Abstract
The intestinal epithelium is in direct contact with a vast microbiota, yet little is known about how epithelial cells defend the host against the heavy bacterial load. To address this question we studied Paneth cells, a key small intestinal epithelial lineage. We found that Paneth cells directly sense enteric bacteria through cell-autonomous MyD88-dependent toll-like receptor (TLR) activation, triggering expression of multiple antimicrobial factors. Paneth cells were essential for controlling intestinal barrier penetration by commensal and pathogenic bacteria. Furthermore, Paneth cell-intrinsic MyD88 signaling limited bacterial penetration of host tissues, revealing a role for epithelial MyD88 in maintaining intestinal homeostasis. Our findings establish that gut epithelia actively sense enteric bacteria and play an essential role in maintaining host-microbial homeostasis at the mucosal interface.
Keywords: commensal bacteria, epithelium, innate immunity, intestine, toll-like receptors
Humans harbor nearly 100 trillion intestinal bacteria that are essential for health. Millions of years of coevolution have molded this human-microbe interaction into a symbiotic relationship in which gut bacteria make essential contributions to human nutrient metabolism and in return occupy a nutrient-rich environment (1). However, bacterial invasion of tissue can result in breakdown of this symbiotic association and lead to pathologies such as inflammatory bowel disease (2). Intestinal epithelia constitute the major interface between the microbiota and internal host tissues. Despite the enormous numbers of commensal bacteria, microbial incursions across mucosal surfaces are relatively rare, suggesting that intestinal epithelia harbor highly effective mechanisms for controlling microbial interactions with the host mucosal interface. However, little is known about how intestinal epithelial cells maintain homeostasis with vast, complex populations of enteric bacteria.
The Paneth cell is a specialized small intestinal epithelial lineage that resides at the base of crypts of Lieberkühn and contributes to intestinal innate immunity by secreting a diverse repertoire of antimicrobial proteins (3). Several antimicrobial factors in Paneth cells are expressed under the control of indigenous microorganisms (4, 5). In addition, ex vivo studies on isolated small intestinal crypts indicate that secretion of antimicrobial products is triggered by bacterial signals (3). However, it is not yet clear whether Paneth cells detect bacteria through cell-autonomous mechanisms. Furthermore, although Paneth cells are known to secrete abundant antimicrobial factors (3), the in vivo functional role of Paneth cells in maintaining homeostasis with commensal bacterial populations has not been established.
In this report, we show that Paneth cells detect enteric bacteria through cell-autonomous MyD88 activation, triggering expression of multiple antimicrobial factors. We show that Paneth cell-intrinsic MyD88 signaling limits bacterial penetration of host tissues, disclosing a role for epithelial MyD88 in maintaining intestinal homeostasis. Using a Paneth cell lineage ablation model, we further reveal that Paneth cells are essential for controlling intestinal barrier penetration by commensal and pathogenic bacteria. These findings elucidate an important in vivo function of Paneth cells and yield general insight into how intestinal epithelial cells maintain homeostasis with the intestinal microbiota.
Results
Intestinal Microbiota Activate Expression of a MyD88-Dependent Antimicrobial Program in Paneth Cells.
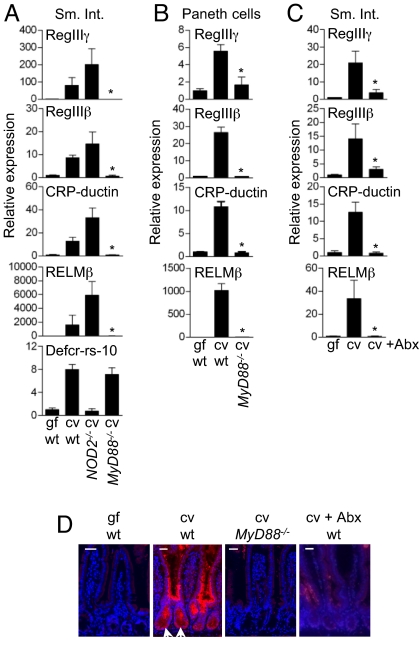
We previously performed a genome-wide expression analysis to assess bacterial regulation of Paneth cell antimicrobial responses (5). Our analysis revealed that bacteria orchestrate expression of a complex antimicrobial transcriptional program that includes RegIIIγ, an antimicrobial factor that binds peptidoglycan and is expressed in both Paneth cells and enterocytes (5) (Fig. 1D); RegIIIβ, which is closely related to RegIIIγ and binds peptidoglycan (H. L. Cash and L.V.H., unpublished data); CRP-ductin, which agglutinates Gram-positive and Gram-negative bacteria (7); the inflammatory modulator resistin-like molecule β (RELMβ) (8, 9); and several members of the α-defensin family of antimicrobial peptides.
Fig. 1.
