Abstract
Stigma complicates the treatment of HIV worldwide. We examined whether a multi-component framework, initially consisting of enacted, felt normative, and internalized forms of individual stigma experiences, could be used to understand HIV-related stigma in Southern India. In Study 1, qualitative interviews with a convenience sample of 16 people living with HIV revealed instances of all three types of stigma. Experiences of discrimination (enacted stigma) were reported relatively infrequently. Rather, perceptions of high levels of stigma (felt normative stigma) motivated people to avoid disclosing their HIV status. These perceptions often were shaped by stories of discrimination against others HIV-infected individuals, which we adapted as an additional component of our framework (vicarious stigma). Participants also varied in their acceptance of HIV stigma as legitimate (internalized stigma). In Study 2, newly-developed measures of the stigma components were administered in a survey to 229 people living with HIV. Findings suggested that enacted and vicarious stigma influenced felt normative stigma; that enacted, felt normative, and internalized stigma were associated with higher levels of depression; and that the associations of depression with felt normative and internalized forms of stigma were mediated by the use of coping strategies designed to avoid disclosure of one's HIV serostatus.
Keywords: India, HIV, stigma, depression, coping
Stigma complicates the management and treatment of HIV worldwide. It reduces testing-seeking (Ma, Detels, Feng, Wu, Shen, Li et al., 2007; Obermeyer & Osborn, 2007), limits HIV-positive individuals' willingness to disclose their infection (Calin, Green, Hetherton, & Brook, 2007; Tarwireyi, 2005), and affects the attitudes of providers who deliver HIV-related care (Li, Wu, Wu, Zhaoc, Jia, & Yan, 2007; Kurien, Thomas, Ahuja, Patel, Shyla, Wig et al., 2007). As such, understanding stigma's precise nature and effects on behavior is vital in the development of interventions to facilitate health among people living with the disease (Nyblade & MacQuarrie, 2006; Weiss, Ramakrishna, & Somma, 2006).
As used here, stigma refers to the devalued status that society attaches to a condition or attribute. Although it can also refer to the discrediting characteristic itself, stigma is very much about the socially constructed meanings associated with that characteristic. By conveying the devalued status of some identities relative to others, stigma defines social roles within interactions (Crocker, Major, & Steele, 1998; Goffman, 1963; Herek, 2002; Jones, Farina, Hastorf, Markus, Miller & Scott, 1984; Leary & Schreindorfer, 1998). The inferior social status of stigmatized individuals means that they have less power than the non-stigmatized and less access to resources valued by society (Herek, 2008; Link & Phelan, 2001).
Based on these considerations, HIV stigma is socially shared knowledge about the devalued status of people living with HIV. It is manifested in prejudice, discounting, discrediting, and discrimination directed at people perceived to have HIV and the individuals, groups, and communities with which they are associated (Herek, 2002; Herek, Mitnick, Burris, Chesney, Devine, Fullilove et al., 1998; Tewksbury & McGaughey, 1997).
Because the meanings attached to the disease are created through social interactions (e.g., experiencing discrimination or learning of other people being mistreated), the experience of HIV stigma can vary across cultures. For example, whereas stigmatizing attitudes have declined in the United States (Herek, Capitanio & Widaman, 2002), they remain more overt in India (Bharat, Aggleton, & Tyrer, 2001). Prior work documented a variety of discriminatory behaviors toward people living with HIV (PLWH) in India, including denial of hospital care, eviction from homes, and termination of employment (“AIDS stigma forms an insidious barrier”, 2002; Bharat, Aggleton, & Tyrer, 2001; “The Next Wave of HIV/AIDS”, 2002). In rural areas, women widowed by the disease have been rejected by their deceased husbands' families and forced to return to the towns or villages in which they were born (Pallikadavath, Garda, Apte, Freedman, & Stones, 2005). In one instance, an entire village became the target of stigma after one of its bus drivers tested positive for HIV, resulting in villagers being unable to find employment, being dismissed from nearby colleges, and having difficulty arranging marriages (“India's First HIV/AIDS Village”, 2001). HIV stigma has also shaped how PLWH respond to the disease. Recognizing the potentially severe consequences of being identified as having HIV, many PLWH avoid disclosing their serostatus to others (Chandra, Deepthivarma, & Manjula, 2003).
Through prior research on HIV stigma, we developed a preliminary framework for understanding the stigmatizing experiences of PLWH in the developed countries of the West, particularly the United States (Herek, 1990, 2002; Herek & Capitanio, 1999; Herek, Capitanio, & Widaman, 2002; Herek & Glunt, 1988; Herek et al., 1998). To examine the cross-cultural applicability of the framework, we undertook new research examining HIV stigma in India.
A Preliminary Conceptual Framework for Understanding the Experience of HIV Stigma
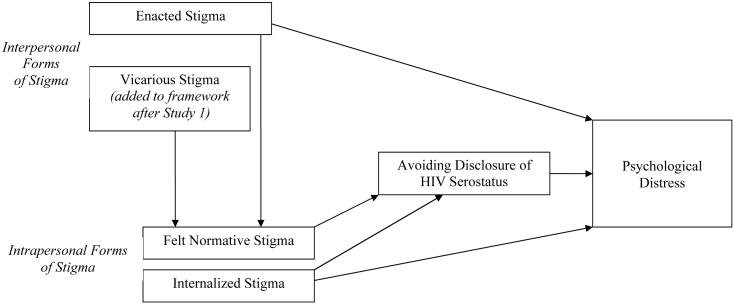
We began with a conceptual framework that builds on Scambler's (1989) hidden distress model. It emphasizes three ways in which individuals experience stigma and considers the importance of stigma management in the social interactions of PLWH (Figure 1). The first component captures interpersonal actions and is labeled enacted stigma. It refers to overt acts of discrimination and hostility directed at a person because of his or her perceived stigmatized status.
Figure 1.
Theoretical Framework Linking Facets of Stigma, Avoidance of HIV Serostatus Disclosure, and Psychological Distress
By contrast, the second and third components are designed to capture intrapersonal experiences of stigma. The second component of our framework, felt normative stigma, refers to the subjective awareness of stigma. Here we operationalized a belief about the prevalence of stigmatizing attitudes among people in the local community, or the degree to which stigma is perceived as normative. These perceptions, in turn, may provide a basis for individual behavior. Felt normative stigma is expected to motivate individuals with a stigmatized condition to take actions to protect against enacted stigma. Such actions can include attempting to pass as a member of the non-stigmatized majority. Successful passing may reduce people's likelihood of experiencing enacted stigma but significantly disrupts their lives and often increases psychological distress (Scambler, 1989).
