAS-II) | ||||
| General adaptive composite | 73 | 66 | 90 | – |
| Intellectual functioning (WPPSI-III/WISC-IV) | ||||
| Full scale IQ | 100 | 90 | 90 | – |
| Verbal IQ/verbal comprehension | 112 | 89 | 95 | – |
| Performance IQ/perceptual reasoning | 100 | 109 | 91 | – |
| Processing speed | 83 | 80 | 85 | – |
| Working memory | 105 | 94 | – | – |
Because scores for the Goldman-Fristoe Test of Articulation – second edition (GFTA-2) are not normally distributed, the correspondence of standard scores to percentiles is not constant across age bands as with other normally distributed abilities; therefore, percentiles are reported for ease of comparison;
Could not score (CNS) because norms are outside the child’s age. Standardized scores have a mean of 100 and an SD of 15. III Third generation; ABAS-II Adaptive Behavior Assessment System – second edition; CELF-4 Clinical Evaluation of Language Fundamentals – fourth edition; CTOPP Comprehensive Test of Phonological Processing; TEWL-2 Test of Early Written Language – second edition; WIAT-II Wechsler Individual Achievement Test – second edition; WISC-IV Wechsler Intelligence Scale for Children – fourth edition; WPPSI-III Wechsler Preschool and Primary Scale of Intelligence – third edition
Psychological profiles
The results of the standardized measures administered by the psychologist with three of the children are outlined in Table 3. The profiles of all three (children III-2, III-4 and III-5) reflected age-appropriate intellectual functioning, although a common weakness was found for processing speed. Academic skills were age appropriate for all. The behavioural profiles were variable across family members, with child III-4 and child III-5 showing a high degree of behavioural difficulty in the home compared with child III-2. Trends in the parental responses on a behavioural rating scale (15) suggested that all three children showed a higher than normal degree of oppositional behaviours, anxiety shyness and emotional lability compared with age expectations. Moreover, in all three cases, behavioural problems were rarely identified by teacher ratings, suggesting that behavioural difficulties in these children are largely restricted to the home environment. Child III-3 was not assessed as part of the present study; he previously has had extensive psychological assessment and had been diagnosed with ADHD.
BMI findings
The height and weight measures, as well as the BMIs for the eldest six children are presented in Table 4. Based on these results, children III-5 (seven years and five months of age) and III-6 (five years of age) were considered to have a healthy weight. No norms were available for the two youngest children. Children III-1, III-2 and III-4 met the criteria for obesity. Child III-3, who has ADHD, met neither the criteria for DCD nor obesity.
TABLE 4.
Height, weight and body mass indexes (BMI) for the children
| Child | Age at time of measurement | Height (cm) | Weight (kg) | BMI (kg/m2) |
|---|---|---|---|---|
| III-1 | 14 years 6 months | 165 | 80.06 | 29.4 |
| >95th percentile | ||||
| III-2 | 12 years 0 months | 168 | 79.83 | 28.5 |
| >95th percentile | ||||
| III-3 | 11 years 4 months | 150 | 43.99 | 19.6 |
| 79th percentile | ||||
| III-4 | 9 years 3 months | 135 | 40.14 | 22.2 |
| >95th percentile | ||||
| III-5 | 7 years 5 months | 122 | 24.72 | 16.7 |
| 70.9th percentile | ||||
| III-6 | 5 years 0 months | 114 | 21.55 | 16.5 |
| 81.4th percentile |
III Third generation
DISCUSSION
For the individuals diagnosed with DCD in the present family, there is a general profile of impaired motor function in the context of intact intellectual, academic and language comprehension skills. However, the family members diagnosed with DCD have, or have previously demonstrated, comorbid speech and/or language difficulties. Multiple comorbid developmental disorders are consistently reported in children with DCD (12,13) with convincing evidence to show the coexistence of DCD and ADHD (6,7), motor impairment and speech and/or language impairments (4,5), and DCD and dyslexia (16). Interestingly, the difficulties seen in the family are primarily in speech sound production (articulation), although two of the younger children (III-5 and III-7) demonstrated additional expressive language-based difficulties. Investigations have found that when a child’s speech production skills are impaired, the impact on the child’s motor skills tends to be greater than that noted for a child with specific difficulties in language (17,18). In particular, speech may be considered a fine motor skill and may be affected in a way that is subtle but specific (such as a lisp for the /s/ or /sh/ sound) (19).