Intestinal microbiota activate expression of a MyD88-dependent antimicrobial program in Paneth cells. (A and B) Expression of key antimicrobial effectors is MyD88 dependent but NOD2 independent. Gene expression was quantitated by real-time quantitative PCR (Q-PCR) of (A) small intestines (Sm. Int.) of germ-free (gf) wild-type (wt), conventional (cv) wt, cv Nod2−/−, and cv MyD88−/− mice (3–4 mice per group), or of (B) small intestinal Paneth cells isolated by laser capture microdissection. (C) Q-PCR analysis of small intestines of cv mice treated with antibiotics (Abx) to deplete the normal microbiota (3–4 mice per group). (D) Visualization of RegIIIγ expression in small intestinal epithelium. Immunostaining with anti-RegIIIγ antiserum reveals expression of RegIIIγ (red) in both Paneth cells (indicated by arrows) and enterocytes of cv wt mice. Sections were counterstained with Hoechst dye (blue). (Scale bars: 50 μm.) All Q-PCR assays were run in triplicate and are shown as mean values normalized to 18S ribosomal RNA. Relative expression levels were calculated relative to gf controls. Error bars indicate ± SEM. *P < 0.05 compared with cv wt.
To delineate the host factors that govern expression of this antimicrobial transcriptional program, we analyzed gene-targeted mice that are deficient in the sensing of conserved microbe-associated molecular patterns. At least two protein families recognize microbial products in mice and humans: the cytoplasmic NOD-like proteins and the membrane bound toll-like receptors (TLRs). NOD2 regulates Paneth cell expression of key α-defensins, including Defcr-rs10 (10). Examination of Nod2−/− mice revealed that, unlike Defcr-rs10, small intestinal expression of RegIIIγ, RegIIIβ, CRP-ductin, and RELMβ was NOD2 independent (Fig. 1A). In contrast, mice lacking the TLR signaling adaptor MyD88 revealed that expression of these genes was MyD88 dependent (Fig. 1A), consistent with previous findings of MyD88-dependent RegIII expression in the small intestine (11, 12). We further established that MyD88-dependent expression of these transcripts occurred in Paneth cells recovered by laser capture microdissection (Fig. 1B). Treatment of wild-type conventional mice with a mixture of broad-spectrum antibiotics (13) showed that expression of the MyD88-dependent antimicrobial program was reversible upon partial microflora depletion (Fig. 1 C and D). Thus, intestinal microbes elicit a dynamic and reversible MyD88-dependent antimicrobial expression program in Paneth cells that is distinct from the NOD2-dependent antimicrobial response.
Paneth Cells Directly Sense Enteric Bacteria Through Cell-Autonomous MyD88 Activation.
MyD88 is involved in signaling through TLRs, the IL-1 receptor (IL-1R), and the IL-18 receptor (IL-18R) (14). Paneth cells express several TLRs, including TLR2, 4, 5, and 9 (15–17). Although we were unable to identify a TLR-deficient mouse that phenocopied the profoundly reduced antimicrobial factor expression observed in MyD88−/− mice, two lines of evidence suggest that TLRs, rather than IL-1R and IL-18R, direct expression of MyD88-dependent antimicrobial factors. First, we directly addressed the possibility that IL-1R or IL-18R might direct antimicrobial gene expression by analyzing Caspase-1−/− mice, which are unable to produce active forms of IL-1β and IL-18 (18). We detected no statistically significant differences in RegIIIγ, RegIIIβ, CRP-ductin, and RELMβ transcript levels between conventional wild-type and Caspase-1−/− mice [supporting information (SI) Fig. S1A], indicating that IL-1R and IL-18R do not direct MyD88-dependent antimicrobial responses. Second, oral administration of the TLR4 ligand lipopolysaccharide (LPS) to germ-free mice elicited dose-dependent expression of RegIIIγ, RegIIIβ, and RELMβ (Fig. S1B). Together, these findings suggest that TLRs, rather than IL-1R or IL-18R, direct expression of the MyD88-dependent antimicrobial response.
We next used this MyD88-dependent antimicrobial expression program to investigate whether Paneth cells directly detect bacteria in vivo or whether other mucosal cells detect and relay bacterial signals to Paneth cells. Prior studies have established a role for hematopoietic cell MyD88 in relaying bacterial signals to intestinal epithelial cells during intestinal injury (13, 19). However, adoptive transfer of wild-type bone marrow into lethally irradiated MyD88−/− mice was insufficient to restore expression of the MyD88-dependent antimicrobial program (12) (Fig. S2), indicating that MyD88 signaling in bone marrow-derived cells does not govern epithelial antimicrobial factor expression. However, these findings were consistent with three possibilities. First, it was possible that nonhematopoietic, nonepithelial cells such as myofibroblasts (20) could detect and relay bacterial signals to Paneth cells. Second, enterocytes could capture and relay bacterial signals to Paneth cells. Third, Paneth cell-autonomous MyD88 activation could govern antimicrobial program expression.
