Abstract
The information-motivation-behavioral skills (IMB) model (Fisher & Fisher, 1992) was used as the theoretical framework for predicting unprotected sexual behavior among substance abusing men and women diagnosed with serious mental illnesses (n = 320; 150 men and 170 women, primarily of minority ethnicity). In a structural equation model, gender, HIV transmission knowledge, and motivational variables of pro-condom norms and attitudes, and perceived susceptibility predicted behavioral skills markers: condom use skills and condom use self-efficacy. Along with the other variables in the model, condom skills and condom self-efficacy were hypothesized to predict condom use over a six-month period. Results showed that greater condom skills were predicted by female gender, positive condom attitudes, and transmission knowledge. Engaging in lower rates of unprotected sex was predicted by pro-condom norms, less perceived susceptibility, and greater condom self-efficacy. Positive attitudes toward condoms had a significant indirect effect on rates of unprotected sex, exerting its influence through condom use self-efficacy. Results suggest that changing personal attitudes about condoms and reinforcing pro-condom attitudes among significant others will encourage condom use among seriously mentally ill (SMI) adults who are at high risk for HIV and other sexually transmitted diseases (STDs).
Keywords: HIV AIDS prevention, psychiatric patients, seriously mentally ill adults
Recent years have seen remarkable breakthroughs in the treatment of HIV infection and there is some evidence for a leveling of new HIV infections in some subpopulations (CDC, 2001). Along with these reasons for hope, however, is the continued spread of HIV in US inner-cities, particularly among impoverished and disenfranchised populations. Among those at greatest risk for HIV infection are adults with serious and persistent mental illnesses living in high HIV prevalence cities. Comprehensive reviews of HIV seroprevalence studies show that approximately 8% of adults with serious mental illnesses in large cities are HIV positive (Carey, Weinhardt, & Carey, 1995; Cournos & McKinnon, 1997). One study of over 500 psychiatric patients found that 6% were HIV infected (Stewart, Zuckerman, & Ingle, 1994) and Rosenberg et al. (2001) reported 3% HIV seroprevalence in a large and ethnically diverse sample of seriously mentally ill (SMI) adults. These rates of HIV infection exceed those in the general population and are often higher than rates found in the highest risk groups, such as injection drug users and sexually transmitted disease (STD) clinic patients (Carey et al., 1997a).
The alarming numbers of HIV infected adults with serious mental illness are exacerbated by high-rates of unprotected sexual activity routinely found in SMI adults (e.g., Kalichman, Kelly, Johnson, & Bulto, 1994; Carey et al., 1997a). Seriously mentally ill adults often have the same risk factors identified in other at-risk populations, such as substance-related disorders which may occur in more than half of people with diagnosed mental disorders (Mueser et al., 1990, 1995; Drake et al., 1991). HIV risks have also been associated with psychiatric symptoms such as impulsivity, sexual acting out, and deficits in social skills and problem solving (Kalichman, Carey, & Carey, 1996). In addition, the downward spiral of mental illness is related to risk-producing social interactions such as transient sexual relationships often involving “survival sex,” exploitation and coercion (Kelly, 1997; Cournos & McKinnon, 1997). Although these social and contextual factors provide insight into the risk behaviors of many men and women with serious mental illnesses, contextual characteristics do not translate directly into intervention strategies aimed at reducing risks. The potential for rapid spread of HIV among the SMI has led to the urgent call for the development of risk reduction interventions designed for people with serious mental illness.