The extent to which an individual accepts stigma as valid is referred to here as internalized stigma. It constitutes the third component of our framework. When stigma is internalized by members of the non-stigmatized majority, the result is prejudice toward the stigmatized. When it is internalized by stigmatized individuals themselves, the result is self-stigma. In the latter case, people's self-concept is congruent with the stigmatizing responses of others; they accept their discredited status as valid (Herek, 2008; Jones et al., 1984).
Based on research with other stigmatized groups and in other settings, we hypothesized that experiencing each of these components of stigma has important consequences for a stigmatized person's overall well-being. As shown in Figure 1, experiencing enacted stigma is likely to increase PLWH's risk for psychological distress, such as depression (Diaz, Ayala, Bein, Henne, & Marin, 2001; Herek, Gillis, & Cogan, 1999). It also is likely to affect beliefs about the prevalence of stigma (felt normative stigma). Felt normative stigma, in turn, is expected to lead PLWH to monitor and modify their behavior, usually with a goal of trying to avoid future enactments of stigma (Burris, 1997). Based on prior research in India, we specifically expected that the primary behavioral modification would be avoiding disclosure of HIV serostatus (Chandra, Deepthivarma & Manjula, 2003). However, these decisions not to disclose come with consequences. By isolating and depriving themselves of needed resources, PLWH are likely to experience psychological distress (Hays, McKusick, Pollack, Hilliard, Hoff & Coates, 1993). Finally, internalized stigma is hypothesized to be associated with psychological distress both directly and indirectly (because it prevents PLWH from seeking social support and other needed resources) (Simbayi, Kalichman, Strebel, Cloete, Hende & Mqeketo 2007).
We began our research in India by conducting qualitative interviews with a small sample of PLWH, focusing on their perceptions of and experiences with HIV stigma. In Study 2, we used our findings from the interviews to create instruments to measure the different components of our stigma framework, and examined the associations of the stigma components with disclosure-avoidance and psychological distress.
STUDY 1
Method
A convenience sample was recruited in the general medicine department in a large, urban, private hospital in Southern India. Eligible persons were referred by their doctors. Interviewers explained the interview's purpose and procedures, and obtained informed consent. Participants were recruited if they were at least 18 years old; capable of communicating verbally in English or a South Indian language (Kannada, Tamil, Telugu, Malayalam); and had known about their HIV diagnosis for at least six months.
Procedures and Analysis
A one-hour interview was conducted by trained Indian interviewers in a private space in the hospital. Participants were asked to discuss their attitudes about HIV and their awareness of HIV-related discrimination against other people, to identify people to whom they had disclosed their serostatus, and to describe personal experiences of HIV-related discrimination. Interviews were audio-recorded and subsequently translated and transcribed in English. During transcription, personally identifying information was deleted.
All transcribed interviews were read by at least two research team members. One individual coded interviews for themes pertaining to the question of interest (Ryan & Bernard, 2003), namely the kinds of stigma experiences and concerns that participants described in relation to their own or someone else's HIV diagnosis. The coded interviews were entered into ATLAS.ti, a software program to manage narrative data. The second team member verified the identified themes. Disagreements among coders were resolved by consensus.
Results
One respondent who was not responsive to interviewer questions was excluded from the analyses, leaving a sample of 16 (11 men, 5 women). Eleven were married, three separated or divorced, and two widowed. Their ages ranged from 26 to 42.
The interviews provided multiple examples of enacted, felt normative, and internalized stigma. Most participants had experienced some type of enacted stigma when others knew about their HIV infection. Seven individuals reported having their HIV status disclosed without permission. Five received inequitable medical treatment, including denial of care and having hospital staff refuse to touch them for fear of infection. Two were rejected completely by family members, two experienced rejection from friends, one from the community, and one by work colleagues.
Consistent with prior stigma theorizing (Scambler, 1989), respondents in our study made efforts to keep their HIV status secret in the belief that it would help minimize future experiences of enacted stigma. Twelve individuals described specific strategies, included stating or implying that they were being treated for a different disease; refusing to discuss their HIV infection unless asked directly about it; lying outright about their HIV status; seeking treatment far away from home; and not explaining written medical documents to illiterate family members. Ten individuals stated explicitly that they feared negative reactions if they told others that they had HIV. Examples of such sentiments included, “Everybody will poke me; they will look down upon me” and “My wife knows that I had gone to the hospital and taken treatment. I told her not to tell anyone as it [is] a humiliation for us.” This sense of vulnerability resulted in part from stories about stigma against other people with HIV. The events in these stories ranged from relatively undeveloped accounts of social ostracism (a man was refused treatment in a hospital when a physician learned that he had HIV) to very vivid and specific stories. For example, one participant said he had heard about a man who stopped his upcoming wedding upon learning that he was infected. When townspeople discovered the reason for the cancellation, they ridiculed the HIV-infected man until he finally committed suicide.
Although respondents perceived high levels of stigma in their communities (felt normative stigma), they varied in their levels of internalized stigma. When asked specifically to describe their opinions, the majority of individuals said that discrimination again PLWH was inappropriate. However, their explanations suggested that these attitudes were complex. For example, one woman said, “What wrong have I committed? Why has god given me this disease? It is okay if I have committed anything wrong; I [would then] deserve this punishment.” For a male participant, the appropriateness of discrimination was dependent on its form. He felt that isolating PLWH was wrong (“[People in the community] should encourage us to have self-confidence and make us feel like ordinary people”), but that restrictions on marriage were at least partially appropriate (“Let [PLWH] get married. But let them choose their life partner from the infected ones”).
Discussion
The findings from the interviews suggest that the constructs of enacted, felt normative, and internalized stigma are applicable to the experiences of PLWH in India. Although limited in number, participants reported personal experiences of enacted stigma, which were similar to experiences reported in other investigations (Bharat, Aggleton, & Tyrer, 2001). Notably, participants had strong expectations about the prevalence of normative stigma (felt normative stigma), which led them to limit disclosure of their infection. However, their personal views about HIV stigma were more nuanced, often reflecting general disapproval of stigmatizing beliefs but leaving open the possibility that discrimination was sometimes appropriate (internalized stigma).