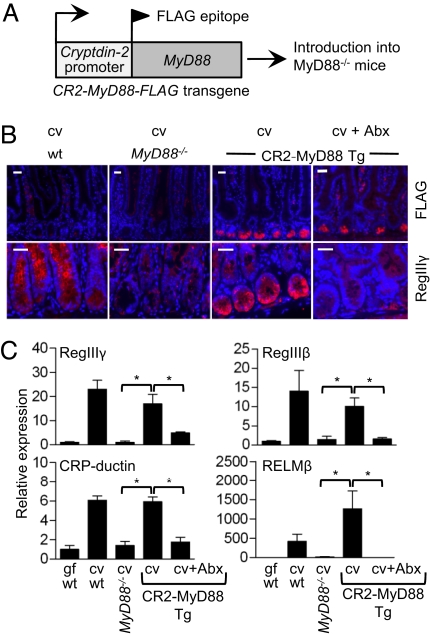
To directly test whether Paneth cells sense bacteria through cell-autonomous mechanisms, we performed a gain-of-function genetic experiment. Here we used the Paneth cell-specific cryptdin-2 (CR2) promoter (21) to direct expression of a FLAG-tagged MyD88 transgene, and then crossed these transgenic mice to MyD88−/− mice to yield a mouse model (CR2-MyD88 Tg) in which Paneth cells were the sole cell lineage expressing MyD88 (Fig. 2Aand Fig. S3). MyD88 expression in Paneth cells was sufficient to restore RegIIIγ expression in the MyD88−/− background (Fig. 2 B and C). Although RegIIIγ is expressed in both Paneth cells and enterocytes in wild-type conventionally reared mice, its expression was restored specifically in Paneth cells (Fig. 2B). Quantitation of RegIIIγ, RegIIIβ, CRP-ductin, and RELMβ transcripts revealed that the broader MyD88-dependent antimicrobial transcriptional program was also restored through Paneth cell-specific MyD88 expression (Fig. 2C). Antimicrobial factor expression in the transgenic model was reversible upon antibiotic treatment (Fig. 2 B and C). This was not due to reversal of transgene expression, as the FLAG-tagged MyD88 was detected in Paneth cells from antibiotic-treated mice (Fig. 2B). Thus, activation of transgenic MyD88 requires bacteria and is not due to nonspecific autoactivation through overexpression of MyD88. Together, these findings show that Paneth cells directly detect intestinal bacteria via cell-autonomous MyD88 activation, revealing a direct dialogue between enteric bacteria and the Paneth cell lineage of the gut epithelium.
Fig. 2.
Paneth cells directly sense enteric bacteria through cell-autonomous MyD88 activation. (A) A MyD88 transgene with an N-terminal FLAG epitope fusion was cloned downstream of the Paneth cell-specific Cryptdin-2 (CR2) promoter and introduced into MyD88−/− mice. (B) FLAG-MyD88 (red) and RegIIIγ (red) are expressed in small intestinal crypts of transgenic mice (on a MyD88−/− background, designated CR2-MyD88 Tg mice). RegIIIγ expression in the transgenic mice is reversible by partial depletion of the microflora through administration of broad-spectrum antibiotics (Abx). Sections were counterstained with Hoechst dye (blue). Arrows indicate Paneth cells. (Scale bars: 50 μm.) (C) Expression of antimicrobial factors was quantitated in small intestines of germ-free (gf) wild-type (wt), conventional (cv) wt, cv MyD88−/−, cv CR2-MyD88 Tg mice, or cv Abx-treated transgenic mice. All Q-PCR assays were performed as described in Fig. 1. Error bars indicate ± SEM. *P < 0.05.
Paneth Cell-Intrinsic MyD88 Expression Is Sufficient to Limit Mucosal Penetration by Commensal and Pathogenic Bacteria.
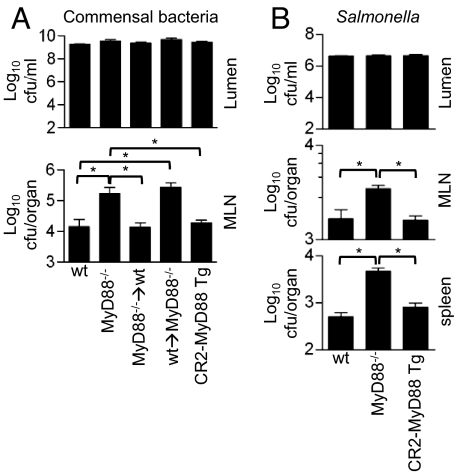
Our finding that Paneth cells directly sense bacteria through MyD88-dependent pathways suggested that intestinal epithelial MyD88 might play a key functional role in maintaining homeostasis with the commensal microbiota. To investigate this role, we further examined wild-type and MyD88−/− mice. Conventionally reared wild-type and MyD88−/− mice revealed no significant differences in luminal densities of commensal bacteria (Fig. 3A). However, bacteria that localize near the apical surface of epithelial cells are sampled by dendritic cells (DCs) and translocated alive to mesenteric lymph nodes (MLN) (22–24) and we reasoned that perhaps MyD88-dependent antimicrobial factors specifically modulate the numbers of bacteria that closely associate with the mucosal surface and are therefore available for uptake to MLN. Consistent with this idea, we recovered ≈10-fold more bacteria from the MLN of MyD88−/− mice as compared with wild-type mice (Fig. 3A). The difference in MLN numbers was not due to MyD88 deficiency in bone marrow-derived cells, as transfer of MyD88−/− bone marrow into wild-type recipients did not result in increased numbers of MLN bacteria relative to wild-type mice (Fig. 3A). In contrast, transfer of wild-type bone marrow into MyD88−/− recipients resulted in numbers of MLN bacteria that were similar to MyD88−/− mice, suggesting that epithelial MyD88 was necessary to limit bacterial translocation to MLN (Fig. 3A). To determine whether expression of MyD88 in the epithelium was sufficient to limit commensal penetration, we examined the CR2-MyD88 Tg mice (on the MyD88−/− background). Transgenic expression of MyD88 in Paneth cells restored wild-type MLN numbers (Fig. 3A), indicating that expression of MyD88 in a single epithelial lineage is sufficient to limit commensal penetration to MLN. It is unlikely that these differences are due to differences in microflora composition among different strains, as we took care to cohouse mice (wt, MyD88−/−, CR2-MyD88 Tg mice, and bone marrow chimeric mice) for 1 week before sacrifice.
