Abstract
Objective
To examine the effect of first trimester obstetric ultrasound (OBUS) on the measurement of the effect of complications ascribed to postterm pregnancies.
Study Design
We conducted a retrospective cohort study of all term, singleton pregnancies delivered at our institution who had an OBUS at ≤24 weeks of gestation. Those women who underwent an OBUS at ≤12 weeks of gestation (OBUS12) were compared to those who had an OBUS at 13–24 weeks of gestation (OBUS13–24). The primary outcome measures were the rates of postterm pregnancies greater than 41 or 42 weeks’ gestation. Secondary outcomes were the differences between the postterm and term gestations in maternal and neonatal outcomes.
Results
In the OBUS12 group, the rate of postterm pregnancy ≥42 weeks was lower (2.7%) as compared to the OBUS13–24 group (3.7%, p=0.022). With regards to reaching 41 weeks of gestation, the OBUS12 group was again lower (18.2%) as compared to the OBUS13–24 group (22.1%, p<0.001). There were also fewer postterm inductions at ≥42 weeks in the OBUS12 group (1.8%) as compared to the OBUS13–24 group (2.6%, p=0.017). When comparing perinatal outcomes between those women who reached 41 weeks of gestation and those prior to 41 weeks of gestation, the OBUS12 group demonstrated greater differences between these two groups.
Conclusion
Our findings suggest that earlier obstetric ultrasound, which leads to better pregnancy dating, reduces the rate of estimated postterm pregnancies. This may, in turn, reduce unnecessary intervention and lead to better identification of postterm pregnancies at greater risk of complications.
Keywords: pregnancy dating, ultrasound, complications of pregnancy, post-term, post-dates
Introduction
Postterm pregnancy continues to be defined as one that progresses to and beyond 42 completed weeks, or 294 days, of gestation.1 This definition is based primarily on outcomes research more than two decades old that demonstrated that pregnancies progressing beyond 42 weeks gestation had higher rates of morbidity and mortality. 2,3,4 However, more recent data finds that pregnancy complications, as well as risk of cesarean delivery, increase beyond 40 and 41 weeks of gestation.5,6,7
One of the reasons for the differences seen between the older and more recent data may be due to improved pregnancy dating since the advent of real time ultrasound.8 It has been demonstrated that improved pregnancy dating leads to fewer women being identified as having postterm pregnancies or requiring induction of labor.9,10 Such improved dating reduces the problem of misclassification bias that exists with the use of dating by history and physical exam. Misclassification bias occurs both because of incorrect memory of the last menstrual period (LMP) as well as oligo- and poly-ovulation. In the setting of each of these events, an estimated date of confinement (EDC) is incorrect and leads to women’s gestational age at delivery being incorrect.
With oligo-ovulation or incorrect recall, a woman may have actually ovulated later than predicted by the LMP, and is thus at an earlier gestational age than predicted. With poly-ovulation or incorrect recall, a woman may have actually ovulated earlier than predicted by the LMP, and is actually at a later gestational age than predicted. With either of these forms of misclassification, the difference in perinatal outcomes between term and postterm pregnancies will be underestimated. In the setting of pregnancies that are actually earlier than predicted, when they progress beyond 41 or 42 weeks of gestation, they are actually earlier and carry the lower risks of an earlier gestation decreasing the difference in perinatal complications (Figure 1). In the setting of pregnancies that are actually further along than predicted, when they deliver at 37–39 weeks of gestation, but are actually 40–42 weeks of gestation, they would increase the perceived risk of term complications among the younger gestational age group. Again, this would decrease the perceived difference in perinatal complications between term and postterm pregnancies. Of note, since it appears that women are more likely to be oligo-ovulatory than poly-ovulatory, the former situation is more likely to exist, thus more women may have been traditionally misdiagnosed as postterm.8
Figure 1. Misclassification Bias and the Comparison Between Term and Postterm Pregnancies.