In addition, the interview responses highlighted how hearing about enactments of stigma represents an important source of perceived norms of stigma. Consistent with social learning theory, which argues that people learn from observing the experiences of others (Bandura, 1979), stories communicated information about the likely consequences of being publicly identified as having HIV and thereby contributed to respondents' perceived need to manage access to information about their health status. Hearing the stories made the possibility of enacted stigma highly salient, even if participants had not personally experienced discrimination. We refer to this channel for transmitting information about enacted stigma as vicarious stigma, and adopted it as a component of our model (Figure 1).
STUDY 2
Based on our findings, we next created instruments to measure the four components of stigma (enacted, vicarious, felt normative, and internalized) in order to test hypothesized associations in our theoretical model (Nyblade & MacQuarrie, 2006). We anticipated that psychological distress (e.g. depression) would be associated with higher levels of enacted, felt normative, and internalized stigma. However, we predicted that the associations between depression and intrapersonal forms of stigma (felt normative, internalized) would be mediated by the use of disclosure-avoidance strategies that limit individuals' access to social support (Hays et al., 1993; Simbayi et al., 2007). Finally, we anticipated that both enacted stigma and the newest framework component, vicarious stigma, would influence perceptions about the prevalence of stigmatizing attitudes in the community (felt normative stigma).
Method
Participants were recruited as part of a larger study of adherence to antiretroviral therapy (ART). All participants were 18 years of age or older, HIV-seropositive, and had taken ART medications for at least one month. Most respondents were referred via the outpatient general medicine department of a large, urban, private hospital in southern India. We intentionally sought to over-represent women (who comprised only 10% of HIV patients at the hospital) to enhance our likelihood of detecting gender differences. A screener in the medical records department flagged the charts of potentially eligible individuals, who were then invited by the clinic charge nurse to meet with a project interviewer while waiting for their appointment. The remaining patients were informed of the study by their physician or by a service provider at local non-governmental agencies (NGO) that served HIV-infected individuals. All referred individuals met privately with a study interviewer, who described the research purpose and obtained informed consent.
Procedures
Participants completed an interviewer-administered, baseline survey on the day of their enrollment into the study. It lasted one hour and assessed a variety of topics, including demographics and health history, HIV stigma, and psychological well-being. Surveys were completed in Kannada, Telugu, Tamil, and English. The instruments were developed in English and then translated into the three Indian languages. All translations were independently back-translated into English to ensure semantic equivalence.
Stigma Assessments
An initial pool of items for the HIV stigma instruments was drawn from anecdotes provided by participants in Study 1, findings from prior work in India (Bharat, Aggleton, & Tyrer, 2001), and, when appropriate, existing measures (e.g., Berger, Ferrans, & Lashley, 2001; Herek, 2006). In order to reduce respondent fatigue and interview time in future research, we intended to use an initial pool of items to identify a smaller set of items to be used in the final version of each scale. The complete sets of items used in all stigma instruments can be found in the appendices (available from the authors on request).
Enacted Stigma
An initial pool of 21 items was assembled to assess if participants had experienced specific discriminatory acts because of their HIV infection. Responses were no (0) or yes (1). Because we expected the incidence of enacted stigma to be fairly low and did not predict that different experiences of enacted stigma would necessarily be correlated, we did not conceptualize our measure of enacted stigma as a scale per se. Rather, it was meant to be an index, capturing the kinds of discriminatory events that people experienced. As such, we initially inspected the outcomes on this measure by looking at the distribution. The 21 enacted stigma items differed widely in terms of the frequency with which they were endorsed, ranging from 0.4% to 26.2% of the sample. We selected 10 items that included both severe and mild enactments and that varied in terms of the frequency of endorsement.
Total scores on the brief and longer versions of the instrument were highly correlated, r (229) = .92, p < .01. Furthermore, the results of all analyses were identical, regardless of which version was used. These findings suggest that the shorter version is representative of the enacted stigma experiences measured by the longer version. The items for this brief version are displayed in Table 2. The appendices display the original pool of items and the frequency with which each item was endorsed by both male and female participants.
Table 2.
Items Selected for Use in the Stigma Assessments
| Enacted Stigma Indexa |
| Has a hospital worker mistreated you because of your HIV |
| Have people looked at you differently because you have HIV? |
| Has a healthcare worker not wanted to touch you because you have HIV? |
| Have you been told not to share your food or utensils with family because of your HIV? |
| Have you been asked not to touch or care for children because of your HIV? |
| Have you been refused medical care or denied hospital services because of your HIV? |
| Have family members forced you to move out of your home because you have HIV? |
| Has a hospital worker made your HIV infection publicly known by marking HIV on your medical record? |
| Has someone threatened to hurt you physically because you have HIV? |
| Have you been refused housing because people suspect you have HIV? |
| Vicarious Stigma (all items begin with the words, “How often have you heard stories about…”)b |
| … a healthcare worker not wanting to touch someone because of his or her HIV? |
| … people being mistreated by hospital workers because of their HIV? |
| … people being refused medical care or denied hospital services because of their HIV? |
| … a healthcare provider talking publicly about a patient with HIV? |
| … someone being refused care from their family when they were sick with HIV? |
| … people being forced by family members to leave their home because they had HIV? |
| … a hospital worker making someone's HIV infection known by marking HIV on their medical records? |
| … families avoiding any relative who has HIV? |
| … people looking differently at those who have HIV? |
| … a village/community ostracizing someone because they had HIV? |
| Felt Normative Stigma Scale (all item begin with the words, “In your community,…”)c |
| … how many mothers would not want someone with HIV to hold their new baby? |
| … how many mothers would not want an HIV-infected person to feed their children? |
| … how many people would not share dishes or glasses someone who has HIV? |
| … how many people think that HIV-infected people have brought shame on their families? |
| … how many people avoid visiting the homes of people with HIV? |
| … how may people think that if you have HIV you have done wrong behaviors? |
| … how many people would not want an HIV-infected person cooking for them? |
| … how many people think that people with HIV should feel guilty about it? |
| … how many people think that a person with HIV is disgusting? |
| … how many people think people with HIV are paying for their karma or sins? |
| Internalized Stigma Scale (all items begin with the words, “How much do you feel…”) d,e |
| … that you should avoid holding a new infant because of your HIV? |
| … that you should avoid feeding children because of your HIV? |
| … that you should avoid sharing dishes or glasses just in case someone might catch HIV from you? |
| … that you have brought shame to your family because you have HIV? |
| … that you should avoid visiting people because of your HIV? |
| … that you have HIV because you have done wrong behaviors? |
| … that you should avoid cooking for people because you have HIV? |
| … guilty about having HIV? |
| … disgusting because of your HIV? |
| … that you are paying for karma or sins because you have HIV? |
Responses were “No” (0) or “Yes (1)
Ratings were made on a 4-point scale ranging from Never (0) to Frequently (3)
Ratings were made on a 4-point scale ranging from No One (0) to Most People (3).
