Abstract
Background
Motivated by a previous study among male veterans (Allen, D.N., Frantom, L.V., Strauss, G.P., van Kammen, D.P., 2005. Differential patterns of premorbid academic and social deterioration in patients with schizophrenia. Schizophr. Res. 75, 389–397), the present analysis examined: (1) patterns of premorbid academic and social functioning during childhood, early adolescence, and late adolescence, and (2) associations between these premorbid functioning dimensions and a number of clinical variables.
Methods
Data on premorbid functioning were collected using the Premorbid Adjustment Scale (PAS) in 95 hospitalized first-episode patients. Analyses were similar to those conducted by Allen and colleagues (2005).
Results
Deterioration was evident in both academic and social functioning from childhood to early adolescence, along with a pronounced/accelerated deterioration in academic functioning from early adolescence to late adolescence, occurring in both male and female patients. Age at onset of prodromal symptoms was predicted by childhood/early adolescent/late adolescent academic functioning scores, and age at onset of psychotic symptoms was significantly associated only with childhood academic functioning. Severity of negative symptoms was predicted by childhood and late adolescent social functioning scores, and severity of general psychopathology symptoms was predicted by late adolescent academic functioning, as well as childhood and late adolescent social functioning scores.
Conclusions
Consistent with prior findings, deterioration in premorbid functioning appears to be more pronounced in the academic than social dimension of the PAS. Some PAS scores are predictive of ages at onset of prodrome/psychosis and severity of psychotic symptoms. Ongoing research on premorbid adjustment in schizophrenia may have implications for future prevention goals.
Keywords: Academic functioning, First-episode psychosis, Premorbid adjustment, Premorbid functioning, Schizophrenia, Social functioning
1. Introduction
Premorbid functioning has received much attention in the field of schizophrenia research. The terms premorbid functioning and premorbid adjustment refer to an individual’s social, interpersonal, academic, and occupational functioning prior to the onset of psychotic symptoms (Addington and Addington, 2005). Numerous studies have shown deficits in premorbid functioning to be related to a number of detrimental illness-related variables, such as early age at onset of illness, cognitive and neuropsychological deficits, and more severe positive and negative symptoms (Addington and Addington, 2005; Addington et al., 2003; Rabinowitz et al., 2002). Premorbid functioning also has been studied as a predictor of treatment outcome, with the general pattern indicating that good premorbid functioning is predictive of better response to treatment (Addington and Addington, 2005; Bailer et al., 1996; Gupta et al., 1995; Haim et al., 2006; Larsen et al., 2004; Rabinowitz et al., 2006; Stoffelmayr et al., 1983).
Some studies on premorbid functioning in schizophrenia have examined premorbid functioning not as a unitary construct, but across two different dimensions, academic functioning and social functioning (Allen et al., 2005; Cannon et al., 1997; van Kammen et al., 1994). Support for such a conceptualization has been provided by factor analyses, as well as the observation that academic adjustment is associated with intelligence, while social functioning is associated with symptom-related variables (Allen et al., 2001). The distinction between academic and social premorbid dimensions has been emphasized as more appropriate than global measures of premorbid functioning because combining the two domains may obscure associations between premorbid deterioration and important clinical variables (Allen et al., 2005).
Evidence of distinct patterns of deterioration in academic and social functioning are informative not only from the standpoint of differential clinical correlates, but also because future prevention-oriented endeavors could be enhanced by measuring deterioration in domains that are relatively specific to the development of schizophrenia as opposed to other serious mental illnesses (Cannon et al., 1997). The present study had a two-fold objective, motivated in part by findings from a sample of 58 male veterans with schizophrenia (Allen et al., 2005). Specifically, this study examined: (1) patterns of premorbid academic and social functioning during childhood, early adolescence, and late adolescence, and (2) associations between these premorbid dimensions and years of educational attainment, age at onset of prodromal symptoms, age at onset of psychotic symptoms, social functioning in the three months prior to first hospitalization, and severity of symptoms in the month prior to hospitalization.
2. Methods
2.1. Setting and Sample
Patients and family members were enrolled in an ongoing study investigating potential predictors of treatment delay in first-episode psychosis. Patients were 18–40 years of age and hospitalized in a psychiatric unit of a large, university-affiliated, public-sector hospital or an urban county psychiatric crisis center. Exclusion criteria included: inability to speak English, known mental retardation, Mini-Mental State Examination (Cockrell and Folstein, 1998; Folstein et al., 2001) score of <23, significant medical condition that could compromise ability to participate, inability to give informed consent for any reason, prior outpatient antipsychotic treatment of >3 months, and a prior hospitalization for psychosis >3 months before the current admission. Family members were ≥18 years of age, able to speak and read English, and had at least monthly contact with the patient during the year prior to admission.
