ABSTRACT
Osteoid osteoma is a benign, neoplastic lesion, characterized by a less-than-2-cm pea-like mass of abnormal bone, the nidus. Traditional treatments have involved either conservative management with pain control or operative excision of the nidus. Today, radio-frequency ablation (RFA) is being used more commonly for the treatment of osteoid osteomas. There have been numerous studies showing the effectiveness of RFA.1–11 Complications of the procedure are rare but have been reported.7,11-15 We report a patient with a full-thickness cutaneous burn after RFA of a tibial osteoid osteoma.
CASE REPORT
A 16-year-old female was referred to our clinic for pain over the anterior aspect of her tibia for four months. She had good relief of her pain with non-steroidal anti-inflammatory drugs (NSAIDs) but difficulties with sporting activities secondary to pain. Her pain did not respond to limited activity and restricted weight bearing. Computed tomography (CT) scan confirmed an anterior tibial cortically based mass consistent with an osteoid osteoma. Treatment options were discussed and radio-frequency ablation was recommended.
After written informed consent was obtained from the patient’s parents, the patient was taken to the CT suite and placed under general anesthesia. A CT scan of the right tibia was performed. The osteoid osteoma was localized within the anterior tibial cortex and the proper trajectory for the drill bit was confirmed. The skin was marked to confirm this location.
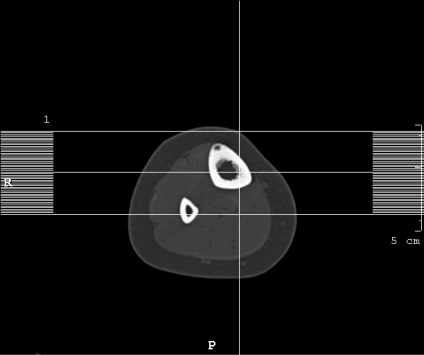
The area was then prepped and draped. A small skin incision was made to accommodate a 2.7 mm drill bit. Then, a Stryker cordless drill the with a 0.045-inch-diameter, six-inch-long Kirschner (K)-wire was advanced through the anterior cortex of the tibia into the intramedullary space. Serial CT scans were performed to confirm the location of the K- wire. Once the K-wire was positioned immediately posterior to the nidus of the osteoid osteoma, the 2.7 mm cannulated drill bit was used to over-drill the K-wire and position itself into the nidus of the osteoid osteoma. This was confirmed with CT scan (Figure 1).
Figure 1.
The radio-frequency electrode was inserted through the drill track into the osteoid osteoma and confirmed with CT. RFA was performed for five minutes at 90 degrees Celsius. Once the RFA probe was removed, the incision was dressed. The patient tolerated the procedure well without immediate complications and was discharged home.
The patient experienced a change in the character of her post-operative pain four days after the procedure. Her parents called our office for her increased localized pain on the anterior tibia and the pain medications were adjusted. Nine days after RFA, she presented to the ER with a small rim of redness in the area of the incision and mild serous drainage. There was no fluctuance in the area. Her erythrocyte sedimentation rate (ESR) was five and her C-reactive protein (CRP) was <0.5, both normal by our institutional standards. Eleven days after the procedure she had her first post-operative clinical visit. Examination of the wound revealed a 7 mm-diameter area of full-thickness skin necrosis in the area of the incision surrounded by a 2-to-3 mm rim of erythematous skin discoloration. There was some clear drainage from the central area (Figure 2). The wound was managed with Silvadene dressing changes twice a day. Fifteen days after the procedure her wound was re-evaluated (Figure 3). There had been a slight spread in erythema and a demarcation of the area of full-thickness skin necrosis. By six weeks from the time of the procedure, the erythema had resolved and the wound was filling in with healthy granulation tissue.
Figure 2.
Figure 3.
DISCUSSION
Osteoid osteoma is a benign neoplastic lesion, characterized by a less than a 2 cm, pea-like mass of abnormal bone, the nidus. The nidus is richly innervated, causing considerable pain usually without systemic symptoms. It has no malignant potential and usually does not grow16-17. It represents 12% of all benign tumors and 3% of primary bone tumors. It is uncommon in African-Americans and has a 2.3:1 male predominance.16 Fifty percent of patients are between 10-20 years old and 90% are between 5-25 years old. It is most commonly found in the long bones.16-17
There are three different methods of treatment for osteoid osteoma: Non-operative, open, and percutaneous. Non-surgical treatment involves use of NSAIDs, which typically relieve most of the pain. Osteoid osteomas will regress, but the time frame for symptom resolution is uncertain. Symptoms are usually severe enough that patients are reluctant to accept this mode of treatment.6,12,18,19
Surgical excision of the nidus is a reliable method of treatment. However, osteoid osteomas can present in difficult locations. Locating the nidus and confirming that it has been excised can be challenging. Further, occasionally significant unaffected bone is destroyed to reach the nidus.