HIV risk reduction interventions designed and tested with seriously mentally ill adults have been based on social cognitive theories of behavior change (Kalichman, Sikkema, Kelly, & Bulto, 1995; Otto-Salaj et al., 2001; Susser et al., 1998). Although a variety of theoretical frameworks have been used as the basis for prevention strategies targeted to the SMI, all of these interventions included information-education, motivational enhancement, and cognitive behavior skills building, all elements of the information-motivation-behavioral skills (IMB) model of health behavior (Fisher & Fisher, 1992). The IMB model states that HIV preventive behavior, such as condom use, is a function of HIV prevention information (e.g., risk education and facts about HIV disease), HIV prevention motivation (e.g., risk sensitization, personal risk recognition, intentions to reduce risk), and AIDS prevention behavioral skills (e.g., interpersonal communication skills, condom skills; (Fisher & Fisher, 1992; Fisher, Fisher, & Malloy, 1994)). Studies have found SMI adults lack correct AIDS information, hold more negative attitudes toward condoms, and demonstrate poor self-efficacy, supporting the use of the IMB model with SMI adults. (Carey, Carey, & Kalichman, 1997a; Carey, Carey, Weinhardt, & Gordon, 1997b; Gordon, Carey, Carey, & Maisto, 1999). Unfortunately, none of the prevention trials tested with seriously mentally ill adults reported thus far have investigated the effects of potential theoretical mediators of behavior change on risk reduction outcomes.
In the IMB model, protective behavioral skills represent a final common pathway for predicting complex preventive behaviors, such as condom use. It is common for studies to use measures of self-efficacy for performing a behavior, that is confidence that one has in their ability to perform a specific behavior under challenging conditions, as a proxy for behavioral skills (e.g., Kalichman, et al., 2001). However, self-efficacy may not represent skill performance as much as personal acceptance for practicing a skill. Direct observational condom skills assessments, however, may offer a better estimate of condom use proficiency that is more relevant to skill performance. In the current study, we include both a measure of self-efficacy and a direct observation measure of condom use proficiency skills as indicators of behavioral skills in the IMB framework.
The current study examined the HIV risk reduction intervention-oriented IMB model in a sample of SMI adults. Specifically, we used Fisher and Fisher’s (1992) IMB model of HIV preventive behavior change to examine risk reduction behaviors in substance using men and women diagnosed with serious and persistent mental illnesses. Using structural equation modeling (SEM), we tested associations among IMB constructs as predictors of risk behaviors in SMI adults. As a fundamental aspect of this research, we included two independent indicators of risk reduction behavioral skills – condom use self-efficacy and observed condom use proficiency skills – and we directly compared the relative contributions of these behavioral skill indicators as predictors of risk reduction in the context of the IMB model.
METHODS
Participants
Participants were 150 severely mentally ill men and 170 women attending community-based substance abuse treatment programs. The typical participant was a single, indigent, ethnic or racial minority adult who abused alcohol, non-injection “crack” cocaine and/or marijuana, and who resided within the inner-city areas of Miami-Dade county. The mean age of the sample was 38.9 years (SD = 9.2), and the average years of education was 11.5 years (SD = 2.6). Fifty-two percent of participants were African-Americans (n = 170), 26.6% were Non-Hispanic White (n = 87); 18% were Hispanic of Mexican, Cuban or Puerto Rican origin (n = 59); and 3.6% identified as either Native American, Asian, “other”, or declined to state (n = 11). Seven percent of the participants were currently married, and an additional 11% stated that they were in a common-law relationship that had lasted for more than 2 years. In terms of HIV testing history, 80% of participants were tested, and 12% were HIV positive. In the current study, HIV positive participants were excluded from analyses.
All participants were screened for eligibility using a brief screening checklist, administered prior to gaining informed consent and proceeding with the intake assessment. Participants met the following entry criteria: (a) planned to live in the local area (Miami-Dade Florida) for the next year; (b) had a history of alcohol and drug problems; and (c) were sexually active in the past six-months. Additional inclusion criteria were a history of severe mental illness, as determined by DSM-IV diagnosis (30% schizophrenia, 20% schizoaffective, 20% bipolar and 30% major depressive disorders) receipt of public-sector treatment for severe and persistent mental illness, and current or recent use of psychotropic medication.
Assessment Procedures
Assessments were conducted in a one-on-one format by trained interviewers with previous experience working with SMI populations. All participants signed approved informed consent documents and were instructed as to what the study entailed. Assessors emphasized the confidential nature of the study and encouraged participants to ask questions about involvement in the protocol. In order to ensure adequate detoxification, measures were administered at least one week after admission to the treatment programs. Assessment staff underwent extensive training under a licensed clinical psychologist, including assigned readings, role-playing exercises, supervised practice in assessing confederate participants, and, at a minimum, four complete, supervised pilot assessments. All assessments were audiotaped for quality assurance monitoring. An administration manual and a procedural checklist was developed and used to ensure standardized administration of the assessment measures.