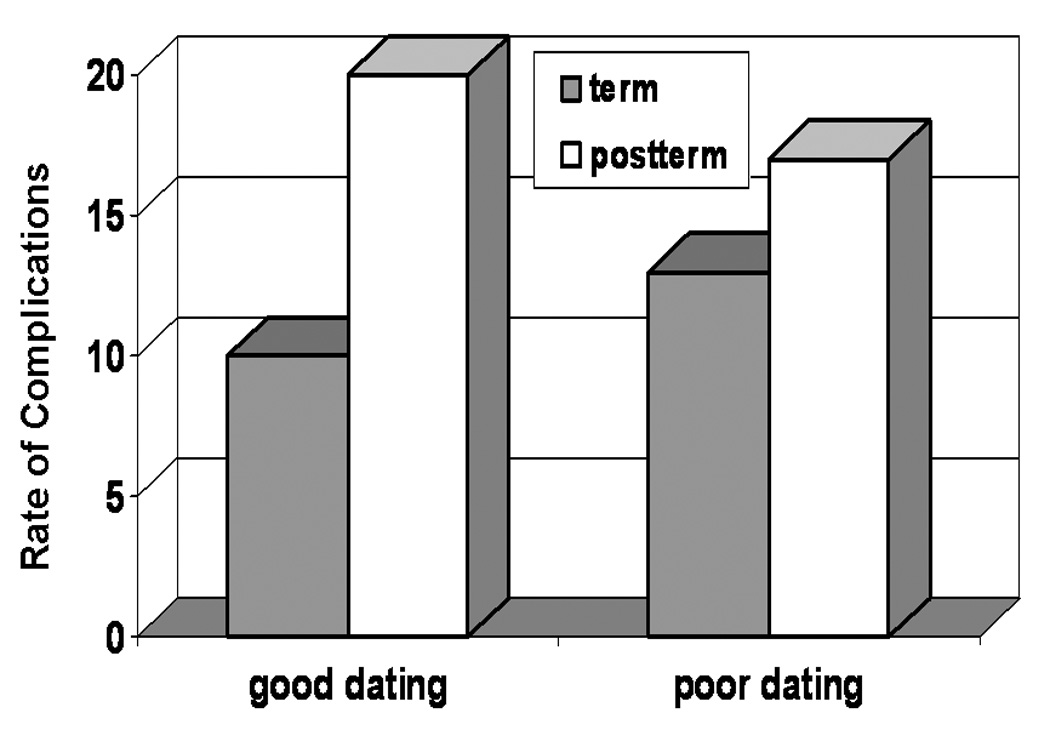
In the figure, note that due to misclassification bias in the poor dating group, the rate of complications is higher in the women diagnosed as term pregnancies due to the inclusion of postterm pregnancies and the rate of complications is lower in the women diagnosed as postterm pregnancies due to the inclusion of term pregnancies. Thus, in the group of women with good dating, the difference in complications between the term and postterm women is greater.
Given these suppositions, ultrasound dating should lead to a lower rate of women being diagnosed as having postterm pregnancies. Further, women who experience a first trimester ultrasound should be at even a lower risk of being diagnosed as postterm than those whose first ultrasound in pregnancy is later. Further, women with a first trimester ultrasound should demonstrate a greater difference in perinatal complications between those with term and postterm pregnancies than those with a second trimester ultrasound only.
In order to test the hypothesis that improved ultrasound dating by first trimester ultrasound both decreases the diagnosis of postterm pregnancy and increases the differential in perinatal complications in those with a postterm pregnancy, we examined this effect in a cohort of women at our institution.
Materials and Methods
We designed a retrospective cohort study of all women delivered beyond 37 weeks gestational age from January 1, 1992 to December 31, 2001 at Moffitt-Long Hospital affiliated with the University of California, San Francisco (UCSF) in order to compare women who experienced a first trimester ultrasound (OBUS12 - less than or equal to 12 weeks gestation) to those who experienced a second trimester ultrasound (OBUS13–24 - 13 to 24 weeks gestation). Medical records were abstracted to determine whether women had received an obstetric ultrasound during their pregnancy. Patients were included in the analysis if they delivered a nonanomalous, singleton pregnancy at or beyond 37 weeks gestation. Gestational age was determined in relation to the estimated date of confinement (EDC) as defined by 280 days from the last menstrual period that was either less than 7 days different from a first trimester ultrasound or 14 days different from a second trimester ultrasound. Otherwise, the EDC from the earliest ultrasound was used.
