Abstract
We describe a case of primary articular synovial chondromatosis in a metacarpophalangeal (MCP) joint of a 48-year-old male. The patient initially presented with MCP joint swelling and pain with normal plain radiographs. Following a fourteen month course of conservative management, surgical debridement of the joint revealed multiple loose bodies consistent with primary articular synovial chondromatosis. Though synovial chondromatosis rarely occurs in hand joints, the diagnosis should be considered in cases of metacarpophalangeal pain when common etiologies have been excluded.
CASE REPORT
A 48-year-old, left-hand dominant male was referred to our orthopedic hand clinic by rheumatologists after a long course of failed conservative therapy for pain and swelling in his left index and long metacarpophalangeal (MCP) joints of unknown etiology. The patient originally presented to the rheumatology clinic with a four-year history of pain that was interfering with his work as a Braille typist. Radiographs taken during the rheumatology evaluation did not reveal any loose bodies, erosions or joint space narrowing (Figure 1a). Past medical history was unremarkable for any trauma, infections, or rheumatologic conditions. Family history was positive for Systemic Lupus Erythematosus in a maternal female cousin but negative for rheumatoid arthritis or any seronegative spondyloarthropathy. After a trial of nonoperative treatment including high dose NSAIDs, intra-articular injections, oral corticosteroids, hydroxychloroquine, acetaminophen, Tramadol, topical capsaicin, and narcotic analgesics, the patient had persistent joint pain and swelling, prompting an MRI to further work-up the condition. The MRI revealed joint effusions with synovial proliferation and erosive changes in the long MCP joint and no changes in the index MCP (Figure 2). Because a diagnosis remained elusive, referral to an orthopedic hand surgeon was made for second opinion and possible biopsy. Upon presentation to our clinic, the patient reported his condition had forced him to discontinue his work as a Braille typist. He had moderate tenderness to palpation in the left index and long MCP joints. There was palpable swelling and thickening over the long MCP joint, but minimal swelling of the index MCP. Repeat plain radiographs were taken in the orthopedic clinic, fourteen months after the initial radiographs taken during the rheumatology work-up, which demonstrated several calcifications in the long MCP joint (Figure 1b). The differential diagnosis at this time included pauciarticular inflammatory arthritis, degenerative changes, or chronic infection from either fungal or mycobacterial origins.
Figure 1a.
Original plain radiograph shows no loose bodies or bony erosions.
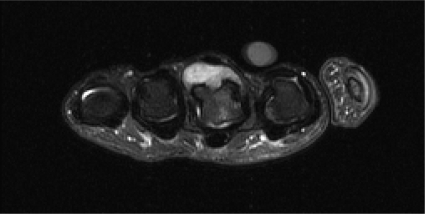
Figure 2.
MRI demonstrates long finger metacarpal head bony edema with adjacent synovial proliferation and joint effusion.
Figure 1b.
Plain radiograph taken fourteen months later reveals calcifications in the MCP joint of the left hand (small arrows).
Because the patient continued to have substantial functional deficits and pain, he was indicated for joint exploration and synovial biopsy. At surgery, multiple firm, smooth, white nodules were found in the long finger MCP joint. No evidence of similar pathology was found in the index MCP joint. The gross appearance of the nodules was consistent with synovial chondromatosis (Figure 3). Histologic studies revealed hypercellular nodules filled with binucleate chondrocytes lined by benign synovial tissue (Figure 4), further supporting the diagnosis of synovial chondromatosis. Mycobacterial and fungal cultures were negative.
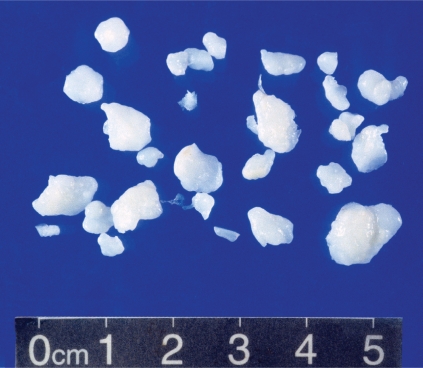
Figure 3.
The loose bodies removed were firm, white, smooth, chondroid nodules with homogeneous cut surfaces.