Fig. 3.
Paneth cell-intrinsic MyD88 expression is sufficient to limit mucosal penetration by commensal and pathogenic bacteria. (A) Commensal bacteria were quantitated in small intestinal lumen and MLN from conventionally reared wt, MyD88−/−, bone marrow chimeric mice, or CR2-MyD88 transgenic mice on the MyD88−/− background (CR2-MyD88 Tg). MyD88−/− → wt, MyD88−/− donor to wt recipient; wt → MyD88−/−, wild-type donor to MyD88−/− recipient. (B) Conventionally raised wt, MyD88−/−, or CR2-MyD88 Tg mice were orally inoculated with 108 cfu of S. typhimurium. Numbers of S. typhimurium in small intestine, MLN, and spleen were quantitated after 48 h. n = 3–4 mice per group, representative of two experiments.
To assess whether Paneth cell MyD88 could also limit pathogen penetration and dissemination, we orally inoculated conventionally reared wild-type, MyD88−/−, and CR2-MyD88 Tg mice with Salmonella typhimurium. After 48 h luminal Salmonella colonization densities were ≈3 logs lower than those of the conventional flora (Fig. 3B), reflecting the fact that the commensal microbiota provides colonization resistance against Salmonella (25). Numbers of luminal Salmonella did not differ among wild-type, MyD88−/−, and CR2-MyD88 Tg mice but increased numbers of Salmonella penetrated to MLN and spleen in MyD88−/− as compared with wild-type mice. Paneth cell-specific expression of MyD88 restored MLN numbers to wild-type levels and significantly reduced the numbers of splenic bacteria (Fig. 3B). The decrease in spleen bacteria was not due to altered bacterial killing, as similar numbers of bacteria were recovered from the spleens of MyD88−/− (8 × 106 ± 3 × 106 CFU) and CR2-MyD88 Tg mice (9 × 106 ± 5 × 106 CFU) following intraperitoneal injection of Salmonella. Thus, expression of MyD88 in Paneth cells is sufficient to limit Salmonella penetration across the mucosal barrier and systemic dissemination.
These findings indicated that expression of MyD88 in a single small-intestinal epithelial lineage was sufficient to limit penetration of commensals and pathogens across the epithelial barrier. Though Salmonella elicited Paneth cell antimicrobial responses when introduced into germ-free mice (Fig. S4A), the relatively low Salmonella numbers in conventional mice were insufficient to stimulate MyD88-dependent responses in excess of the basal levels elicited by the commensal microbiota (Fig. S4B). Thus, the protection afforded against Salmonella penetration and dissemination is likely the result, in part, of commensal stimulation of MyD88. This suggests that commensals protect their host against pathogen invasion not only through colonization resistance but also by activating MyD88-dependent signaling in the host epithelium.
Paneth Cells Are Essential for Limiting Mucosal Penetration by Commensal and Pathogenic Bacteria.
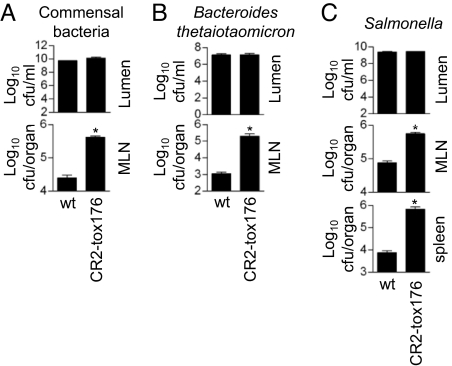
These findings suggested that a key function of intestinal epithelial cells is to actively limit bacterial penetration of the mucosal barrier. To test this idea, we examined a transgenic mouse model in which Paneth cells are specifically ablated by expressing a diphtheria toxin fragment (tox176) under the control of the cryptdin-2 promoter (21). Although isolated CR2-tox176 crypts show reduced antimicrobial peptide secretion (3), the mice are overtly healthy, harbor a normal distribution of gut-associated lymphoid tissue, and exhibit no differences in the numbers of luminal bacteria (21) (Fig. 4A). Given our finding that Paneth cell-intrinsic MyD88 limits bacterial penetration of the mucosal barrier, we hypothesized that Paneth cell-deficient (CR2-tox176) mice might exhibit increased bacterial penetration of the mucosa. Though conventional CR2-tox176 mice and their wild-type littermates harbored similar luminal bacterial loads, we recovered higher numbers of bacteria from CR2-tox176 MLNs (Fig. 4A). Similarly, oral challenge of germ-free CR2-tox176 mice and their wild-type littermates with B. thetaiotaomicron resulted in ≈200-fold more MLN bacteria in CR2-tox176 mice (Fig. 4B). This was not due to higher luminal bacterial loads, as luminal numbers were similar between the two groups (Fig. 4B). No bacteria were recovered from the spleens of either CR2-tox176 or wild-type mice. Thus, Paneth cells are essential for limiting translocation of commensals across the intestinal barrier, but have little impact on overall small intestinal bacterial load.