2.2. Measures
Basic sociodemographic variables were obtained. Nonaffective primary psychotic disorders and substance use disorders were determined using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; APA, 2000; First et al., 1998). Consensus-based best estimates of age at onset of prodromal symptoms and psychotic symptoms were derived using information obtained from patients and family members with the Symptom Onset in Schizophrenia inventory (SOS; Perkins et al., 2000) and select items from the Course of Onset and Relapse Schedule / Topography of Psychotic Episode (CORS/TOPE; Norman and Malla, 2002). Symptom severity was rated with the widely used positive, negative, and general psychopathology subscales of the Positive and Negative Syndrome Scale (PANSS; APA, 2000; Kay et al., 1987). Social functioning during the three months prior to hospitalization was assessed using the Social Functioning Scale (SFS; Birchwood et al., 1990), which includes subscales in the following domains: social engagement/withdrawal, interpersonal behavior, independence–performance, recreation, prosocial, independence–competence, and employment/occupation.
The Premorbid Adjustment Scale (PAS; Cannon-Spoor et al., 1982) assesses the degree to which a person has successfully attained certain developmental goals at various life stages preceding the initial onset of psychotic symptoms. The instrument has been used widely in schizophrenia research, and reliability, validity, and predictive utility have been reported previously (Alvarez et al., 1987; Cannon-Spoor et al., 1982; Krauss et al., 1998). Functioning is assessed across four age periods: childhood (≤11 years), early adolescence (12–15 years), late adolescence (16–18 years), and adulthood (≥19 years). Functioning in each of these age periods is assessed across five major psychosocial domains that are rated from 0 (normal adjustment) to 6 (severe impairment): sociability and withdrawal, peer relationships, scholastic performance, adaptation to school, and social-sexual functioning. Social-sexual functioning is not included as a psychosocial domain during the childhood period, while scholastic performance and adaptation to school are not measured during the adulthood period. As mentioned below, the adulthood period was not assessed in the present study. Thus, in childhood, academic functioning includes scholastic performance and adaptation to school, and the social functioning encompasses sociability and withdrawal and peer relationships. In both early adolescence and late adolescence, academic functioning is comprised of scholastic performance and adaptation to school, and social functioning includes sociability and withdrawal, peer relationships, and social-sexual functioning.
Information on premorbid adjustment was gathered by a semi-structured interview with the patient after a thorough chart review and, when available, with an informant (typically the patient’s mother or another first-degree relative). Of the 95 patients, 41 had informants who provided collateral information, and among these, the patient’s and informant’s scores were averaged to yield best estimates. Similar to the study conducted by Allen and colleagues (2005), academic and social domain scores were calculated for each of three age periods: childhood, early adolescence, and late adolescence. Scores for the adulthood period were not examined because many participants had entered the prodromal phase of illness by early adulthood. Additionally, premorbid functioning was not assessed in any age period that would have included the year before the onset of prodromal symptoms to further safeguard against inadvertently assessing prodromal functioning during the rating of premorbid functioning.
2.3. Data Analyses
Basic sociodemographic and clinical characteristics of the sample were described, as were mean scores in the two premorbid areas (academic and social functioning) across the three age periods (childhood, early adolescence, and late adolescence). As an exploratory analysis, mean scores also were examined in male and female patients separately. Inter-correlations between PAS academic and social functioning scores across the three age periods were assessed. As in Allen et al. (2005), a repeated-measures multivariate analysis of variance (MANOVA) was calculated to assess progression of premorbid deterioration across the three age periods. Trajectories of deterioration were explored further using repeated-measures analyses of variance (ANOVAs) and paired-samples Student’s t-tests. Correlation analyses examined associations between PAS scores and key clinical variables. To enable comparisons of select correlation coefficients, the Fisher’s r to z transformation was used.
3. Results
3.1. Sample Characteristics
Sociodemographic characteristics of the sample are shown in Table 1. Ages ranged from 18 to 39 years (mean, 23.1±4.7). The majority of participants were male (76, 80.0%) and African American (86, 90.5%). In general, the sample was composed of patients who were single and never married (88, 92.6%), unemployed (60, 63.2%), impoverished (52 out of 83 with available data, 62.7%), and had a history of arrest (69, 72.6%). The mean number of years of educational attainment was 11.6±2.6.