Ratings were made on a 4-point scale ranging from Not At All (0) to A Great Deal (3).
By design, internalized stigma items parallel items in the Felt Normative Stigma Scale.
Vicarious Stigma
An initial pool of 20 items captured the frequency with which participants had heard stories about people being mistreated because of HIV infection. For each item, the participant responded on a 4-point scale that ranged from 0 (never) to 3 (frequently).
Felt Normative Stigma
An initial pool of 15 items assessed participants' perceptions of the prevalence of HIV stigmatizing attitudes. They reported their expectations of how many people in their community would engage in a discriminatory behavior or would endorse a stigmatizing belief. Responses were given on a 4-point scale ranging from 0 (no one) to 3 (most people).
Internalized Stigma
Using parallel versions of the 15 felt normative stigma items, participants reported the extent to which they believed that, as HIV-infected people, they should be treated in a discriminatory manner or be a target of stigmatizing beliefs. Responses were given on a 4-point scale running from 0 (not at all) to 3 (a great deal).
Psychometric reduction of Stigma measures
For vicarious, felt normative, and internalized stigma, we entered items from each scale into an exploratory principal axis factor analysis with an oblique (promax) rotation. Initially, we permitted an analysis to return all factors with eigenvalues above 1.0. We then inspected the scree plot and factor loadings to determine if the full solution was interpretable or if it was advisable to limit the number of factors. As appropriate, we ran subsequent analyses specifying the number of factors to be extracted; 2-factor solutions emerged, with the first factor accounting for most of the explained variance. However, for all three sets of items, the two factors were highly correlated (vicarious: r = .63; felt normative: r = .78; internalized: r = .43), suggesting that, in each case, they were facets of the same stigma construct and could be appropriately combined into a single unidimensional scale. Therefore, for each scale, we selected five of the highest loading items from each of the original factors to create 10-item measures. To ensure equivalence between felt normative and internalized stigma, we selected parallel items. The final 10-item versions of the scales all demonstrated acceptable reliability (Vicarious Stigma Scale: α = .88; Felt Normative Stigma Scale: α = .94; Internalized Stigma Scale: α = .83). Table 2 provides the final set of items in each scale. The appendices display the original multi-factor solutions and the final single factor solutions.
Other Assessments
Disclosure Avoidance
Study 1 findings confirmed our expectation that felt normative stigma motivates many PLWH to limit their disclosure of HIV. Thus, we developed a 14-item measure assessing the use of strategies to avoid revealing that one has HIV. Examples included hiding medications, describing one's illness as tuberculosis, and seeking care away from one's local village. For each item, participants indicated the frequency with which they employed a disclosure-avoidance technique using a 4-point scale ranging from 0 (never) to 3 (often). Scores were derived by averaging responses to the questions (Cronbach's α= .82). The scale's items are provided in the appendices.
Beck Depression Inventory
To assess psychological distress, which we predicted would result from stigma and use of disclosure-avoidance techniques, we included a variant of the Beck Depression Inventory (Version I) (BDI) that had been validated previously in Southern India (Chandra, Gandhi, Satishchandra, Kamat, Desai, Ravi et al., 2006). The scale was available in Kannada. We translated it into Tamil and Telugu, and then translated all Indian language versions into English to ensure semantic equivalence. The Indian version of the BDI uses the same items as found in the United States. However, some wording is modified to reflect local cultural norms or to make statements understandable in Indian languages. The scale had acceptable reliability in our sample (Cronbach's α= .90).
Visibility of HIV Status
We opted to include an additional measure that captured the degree to which a person's HIV status is known to others. This concept is not represented formally in our model (Figure 1) because disclosure avoidance is thought to be potentially harmful regardless of its success at helping a person pass as a member of the nonstigmatized majority (e.g, Scambler, 1989). Nonetheless, in spite of disclosure avoidance, a substantial number of participants in Study 1 reported that their HIV status had been disclosed to others without permission.
In our measure, participants were asked to identify (by name or pseudonym) the people to whom they turned for emotional support and assistance, and to indicate how many of these people knew of their serostatus, regardless of the source. We computed the ratio of the number of people who knew of the person's HIV status to the total number of people she or he listed as sources of support. Scores could range from 0 (none of support network knows of infection) to 1 (100% of support network knows of infection).
Participant demographic and health history characteristics
Individuals were asked to describe their gender, age, marital status, household composition, employment status, monthly income, years of education, religion, and length of time since HIV diagnosis.
Data Analyses
Composite scores for all stigma measures were correlated with psychological and behavioral outcomes. To examine the potential for mediation among our measures, we regressed a presumed mediator onto the respective predictor variable, and the outcome variable onto a predictor variable both when the mediator was included in and excluded from the model (Baron & Kenny, 1986). Analyses were conducted using SPSS 13.0.
Results
The sample consisted of 229 respondents. A majority were male, married, and Hindu (Table 1). Most had obtained 10 or fewer years of education and reported earnings of 3000 or fewer rupees per month, indicative of low socioeconomic status. Participants reported living with a variety of relatives, including spouses (n = 160; 70%), children (n = 161; 70%), parents (n = 81, 35%), siblings (n = 54; 23%), and other extended family (n = 45; 20%). A majority could read Kannada (n = 161; 70%), whereas smaller percentages could read English (n = 110; 48%), Hindi (n = 56; 25%), Telegu (n = 52; 23%), and Tamil (n = 28; 12%). Participants had been diagnosed with HIV for an average of 3.85 years (range: 0.13-17.22 years). Although we do not have information on individuals who refused participation, the age and religious profile of our sample was similar to the profile of all patients in the HIV clinic at the hospital where the study was conducted. The sample's representation of women was higher (31% female vs. 10% female among all HIV patients at the hospital), a reflection of our intentional efforts to oversample females.
Table 1.