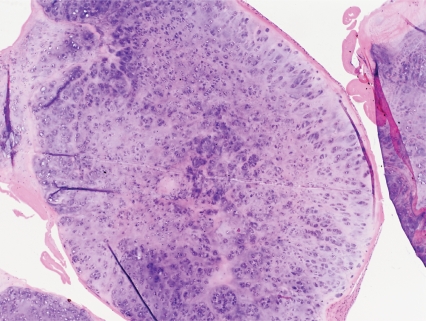
Figure 4.
Histologic examination reveals lobules of cartilage, with slightly increased cellularity, but no significant cellular atypia. The lobules are lined by benign synovium.
Physical therapy for range of motion was initiated two weeks after surgery. Three months after surgery, the patient’s pain has decreased, and his MCP range of motion has improved to 0 to 75 degrees in his index finger and 0 to 84 degrees in his long finger.
DISCUSSION
Primary synovial chondromatosis results from benign metaplasia of synovial tissue into cartilaginous tissue. The primary form of synovial chondromatosis is distinct from the more common secondary osteochondromatosis that consists of free articular cartilage fragments resulting from either degenerative disease or trauma. Primary synovial osteochondromatosis may arise from either articular synovium or tendon sheath synovium. Males are affected twice as frequently as females, and presenting symptoms can include pain, swelling, or decreased range of motion. The knee is the most common articular location followed by the hip and elbow. For lesions arising from tendon sheaths, the feet and hands are the most common locations. Review of the literature demonstrates that primary articular synovial chondromatosis of the MCP joint, as seen in our patient, is exceedingly rare. To our knowledge, the articular MCP location of this case of primary synovial chondromatosis has been previously reported only a handful of times.1–4 All of these reported cases were monoarticular in nature, and all were treated successfully with surgical debridement without recurrence.
The disease can also be classified based on the phase of maturation of the lesion. Milgram proposed three phases of the disease in 1977: early, transitional, and late. In early synovial chondromatosis, no loose bodies are present, but active synovial disease exists. In the transitional phase, there are both loose bodies and active synovial disease. Finally, in late synovial chondromatosis, there is no longer active synovial disease, but loose bodies persist.5 As in this case, patients that present in the early phase may have synovitis and pain without any radiographic changes, obscuring the diagnosis. In cases of refractory monarticular synovitis, repeat imaging may be indicated to look for the appearance of loose bodies. The presence of multiple intraarticular loose bodies on plain radiographs should raise suspicion of primary synovial chondromatosis, even in joints such as the MCP joint that are not typically affected by the disease.
Nonoperative treatments may ameliorate symptoms for some patients, but synovectomy and removal of loose bodies is indicated for persistent symptoms. Recurrence after resection has been reported, likely resulting from incomplete excision.6 Malignant degeneration of synovial chondromatosis is exceedingly rare.
In conclusion, primar y synovial chondromatosis should be included in the differential diagnosis of monoarticular synovitis of the MCP joints. Though plain radiographs may appear normal during the early phase of the disease, subsequent imaging may reveal intraarticular calcifications suggestive of loose bodies. Synovectomy successfully relieves pain and swelling in most cases.
REFERENCES
- 1.Linden O. Case of chondromatosis of a metacarpophalangeal joint. European Journal of Surgery. 1934;75:181. [Google Scholar]
- 2.Szepesi J. Synovial chondromatosis of the metacarpophalangeal joint: a case report. Acta. Orthopedica Scandinavica. 1975;46:926–930. doi: 10.3109/17453677508989280. [DOI] [PubMed] [Google Scholar]
- 3.Reed SC, Wright CS. Synovial chondromatosis of the metacarpophalangeal joint: case report and review of the literature. Canadian Journal of Surgery. 1996;39:407–409. [PMC free article] [PubMed] [Google Scholar]
- 4.Hettiaratchy SP, Nanchahal J. Synovial chondromatosis of the metacarpophalangeal joint. Journal of Hand Surgery. 2002;27B(1):104–106. doi: 10.1054/jhsb.2001.0677. [DOI] [PubMed] [Google Scholar]
- 5.Milgram JW. Synovial osteochondromatosis: a histopathological study of thirty cases. Journal of Bone and Joint Surgery. 1977;59A:792–801. [PubMed] [Google Scholar]
- 6.Floyd WE, III, Troum S. Benign cartilaginous lesions of the upper extremity. Hand Clinics. 1995;11:119–132. [PubMed] [Google Scholar]