Table 1.
Sociodemographic Characteristics of the Sample (n=95)
| Age, years (mean, SD) | 23.1 | 4.7 |
| Gender, male (n, %) | 76 | 80.0 |
| Race, African American (n, %) | 86 | 90.5 |
| Marital status (n, %) | ||
| Single, never married | 88 | 92.6 |
| Married or living with a partner | 3 | 3.2 |
| Divorced | 4 | 4.2 |
| Years of education completed, years (mean, SD) | 11.6 | 2.6 |
| Employed during the month prior to hospitalization (n, %) | 35 | 36.8 |
| At or below the federal poverty level, n=83 (n, %) | 52 | 62.7 |
| Ever arrested (n, %) | 69 | 72.6 |
Clinical characteristics are given in Table 2. More than half of participants were diagnosed with schizophrenia (56, 58.9%). Among these, 42 (44.2%) had paranoid type; 10 (10.5%) had disorganized type; two (2.1%) had undifferentiated type; and two (2.1%) had residual type. Twenty-one patients (22.1%) were diagnosed with schizophreniform disorder. Seven participants (7.4%) had schizoaffective disorder, four (4.2%) with bipolar type, and three (3.2%) with depressive type. Eleven patients (11.6%) were diagnosed with psychotic disorder not otherwise specified. Nineteen patients (20.0%) had an alcohol use disorder and 43 (45.3%) had a cannabis use disorder. As shown in Table 2, the mean age at onset of prodromal symptoms was 19.2±5.4 years, and the mean age at onset of psychotic symptoms was 21.6±4.9 years. Mean PANSS subscale scores and SFS total score also are shown in Table 2.
Table 2.
Clinical Characteristics of the Sample (n=95)
| Primary psychotic disorder diagnoses (n, %) | ||
| Schizophreniform disorder | 21 | 22.1 |
| Schizophrenia | 56 | 58.9 |
| Schizoaffective disorder | 7 | 7.4 |
| Psychotic disorder not otherwise specified | 11 | 11.6 |
| Substance use disorder diagnoses (n, %) | ||
| Alcohol abuse | 9 | 9.5 |
| Alcohol dependence | 10 | 10.5 |
| Cannabis abuse | 13 | 13.7 |
| Cannabis dependence | 30 | 31.6 |
| Age at onset of prodromal symptoms, years (mean, SD) | 19.2 | 5.4 |
| Age at onset of psychotic symptoms, years (mean, SD) | 21.6 | 4.9 |
| Positive and Negative Syndrome Scale subscales (mean, SD) | ||
| Positive | 23.9 | 4.5 |
| Negative | 21.7 | 6.9 |
| General psychopathology | 42.0 | 8.9 |
| Social Functioning Scale (mean, SD) | 123.9 | 27.8 |
3.2. Descriptive Characteristics of Premorbid Functioning
Mean PAS academic and social functioning scores for the overall sample are shown in Table 3. In each instance, scores increased numerically (indicating worsening premorbid functioning) across the childhood, early adolescence, and late adolescence age periods. Mean scores for male and female patients separately also are shown. Table 4 shows inter-correlations between PAS academic and social functioning scores across the three age periods. All correlations were statistically significant, and as expected, scores in consecutive age periods (i.e., childhood and early adolescence, and early adolescence and late adolescence) were more strongly correlated (r=.50–.76, all p≤.01) than those in the non-consecutive age periods (i.e., childhood and late adolescence).
Table 3.
Descriptive Statistics for the PAS Academic and Social Scores by Age Period
| PAS Age Periods | ||||||
|---|---|---|---|---|---|---|
| PAS Domains | Childhood | Early adolescence | Late Adolescence | |||
| Mean | SD | Mean | SD | Mean | SD | |
| Overall Sample | ||||||
| Social | 1.30 | 1.14 | 1.50 | 1.05 | 1.53 | 1.10 |
| Academic | 1.68 | 0.92 | 1.99 | 0.88 | 3.10 | 1.67 |
| Male Patients | ||||||
| Social | 1.29 | 1.06 | 1.50 | 0.95 | 1.57 | 1.05 |
| Academic | 1.72 | 0.93 | 2.04 | 0.86 | 3.17 | 1.72 |
| Female Patients | ||||||
| Social | 1.33 | 1.41 | 1.51 | 1.42 | 1.39 | 1.28 |
| Academic | 1.53 | 0.89 | 1.80 | 0.94 | 2.82 | 1.48 |
Table 4.