Measures
The latent variables described below were primarily based on responses to multi-item scales that were hypothesized to reflect key constructs of the IMB model. Responses are used as measured indicators of underlying latent variables. Single items were used to represent some constructs. To improve the specificity of the model, as recommended by Fisher and Fisher (1992), all measures included in the model were primarily focused on condom use during vaginal intercourse.
Information
Knowledge
Knowledge regarding HIV transmission modes was assessed using the 6 condom-specific items from a scale adapted from St. Lawrence, Jefferson, Alleyne and Brasfield (1995) in which items are rated “true” or “false”. Illustrative item: “Condoms make intercourse completely safe”. The number of correctly answered items served as a single score indicator of Knowledge.
Motivation
Pro-Condom Norms were assessed with a measure of perceived social norms adapted from Jemmott, Jemmott, and Fong (1992), which assesses (1) how important the approval of referents was in using condoms, 1 = “extremely unimportant”, 5 = “extremely important”, and (2) how much these referents would approve or disapprove of their use of condoms, 1 = “disapprove strongly”, 5 = “approve strongly”. Key referents included “most people important to you”, “your most recent sex partner”, “your parents”, and “your friends”. The mean of the responses associated with the two items for each key referent were calculated yielding four items as indicators of a latent variable of pro-condom norms.
Condom Attitudes were assessed as a second motivational indicator with the 20-item condom attitudes scale from the AIDS Risk Reduction Model (ARRM) Questionnaire Revised (ARRM-QR: Gibson, Lovelle-Drache, Young, & Chesney, 1992). The ARRM-QR was developed to reliably and validly measure HIV-specific prevention constructs (Catania, Kegeles & Coates, 1990). Typical items from the scale included: “A condom is not necessary if you know the person” and “Condoms are messy”. The items were scored on a scale ranging from 1 = “disagree strongly”, to 4 = “agree strongly”. Items were reverse-scored where appropriate so that higher scores indicated more positive attitudes toward use of condoms. To reduce the number of indicators, the 20 items were combined randomly into 4 parcels used as measured indicators and were labeled condom attitudes 1, condom attitudes 2, condom attitudes 3, and condom attitudes 4, with means of the combined items used for each parcel.
Perceived susceptibility was used as a third indicator of motivation and was assessed by one item from the ARRM-QR: “It would be easy for me to get the HIV infection or AIDS.” This item was scored 1 = “disagree strongly”, 4 = “agree strongly", and not reverse-scored. Therefore, a high score indicates more feelings of vulnerability or susceptibility to AIDS.
Behavioral Skills
Condom Self-Efficacy, defined as confidence in one’s ability to adopt and maintain condom use under challenging conditions (Bandura, 1997), was used as an indicator of condom use behavioral skills. Six items from the ARRM-QR (Gibson et al., 1992) were paired randomly and summed to create three indicators of condom self-efficacy. Representative items included: “It’s hard to always use condoms”, and “Safer sex is hard when you’re really turned on to someone”. Items were responded to on a four-point scale, 1 = “disagree strongly”, 4 = “agree strongly”, and reverse-scored so that higher scores indicate greater self-efficacy.
Condom skills were determined by rating the participant’s ability to properly enact nine steps for correctly placing a condom on a penis model (adapted from Somlai et al., 1998; Sorensen, London, & Morales, 1991). Participants were scored for the presence or absence of specific actions, including opening the condom package without tearing the condom; pinching the tip of the condom to remove air; and rolling the condom to the base of the penis model. This measure recorded observed actions and was developed as a simple direct observation measure of condom use skills. Scores reflect the total number of correct observed steps.