Fig. 4.
Paneth cells are essential for limiting mucosal penetration by commensal and pathogenic bacteria. (A) Commensal bacteria were quantitated in conventionally reared Paneth cell-deficient mice (CR2-tox176) transgenic mice and their wild-type (wt) littermates. (B and C) Germ-free CR2-tox176 mice and their wt littermates were orally challenged with 108 cfu of (B) Bacteroides thetaiotaomicron or (C) S. typhimurium, and bacterial numbers were quantitated 48 h later. No commensals or B. thetaiotaomicron were recovered from spleens of wt or CR2-tox176 mice. Error bars indicate ± SEM. n = 3–4 mice per group, representative of two experiments.
To determine whether Paneth cells also play an essential role in limiting pathogen penetration, we challenged germ-free CR2-tox176 mice orally with S. typhimurium. Though luminal colonization levels were similar 48 h later, we recovered ≈7-fold more Salmonella from CR2-tox176 as compared with wild-type MLN. Moreover, 90-fold more Salmonella were recovered from the spleens of CR2-tox176 as compared with wild-type mice (Fig. 4C), revealing an essential role for Paneth cells in limiting pathogen translocation and dissemination.
Discussion
The intestinal epithelium is the primary barrier between the vast enteric microbial community and internal host tissues. However, little is known about how epithelial cells regulate interactions with the intestinal microbiota. In this study we gained new insight into this question by examining Paneth cells, a key small intestinal epithelial lineage. Our results reveal that Paneth cells detect enteric bacteria through cell-autonomous MyD88 activation, triggering expression of a complex antimicrobial program that includes RegIIIγ, RegIIIβ, CRP-ductin, and RELMβ. We found that Paneth cell-intrinsic MyD88 activation limits translocation and dissemination of microbes across the mucosal barrier, while having little impact on luminal microbial numbers. Finally, by analyzing mice that lack Paneth cells through specific lineage ablation, we have uncovered an essential role for Paneth cells in controlling mucosal penetration by both commensal and pathogenic bacteria.
Our findings suggest a previously unappreciated role for epithelial MyD88 in maintaining host-microbial homeostasis at the mucosal interface. Paneth cell-specific expression of a MyD88 transgene restored expression of a complex antimicrobial program in MyD88-deficient mice and limited translocation of commensals and pathogens across the mucosal barrier. Moreover, our findings suggest that the protection afforded against Salmonella dissemination results in part from stimulation of epithelial MyD88 by commensals. Thus, commensals provide protection against pathogen invasion through at least two mechanisms: colonization resistance (26) and stimulation of MyD88 in host epithelial cells.
Although our study specifically addresses the function of Paneth cell MyD88, several lines of evidence suggest that enterocyte MyD88 also contributes to mucosal homeostasis. First, enterocytes express MyD88-dependent antimicrobial factors, including RegIIIγ. Second, Paneth cell-specific MyD88 expression restored RegIIIγ expression only in Paneth cells, but did not restore its expression in enterocytes. This shows that Paneth cell MyD88 signals are not relayed to enterocytes, and instead suggests that enterocytes harbor their own cell-intrinsic bacterial sensing mechanisms. It thus seems likely that enterocyte MyD88 is also important for maintaining homeostasis with enteric bacteria.
Our analysis of Paneth cell-deficient mice (CR2-tox176) has revealed an essential role for Paneth cells in maintaining homeostasis with enteric microbes. Absence of Paneth cells was associated with enhanced penetration of commensals to MLN. Additionally, we observed increased dissemination of pathogenic Salmonella to spleen. These findings are consistent with prior studies showing that Paneth cell α-defensins protect against Salmonella-induced pathogenicity (27, 28). Thus, Paneth cells play an active role in limiting penetration of both commensals and pathogens across the epithelial barrier.
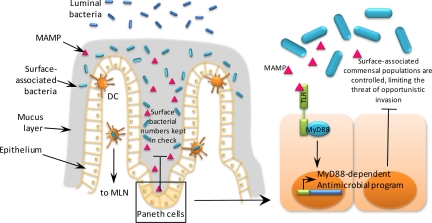
A key finding is that Paneth cell MyD88 expression (gain of function) and Paneth cell ablation (loss of function) both modulate numbers of translocating bacteria but not luminal bacterial densities. A plausible model to explain these observations is that Paneth cell antimicrobial factors regulate the numbers of bacteria that are closely apposed to the mucosal surface (Fig. 5). As bacteria must become mucosa associated before uptake by DCs for translocation to MLN or before invasion into the lamina propria, Paneth cells could limit bacterial penetration of host tissues by controlling the numbers of mucosa-associated bacteria. This idea is consistent with the fact that secreted Paneth cell antibacterial factors are retained by the mucus layer that overlies the intestinal epithelium, but are virtually absent from luminal content (29). This relatively impermeable mucus barrier may thus define a confined space that allows the host to specifically monitor and regulate bacteria that are in close contact with the intestinal surface. This model is further supported by our finding that Paneth cells sense bacteria that closely associate with the mucosal surface (resulting in activation of MyD88-dependent antimicrobial responses), but are insensitive to overall luminal bacterial loads (Fig. S5). Together, our findings suggest that intestinal host-microbial relationships are negotiated through local interactions at the mucosal interface, and that Paneth cells dictate the outcome of these interactions by actively sensing and limiting bacterial population densities at the mucosal surface. By specifically controlling bacterial interactions with the mucosal surface, Paneth cells may also avoid disrupting the composition of luminal microbial communities that are crucial for host metabolic health.