Inter-correlations between PAS Academic Scores across the Three Age Periods and PAS Social Scores across the Three Age Periods
| Childhood Academic | Early Adolescence Academic | Early Adolescence Social | Late Adolescence Social | ||
|---|---|---|---|---|---|
| Childhood Academic | Childhood Social | ||||
| Early Adolescence Academic | .76** | Early Adolescence Social | .50** | ||
| Late Adolescence Academic | .26* | .56** | Late Adolescence Social | .40** | .62** |
p≤.05
p≤.01
3.3. Differential Patterns of Deterioration in Premorbid Academic and Social Functioning
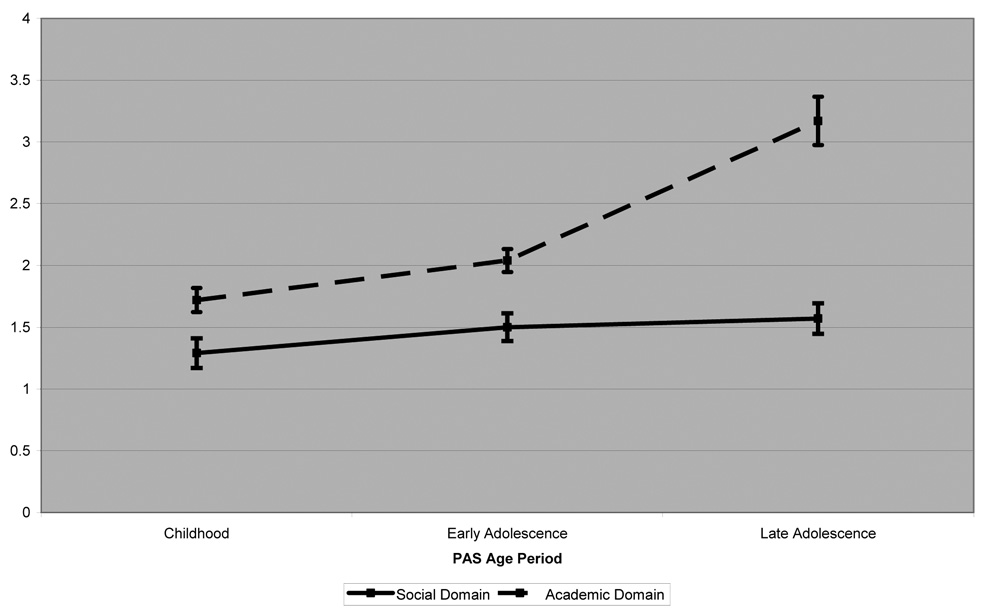
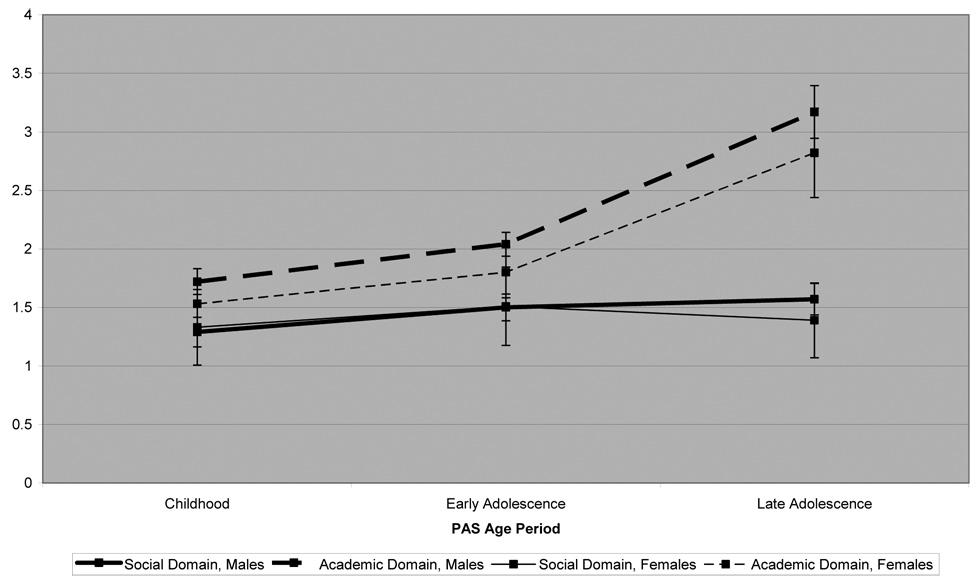
Tests of within-subjects effects indicated a significant effect for age period (F=23.66; df=2, 71; p<.001), a significant effect for premorbid domain (F=39.64; df=1, 72; p<.001), and a significant effect for the age period by premorbid domain interaction term (F=21.98; df=2, 72; p<.001). Means and standard errors are shown in Figure 1. The graphs display the deterioration in both academic and social functioning from childhood to early adolescence, and the pronounced/accelerated deterioration in academic functioning from early adolescence to late adolescence without a concomitant decline in social functioning from early adolescence to late adolescence. As shown in Figure 2, graphs are very similar when plotting mean scores of male and female patients separately, though female participants had numerically lower academic domain scores across each age period, indicating better academic functioning.