Sexual Risk Behaviors
Sexual risk behaviors were assessed using a modified version of a sexual risk assessment instrument previously used in other research (Kalichman et al., 1994). The sexual risk assessments included retrospective recall of numbers of unprotected and protected sex acts during the previous six-months. Percentage of unprotected vaginal sex acts was calculated by taking the proportion of unprotected acts relative to all acts of vaginal intercourse and used as the dependent variable in this study.
Data Analyses
The structural equation model presented here was guided by the IMB model described above (Fisher & Fisher, 1992). The model simultaneously examines whether variables related to information and motivation are significant predictors of behavioral skills (condom skills and condom self-efficacy), and whether condom skills and/or self-efficacy in turn are significant predictors of percent unprotected sex in the past six-months. Gender was included as an additional control in predicting risk reduction behavioral skills. In preliminary analyses, the influence of age was tested and, because it was not related to any variable of interest in the model, was not included in the analyses reported below in the interest of parsimony.
The latent variable analyses were performed using the EQS SEM program (Bentler, 2002). Structural equation modeling compares a model specifying hypothesized relationships in the data, in this case the IMB model, with a set of actual data. The closeness of fit between the theoretical model and the data is evaluated through various goodness of fit indices; comparative fit index (CFI) and Robust CFI (RCFI), chi-square values (both maximum likelihood (ML χ 2) and the adjusted Satorra-Bentler robust χ 2 (S-B χ 2), and the root mean square errors of approximation (RMSEAs, Bentler, 2002; Bentler & Dudgeon, 1996; Hu & Bentler, 1999). The CFI and RCFI indicate the proportion of improvement in the overall fit of the hypothesized model relative to a null model in which all covariances between variables are zero; values of .95 or greater are desirable for the CFI and RCFI (Hu & Bentler, 1999). The RMSEA indicates the size of the residuals between the hypothesized model and the observed data; values less than .06 indicate a good fit (Hu & Bentler, 1999).
RESULTS
The means, standard deviations, and ranges for the information, motivation, behavioral skills, and behavior variables appear in Table 1. Knowledge about the role of condoms in lowering HIV risk was high; the average knowledge test score was 5 out of a possible 6 correct responses; however 30% of the sample scored 4 or less on the knowledge test. As measured by the number of correct steps demonstrated on the objective condom skills task, the average participant performed slightly over half of the nine steps correctly (Mean = 5, Median = 5). Less than 1% (n = 3) correctly performed all nine of the condom skills steps, and 55% failed to perform at least six of the steps correctly. Results showed this sample presented relatively high rates of risk behaviors for HIV and other STDs. On average participants reported that 30% of their vaginal intercourse occasions in the previous six-months were unprotected. Forty-four percent of participants reported 100% condom use in the past six-months, and 25% reported never using a condom during that time period.
TABLE 1.
Descriptive Statistics and Factor Loadings of Measured Variables in the Confirmatory Factor Analysis of IMB Model Variables Among Severely Mentally Ill Adults (n = 327)
| Variable | Range | Mean | SD | Factor Loading* |
|---|---|---|---|---|
| Gender (0 = male, 1 = female) | 0–1 | .54 | .47 | N.A. |
| Knowledge | 1–6 | 5.01 | 1.13 | N.A. |
| Pro-condom Norms | ||||
| Important People | 1–5 | 4.09 | .92 | .58 |
| Sex Partner | 1–5 | 3.79 | 1.08 | .50 |
| Parents | 1–5 | 4.29 | .75 | .59 |
| Friends | 1–5 | 3.97 | .97 | .70 |
| Condom Attitude | ||||
| Condom Attitude 1 | 1–4 | 3.21 | .47 | .63 |
| Condom Attitude 2 | 1–4 | 3.30 | .52 | .73 |
| Condom Attitude 3 | 1–4 | 3.44 | .46 | .64 |
| Condom Attitude 4 | 1–4 | 2.88 | .74 | .68 |
| Perceived Susceptibility | 1–4 | 2.98 | 1.18 | N.A. |
| Condom Self-efficacy | ||||
| Self-efficacy 1 | 1–4 | 2.87 | .70 | .57 |
| Self-efficacy 2 | 1–4 | 2.91 | .74 | .57 |
| Self-efficacy 3 | 1–4 | 3.17 | .60 | .62 |
| Condom Skill | (0–9) | 5.01 | 1.84 | N.A. |
| Six-month Unprotected Sex (%) | (0–100) | 38 | 43 | N.A. |
All factor loadings significant, p ≤ .001.