With regard to the intellectual ability of the children who were assessed, a common intellectual weakness is found for processing speed. While poor motor functioning is known to impact negatively on processing speed (20), the observed processing speed weakness is not believed to be purely motoric, but includes a visual processing component. A similar finding has been reported by Cummins et al (21).
The three eldest children who had DCD were classified as obese, and were reported by their mother to have a preference for sedentary activities. Children with DCD have been noted to be less likely to participate in physical activities, are at a greater risk for being overweight and/or obese and have low cardiorespiratory fitness (22). Child III-5 with DCD and a healthy weight had, as reported by her mother, also developed a predilection for sedentary activities and, thus, appeared to be at risk for becoming overweight. The children with DCD in the family showed early signs of obesity that, as suggested by recent literature (22), may be linked to withdrawal from or decreased levels of physical activity (23). The presence of DCD in the mother raises the question regarding the extent to which the environment (ie, family lifestyle) may also be a contributing factor to physical inactivity.
The genetic etiology of DCD and related disorders is not well understood, and the inheritance pattern is likely complex, with both genes and environmental factors playing a role. It is interesting to note that, when all family members were examined systematically, all of the female members met the diagnostic criteria for DCD. While many studies have suggested a higher incidence of DCD in male children, some authors have proposed that the difficulties of girls who have DCD are less likely to be noticed (24). Research studies into other childhood disorders, such as autism (25), specific language impairment (26), dyslexia (27) and ADHD (28) have focused on familial clustering to further examine genetic contribution. Recent studies have investigated a possible shared genetic basis for motor disorders and comorbid childhood developmental disorders. These include reading disability and motor ability (29), specific speech and language impairment and motor immaturity (17), as well as DCD and ADHD (6). It is likely that the etiology of DCD is as complex as for the other neurodevelopmental disorders, and there may be shared genetic causality for some of these syndromes. Identification and investigation of families, such as the present one, may provide valuable resources for future studies that will examine this hypothesis. Additional studies are needed to determine the incidence and spectrum of neurodevelopmental disorders in first-degree relatives of children with DCD.
TAKE HOME MESSAGES
The present family study provides evidence to suggest that DCD clusters in families are likely due to both genetic and environmental factors. As such, the following ‘take home messages’ for physicians in practice are proposed:
DCD is highly comorbid with other developmental conditions including speech and/or language impairments – if one is present, the other should be investigated.
Siblings of children diagnosed with DCD should be screened for signs of motor, speech and/or language impairments and attentional difficulties.
Both genetic and environmental factors may contribute to familial clustering of developmental conditions. When motor coordination difficulties are evident, a detailed family history is recommended as part of the medical assessment.
Acknowledgments
The authors thank the family for their willing cooperation. This research was funded by a Primary Health Care Transition Fund grant from the Ontario Ministry of Health and Long-Term Care.