The primary outcomes examined were the whether the pregnancy proceeded beyond 41 or 42 weeks of gestation. Secondary outcomes included those that have been previously associated with postterm pregnancies including: meconium, postpartum hemorrhage, and chorioamnionitis. Neonatal outcomes of macrosomia (birthweight greater than or equal to 4,000 gms) and Apgar score less than 7 were also examined. Finally, outcomes between pregnancies that had progressed beyond 41 weeks of gestation were compared to those less than 41 weeks of gestation in each ultrasound group to determine whether experiencing an earlier ultrasound had an effect on measured differences in perinatal outcomes.
The data were then compiled and analyzed using STATA v. 7 software (StataCorp – College Station, TX). As the primary predictor of interest was first versus second trimester ultrasound, the dependent variables of interest were first examined in a bivariate fashion. In order to control for potential confounding, outcomes of interest were examined with multivariable logistic regression controlling for maternal age, ethnicity, marital status, Medicaid insurance, education, parity, gestational age at first prenatal visit, and year of delivery. In order to further account for the differences between women who present in the first and second trimester of pregnancy, an analysis was done just of the women who presented for care in the first trimester. Statistical significance was designated by a p-value less than 0.05. This study was approved by the Committee on Human Research at UCSF.
Results
During the study period, there were 7,894 women who delivered at or beyond 37 completed weeks of gestation who had a documented ultrasound at or before 24 weeks gestation. Women who had a first trimester ultrasound, OBUS12, as compared to those with a second trimester ultrasound, OBUS13–24, were more likely to be 35 years or older, college educated, Caucasian race, married, and to have private insurance.(Table 1). They were also less likely to experience a postterm pregnancy beyond 41 or 42 weeks gestation (Table 2). This increased rate of postterm pregnancy seen among those women whose first ultrasound was in the second trimester persisted when controlling for potential confounders with adjusted odds ratios of 1.41 (95% CI 1.22 – 1.61) for 41 weeks gestation and 1.54 (95% CI 1.12 – 2.11) for 42 weeks gestation.
Table 1.
First Versus Second Trimester Ultrasound: Demographics and Characteristics
| First Trimester US (OBUS12) N=2115 | Second Trimester US (OBUS13–24) N=5779 | p-value | |
|---|---|---|---|
| Maternal age >=35 | 25.9% | 15.5% | <0.001 |
| Race/ethnicity | < 0.001 | ||
| African-American | 14.0% | 16.1% | |
| Asian | 25.4% | 28.3% | |
| Caucasian | 46.2% | 37.2% | |
| Latina | 10.1% | 13.6% | |
| Other | 4.4% | 4.9% | |
| Nulliparity | 57.4% | 55.5% | 0.134 |
| Obese | 14.4% | 15.0% | 0.645 |
| Attended College | 64.8% | 57.1% | <0.001 |
| Medicaid Insurance | 32.5% | 46.0% | <0.001 |
| Single Marital Status | 29.6% | 36.0% | <0.001 |
Table 2.
First Versus Second Trimester Ultrasound: Perinatal Outcomes
| First Trimester US (OBUS12)N=2115 | Second Trimester US (OBUS13–24)N=5779 | p-value | |
|---|---|---|---|
| Prolonged Pregnancy | |||
| ≥41 weeks | 18.2% | 22.1% | <0.001 |
| ≥42 weeks | 2.7% | 3.7% | 0.022 |
| Postterm Induction | |||
| ≥42 weeks | 1.8% | 2.6% | 0.017 |
| Meconium | 21.7% | 23.9% | 0.040 |
| Chorioamnionitis | 10.3% | 11.4% | 0.177 |
| Postpartum hemorrhage* | 15.3% | 16.8% | 0.192 |
| Macrosomia** | 10.8% | 12.1% | 0.100 |
| 5 minute Apgar <7 | 2.2% | 2.6% | 0.326 |
Postpartum hemorrhage was defined as an EBL> 500 ml for a vaginal delivery and >1000 ml for a cesarean delivery
Macrosomia was defined as a birthweight of 4,000 gms or greater
Rates of some secondary perinatal outcomes examined were also lower in the women who had first trimester ultrasounds (Table 2). The rate of postterm induction at 42 weeks of gestation was lower (1.8% vs. 2.6%, p=0.017) as was the presence of meconium (21.7% vs. 23.9%). However, there were no differences seen in the rates of chorioamnionitis, postpartum hemorrhage, fetal macrosomia, or five minute Apgar scores less than 7. These findings, both positive and negative, persisted when confounders were controlled with multivariable analyses (Table 3).