Confirmatory Factor Analysis of IMB Model Components
A preliminary confirmatory factor analysis (CFA) model estimated the factor structure and relationships among all of the IMB variables and the demographic variable of gender. Table 1 reports the factor loadings from the CFA model. All factor loadings were significant (p ≤ 0.001). Fit indexes were also in the acceptable range: ML χ2 = 129.3, df = 81; CFI = .94, RMSEA = .04. Robust statistics were somewhat better: S-B χ2 = 117.04, df = 81; RCFI = .95, RMSEA = .04. The standardized kurtosis estimate was 8.8, which indicates that the Robust solution may be more reliable in this model. However, both methods indicated a well-fitting structure. No supplementary paths or covariances were added to this initial model.
Table 2 reports the bivariate correlations among constructs in the model without any directionality of influence among them. The women reported more positive condom attitudes and demonstrated better condom skills. Favorable condom attitudes were significantly and positively associated with each IMB variable except for perceived susceptibility; favorable condom attitudes were significantly and negatively associated with unprotected sex. More knowledge was significantly associated with more positive condom attitudes, and greater condom skills. Pro-condom norms were significantly associated with positive condom attitudes, greater condom use self-efficacy, and less unprotected sex. Perceived susceptibility was negatively associated with more unprotected sex. Condom self-efficacy was significantly correlated with more skills and less unprotected sex.
TABLE 2.
Correlations Among Constructs in IMB Model Among Severely Mentally Ill Adults
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| Knowledge | – | ||||||
| Pro-condom Norms | .04 | – | |||||
| Condom Attitudes | .30*** | .44*** | – | ||||
| Perceived Susceptibility | .01 | .11 | .09 | – | |||
| Condom Skills | .15** | −.03 | .23*** | −.04 | – | ||
| Condom Self-efficacy | .11 | .26*** | .68*** | .02 | .23*** | – | |
| Six-months Unprotected Sex | .09 | −.26*** | −.31*** | −.10* | −.10* | −.26*** | – |
| Female Gender | .06 | .03 | .21*** | .08 | .16** | .10 | .05 |
p ≤ .05,
p ≤ .01,
p ≤ .001.
Predictive Structural Equation Model
The final predictive IMB structural equation model is presented in Figure 1. Through use of procedures suggested by MacCallum (1986), non-significant paths were gradually dropped until only significant ones remained in this final trimmed model. Measured variables are in rectangles and multiple-indicator latent variables are in ovals. Fit indexes were acceptable: ML χ 2 = 147.6, df = 96; CFI = .94, RMSEA = .04. Robust statistics were better and are more appropriate: S-B χ2 = 135.4, df = 96; RCFI = .95, RMSEA = .03.
FIGURE 1.
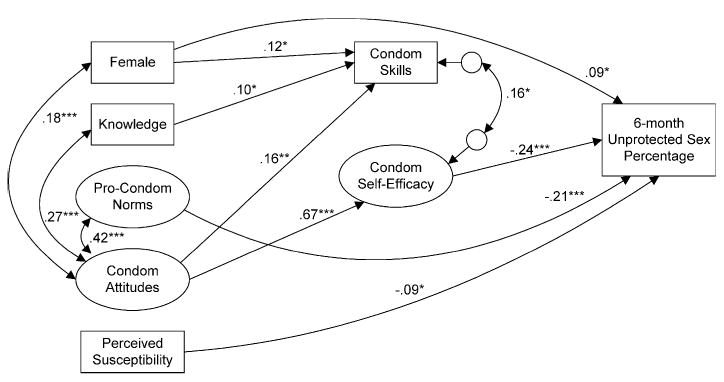
Significant Regression Paths in IMB Model Predicting Six-Month Unprotected Sex Percentage Among 327 Severely Mentally Ill Individuals. Ovals Represent Multiple-Indicator Latent Variables, Rectangles Represent Single-Item Indicators
Lines with Single Arrows Represent Regression Paths, Double-Headed Arrows Represent Significant Correlations Between the Predictors. Regression Coefficients are Standardized (*p ≤ .05, **p ≤ .01, ***p ≤ .001).