Thus, radiographically guided thermal ablation is now the most common method of treatment. Radiofrequency energy can selectively ablate limited and controlled volumes of tissues, causing necrosis by thermal coagulation. The RF electrode alternates polarity causing charged particles in the area to be attracted and repelled in rapid oscillation. This increase in energy heats the surrounding tissue. A simple straight electrode with a 5 mm exposed tip heated to 90C will expose a 1 cm sphere of surrounding tissue to lethal temperatures. This, along with the ease of targeting the device under CT guidance, makes RFA an ideal method for obliterating small, solitary, osteoid osteomas.
Success rates have been reported from 78-100% across many different series.1-7,9-13 Complications in these series have been rare, with cellulitis and superficial skin burns being most common.1,2,7,11,15 Venbrux reported a full-thickness skin burn 0.5 × 0.8 cm in diameter over the medial border of the distal tibia at the site of an RFA probe insertion. The burn healed with local wound care and no adverse outcomes.11 Pinto described treating an osteoid osteoma of the subcutaneous tibia resulting in a fistula.15 Donkol reported two skin burns from his series of 21 pediatric patients.1 There was one other case report which described a full-thickness skin burn with almost the exact time course and clinical picture as our patient. It was also a burn of the subcutaneous border of the tibia.20
Pinto reported cutaneous burns are a possible complication of this procedure and recommended the outer cannula of the probe be withdrawn to approximately 1 cm above the non-insulated tip of the coagulation cannula. He hypothesized that cutaneous burns occur due to a defect of the insulation material covering the thermal ablation cannula.15 The RFA device is discarded at our institution after use, so this could not be confirmed in our case.
Skin and soft tissue thermal necroses are unusual complications. The areas at greatest risk are those without much subcutaneous fat or muscle, such as the anterior tibia. Thermal necrosis to adjacent tissues should be considered and discussed with patients prior to recommending and performing RFA. Several precautions have been recommended to prevent unwanted damage to at-risk tissue. These include using a probe appropriate for the size and depth of the lesion as well as retracting the cannula to insure the insulation is intact.15,20
With the correct indications and proper technical steps, RFA is a safe, effective method for treatment of osteoid osteoma. It is prudent to be aware of and prevent the rare complications associated with the procedure.
REFERENCES
- 1.Donkol R, Al-Nammi A, Moghazi K. Efficacy of percutaneous radiofrequency ablation of osteoid osteoma in children. Pediatric Radiology. 2007;38:180–185. doi: 10.1007/s00247-007-0690-z. [DOI] [PubMed] [Google Scholar]
- 2.Akhlaghpoor S, Tomasian A, Shabestari A, Ebrahimi M, Alinaghizadeh M. Percuatneous ostoid ostoma treatment with combination of radiofrequency and alcohol ablation. Clinical radiology. 2007;62:268–273. doi: 10.1016/j.crad.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 3.Gangi A, Dietemann JL, Clavert JM, Dodelin A, Mortazavi R, Durckel J, Roy C. Treatment of osteoid osteoma using laser photocoagulation: apropos of 28 cases. Rev Chir Orthop Reparatrice Appar Mot. 1998;84:676–684. [PubMed] [Google Scholar]