Table 3.
First Versus Second Trimester Ultrasound: Multivariable Analysis of Perinatal Outcomes
| Adjusted Odds Ratio* Comparing OBUS12 to OBUS13–24 | 95% Confidence Interval | ||
|---|---|---|---|
| Prolonged Pregnancy | |||
| ≥41 weeks | 1.41 | 1.22 – 1.61 | |
| ≥42 weeks | 1.54 | 1.12 – 2.11 | |
| Postterm Induction | |||
| ≥42 weeks | 1.45 | 1.01 – 2.09 | |
| Meconium | 1.17 | 1.03 – 1.33 | |
| Chorioamnionitis | 0.90 | 0.75 – 1.08 | |
| Postpartum hemorrhage* | 1.09 | 0.88 – 1.37 | |
| Macrosomia** | 1.14 | 0.95 – 1.39 | |
| 5 minute Apgar <7 | 1.03 | 0.73 – 1.51 | |
Multivariable models controlled for maternal age, race/ethnicity, parity, education, obesity, marital status, and Medicaid insurance
When comparing perinatal outcomes between women whose pregnancies persisted beyond 41 weeks of gestation to those who delivered prior to this threshold, the risk of complications was consistently higher in those women beyond 41 weeks of gestation (Table 4). Further, the differences between women before or after 41 weeks of gestation, as measured by the adjusted odds ratio, were consistently higher in those women who had undergone a first trimester ultrasound. In a sensitivity analysis of the data in order to further examine the potential effect that gestational age at first visit may have on the results, we conducted analyses excluding all women who presented for care at 13 weeks and beyond. While we had slightly less power in these analyses, the findings in both sets of multivariable analyses persisted (data not shown).
Table 4.
First Versus Second Trimester Ultrasound: Comparing Outcomes Before and After 41 weeks of Gestation
| First Trimester US (OBUS12) | Second Trimester US (OBUS13–24) | |
|---|---|---|
| Meconium | 3.05 (2.40–3.87) | 2.29 (2.00–2.67) |
| Chorioamnionitis | 1.70 (1.39–2.07) | 1.45 (1.01–2.09) |
| Postpartum hemorrhage* | 1.58 (1.12–2.24) | 1.39 (1.14–1.70) |
| Macrosomia** | 3.46 (2.94–4.08) | 2.63 (1.94–3.54) |
| 5 minute Apgar <7 | 2.20 (1.54–3.14) | 1.54 (0.76–3.15) |
Multivariable models compared outcomes between term pregnancies that delivered before and after 41 weeks of gestation. Models controlled for maternal age, race/ethnicity, parity, education, obesity, marital status, and Medicaid insurance
Comment
When we compared women who had undergone a first versus a second trimester ultrasound, those who had a first trimester ultrasound were less frequently diagnosed with a prolonged pregnancy beyond 41 weeks gestation or postterm pregnancy beyond 42 weeks gestation. Further, these women were less likely to experience a postterm induction of labor. Furthermore, we demonstrated that due to the decrease in misclassification bias in women with a first trimester ultrasound, the differences in perinatal complications is actually higher in these women when comparing pregnancies before and after 41 weeks of gestation.