Demographic profile of the cohort participants
| Gender | N (%) | Employment Status | N (%) |
| Male | 159 (69.4%) | Not employed | 66 (28.8) |
| Female | 70 (30.6%) | Currently employed | 163 (71.2%) |
| Marital Status | N (%) | Religion | N (%) |
| Married | 175 (76.4%) | Hindu | 202 (88.2%) |
| Never married | 26 (11.4%) | Muslim | 9 (3.9%) |
| Divorced/separated | 2 (0.9%) | Christian | 17 (7.4%) |
| Widowed | 26 (11.4%) | Jain | 1 (0.4%) |
| Education | N (%) | Interview language | N (%) |
| ≤ 9 years | 70 (30.6%) | Kannada | 181 (79.0%) |
| 10 years | 69 (30.1%) | Tamil | 14 (6.1%) |
| Vocational training | 63 (27.5%) | Telugu | 29 (12.7%) |
| At least some college | 27 (11.8%) | English | 5 (2.2%) |
| Age | Income/month (in rupees) | ||
| Mean: 37.6 | Mean: 4510.99 | ||
| Range: 23-74 | Range: 0-22,000 |
Mean Levels of Stigma
Reports of enacted stigma on the 10 item scale were low (M = 0.73, SD = 1.41). Seventy-one percent of participants (n = 163) did not report any instance of discrimination as a result of their HIV status. Vicarious, felt normative, and internalized stigma scores were computed by summing the responses and dividing by the number of items. Scores could range between 0 and 3, with higher scores indicating greater levels of stigma. Participants reported more felt normative stigma (M = 1.19, SD = 1.00) than internalized stigma (M = 0.60, SD = 0.64; Z = 7.63, p < .001) or vicarious stigma (M = 0.82, SD = 0.72; Z = 5.75, p < .001).
There were a limited number of significant correlations between the stigma instruments and demographic characteristics. Women had experienced more vicarious stigma than men: Women: M = 0.99, SD = 0.84; Men: M = 0.75, SD = 0.65; F(1, 227) = 5.33, p < .05, η2 = .02. However men had higher scores than women on internalized stigma: Men: M = 0.65, SD = 0.65; Women: M = 0.47, SD = 0.57; F(1, 227) = 4.30, p < .05, η2 = .02. There were no gender differences for enacted or felt normative stigma. Having been diagnosed with HIV for longer periods of time was correlated with higher scores for vicarious stigma, r (229) = .25, p < .01, but lower scores for internalized stigma, r (229) = −.13, p < .05. And increasing age was negatively associated with vicarious stigma, r (229) = −.20, p < .01.
Association of HIV Stigma with Disclosure, Disclosure Avoidance, and Depression
Table 3 displays correlations among the constructs in our model (Figure 1), i.e., the four stigma instruments and the measures of avoidant coping (M = 0.82, SD = 0.59) and depression (M = 12.69, SD = 11.42). Greater levels of depression were associated with felt normative, internalized, and enacted stigma, but not with vicarious stigma. Furthermore, the use of disclosure avoidance techniques was associated positively with all forms of stigma, as well as with depression. This pattern of associations did not differ by gender, nor were there gender differences in the overall reported levels of disclosure-avoidance and depression.
Table 3.
Correlations Among Stigma Instruments, HIV Serostatus Disclosure Avoidance, and Depression
| Felt | ||||||
|---|---|---|---|---|---|---|
| Enacted | Vicarious | Normative | Internalized | Disclosure | Depression | |
| Stigma | Stigma | Stigma | Stigma | Avoidance | (BDI) | |
| Enacted Stigma | 1.00 | |||||
| Vicarious Stigma | 0.46** | 1.00 | ||||
| Felt Normative Stigma | 0.35** | 0.52** | 1.00 | |||
| Internalized Stigma | 0.07 | −0.02 | 0.30** | 1.00 | ||
| Disclosure Avoidance | 0.16* | 0.14* | 0.29** | 0.33** | 1.00 | |
| Depression (BDI) | 0.19** | 0.05 | 0.19** | 0.49** | 0.29** | 1.00 |
p<.05
p<.01
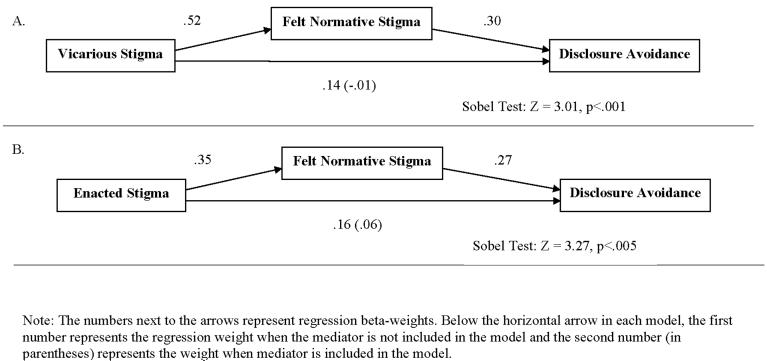
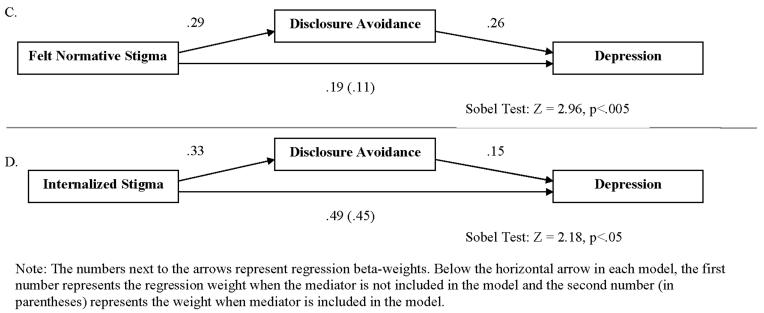
Mediation Among Stigma, Disclosure Avoidance, and Depression
The conceptual model depicted in Figure 1 predicted that several of the observed correlations (specifically, the associations between vicarious stigma and disclosure avoidance, enacted stigma and disclosure avoidance, felt normative stigma and depression, and internalized stigma and depression) would be partially or fully mediated by associations with other variables. To test for the possibility of mediation, we looked to see if the size of the beta-weight for a predictor variable was reduced significantly by including a mediator in a regression model (Baron & Kenny, 1986). Figure 2 diagrams four successful tests of mediation. In each depiction, the beta weights represented along the bottom (horizontal) arrow are critical. The first number is the beta weight of the predictor without the mediator in the model. The second number (in parentheses) is the reduced weight for the predictor with the mediator included in the model. The Sobel test identifies if this reduction in the beta weight size is significant.
Figure 2.