Figure 1.
Patterns of Deterioration in Mean Premorbid Social and Academic Domain Scores
Figure 2.
Patterns of Deterioration in Mean Premorbid Social and Academic Domain Scores, By Gender
Also as conducted by Allen and colleagues (2005), repeated-measures ANOVAs then were used to investigate the interaction effect. Regarding the academic domain, a significant within-subjects effect was observed (F=49.46; df=1.16, 83.73; p<0.001). Within-subjects contrasts indicated that childhood academic functioning was significantly better than early adolescent academic functioning (p<0.001) and late adolescent academic functioning (p<0.001). Additionally, early adolescent and late adolescent academic functioning differed significantly (p<0.001). For this repeated-measures ANOVAs, the Greenhouse-Geisser correction was applied (ε was <.75) to correct the df due to a significant Mauchly’s test of sphericity. Regarding the social domain, a significant within-subjects effect was observed (F=3.60; df=1.9, 142.7; p=0.03). Within-subjects contrasts indicated that childhood social functioning was significantly better than early adolescent social functioning (p=0.03) and late adolescent social functioning (p=0.03). However, early adolescent and late adolescent social functioning did not differ (p=0.61). For this repeated-measures ANOVAs, the Huynh-Feldt correction was applied (ε was >.75) to correct the df due to a significant Mauchly’s test of sphericity.
Paired samples t-tests revealed significant differences between academic and social PAS scores during childhood (t=3.04, df=89, p=0.03), early adolescence (t=3.37, df=86, p=0.001), and late adolescence (t=7.93, df=72, p<0.001). When averaging PAS scores across age periods, a significant difference between academic and social domains also was evident (t=5.54, df=89, p<0.001).
3.4. Correlates of Premorbid Academic and Social Functioning
Not surprisingly, patients’ years of education was predicted by the PAS late adolescent academic functioning score (r=−.30, p≤.01). However, years of educational attainment was not predicted by childhood or early adolescent academic functioning or by social functioning in any of the three age periods (Table 5). Age at onset of prodromal symptoms was predicted by childhood, early adolescent, and late adolescent academic functioning scores—poorer academic functioning (indicated by higher PAS scores) was associated with a younger age at onset of prodromal symptoms (r=−.23–−.24, all p<.05). Counterintuitively, age at onset of prodromal symptoms appeared to be positively associated with early adolescent social functioning (r=.25, p<.05), though this correlation was not apparent in the other two age periods. Age at onset of psychotic symptoms was significantly associated only with childhood academic functioning (r=−.23, p<.05). However, comparisons of correlation coefficients using Fisher’s r to z transformations revealed no significant differences between the correlations pertaining to childhood academic functioning (r=−.23), early adolescent academic functioning (r=−.21), and late adolescent academic functioning (r=−.20).
Table 5.
Correlates of Premorbid Academic and Social Functioning
| Years of Education | Age at Onset of Prodrome | Age at Onset of Psychosis | Positive Symptoms | Negative Symptoms | General Psychopathology | SFS Total Score | |
|---|---|---|---|---|---|---|---|
| Childhood Academic | −.12 | −.23* | −.23* | .12 | .15 | .10 | .10 |
| Early Adolescence Academic | −.14 | −.24* | −.21 | .12 | .18 | .16 | −.05 |
| Late Adolescence Academic | −.30** | −.24* | −.20 | .14 | .21 | .24* | −.16 |
| Childhood Social | .00 | −.08 | −.13 | .14 | .24* | .23* | .01 |
| Early Adolescence Social | .13 | .25* | .18 | .13 | .20 | .16 | −.17 |
| Late Adolescence Social | −.02 | .04 | −.02 | .21 | .38** | .25* | −.06 |
p≤.05
p≤.01
PAS scores were not associated with severity of positive symptoms. The severity of negative symptoms was predicted by childhood (r=.24, p<.05) and late adolescent (r=.38, p<.01) social functioning scores. However, it should be noted that the magnitudes of the correlation coefficients regarding negative symptoms were similar for all PAS domains. In fact, Fisher’s z tests revealed no significant differences between the correlations pertaining to childhood social functioning (r=.24), early adolescent social functioning (r=.20), and late adolescent academic functioning (r=.21). The severity of general psychopathology symptoms was predicted by late adolescent academic functioning scores, as well as childhood and late adolescent social functioning scores (r=−.23–−.25, all p<.05).