REFERENCES
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th edn. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.Missiuna C, Gaines R, Soucie H, McLean J. Parental questions about developmental coordination disorder: A synopsis of current evidence. Paediatr Child Health. 2006;11:507–12. doi: 10.1093/pch/11.8.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jongmans MJ, Smits-Engelsman BC, Schoemaker MM. Consequences of comorbidity of developmental coordination disorders and learning disabilities for severity and pattern of perceptual-motor dysfunction. J Learn Disabil. 2003;36:528–37. doi: 10.1177/00222194030360060401. [DOI] [PubMed] [Google Scholar]
- 4.Gaines R, Missiuna C. Early identification: Are speech/language-impaired toddlers at increased risk for developmental coordination disorder? Child Care Health Dev. 2007;33:325–32. doi: 10.1111/j.1365-2214.2006.00677.x. [DOI] [PubMed] [Google Scholar]
- 5.Webster RI, Erdos C, Evans K, et al. The clinical spectrum of developmental language impairment in school-aged children: Language, cognitive, and motor findings. Pediatrics. 2006;118:e1541–9. doi: 10.1542/peds.2005-2761. [DOI] [PubMed] [Google Scholar]
- 6.Martin NC, Piek JP, Hay D. DCD and ADHD: A genetic study of their shared aetiology. Hum Mov Sci. 2006;25:110–24. doi: 10.1016/j.humov.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 7.Sergeant JA, Piek JP, Oosterlaan J. ADHD and DCD: A relationship in need of research. Hum Mov Sci. 2006;25:76–89. doi: 10.1016/j.humov.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Dewey D, Kaplan BJ, Crawford SG, Wilson BN. Developmental coordination disorder: Associated problems in attention, learning, and psychosocial adjustment. Hum Mov Sci. 2002;21:905–18. doi: 10.1016/s0167-9457(02)00163-x. [DOI] [PubMed] [Google Scholar]
- 9.Piek JP, Rigoli D, Pearsall-Jones JG, et al. Depressive symptomatology in child and adolescent twins with attention-deficit hyperactivity disorder and/or developmental coordination disorder. Twin Res Hum Genet. 2007;10:587–96. doi: 10.1375/twin.10.4.587. [DOI] [PubMed] [Google Scholar]
- 10.Gaines R, Missiuna C, Egan M, McLean J. Educational outreach and collaborative care enhances physician’s perceived knowledge about developmental coordination disorder. BMC Health Services Research. 2008;8:21. doi: 10.1186/1472-6963-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Missiuna C, Gaines R, Soucie H. Why every office needs a tennis ball: A new approach to assessing the clumsy child. Can Med Assoc J. 2006;175:471–7. doi: 10.1503/cmaj.051202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Missiuna C, Gaines R, McLean J, De Latte D, Egan M, Soucie H. Description of children who are identified by physicians as having developmental coordination disorder. Dev Med Child Neurol. 2008;50:839–44. doi: 10.1111/j.1469-8749.2008.03140.x. [DOI] [PubMed] [Google Scholar]
- 13.Visser J. Developmental coordination disorder: A review of research on subtypes and comorbidities. Hum Mov Sci. 2003;22:479–93. doi: 10.1016/j.humov.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 14.Department of Health and Human Services, Centers for Disease Control and Prevention, USA. BMI – body mass index: About BMI for children and teens (Version current at October 21, 2007).