Greater condom skills were predicted by female gender, positive condom attitudes, and greater knowledge. Condom self-efficacy was strongly predicted by condom attitudes. Female gender was a significant predictor of more unprotected sex. Less unprotected sex was predicted by pro-condom norms, less perceived susceptibility, and greater condom self-efficacy. In addition, although the latent variable of positive condom attitudes was not a significant direct predictor of less unprotected sex, it was a significant indirect predictor, exerting its influence through condom use self-efficacy (p ≤ .01; standardized regression coefficient of the indirect effect = −.16).
DISCUSSION
The current study findings may help further our understanding of the positive and negative outcomes of past HIV risk reduction interventions and may have practical implications for refining and tailoring future prevention interventions for SMI adults. However, these implications may be constrained by several methodological considerations. Our study, like others in the field of HIV risk and risk reduction, relied on self-report behavioral assessments. Due to the sensitivity of sexual and substance use issues that were assessed, social desirability biases, privacy concerns, and potential embarrassment may have led to under-reporting of key behaviors. Although our study included a measure of direct observation for condom use proficiency skills, the possible effects of self-report biases on all other measures must be considered. In addition, the current study was conducted with SMI adults receiving mental health services from a psychiatric facility in an AIDS epicenter. Therefore, the study findings may have limited generalizability to other clinical populations. Finally, our findings are based on a relatively small sample size, suggesting the need for further studies to replicate the observed associations. Despite these study limitations, the current findings are likely to offer new information regarding HIV risks and the use of the IMB model in predicting risk reduction behaviors in adults with serious mental illnesses.
Previous HIV risk reduction efforts have delivered intervention components that are consistent with the information-education, motivational enhancement, and behavioral skills building activities that encompass the IMB model of health behavior change. However, prevention interventions for SMI adults have not yet tested mediating effects of any theoretical constructs on risk behavior change. We assert that interventions that have demonstrated positive outcomes are those that have most effectively increased positive attitudes toward condoms and increased perceived self-efficacy for instituting risk behavior changes. Although all interventions for SMI adults have reported using skills rehearsal to improve condom application skills, we did not find evidence for an association between proficiency in applying condoms with fewer errors and actual condom use. Thus, our data suggest that behavioral skills training for proficient use of condoms will only be effective to the degree that the training exercises build confidence or self-efficacy in the ability to use condoms under difficult circumstances. We also contend that the effects of skills proficiency training in other risk reduction behavioral domains, such as maintaining abstinence and cleaning injection equipment, will be due to enhanced self efficacy.
Our findings also help explain gender differences observed in some HIV risk reduction interventions for SMI adults. Intervention studies have shown more positive risk reduction behavioral changes in SMI women than men. For example, Otto-Salaj et al. (2001) found that an HIV risk reduction intervention that included IMB components increased frequency of condom-protected sex, the percentage of protected vaginal intercourse occasions, and increased positive attitudes toward condoms. However, there were large gender differences displayed in response to this intervention. Men showed only significant change in HIV risk knowledge scores in response to the intervention, whereas women showed significant changes in condom attitudes, risk reduction behavioral intentions, and reported reductions in sexual risk behaviors between baseline and six-month follow-up assessments (Otto-Salaj et al., 2001). Results of the current study demonstrated more positive attitudes toward condoms and greater proficiency in applying condoms among women. We conclude that a greater degree of comfort and openness toward condoms among women may facilitate the adoption of risk reduction practices resulting from intervention activities. That women in the current study were found to have more positive condom attitudes and more proficient condom skills, and yet were engaging in high rates of risk practices indicates the need for prevention interventions targeted to women with serious mental illnesses.