Regarding social functioning in the three months prior to hospitalization for first-episode psychosis, none of the six PAS subscale scores were predictive of SFS total score. However, when the seven SFS subscales were examined in relation to premorbid social functioning in an exploratory correlational analysis, poorer childhood, early adolescent, and late adolescent social functioning was associated with poorer social engagement SFS subscale scores (r=−.35, r=−.30, r=−.26, respectively, all p<.05). There were no correlations between premorbid social functioning and the other six SFS subscales.
4. Discussion
Results of this study generally parallel those of Allen and colleagues (2005), with patterns of deterioration evident in both academic and social premorbid functioning. A pronounced deterioration in academic functioning between early adolescence and late adolescence was observed, in both male and female first-episode patients, although there was no analogous deterioration in social functioning from early to late adolescence. Clinical variables associated with academic premorbid functioning included years of education, age at onset of prodromal symptoms, age at onset of psychotic symptoms, and general psychopathology symptom scores; variables associated with social functioning included age at onset of prodromal symptoms, negative symptom scores, general psychopathology symptom scores, and the social engagement aspect of social functioning. Interestingly, age at onset of prodromal symptoms was found to be specifically associated with early adolescent social functioning (and not childhood or late adolescent social functioning), in addition to being associated with academic functioning in all three age periods.
The present findings support the need for examining premorbid functioning not as a unitary construct, but as one that can be divided into at least two distinct domains, namely academic and social functioning. Examination of these two domains across age periods shows differential patterns of deterioration over time. Given that academic deterioration was more pronounced during adolescence, it could represent an important marker, perhaps with some degree of specificity, for the later onset of schizophrenia. A study conducted by Cannon and colleagues (1997) showed deterioration in both academic and social functioning during adolescence among patients diagnosed with schizophrenia, but only deterioration in the social domain during adolescence among bipolar patients.
Academic premorbid functioning predicted ages at onset of prodromal and psychotic symptoms. This suggests developmentally-relevant cognitive and neurocognitive variables that may be associated specifically with schizophrenia and that may serve as predictive markers of severity and long-term outcome (Schenkel and Silverstein, 2004). Other studies have found that early neuromotor performance, intellectual functioning, and verbal memory are linked to varying degrees with later risk for developing schizophrenia (Addington et al, 2003; Schenkel and Silverstein, 2004).
Social premorbid functioning was predictive of negative and general symptoms. Strous and colleagues (2004) found that impaired sociability in particular correlated with longer treatment response, more severe negative symptoms, and increased Parkinsonian symptoms, all generally reflecting poorer treatment outcome. The development of social functioning deficits across childhood has been documented among individuals who develop schizophrenia, but the finding in this study that social functioning did not significantly deteriorate from early to late adolescence may indicate a greater importance of deficits in social development occurring earlier in life. One study found that abnormalities in social adjustment were detectable as early as the age of 7 in some people who later developed psychiatric illness (Done et al., 1994). Regardless of what specific age period is most relevant in terms of social deficits and the development of schizophrenia, it can be asserted that the psychosocial disability associated with schizophrenia occurs well before the onset of psychotic symptoms or even prodromal symptoms. Thus, future preventive efforts may be critical in the premorbid and/or prodromal periods to minimize or avert further social disability that has already begun to develop by the time of symptom onset.
Several methodological limitations are noteworthy. First, the specific sociodemographic and clinical characteristics of the sample limit generalizability to dissimilar populations. However, it is of interest that this study documents very similar findings to those of Allen and colleagues (2005), who studied an exclusively male sample of veterans with chronic schizophrenia. The latter sample, by virtue of acceptance into the military, would presumably have had better premorbid adjustment; yet, comparison of PAS scores in that sample and the current study revealed remarkably similar means. Second, premorbid functioning obviously must be assessed retrospectively, which may lead to inaccurate reporting. However, the use of a first-episode sample with a mean age of 23 years likely minimizes these inaccuracies to a large extent. Third, collateral information on premorbid adjustment was available for only 41 patients (43%). Future analyses should examine reliability and validity of PAS scores when only patients’ data are used, as well as psychometric properties when various ways of integrating patients’ and informants’ reports are utilized.