Mediation Analyses Examining Associations Among Stigma, Disclosure Avoidance, and Depression
For the correlation between vicarious stigma and disclosure avoidance, we predicted that the association would be mediated by felt normative stigma. As seen in Figure 2, Cell A, this mediated model was fully supported. The association between vicarious stigma and disclosure avoidance was reduced to near 0 when felt normative stigma was included in the regression. Similarly, as seen in Figure 2, Cell B, felt normative stigma fully mediated the association between enacted stigma and disclosure avoidance, consistent with our predictions in Figure 1. We next examined whether disclosure avoidance mediated the associations between felt normative stigma and depression (Figure 2, Cell C) and between internalized stigma and depression (Figure 2, Cell D). The regression weight for felt normative stigma dropped to non-significant levels when disclosure avoidance was included in the model, suggestive of full mediation as predicted by Figure 1. Similarly, the correlation between internalized stigma and depression was reduced significantly with the inclusion of disclosure avoidance in a regression model. However, internalized stigma still remained a significant unique predictor of depression. This pattern of results suggests that disclosure avoidance only partially mediates the association between internalized stigma and depression, which is consistent with Figure 1.
HIV Serostatus Visibility
Although not formally diagrammed in our model, we included a measure of HIV serostatus visibility (M = 0.44, SD = 0.40; median number of individuals who had knowledge of a participant's serostatus = 4) in order to examine the degree to which disclosure avoidance strategies were successful. Interestingly, there were notable gender differences in the average levels of HIV status visibility (men: M = 0.38, SD = .39; women: M = 0.59, SD = 0.38; F(1, 223) = 13.65, p < .001, η2 = .06) and in how visibility correlated with disclosure avoidance and with stigma. For men, higher serostatus visibility was significantly associated with lower levels of disclosure avoidance, r (158) = −.22, p < .01, but was uncorrelated with reports of enacted, r (158) = .07, p = .33; vicarious r (158) = .05, p = .50; or felt normative stigma, r (158) = .05, p =.46. For women, however, the pattern of results was almost exactly opposite. Greater serostatus visibility was unrelated to disclosure avoidance, r (67) = −.01, p = .95, but was significantly correlated with enacted, r (67) = .24, p = .05 and vicarious stigma, r (67) = .35, p < .01. Furthermore, although the association between serostatus visibility and felt normative stigma was not significant among women, (r (67) = .16, p = .19), the size of correlation was substantially greater than that observed among men and would likely be significant with a larger sample of women. This pattern of results suggests that nondisclosure efforts may be more successful for men than women in hiding HIV infection.
General Discussion
We developed four new instruments to assess different facets of HIV stigma—enacted, vicarious, felt normative, and internalized. All demonstrated good psychometric properties and proved useful in understanding experiences and beliefs in the Indian context. Participants reported very few enactments of stigma. Rather, they were more likely to perceive high levels of HIV stigma in the community (felt normative stigma), and to personally hold mixed views about the validity of this stigma (internalized stigma). Because stigma enactments were low, felt normative stigma was driven most strongly by stories that participant had heard of other PLWH experiencing discrimination. The addition of vicarious stigma to our framework was critical. It helped explain the observed pattern of results by documenting a channel for the communication of HIV information. Participants did not need to encounter actual enactments of stigma to fear its social consequences. Stories communicated norms about HIV and shaped behavior.
Although striking, the low levels of enacted stigma and the relatively higher levels of felt normative stigma are consistent with prior research. Early stigma theories classified scorned conditions into those that create discredited and discreditable identities (Goffman, 1963). The distinction focuses on a condition's visibility. Those that cannot be hidden create discredited identities, in which a person's inferior status is known in all social situations and the individual must develop strategies for coping with the resulting prejudice and discrimination. By contrast, conditions that can be hidden create discreditable identities. In this case, the fundamental challenge becomes the management of stigma information. A person with a discreditable condition tries to control who does and does not know about a scorned condition to minimize the likelihood of being assigned a discredited status.
Our data clearly align with the latter category. Participants experienced low levels of enacted stigma, which is to be expected given that HIV is often not readily apparent (unless a person develops symptoms stereotypically associated with the disease). By contrast, participants were more acutely aware of the potential for stigma and employed strategies such as disclosure avoidance, that they thought would help protect against being discredited (i.e., stigmatized). Unfortunately, these strategies come with a cost. In our second study, greater efforts to limit disclosure of HIV status were associated with higher levels of depression. In addition, disclosure-avoidance techniques did not always accomplish their intended goal. For women specifically, disclosure avoidance had no relationship to the proportion of people in their social networks who knew of their infections. This observation may reflect how gender influences HIV care. Prior research has shown that the consequences of HIV stigma are particularly harsh for women, including rejection from husbands' families and fewer financial resources for managing the disease (Pallikadavath et al., 2005). These consequences may place women at the mercy of extended relatives or public assistance programs, making it more challenging to maintain medical privacy.
By design, our felt normative and internalized stigma instruments paralleled each other. Although responses on these measures were correlated, it was clear that personal endorsements of stigmatizing beliefs were driven only partially by perceptions of stigma in the local community. The finding reinforces the importance of keeping perceptions of stigma levels (felt normative) and endorsement of stigma (internalized) conceptually distinct (Herek, 2008). Furthermore, the consequences of felt normative and internalized stigma are somewhat different. Perception of high levels of stigma was linked to depression exclusively through its influence on disclosure-avoidance behaviors. By contrast, internalized stigma directly correlated with depression, even while also influencing disclosure-avoidance behaviors. Our data do not allow us to understand why some people believe HIV stigma is valid whereas others do not. But, given the strong link with depression, it is clear that a major need for people with high internalized stigma is helping them challenge their negative beliefs about the disease. It also points to the importance of reducing negative stereotyping in popular media, which could reinforce internalized stigmatizing beliefs.
Our findings offer several potential avenues for developing stigma interventions in India. First, the critical mediating role of disclosure-avoidance indicates that programs are needed to help participants disclose their infection. Interestingly, the link between disclosure-avoidance and depression held true for men and women, even though there were gender differences in the effectiveness of the strategies at limiting knowledge of a participant's serostatus. This suggests that it may be the act itself (and not the success of its intended outcome) that makes disclosure avoidance psychologically damaging. Indeed, prior research has shown that disclosure of one's HIV status sometime has direct health benefits (Cole, Kemeny, Fahey, Zack, & Naliboff, 2003; Cole, Kemeny, Taylor, Visscher, & Fahey, 1996; Smyth & Pennebaker, 2001; Strachan, Bennett, Russo, & Roy-Byrne, 2007). Thus, a critical first step may be providing opportunities for disclosure, even if it is to people who do not provide critical forms of social support in daily life.