Fig. 5.
Model of small intestinal Paneth cell function. We have shown that Paneth cells directly sense enteric bacteria through cell-autonomous MyD88 activation and limit bacterial penetration of the mucosal surface. MyD88-dependent sensing triggers expression of a complex antimicrobial program that could function to limit the numbers of bacteria that localize at the mucosal surface, in or beneath the mucus layer. This would in turn limit the numbers of bacteria that are translocated to mesenteric lymph nodes (MLN) via dendritic cells (DCs). In the same way, Paneth cells could inhibit pathogen access to surface niches, thus accounting for the essential role of Paneth cells in limiting mucosal penetration and dissemination of Salmonella.
Our findings may provide insight into pathologic features of inflammatory bowel diseases (IBD), a group of chronic intestinal inflammatory disorders whose exact causes remain obscure. Enhanced mucosal expression of Reg lectin family members is frequently observed in IBD patients (30). Given the findings of this study, we suggest that elevated Reg expression in IBD mucosa may signify increased mucosal adherence by enteric bacteria, which could initiate and perpetuate mucosal inflammation. This idea is consistent with the observation of increased numbers of mucosa-adherent bacteria in IBD patients (31).
In conclusion, by studying a key intestinal epithelial cell lineage, we have revealed a vital role for gut epithelia in regulating host-bacterial interactions at the mucosal interface. Epithelial innate immune function is thus likely to be crucial for maintaining symbiotic relationships with the enteric microbiota and for protecting against pathogenic bacterial challenge. We believe that the findings in this study will provide a framework for considering the functions of other epithelial cell lineages in the intestine and at other mucosal sites.
Materials and Methods
Mice.
Conventionally reared wild-type and MyD88−/− C57BL/6 mice were maintained in the barrier facility at the University of Texas Southwestern Medical Center at Dallas. NOD2−/− mice on the C57BL/6 background were obtained from Jackson Laboratories and were bred in the barrier facility at University of Texas Southwestern (UT Southwestern). Caspase-1−/− mice were obtained from Dr. Richard Flavell (18). All experiments were performed using protocols approved by the Institutional Animal Care and Use Committees of the UT Southwestern Medical Center. All conventional mice within an experiment were cohoused for 1 week to normalize the microflora among the different mouse strains. This was done either by placing mice into a single cage, or in the case of experiments involving larger numbers of mice, by daily mixing of bedding among multiple cages. Germ-free C57BL/6 mice were maintained in plastic gnotobiotic isolators as previously described (5).
Generation of CR2-MyD88 Transgenic Mice.
FLAG-MyD88 was amplified using primers containing BglII restriction sites (Table S1) from pCMV-FLAG-MyD88 (a kind gift of R. Medzhitov). The TAg fragment of pCR-TAg-hGH (21) was removed by digestion with BamHI and replaced with the BglII-digested FLAG-MyD88 fragment. Correct orientation of the cloned FLAG-MyD88 was determined by restriction mapping and sequencing. This yielded pCR2-FLAG-MyD88-hGH, which contained FLAG-MyD88 under the control of nucleotides −6,500 to 134 of the mouse Cryptdin-2 (CR2) gene (32) and immediately upstream of hGH+3 to +2150. The hGH sequences enhance the efficiency of transgene expression; however, hGH protein is not produced from the RNA transcript (21). A 10.2 kb fragment containing CR2-FLAG-MyD88-hGH was released from pCR2-FLAG-MyD88-hGH by digestion with EcoRI, and was used to generate transgenic mice (UT Southwestern Transgenic Core Facility). The CR2-FLAG-MyD88 mice were backcrossed to MyD88−/− mice. Expression of the MyD88 transgene was assessed by RT-PCR using specific primers (Table S1). Endogenous MyD88 genotype was verified using the primers directed against the MyD88 gene (Table S1).
Laser Capture Microdissection.
Cryosections 7 μm thick were cut from OCT-embedded small intestine using previously published protocols (33). Paneth cells were harvested by laser capture microdissection using an Arcturus PixCell II system and CapSure HS LCM caps (Arcturus) as previously described (5). Total RNA was prepared from captured cells using the Arcturus PicoPure RNA Isolation Kit, and was used as template for cDNA synthesis as previously described (5).
Quantitative PCR (Q-PCR).
Total RNA was isolated from small intestinal tissues using the Qiagen RNeasy RNA Isolation Kit and was used to synthesize cDNA. SYBR green-based Q-PCR used Stratagene Brilliant Q-PCR Master Mix and specific primers (Table S1). Signals were normalized to 18S rRNA levels within each sample using published primers (5), and normalized data were used to quantitate relative levels of gene expression using ΔΔCt analysis.