The present findings raise a number of interesting questions for future research. First, do the distinct patterns of deterioration in academic and social performance replicated in this study represent actual premorbid processes, or are they reflective of the specific items of the PAS? Future studies would benefit from more extensive and cross-validated measures of both academic, social, and other aspects of premorbid adjustment. Additionally, larger sample sizes would allow for a more thorough characterization of gender-specific patterns in premorbid functioning. Second, is it possible that interventions that could be designed to ameliorate academic and social deterioration, especially among high-risk adolescents, could delay the age at onset of prodromal or psychotic symptoms? Cross-sectional observational studies such as this one cannot clarify causality, so it remains unknown whether declining premorbid performance is caused by the imminent onset of a psychotic disorder (the presumed direction of causality) or whether declining premorbid performance causes the imminent onset of a psychotic disorder (which, if supported, would convey preventive implications). Third, could detailed examination of patterns of premorbid deterioration in ultra-high-risk (potentially prodromal) adolescents inform specific preventive interventions? For example, if further research replicates the finding that poor premorbid social functioning is predictive of later negative symptoms, it could be possible that preventive interventions eventually designed to target negative, rather than positive symptoms, would be indicated in adolescents with prominent deterioration in premorbid social functioning. These and other questions suggest that ongoing research into the premorbid period of schizophrenia is a worthy pursuit.
Acknowledgements
This research was supported by National Institute of Mental Health (NIMH) grant K23 MH067589 to the third author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Addington J, Addington D. Patterns of premorbid functioning in first episode psychosis: relationship to 2-year outcome. Acta Psychiatr. Scand. 2005;112:40–46. doi: 10.1111/j.1600-0447.2005.00511.x. [DOI] [PubMed] [Google Scholar]
- Addington J, van Mastrigt S, Addington D. Patterns of premorbid functioning in first-episode psychosis: initial presentation. Schizophr. Res. 2003;62:23–30. doi: 10.1016/s0920-9964(02)00408-5. [DOI] [PubMed] [Google Scholar]
- Allen DN, Frantom LV, Strauss GP, van Kammen DP. Differential patterns of premorbid academic and social deterioration in patients with schizophrenia. Schizophr. Res. 2005;75:389–397. doi: 10.1016/j.schres.2004.11.011. [DOI] [PubMed] [Google Scholar]
- Allen DN, Kelley ME, Miyatake RK, Gurklis JA, van Kammen DP. Confirmation of a two-factor model of premorbid adjustment in males with schizophrenia. Schizophr. Bull. 2001;27:39–46. doi: 10.1093/oxfordjournals.schbul.a006858. [DOI] [PubMed] [Google Scholar]
- Alvarez E, Garcia-Ribera C, Torrens M, Udina C, Guillamat R, Casas M. Premorbid Adjustment Scale as a prognostic predictor for schizophrenia. Br. J. Psychiatry. 1987;150:411. doi: 10.1192/bjp.150.3.411. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Handbook of Psychiatric Measures. Washington, D.C.: American Psychiatric Association; 2000. [Google Scholar]
- Bailer J, Brauer W, Rey ER. Premorbid adjustment as predictor of outcome in schizophrenia: results of a prospective study. Acta Psychiatr. Scand. 1996;93:368–377. doi: 10.1111/j.1600-0447.1996.tb10662.x. [DOI] [PubMed] [Google Scholar]
- Birchwood M, Smith J, Cochrane R, Wetton S, Copestake S. The Social Functioning Scale: the development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenia patients. Br. J. Psychiatry. 1990;157:853–859. doi: 10.1192/bjp.157.6.853. [DOI] [PubMed] [Google Scholar]
- Cannon M, Jones P, Gilvarry C, Rifkin L, McKenzie K, Foerster A, Murray RM. Premorbid social functioning in schizophrenia and bipolar disorder: similarities and differences. Am. J. Psychiatry. 1997;154:1544–1550. doi: 10.1176/ajp.154.11.1544. [DOI] [PubMed] [Google Scholar]
- Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr. Bull. 1982;8:470–484. doi: 10.1093/schbul/8.3.470. [DOI] [PubMed] [Google Scholar]
- Cockrell JR, Folstein MF. Mini-Mental State Examination (MMSE) Psychopharmacol. Bull. 1998;24:689–692. [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. New York: New York State Psychiatric Institute Biometrics Research Department; 1998. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR, Fanjiang G. Mini-Mental State Examination: User’s Guide. Florida: Psychological Assessment Resources, Inc.; 2001. [Google Scholar]
- Gupta S, Rajaprabhakaran R, Arndt S, Flaum M, Andreasen NC. Premorbid adjustment as a predictor of phenomenological and neurobiological indices in schizophrenia. Schizophr. Res. 1995;16:189–197. doi: 10.1016/0920-9964(94)00073-h. [DOI] [PubMed] [Google Scholar]
- Haim R, Rabinowitz J, Bromet E. The relationship of premorbid functioning to illness course in schizophrenia and psychotic mood disorders during two years following first hospitalization. J. Nerv. Ment. Dis. 2006;194:791–795. doi: 10.1097/01.nmd.0000240158.39929.e3. [DOI] [PubMed] [Google Scholar]
- Kay SR, Fizbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr. Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Krauss H, Warwinski K, Held T, Rietchel M, Freyberger HJ. Reliability and validity of the Premorbid Adjustment Scale (PAS) in a German sample of schizophrenic and schizoaffective patients. Eur. Arch. Psychiatry Clin. Neurosci. 1998;248:277–281. doi: 10.1007/s004060050050. [DOI] [PubMed] [Google Scholar]
- Larsen TK, Friis S, Haahr U, Johannessen JO, Melle I, Opjordsmoen S, Rund BR, Simonsen E, Vaglum P, McGlashan TH. Premorbid adjustment in first-episode non-affective psychosis: distinct patterns of pre-onset course. Br. J. Psychiatry. 2004;185:108–115. doi: 10.1192/bjp.185.2.108. [DOI] [PubMed] [Google Scholar]
- Norman RMG, Malla AK. Course of Onset and Relapse Schedule: Interview and Coding Instruction Guide. London, Ontario, Canada: Prevention and Early Intervention for Psychosis Program; 2002. [Google Scholar]
- Perkins DO, Leserman J, Jarskog LF, Graham K, Kazmer J, Lieberman JA. Characterizing and dating the onset of symptoms in psychotic illness: the Symptom Onset in Schizophrenia (SOS) inventory. Schizophr. Res. 2000;44:1–10. doi: 10.1016/s0920-9964(99)00161-9. [DOI] [PubMed] [Google Scholar]
- Rabinowitz J, De Smedt G, Harvey PD, Davidson M. Relationship between premorbid functioning and symptom severity as assessed at first episode of psychosis. Am. J. Psychiatry. 2002;159:2021–2026. doi: 10.1176/appi.ajp.159.12.2021. [DOI] [PubMed] [Google Scholar]
- Rabinowitz J, Harvey PD, Eerdekens M, Davidson M. Premorbid functioning and treatment response in recent-onset schizophrenia. Br. J. Psychiatry. 2006;189:31–35. doi: 10.1192/bjp.bp.105.013276. [DOI] [PubMed] [Google Scholar]
- Schenkel LS, Silverstein SM. Dimensions of premorbid functioning in schizophrenia: a review of neuromotor, cognitive, social, and behavioral domains. Genet. Soc. Gen. Psychol. Monogr. 2004;130:241–270. doi: 10.3200/MONO.130.3.241-272. [DOI] [PubMed] [Google Scholar]
- Stoffelmayr BE, Dillavou D, Hunter JE. Premorbid functioning and outcome in schizophrenia: a cumulative analysis. J. Consult. Clin. Psychol. 1983;51:338–352. doi: 10.1037//0022-006x.51.3.338. [DOI] [PubMed] [Google Scholar]
- Strous RD, Alvir JM, Robinson D, Gal G, Sheitman B, Chakos M, Lieberman JA. Premorbid functioning in schizophrenia: relation to baseline symptoms, treatment response, and medication side effects. Schizophr. Bull. 2004;30:265–278. doi: 10.1093/oxfordjournals.schbul.a007077. [DOI] [PubMed] [Google Scholar]
- Van Kammen DP, Kelley ME, Gilbertson MW, Gurklis JA, O’Connor DT. CSF dopamine b-hydroxylase in schizophrenia: associations with premorbid functioning and brain computerized tomography scan measures. Am. J. Psychiatry. 1994;151:372–378. doi: 10.1176/ajp.151.3.372. [DOI] [PubMed] [Google Scholar]