Establishing opportunities for disclosure and social support—even ones as straightforward as hospital-based social groups or peer counselors—holds significant challenges. First, hospitals that provide HIV care attract patients from large geographical areas. PLWH from rural areas often travel long distances to receive treatment. As such, their access to support services may be limited, particularly if they rely on family for transportation and housing when seeking care. Second, PLWH may not always be able to communicate with one another. In southern India alone, there are four major languages (in addition to English). If people are unwilling to seek services locally, one must implement programs in urban centers where PLWH do not all speak a common language. Fortunately, many Indian NGOs already are tackling these and similar challenges as they develop services for PLWH.
A second area for intervention development is challenging PLWH's own stigmatizing beliefs about the disease. How this is best accomplished remains an area in need of urgent study. Prior research has suggested that accurate knowledge about the disease is a major determinant of attitudes (Ambati, Ambati, & Rao, 1997), highlighting a potential role for education. But there may also be culturally-specific beliefs that complicate education-based strategies. For example, traditional Hindu theology places importance on accepting one's fate. Endorsement of this tenet may make people hesitant to challenge beliefs about the disease.
Third, it is critical to consider how interventions can create structural change. As suggested earlier, many women may not have—by circumstances, family, or finances—the ability to exert agency over how they respond to their own infection. Social support groups and educational programs will have little influence if a person's attitudes, beliefs, and behaviors are driven primarily by environmental constraints. Finally, future study is needed to understand how interventions should address related forms of stigma, such as prejudices against sex workers, migrant laborers, injection drug users, and men who have sex with men. Our current study doesn't allow us to determine to what degree these stigma drive beliefs about HIV, nor how they might modify the kind of interventions needed for PLWH. But it is notable that many of the better-performing items in our felt normative and internalized scales related to morality and shame. This suggests that attitudes about the disease are still driven by judgments about how it is acquired.
Our findings are limited by several aspects of the study design. First, the scales were examined in a cross-sectional assessment, precluding definitive conclusions about causality. We currently are collecting longitudinal data to determine how stigma, disclosure avoidance, and psychological reactions relate over time. Second, our sample consisted of PLWH on antiretroviral treatment. As such, it over-represents individuals in later stages of the disease when immune system impairments may produce more visible symptoms. (That said, it should be noted that the primary symptom of HIV in India is tuberculosis, a condition that also occurs commonly among people uninfected with HIV. Characterizing one's HIV illnesses as being due solely to tuberculosis was one of the more common disclosure-avoidance strategies employed by our participants.) Finally, the findings may be affected by selection bias. It is possible that individuals who experienced very high levels of stigma were unwilling to participate in an HIV-specific study.
Stigma is an important consideration in the response to HIV in India. Interventions and policies are needed to ensure the PLWH have the safety and security to disclose their serostatus and to promote more positive opinions about the disease to ensure psychological well-being among people living with the disease.
Acknowledgments
Funding for this project was provided by the United States National Institute of Mental Health (R01MH067513; PI: M.L. Ekstrand). The authors wish to thank the following people for their assistance in the design of the study and the collection of the data reported in this paper: Charles Allwin, David Huebner, Margery Lazarus, Prem Pais, Shibu Paul, Thomas Osmand, Girija Singh, and Nicolas Sheon.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary Material
References
- AIDS stigma forms an insidious barrier to prevention/care: HIV experts describe problem in India. AIDS Alert. 2002;17:111–113. [PubMed] [Google Scholar]
- Ambati BK, Ambati J, Rao AM. Dynamics of knowledge and attitudes about AIDS among the educated in southern India. AIDS Care. 1997;9:319–30. doi: 10.1080/09540129750125118. [DOI] [PubMed] [Google Scholar]
- Bandura A. The social learning perspective: Mechanism of aggression. In: Toch H, editor. Psychology of crime and criminal justice. Holt, Rinehart & Winston; New York: 1979. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV Stigma Scale. Research in Nursing and Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Bharat S, Aggleton P, Tyrer P. India: HIV and AIDS-related discrimination, stigma and denial. UNAIDS; Geneva: 2001. [Google Scholar]
- Burris S. Driving the epidemic underground? A new look at law and the social risk of HIV testing. AIDS and Public Policy Journal. 1997;12:66–78. [PubMed] [Google Scholar]
- Calin T, Green J, Hetherton J, Brook G. Disclosure of HIV among black African men and women attending a London HIV clinic. AIDS Care. 2007;19:385–391. doi: 10.1080/09540120600971224. [DOI] [PubMed] [Google Scholar]
- Chandra PS, Deepthivarma S, Manjula V. Disclosure of HIV infection in south India: patterns, reasons and reactions. AIDS Care. 2003;15:207–215. doi: 10.1080/0954012031000068353. [DOI] [PubMed] [Google Scholar]
- Chandra PS, Gandhi C, Satishchandra P, Kamat A, Desai A, Ravi V, et al. Quality of life in HIV subtype C infection among asymptomatic subjects and its association with CD4 counts and viral loads--a study from South India. Quality of Life Research. 2006;15:1597–1605. doi: 10.1007/s11136-006-9001-7. [DOI] [PubMed] [Google Scholar]
- Cole SW, Kemeny ME, Fahey JL, Zack JA, Naliboff BD. Psychological risk factors for HIV pathogenesis: Mediation by the autonomic nervous system. Biological Psychiatry. 2003;54:1444–1456. doi: 10.1016/s0006-3223(02)01888-7. [DOI] [PubMed] [Google Scholar]