These findings support a body of literature that suggests that pregnancies which progress beyond their EDC and certainly beyond 41 weeks of gestation are at increased risk for perinatal complications. The evidence for misclassification bias that persists even among pregnancies that undergo a second trimester ultrasound should lead to several changes. First, researchers should be encouraged to conduct studies of perinatal outcomes by gestational age among populations that are well dated or at least to consider dating in such studies by conducting subgroup analyses. Second, clinicians should endeavor to date women’s pregnancies with the use of a first trimester ultrasound, particularly if there is any uncertainty regarding the LMP or a woman has any history of irregular menses or cycles that are not routinely 28 days in length. As more of our patients undergo the nuchal translucency screening test, it remains to be seen whether such ultrasounds, commonly done at 11–13 weeks of gestation, will provide adequate dating and studies comparing such dating to an early first trimester ultrasound should be conducted.
An important practice and policy question remains, whether in women who will not otherwise receive a first trimester ultrasound, the practice of a routine first trimester ultrasound is cost-effective with respect to pregnancy dating. In order to conduct such a study considerations would include the benefits to women of improved dating as well as the cost savings of less antenatal testing and labor inductions in those women who were improperly dated. Such studies may be necessary to encourage insurance companies to provide reimbursement for more than one routine ultrasound in pregnancy similar to the care commonly provided in many European countries.
From the findings that the risk of perinatal complications are likely to be even higher than previously noted in women whose pregnancies progress to 41 weeks gestation and beyond, how should we respond? Considering the findings of a large randomized, control trial and a recent meta-analysis, it appears that induction of labor at 41 weeks gestation as compared to expectant management beyond 41 weeks actually leads to lower rates of cesarean deliveries and perinatal morbidity.11,12 Certainly, at the very least, antenatal testing should be utilized to identify those women whose pregnancies are the highest risk of complication. 13 Prior to 41 weeks of gestation, the number of studies of routine induction of labor are limited and outdated, though they do find a lower risk of cesarean delivery with induction.14 Thus, it is unclear what interventions prior to 41 weeks of gestation are merited.
While our study did verify that first trimester ultrasound dating may lead to less misdiagnosis of postterm pregnancies, it is not without limitations. First, as a nonrandomized study, it is prone to confounding bias, particularly because women receiving a first trimester ultrasound may differ from those who did not. In fact we did identify several potential confounders that differed between the two groups. However, the differences we found persisted even when controlling for these confounders utilizing multivariable analyses. Additionally, our study might be prone to further misclassification bias in the second trimester ultrasound group. While we searched the medical record for evidence of early ultrasound, it may be that some of these women experienced an early ultrasound elsewhere that did not make it into the record at UCSF. However, such misclassification would actually result in a bias towards the null effect, so any difference that we did identify would be larger. Another potential confounder is year of delivery as practice may have changed over time. However, we did not identify obvious changes in the practice of induction of labor during the time period of the study and we controlled for year of delivery in the multivariable analyses.
In spite of these theoretical concerns, we believe that we have demonstrated that first trimester ultrasound dating leads to less misclassification with respect to gestational age. The result of such improved dating is that fewer women are misdiagnosed as having a prolonged gestation. However, it also unmasks larger risks of perinatal complications in such women who do progress to and beyond 41 weeks of gestation. Thus, these findings would suggest that women will benefit from a first trimester ultrasound to confirm or adjust pregnancy dating. Additionally, closer attention to the issue of pregnancies that progress beyond their due date should be paid by both clinicians and researchers in order to reduce the perinatal morbidity and mortality in term and postterm pregnancies. However, before we support the practice of routine induction of labor or antenatal testing at 39 or 40 weeks of gestation, large prospective, randomized, controlled trials of such interventions should be conducted.