There remains an urgent need for HIV prevention interventions for men and women diagnosed with serious mental illnesses. Interventions that provide risk and preventive education, sensitize people to their risks, facilitate personal and social normative acceptance of condoms, and enhance self-efficacy for using condoms hold the greatest promise for risk behavior change. It is essential that HIV risk reduction interventions be adapted for SMI men and women, particularly attending to gender specific needs and values. Finally, it is essential that risk reduction interventions at the very least be designed for implementation by community service providers, and optimally be integrated within existing community services. For example, HIV risk reduction interventions delivered in small groups can be integrated into community programs that conduct group education or group therapy, or can be placed within the context of inpatient or outpatient substance abuse treatment services. In addition, case management and one-on-one counseling services can integrate the same IMB intervention components typically found in small group interventions (Kalichman et al., 2001). Behavioral interventions remain the only hope for stemming the spread of HIV-AIDS and those interventions that are grounded in sound behavior change theory offer the greatest hope for preventing new HIV infections.
Acknowledgments
This work was funded in part by R01 AA12115 from NIAAA awarded to Dr. Malow and Grant PO1 DA 01070-28 from NIDA (Dr. Stein).
References
- Bandura A. Self-efficacy: The exercise of control. New York: Freeman; 1997. [Google Scholar]
- Bentler PM. EQS 6 structural equations program manual. Encino, CA: Multivariate Software, Inc; 2002. [Google Scholar]
- Bentler PM, Dudgeon P. Covariance structure analysis: Statistical practice, theory, and directions. Annual Review of Psychology. 1996;47:563–592. doi: 10.1146/annurev.psych.47.1.563. [DOI] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Kalichman SC. Risk for human immunodeficiency virus (HIV) infection among persons with severe mental illness. Clinical Psychology Review. 1997a;17:271–291. doi: 10.1016/s0272-7358(97)00019-6. [DOI] [PubMed] [Google Scholar]
- Carey MP, Carey K, Weinhardt L, Gordon C. Behavioral risk for HIV infection among adults with a severe and persistent mental illness: Patterns and psychological antecedents. Community Mental Health Journal. 1997b;33:133–142. doi: 10.1023/a:1022423417304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Weinhardt LS, Carey KB. Prevalence of infection with HIV among the seriously mentally ill: Review of research and implications for practice. Professional Psychology: Research and Practice. 1995;26:262–268. [Google Scholar]
- Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behavior: An AIDS risk reduction model (ARRM) Health Education Quarterly. 1990;17:53–72. doi: 10.1177/109019819001700107. [DOI] [PubMed] [Google Scholar]
- CDC. HIV incidence among young men who have sex with men – seven US cities 1994–2000. MMWR. 2001;50:440–444. [PubMed] [Google Scholar]
- Cournos F, McKinnon K. HIV seroprevalence among people with severe mental illness in the United States: A critical review. Clinical Psychology Review. 1997;17:259–269. doi: 10.1016/s0272-7358(97)00018-4. [DOI] [PubMed] [Google Scholar]
- Drake R, McLaughlin P, Pepper B, Minkoff K. Dual diagnosis of major mental illness and substance disorder: An overview. New Directions for Mental Health Services. 1991;50:3–12. doi: 10.1002/yd.23319915003. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychology. 1994;13:238–250. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- Gibson DR, Lovelle-Drache J, Young MT, Chesney M. HIV risk linked to psychopathology in IV drug users. International Conference on AIDS, Abstract POC 4691. 1992:1992. [Google Scholar]