Immunohistochemistry.
Bouins-fixed, paraffin-embedded tissue sections were stained with anti-RegIIIγ antiserum (6) or preimmune serum and detected using a goat anti-rabbit IgG Cy3 conjugate (Biomeda). Tissues were counterstained with Hoechst dye. Anti-FLAG immunohistochemistry was carried out using a polyclonal anti-FLAG antibody raised in rabbits (Sigma) and goat anti-rabbit IgG Cy3 conjugate. All images were captured using a 250 ms exposure.
Depletion of the Intestinal Microflora Through Antibiotic Treatment.
Age-matched conventional C57B6 wild-type and CR2-MyD88 Tg mice were given ampicillin (1g/L; Sigma), vancomycin (500 mg/L; Sigma), neomycin sulfate (1g/L; Sigma), and metronidazole (1g/L; Sigma) in drinking water for 4 weeks as described previously (13). Depletion of the commensal microbiota was verified by aerobic and anaerobic culture of feces. At the end of the treatment, mice were killed and intestinal tissues were snap frozen for RNA extraction or prepared for immunohistochemistry. Depletion of the small intestinal microbiota was verified by aerobic and anaerobic culture of luminal contents following sacrifice.
Bacterial Enumeration in Conventional Mice.
Age-matched conventional C57B6 wild-type, Myd88−/−, and CR2-MyD88 Tg mice were cohoused together in the same cage for 1 week to minimize microflora composition differences among the different mouse strains and among mice that had been housed in different cages. The mice were killed, and small intestinal colonization levels were measured by dilution plating of luminal contents. Bacterial levels in spleen and mesenteric lymph nodes were determined by dilution plating of homogenized tissue. For additional information, see SI Materials and Methods.
Supplementary Material
Acknowledgments.
We thank A. Neish and L. Comstock for providing bacterial strains, R. Medzhitov for the MyD88 transgene, R. Flavell for mice, and C. Pasare and F. Yarovinsky for helpful discussions. S. Murray, H. Ramos, C. Hinkley, and T. Troutman provided invaluable assistance with experiments. This work was supported by the National Institutes of Health Grants DK070855 (to L.V.H.) and DK70867 (to L.E.), the Crohn's and Colitis Foundation of America (L.V.H.), a Burroughs Wellcome Foundation New Investigators in the Pathogenesis of Infectious Disease Award (L.V.H.), and the Howard Hughes Medical Institute.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/cgi/content/full/0808723105/DCSupplemental.
References
- 1.Turnbaugh PJ, et al. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 2.Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448:427–434. doi: 10.1038/nature06005. [DOI] [PubMed] [Google Scholar]
- 3.Ayabe T, et al. Secretion of microbicidal α-defensins by intestinal Paneth cells in response to bacteria. Nat Immunol. 2000;1:113–118. doi: 10.1038/77783. [DOI] [PubMed] [Google Scholar]
- 4.Hooper LV, Stappenbeck TS, Hong CV, Gordon JI. Angiogenins: A new class of microbicidal proteins involved in innate immunity. Nat Immunol. 2003;4:269–273. doi: 10.1038/ni888. [DOI] [PubMed] [Google Scholar]
- 5.Cash HL, Whitham CV, Behrendt CL, Hooper LV. Symbiotic bacteria direct expression of an intestinal bactericidal lectin. Science. 2006;313:1126–1130. doi: 10.1126/science.1127119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cash HL, Whitham CV, Hooper LV. Refolding, purification, and characterization of human and murine RegIII proteins expressed in Escherichia coli. Protein Expr Purif. 2006;48:151–159. doi: 10.1016/j.pep.2006.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Madsen J, et al. CRP-ductin, the mouse homologue of gp-340/deleted in malignant brain tumors 1 (DMBT1), binds gram-positive and gram-negative bacteria and interacts with lung surfactant protein D. Eur J Immunol. 2003;33:2327–2336. doi: 10.1002/eji.200323972. [DOI] [PubMed] [Google Scholar]
- 8.Artis D, et al. RELMβ/FIZZ2 is a goblet cell-specific immune-effector molecule in the gastrointestinal tract. Proc Natl Acad Sci USA. 2004;101:13596–13600. doi: 10.1073/pnas.0404034101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zaph C, et al. Epithelial-cell-intrinsic IKK-β expression regulates intestinal immune homeostasis. Nature. 2007;446:552–556. doi: 10.1038/nature05590. [DOI] [PubMed] [Google Scholar]
- 10.Kobayashi KS, et al. Nod2-dependent regulation of innate and adaptive immunity in the intestinal tract. Science. 2005;307:731–734. doi: 10.1126/science.1104911. [DOI] [PubMed] [Google Scholar]
- 11.Rakoff-Nahoum S, Medzhitov R. Regulation of spontaneous intestinal tumorigenesis through the adaptor protein MyD88. Science. 2007;317:124–127. doi: 10.1126/science.1140488. [DOI] [PubMed] [Google Scholar]