Acknowledgments
ABC is supported by the National Institute of Child Health and Human Development, Grant # HD01262 as a Women’s Reproductive Health Research Scholar and by the Robert Wood Johnson Foundation as a Physician Faculty Scholar
Footnotes
This study was presented at the Pacific Coast Obstetrical and Gynecological Society Meeting in Las Vegas, NV in October, 2007
Condensation: Women with first trimester ultrasounds are diagnosed with postterm pregnancies and experience postterm induction less often than those with a second trimester ultrasound.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American College of Obstetricians and Gynecologists. Management of postterm pregnancy, ACOG Practice Bulletin No. 55. Washington, D.C.: ACOG; 2004. [Google Scholar]
- 2.Hauth J, Goodman MT, Gilstrap LC, et al. Post-Term Pregnancy. Obstet Gynecol. 1980;56:467. [PubMed] [Google Scholar]
- 3.Lucas WE, Anctil AO, Callagan DA. The Problem of Postterm Pregnancy. Am J Obstet Gynecol. 1965 Jan 15;91:241–250. doi: 10.1016/0002-9378(65)90207-3. [DOI] [PubMed] [Google Scholar]
- 4.Naeye RL. Causes of perinatal mortality excess in prolonged gestations. Am J Epidemiol. 1978;108:429–433. doi: 10.1093/oxfordjournals.aje.a112641. [DOI] [PubMed] [Google Scholar]
- 5.Caughey AB, Musci TJ. Complications of term pregnancies beyond 37 weeks of gestation. Obstet Gynecol. 2004;103:57–62. doi: 10.1097/01.AOG.0000109216.24211.D4. [DOI] [PubMed] [Google Scholar]
- 6.Nicholson JM, Kellar LC, Kellar GM. The impact of the interaction between increasing gestational age and obstetrical risk on birth outcomes: evidence of a varying optimal time of delivery. J Perinatol. 2006;26:392–402. doi: 10.1038/sj.jp.7211528. [DOI] [PubMed] [Google Scholar]
- 7.Caughey AB, Washington AE, Laros RK. Neonatal complications of term pregnancies: rates increase in a continuous, not threshold fashion. Am J Obstet Gynecol. 2005;192:185–189. doi: 10.1016/j.ajog.2004.06.068. [DOI] [PubMed] [Google Scholar]
- 8.Taipale P, Hilesmaa V. Predicting Delivery Date by Ultrasound and Last Menstrual Period in Early Gestation. Obstet Gynecol. 2001;97:189–194. doi: 10.1016/s0029-7844(00)01131-5. [DOI] [PubMed] [Google Scholar]
- 9.Savitz DA, Terry JW, Jr, Dole N, Thorp JM, Jr, Siega-Riz AM, Herring AH. Comparison of pregnancy dating by last menstrual period, ultrasound scanning, and their combination. Am J Obstet Gynecol. 2002;187:1660–1666. doi: 10.1067/mob.2002.127601. [DOI] [PubMed] [Google Scholar]
- 10.Bennett KA, Crane JM, O’Shea P, Lacelle J, Hutchens D, Copel JA. First trimester ultrasound screening is effective in reducing postterm labor induction rates: a randomized controlled trial. Am J Obstet Gynecol. 2004;190:1077–1081. doi: 10.1016/j.ajog.2003.09.065. [DOI] [PubMed] [Google Scholar]
- 11.Hannah ME, Hannah WJ, Hellmann J, Hewson S, Milner R, Willan A. Induction of labor as compared with serial antenatal monitoring in post-term pregnancy. A randomized controlled trial. The Canadian Multicenter Post-Term Pregnancy Trial Group. N Engl J Med. 1992;326:1587–1592. doi: 10.1056/NEJM199206113262402. [DOI] [PubMed] [Google Scholar]
- 12.Sanchez-Ramos L, Olivier F, Delke I, Kaunitz AM. Labor induction versus expectant management for postterm pregnancies: A systematic review with meta-analysis. Obstet Gynecol. 2003;101:1312–1318. doi: 10.1016/s0029-7844(03)00342-9. [DOI] [PubMed] [Google Scholar]
- 13.Bochner CJ, Williams J, III, Castro L, et al. The efficacy of starting postterm antenatal testing at 41 weeks as compared with 42 weeks of gestational age. Am J Obstet Gynecol. 1988;159:550–554. doi: 10.1016/s0002-9378(88)80005-x. [DOI] [PubMed] [Google Scholar]
- 14.Gülmezoglu AM, Crowther CA, Middleton P. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev. 2006 Oct 18;4:CD004945. doi: 10.1002/14651858.CD004945.pub2. [DOI] [PubMed] [Google Scholar]