- Gordon C, Carey M, Carey K, Maisto S, Weinhardt L. Understanding HIV related risk among persons with severe and persistent mental illness: Insights from qualitative inquiry. Journal of Nervous and Mental Disease. 1999;187:208–216. doi: 10.1097/00005053-199904000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jemmott JB, Jemmott LS, Fong GT. Reductions in HIV risk-associated sexual behaviors among black male adolescents: Effects of an AIDS prevention intervention. American Journal of Public Health. 1992;82:372–377. doi: 10.2105/ajph.82.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Carey MP, Carey KB. Human immunodeficiency virus (HIV) risk among the seriously mentally ill. Clinical Psychology: Science and Practice. 1996;3:130–143. [Google Scholar]
- Kalichman SC, DiFonzo K, Kyomugsha F, Simpson D, Presser K, Bjordstrom B. When briefer can be better: Single session approaches to HIV risk reduction interventions. Interamerican Journal of Psychology. 2001;35:41–58. [Google Scholar]
- Kalichman SC, Kelly JA, Johnson J, Bulto M. Factors associated with risk for Human Immunodeficiency Virus (HIV) infection among chronic mentally ill adults. American Journal of Psychiatry. 1994;151:221–227. doi: 10.1176/ajp.151.2.221. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Sikkema KJ, Kelly JA, Bulto M. Use of a brief behavioral skills intervention to prevent HIV infection among chronic mentally ill adults. Psychiatric Services. 1995;46:275–280. doi: 10.1176/ps.46.3.275. [DOI] [PubMed] [Google Scholar]
- Kelly JA. HIV risk reduction interventions for persons with severe mental illness. Clinical Psychology Review. 1997;17:293–209. doi: 10.1016/s0272-7358(97)00020-2. [DOI] [PubMed] [Google Scholar]
- MacCallum R. Specification searches in covariance structure modeling. Psychological Bulletin. 1986;100:107–120. [Google Scholar]
- Mueser KT, Bennett M, Kushner MG. Epidemiology of substance abuse among persons with chronic mental disorders. In: Lehman AF, Dixon L, editors. Double Jeopardy: Chronic Mental Illness and Substance Abuse. New York: Harwood Academic Publishers; 1995. [Google Scholar]
- Mueser KT, Yarnold PR, Levinson DF, Singh H, Bellack AS, Kee K, Marrison RL, Yadalam KG. Prevalence of substance abuse in schizophrenia: Demographic and clinical correlates. Schizophrenia Bulletin. 1990;16:31–56. doi: 10.1093/schbul/16.1.31. [DOI] [PubMed] [Google Scholar]
- Otto-Salaj L, Kelly J, Stevenson L, Hoffman R, Kalichman S. Outcomes of a randomized small-group HIV prevention intervention trial for people with serious mental illness. Community Mental Health Journal. 2001;37:123–144. doi: 10.1023/a:1002709715201. [DOI] [PubMed] [Google Scholar]
- Rosenberg SD, Goodman LA, Osher FC, Swartz M, Essock SM, Butterfield MI, Constantine N, Wolford GL, Salyers M. Prevalence of HIV, Hepatitis B and Hepatitis C in people with severe mental illness. American Journal of Public Health. 2001;91:31–37. doi: 10.2105/ajph.91.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somlai A, Kelly J, McAuliffe T, Gudmundson J, Murphy D, Sikkema K, Hackl K. Role play assessments of sexual assertiveness skills: Relationships with HIV/AIDS sexual risk behavior practices. AIDS and Behavior. 1998;2:319–328. [Google Scholar]
- Sorensen JL, London J, Morales E. Group counseling to prevent AIDS. In: Sorensen J, Wermuth D, Gibson K, Choi J, Guydish S, Batki S, editors. Preventing AIDS in drug users and their sexual partners. Guilford; New York: 1991. pp. 99–115. [Google Scholar]
- Stewart DL, Zuckerman CJ, Ingle JM. HIV seroprevalence in a chronically mentally ill population. Journal of the National Medical Association. 1994;86(7):519–523. [PMC free article] [PubMed] [Google Scholar]
- St Lawrence JS, Jefferson KW, Alleyne E, Brasfield TL. Comparison of education versus behavioral skills training interventions in lowering sexual HIV-risk behavior of substance-dependent adolescents. Journal of Consulting and Clinical Psychology. 1995;63:154–157. doi: 10.1037//0022-006x.63.1.154. [DOI] [PubMed] [Google Scholar]
- Susser E, Valencia E, Berkman A, Sohler N, Conover S, Torres J, Betne P, Felix A, Miller S. Human immunodeficiency virus sexual risk reduction in homeless men with mental illness. Archives of General Psychiatry. 1998;55:266–272. doi: 10.1001/archpsyc.55.3.266. [DOI] [PubMed] [Google Scholar]