- Cole SW, Kemeny ME, Taylor SE, Visscher BR, Fahey JL. Accelerated course of human immunodeficiency virus infection in gay men who conceal their homosexual identity. Psychosomatic Medicine. 1996;58:219–231. doi: 10.1097/00006842-199605000-00005. [DOI] [PubMed] [Google Scholar]
- Crocker J, Major B, Steele C. Social stigma. In: Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social psychology. 4th ed. Vol. 2. McGraw-Hill; Boston: 1998. pp. 504–553. [Google Scholar]
- Diaz RM, Ayala G, Bein E, Henne J, Marin BV. The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: Findings from 3 US cities. American Journal of Public Health. 2001;91:927–932. doi: 10.2105/ajph.91.6.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. Prentice-Hall; Englewood Cliffs, NJ: 1963. [Google Scholar]
- Hays RB, McKusick L, Pollack L, Hilliard R, Hoff C, Coates TJ. Disclosing HIV seropositivity to significant others. AIDS. 1993;7:425–431. doi: 10.1097/00002030-199303000-00019. [DOI] [PubMed] [Google Scholar]
- Herek GM. Illness, stigma, and AIDS. In: Costa PT Jr., VandenBos GR, editors. Psychological aspects of serious illness: Chronic conditions, fatal diseases, and clinical care. American Psychological Association; Washington, D. C.: 1990. [Google Scholar]
- Herek GM. Thinking about AIDS and stigma: A psychologist's perspective. Journal of Law, Medicine, and Ethics. 2002;30:594–607. doi: 10.1111/j.1748-720x.2002.tb00428.x. [DOI] [PubMed] [Google Scholar]
- Herek GM. Stigma, coping, and psychological and physical well-being in people with HIV/AIDS. Relationship between stigma and well-being: New factors in coping and change; New Orleans, LA: American Psychological Association; 2006. Paper presented in J. Stone (Chair) [Google Scholar]
- Herek GM. Understanding sexual stigma and sexual prejudice in the United States: A conceptual framework. In: Hope D, editor. Contemporary perspectives on lesbian, gay, & bisexual identities: The 54th Nebraska Symposium on Motivation. Springer; New York: 2008. [Google Scholar]
- Herek GM, Capitanio JP. AIDS stigma and sexual prejudice. American Behavioral Scientist. 1999;42:1130–1147. [Google Scholar]
- Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991-1999. American Journal of Public Health. 2002;92:371–377. doi: 10.2105/ajph.92.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM, Gillis JR, Cogan JC. Psychological sequelae of hate-crime victimization among lesbian, gay, and bisexual adults. Journal of Consulting and Clinical Psychology. 1999;67:945–951. doi: 10.1037//0022-006x.67.6.945. [DOI] [PubMed] [Google Scholar]
- Herek GM, Glunt EK. An epidemic of stigma: Public reactions to AIDS. American Psychologist. 1988;43:886–891. doi: 10.1037//0003-066x.43.11.886. [DOI] [PubMed] [Google Scholar]
- Herek GM, Mitnick L, Burris S, Chesney M, Devine P, Fullilove MT, et al. AIDS and Stigma: A conceptual framework and research agenda. AIDS and Public Policy Journal. 1998;13:36–47. [PubMed] [Google Scholar]
- India's First HIV/AIDS Village . Inter Press Service. 2001. [Google Scholar]
- Jones EE, Farina A, Hastorf AH, Markus H, Miller DT, Scott RA. Social stigma: The psychology of marked relationships. W. H. Freeman; New York: 1984. [Google Scholar]
- Kurien M, Thomas K, Ahuja RC, Patel A, Shyla PR, Wig N, et al. Screening for HIV infection by health professionals in India. National Medical Journal of India. 2007;20:59–66. [PubMed] [Google Scholar]
- Leary MR, Schreindorfer LS. The stigmatization of HIV and AIDS: Rubbing salt in the wound. In: Derlega VJ, Bargee AP, editors. HIV and social interaction. Sage; Thousand Oaks, CA: 1998. pp. 12–29. [Google Scholar]
- Li L, Wu Z, Wu S, Zhaoc Y, Jia M, Yan Z. HIV-related stigma in health care settings: A survey of service providers in China. AIDS Patient Care and STDs. 2007;21:753–762. doi: 10.1089/apc.2006.0219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Annual Review of Sociology. 2001;27:363–385. [Google Scholar]
- Ma W, Detels R, Feng Y, Wu Z, Shen L, Li Y, et al. Acceptance of and barriers to voluntary HIV counselling and testing among adults in Guizhou province, China. AIDS. 2007;21(Suppl 8):S129–S135. doi: 10.1097/01.aids.0000304708.64294.3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyblade L, MacQuarrie K. Can we measure HIV/AIDS-related stigma and discrimination? Current knowledge about quantifying stigma in developing countries. United States Agency for International Development; Washington, DC: 2006. [Google Scholar]
- US National Intelligence Council . The Next Wave of HIV/AIDS: Nigeria, Ethiopia, Russia, India, and China. 2002. [Google Scholar]
- Obermeyer CM, Osborn M. The utilization of testing and counseling for HIV: A review of the social and behavioral evidence. American Journal of Public Health. 2007;97:1762–1774. doi: 10.2105/AJPH.2006.096263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallikadavath S, Garda L, Apte H, Freedman J, Stones RW. HIV/AIDS in rural India: Context and health care needs. Journal of Biosocial Science. 2005;37:641–655. doi: 10.1017/S0021932004006893. [DOI] [PubMed] [Google Scholar]
- Ryan GW, Bernard HR. Techniques to identify themes. Field Methods. 2003;15:85–109. [Google Scholar]
- Scambler G. Epilepsy. Routledge; London: 1989. [Google Scholar]
- Simbayi LC, Kalichman S, Strebel A, Cloete A, Hende N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social Science and Medicine. 2007;64:1823–1831. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth JM, Pennebaker JW. What are the health effects of disclosure? In: Baum A, Revenson TA, Singer JE, editors. Handbook of health psychology. Lawrence Erlbaum; Mahwah, NJ: 2001. [Google Scholar]
- Strachan ED, Bennett WRM, Russo J, Roy-Byrne PP. Disclosure of HIV status and sexual orientation independently predicts increased absolute CD4 cell counts over time for psychiatric patients. Psychosomatic Medicine. 2007;69:74–80. doi: 10.1097/01.psy.0000249900.34885.46. [DOI] [PubMed] [Google Scholar]
- Tarwireyi F. Stigma and discrimination: Coping behaviours of people living with HIV and AIDS in an urban community of Mabvuku and Tafara, Harare, Zimbabwe. Central African Journal of Medicine. 2005;51:71–76. [PubMed] [Google Scholar]
- Tewksbury R, McGaughey D. Stigmatization of persons with HIV disease: Perceptions, management, and consequences of AIDS. Sociological Spectrum. 1997;17:49–70. [Google Scholar]
- Weiss MG, Ramakrishna J, Somma D. Health-related stigma: rethinking concepts and interventions. Psychology, Health, & Medicine. 2006;11:277–287. doi: 10.1080/13548500600595053. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.