- 12.Brandl K, Plitas G, Schnabl B, Dematteo RP, Pamer EG. MyD88-mediated signals induce the bactericidal lectin RegIIIγ and protect mice against intestinal Listeria monocytogenes infection. J Exp Med. 2007;204:1891–1900. doi: 10.1084/jem.20070563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004;118:229–241. doi: 10.1016/j.cell.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 14.Takeda K, Akira S. TLR signaling pathways. Semin Immunol. 2004;16:3–9. doi: 10.1016/j.smim.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Hornef MW, Frisan T, Vandewalle A, Normark S, Richter-Dahlfors A. Toll-like receptor 4 resides in the Golgi apparatus and colocalizes with internalized lipopolysaccharide in intestinal epithelial cells. J Exp Med. 2002;195:559–570. doi: 10.1084/jem.20011788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanabe H, et al. Mouse paneth cell secretory responses to cell surface glycolipids of virulent and attenuated pathogenic bacteria. Infect Immun. 2005;73:2312–2320. doi: 10.1128/IAI.73.4.2312-2320.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rumio C, et al. Degranulation of paneth cells via toll-like receptor 9. Am J Pathol. 2004;165:373–381. doi: 10.1016/S0002-9440(10)63304-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuida K, et al. Altered cytokine export and apoptosis in mice deficient in interleukin-1 β converting enzyme. Science. 1995;267:2000–2003. doi: 10.1126/science.7535475. [DOI] [PubMed] [Google Scholar]
- 19.Pull SL, Doherty JM, Mills JC, Gordon JI, Stappenbeck TS. Activated macrophages are an adaptive element of the colonic epithelial progenitor niche necessary for regenerative responses to injury. Proc Natl Acad Sci USA. 2005;102:99–104. doi: 10.1073/pnas.0405979102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Otte JM, Rosenberg IM, Podolsky DK. Intestinal myofibroblasts in innate immune responses of the intestine. Gastroenterology. 2003;124:1866–1878. doi: 10.1016/s0016-5085(03)00403-7. [DOI] [PubMed] [Google Scholar]
- 21.Garabedian EM, Roberts LJ, McNevin MS, Gordon JI. Examining the role of Paneth cells in the small intestine by lineage ablation in transgenic mice. J Biol Chem. 1997;272:23729–23740. doi: 10.1074/jbc.272.38.23729. [DOI] [PubMed] [Google Scholar]
- 22.Rescigno M, et al. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat Immunol. 2001;2:361–367. doi: 10.1038/86373. [DOI] [PubMed] [Google Scholar]
- 23.Macpherson AJ, Uhr T. Induction of protective IgA by intestinal dendritic cells carrying commensal bacteria. Science. 2004;303:1662–1665. doi: 10.1126/science.1091334. [DOI] [PubMed] [Google Scholar]
- 24.Niess JH, et al. CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science. 2005;307:254–258. doi: 10.1126/science.1102901. [DOI] [PubMed] [Google Scholar]
- 25.Stecher B, et al. Salmonella enterica serovar typhimurium exploits inflammation to compete with the intestinal microbiota. PLoS Biol. 2007;5:2177–2189. doi: 10.1371/journal.pbio.0050244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stecher B, et al. Comparison of Salmonella enterica serovar Typhimurium colitis in germfree mice and mice pretreated with streptomycin. Infect Immun. 2005;73:3228–3241. doi: 10.1128/IAI.73.6.3228-3241.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilson CL, et al. Regulation of intestinal α-defensin activation by the metalloproteinase matrilysin in innate host defense. Science. 1999;286:113–117. doi: 10.1126/science.286.5437.113. [DOI] [PubMed] [Google Scholar]
- 28.Salzman NH, Ghosh D, Huttner KM, Paterson Y, Bevins CL. Protection against enteric salmonellosis in transgenic mice expressing a human intestinal defensin. Nature. 2003;422:522–526. doi: 10.1038/nature01520. [DOI] [PubMed] [Google Scholar]
- 29.Meyer-Hoffert U, et al. Secreted enteric antimicrobial activity localizes to the mucus surface layer. Gut. 2008;57:764–771. doi: 10.1136/gut.2007.141481. [DOI] [PubMed] [Google Scholar]
- 30.Wehkamp J, et al. Reduced Paneth cell α-defensins in ileal Crohn's disease. Proc Natl Acad Sci USA. 2005;102:18129–18134. doi: 10.1073/pnas.0505256102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Swidsinski A, Weber J, Loening-Baucke V, Hale LP, Lochs H. Spatial organization and composition of the mucosal flora in patients with inflammatory bowel disease. J Clin Microbiol. 2005;43:3380–3389. doi: 10.1128/JCM.43.7.3380-3389.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huttner KM, Selsted ME, Ouellette AJ. Structure and diversity of the murine cryptdin gene family. Genomics. 1994;19:448–453. doi: 10.1006/geno.1994.1093. [DOI] [PubMed] [Google Scholar]
- 33.Stappenbeck TS, Hooper LV, Manchester JK, Wong MH, Gordon JI. Laser capture microdissection of mouse intestine: Characterizing mRNA and protein expression, and profiling intermediary metabolism in specified cell populations. Methods Enzymol. 2002;356:167–196. doi: 10.1016/s0076-6879(02)56932-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.