- 15.Conners CK. Conners’ Parent Rating Scale – Revised (L) North Tonawanda: MHS; 2002. [Google Scholar]
- 16.Iversen S, Berg K, Ellertsen B, Tonnessen FE. Motor coordination difficulties in a municipality group and in a clinical sample of poor readers. Dyslexia. 2005;11:217–31. doi: 10.1002/dys.297. [DOI] [PubMed] [Google Scholar]
- 17.Bishop DV. Motor immaturity and specific speech and language impairment: Evidence for a common genetic basis. Am J Med Genet. 2002;114:56–63. doi: 10.1002/ajmg.1630. [DOI] [PubMed] [Google Scholar]
- 18.Visscher C, Houwen S, Scherder EJ, Moolenaar B, Hartman E. Motor profile of children with developmental speech and language disorders. Pediatrics. 2007;120:e158–63. doi: 10.1542/peds.2006-2462. [DOI] [PubMed] [Google Scholar]
- 19.Rodger S, Watter P, Marinac J, Woodyatt G, Ziviani J, Ozanne A. Assessment of children with developmental coordination disorder (DCD): Motor, functional, self-efficacy and communication abilities. New Zealand Journal of Physiotherapy. 2007;35:99–109. [Google Scholar]
- 20.Sigmundsson H, Hopkins B. Do ‘clumsy’ children have visual recognition problems? Child Care Health Dev. 2005;31:155–8. doi: 10.1111/j.1365-2214.2004.00463.x. [DOI] [PubMed] [Google Scholar]
- 21.Cummins A, Piek JP, Dyck MJ. Motor coordination, empathy, and social behaviour in school-aged children. Dev Med Child Neurol. 2005;47:437–42. doi: 10.1017/s001216220500085x. [DOI] [PubMed] [Google Scholar]
- 22.Cairney J, Hay JA, Faught BE, Hawes R. Developmental coordination disorder and overweight and obesity in children aged 9–14 y. Int J Obes (Lond) 2005;29:369–72. doi: 10.1038/sj.ijo.0802893. [DOI] [PubMed] [Google Scholar]
- 23.Bouffard M, Watkinson EJ, Thompson LP, Causgrove Dunn JL, Romanow SKE. A test of the activity deficit hypothesis with children with movement difficultes. Adapt Phys Activ Q. 1996;13:61–73. [Google Scholar]
- 24.Rivard LM, Missiuna C, Hanna S, Wishart L. Understanding teachers’ perceptions of the motor difficulties of children with developmental coordination disorder (DCD) Br J Educ Psychol. 2007;77:633–48. doi: 10.1348/000709906X159879. [DOI] [PubMed] [Google Scholar]
- 25.DeLong GR, Ritch CR, Burch S. Fluoxetine response in children with autistic spectrum disorders: Correlation with familial major affective disorder and intellectual achievement. Dev Med Child Neurol. 2002;44:652–9. doi: 10.1017/s0012162201002717. [DOI] [PubMed] [Google Scholar]
- 26.Lewis BA, Freebairn LA, Hansen A, Gerry Taylor H, Iyengar S, Shriberg LD. Family pedigrees of children with suspected childhood apraxia of speech. J Commun Disord. 2004;37:157–75. doi: 10.1016/j.jcomdis.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 27.Lyytinen H, Ahonen T, Eklund K, et al. Early development of children at familial risk for dyslexia – follow-up from birth to school age. Dyslexia. 2004;10:146–78. doi: 10.1002/dys.274. [DOI] [PubMed] [Google Scholar]
- 28.Slaats-Willemse D, Swaab-Barneveld H, De Sonneville L, Buitelaar J. Familial clustering of executive functioning in affected sibling pair families with ADHD. J Am Acad Child Adolesc Psychiatry. 2005;44:385–91. doi: 10.1097/01.chi.0000153227.34473.c7. [DOI] [PubMed] [Google Scholar]
- 29.Lyytinen H, Ahonen T, Eklund K, et al. Developmental pathways of children with and without familial risk for dyslexia during the first years of life. Dev Neuropsychol. 2001;20:535–54. doi: 10.1207/S15326942DN2002_5. [DOI] [PubMed] [Google Scholar]
- 30.Missiuna C, Pollack N, Egan M, DeLaat D, Gaines R, Soucie H. Enabling occupation through facilitating the diagnosis of developmental coordination disorder. Can J Occup Ther. 2008;75:26–34. doi: 10.2182/cjot.07.012. [DOI] [PubMed] [Google Scholar]
- 31.Bruininks R, Bruininks B. Bruininks-Oseretsky Test of Motor Proficiency. 2nd edn. Circle Pines: AGS Publishing (American Guidance Services); 2005. [Google Scholar]
- 32.Henderson SE, Sugden DA. Movement Assessment Battery for Children. London: The Psychological Corporation; 1992. [Google Scholar]
- 33.Kaufmann AS, Kaufmann NL. Kaufman Brief Intelligence Test. 2nd edn. Circle Pines: American Guidance Service Inc; 2004. [Google Scholar]