- 4.Barei DP, Moreau G, Scarborough MT, Neel MD. Percutaneous radiofrequency ablation of osteoid osteoma. Clin Orthop Relat Res. 2000;373:115–124. doi: 10.1097/00003086-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Dupuy DE. Radiofrequency ablation: an outpatient percutaneous treatment. Med Health R I. 1999;82:213–216. [PubMed] [Google Scholar]
- 6.Freiberger RH, Loitman BS, Helpern M, Thompson TC. Osteoid osteoma: a report on 80 cases. Am J Roentgenol Radium Ther Nucl Med. 1959;82:194–205. [PubMed] [Google Scholar]
- 7.Rosenthal DI, Hornicek FJ, Torriani M, Gebhardt MC, Mankin HJ. Osteoid osteoma: percutaneous treatment with radiofrequency energy. Radiology. 2003;229:171–175. doi: 10.1148/radiol.2291021053. [DOI] [PubMed] [Google Scholar]
- 8.Frassica FJ, Waltrip RL, Sponseller PD, Ma LD, McCarthy EF., Jr. Clinicopathologic features and treatment of osteoid osteoma and osteoblastoma in children and adolescents. Orthop Clin North Am. 1996;27:559–574. [PubMed] [Google Scholar]
- 9.Cribb GL, Goude WH, Cool P, Tins B, Cassarpullicino VN, Mangham DC. Percutaneous radiofrequency thermocoagulation of osteoid osteomas: factors affecting therapeutic outcome. Skeletal Radiol. 2005;34:702–706. doi: 10.1007/s00256-005-0947-2. [DOI] [PubMed] [Google Scholar]
- 10.Lindner NJ, Ozaki T, Roedl R, Gosheger G, Winkelmann W, Wortler K. Percutaneous radiofrequency ablation in osteoid osteoma. J Bone Joint Surg Br. 2001;83:391–396. doi: 10.1302/0301-620x.83b3.11679. [DOI] [PubMed] [Google Scholar]
- 11.Venbrux AC, Montague BJ, Murphy KP, Bobonis LA, Washington SB, Soltes AP, Frassica FJ. Image-guided percutaneous radiofrequency ablation for osteoid osteomas. J Vasc Interv Radiol. 2003;14:375–380. doi: 10.1097/01.rvi.0000058420.01661.8c. [DOI] [PubMed] [Google Scholar]
- 12.Gallazzi MB, Arborio G, Garbagna PG, perrucchini G, Daolio PA. Percutaneous radio-frequency ablation of osteoid osteoma: technique and preliminary results [in Italian] Radiol Med (Torino) 2001;102:329–334. [PubMed] [Google Scholar]
- 13.Rosenthal DI, Alexander A, Rosenberg AE, Springfield D. Ablation of osteoid osteomas with a percutaneously placed electrode: a new procedure. Radiology. 1992;183:29–33. doi: 10.1148/radiology.183.1.1549690. [DOI] [PubMed] [Google Scholar]
- 14.Wood TF, Rose DM, Chung M, Allegra DP, Foshag LJ, Bilchik AJ. Radiofrequency ablation of 231 unresectable hepatic tumors: indications, limitations, and complications. Ann Surg Oncol. 2000;7:593–600. doi: 10.1007/BF02725339. [DOI] [PubMed] [Google Scholar]
- 15.Pinto CH, Taminiau AH, Vanderschueren GM, Hogendoorn PC, Bloem JL, Obermann WR. Technical considerations in CT-guided radiofrequency thermal ablation of osteoid osteoma: tricks of the trade. AJR Am J Roentgenol. 2002;179:1633–1642. doi: 10.2214/ajr.179.6.1791633. [DOI] [PubMed] [Google Scholar]
- 16.Mirra J, editor. Bone Tumors: Clinical, Radiologic, and Pathologic Correlations. Philadelphia, PA: Lea & Febiger; 1989. pp. 143–438. [Google Scholar]
- 17.Bullough P, editor. Orthopaedic Pathology. Philadelphia, PA: Elsevier; 2004. pp. 371–373. [Google Scholar]
- 18.Vickers CW, Pugh DC, Ivins JC. Osteoid osteoma; a fifteen-year follow-up of an untreated patient. J Bone Joint Surg Am. 1959;41:357–358. [PubMed] [Google Scholar]
- 19.Yanagawa T, Watanabe H, Shinozaki T, Ahmed AR, Shirakura K, Takagishi K. The natural history of disappearing bone tumours and tumour-like conditions. Clin Radiol. 2001;56:877–886. doi: 10.1053/crad.2001.0795. [DOI] [PubMed] [Google Scholar]
- 20.Finstein J, Hosalkar H, Christian M, Lackman R. An unusual complication of radiofrequency ablation treatment of osteoid osteoma. Clinical Orthopaedics and Related Research. 2006;448:248–251. doi: 10.1097/01.blo.0000214412.98840.a1. [DOI] [PubMed] [Google Scholar]