Abstract
Objectives
To study mechanisms to explain why single premature atrial complexes (PACs) from the pulmonary veins (PV) may initiate human atrial fibrillation (AF).
Background
Theoretically, single PACs may initiate AF if the rate-response of action potential duration (APD restitution) has slope > 1. However, human left atrial APD restitution and its relationship to AF have not been studied. We hypothesized that APD restitution slope > 1 near PVs explains the initiation of clinical AF.
Methods
We studied 27 patients with paroxysmal and persistent (n=13) AF. We advanced monophasic action potential catheters trans-septally to superior PVs. Restitution was plotted as APD of progressively early PACs against their diastolic interval (DI) from prior beats. Activation time restitution was measured using the time from the pacing artifact to each PAC.
Results
Compared to paroxysmal AF, patients with persistent AF had shorter left atrial APD and ERP (p=0.01). In paroxysmal AF, maximum left atrial APD restitution slope was 1.5±0.4; and 12/13 patients had slope > 1 (p<0.001). In persistent AF, PACs encountered prolonged activation for a wider range of beats than paroxysmal AF (p=0.01), that prolonged DI and flattened APD restitution (slope 0.7±0.2; p<0.001); no patient had APD restitution slope > 1. A single PAC produced AF in 5 patients; in all, APD restitution slope > 1 caused extreme APD oscillations after the PAC, then AF.
Conclusions
In patients with paroxysmal AF, maximum APD restitution slope > 1 near the PVs enables single PACs to initiate AF. However, patients with persistent AF exhibit marked dynamic activation delay near PVs that flattens APD restitution. Studies should determine how regional APD and conduction dynamics contribute to the substrates of persistent AF.
Keywords: Atrial Fibrillation, Human, Action Potential Duration, Conduction Velocity, Electrical Restitution, Monophasic Action Potentials, Electrical Remodeling
Introduction
The mechanisms separating persistent from paroxysmal atrial fibrillation (AF) remain unclear. Paroxysmal AF typically requires premature atrial complexes (PAC) (1) or sustaining mechanisms (2) from pulmonary (PV) and thoracic veins, yet persistent AF often initiates and sustains after isolating such veins (3,4). Two central questions are why PACs from PVs initiate paroxysmal AF, and why they may be less important in persistent AF. Elegant computational studies (5) recently showed that steep rate-related change (restitution) in action potential duration (APD) enable single PACs to initiate AF, yet this hypothesis has not been tested in humans nor compared between paroxysmal and persistent AF.
We hypothesized that APD restitution slope should be > 1 near PVs in patients with AF. Restitution relates APD to the diastolic interval (DI) from the prior beat (6) and, when slope > 1 (“steep”), explains self-amplifying APD oscillations. An early beat shortens DI, yet shortens APD to a greater extent; this further lengthens DI/APD and so on, to cause APD alternans and wavebreak. In animal (7) and human (8) ventricles, this may cause fibrillation. However, there are no data linking this mechanism with AF. Although right atrial APD restitution slope > 1 in AF patients (9), this has not been linked with AF nor studied in left atrium where most triggers arise (10). We have reported APD alternans in the right atrium heralding the disorganization of typical atrial flutter to AF (11), yet it is unclear whether that mechanism explains AF initiated by PV-PACs.
To test our hypothesis, we studied APD restitution and activation delay for PACs near the left atrial PV ostia and high right atrium, where PACs may trigger AF, vis-à-vis AF initiation in 27 patients prior to AF ablation.
Methods
Patient Recruitment
We studied 27 patients (age 63±9 years) referred for AF ablation to the Veterans Affairs Medical Center, San Diego. The study was approved by the joint VA/UCSD Institutional Review Board, and all patients provided written informed consent. Left atrial thrombus was excluded by transesophageal echocardiography in patients with persistent AF.
Catheter placement
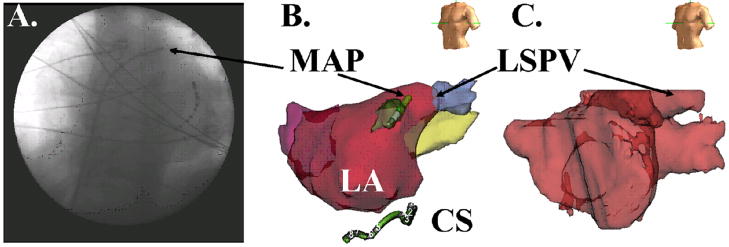
Electrophysiology study was performed in the fasted state, > 5 half-lives after discontinuing anti-arrhythmic medications (> 4 weeks after discontinuing amiodarone; Table 1). A decapolar catheter was placed in the coronary sinus. After trans-septal puncture, LA geometry was digitally reconstructed using NavX (St Jude Medical, Sylmar, CA) referenced to patient-specific computed tomography (figure 1). A deflectable 7F monophasic action potential (MAP) catheter (Boston Scientific, Sunnyvale, CA) was advanced to record AP adjacent to the NavX-verified antrum of the left superior (LSPV, figure 1) or right superior (RSPV) pulmonary veins. APs were recorded at the high right atrium just inferior to the superior vena cava in fourteen patients. Three patients (n=2 persistent) provided only right atrial data.
Table I.
Clinical Characteristics.
| Characteristic | Paroxysmal AF | Persistent AF | P |
|---|---|---|---|
| Numbers (male) | 14 (13) | 13 (13) | 0.81 |
| Age /years | 63±8 | 62±10 | 0.67 |
| Duration of AF / months | 69±144 | 77±69 | 0.87 |
| Left atrial diameter /mm | 40±5 | 48±5 | 0.001 |
| Left ventricular ejection fraction /% | 60±8 | 53±12 | 0.12 |
| Hypertension /% | 8 (57) | 11 (85) | 0.49 |
| Coronary Disease / n (%) | 4 (29) | 2 (17) | 0.92 |
| Diabetes Mellitus /% | 5 (36) | 4 (31) | 0.99 |
| Prior Cardiac Surgery or PCI /% | 5 (36) | 1 (8) | 0.38 |
| Medications | |||
| ACEI/ARB /% | 7 (50) | 7 (54) | 1.00 |
| Statins /% | 9 (64) | 6 (46) | 0.83 |
| Beta-blockers /% | 7 (50) | 10 (77) | 0.55 |
| Class I agents /% | 2 (14) | 1 (8) | 0.96 |
| Amiodarone /% | 1 (8) | 2 (15) | 0.94 |
| Sotalol /% | 3 (21) | 0 | 0.37 |
| Dofetilide /% | 2 (14) | 0 | 0.57 |
Key: PCI, percutaneous coronary intervention
Figure 1.
Left Atrial Monophasic Action Potential (MAP) recording site, in a 74 year old man with persistent AF and LA diameter 48 mm. (A) Fluoroscopy (Left Anterior Oblique 30o) showing MAP catheter within a trans-septal sheath near the left superior PV (LSPV), and the coronary sinus (CS) catheter; (B) Digital Reconstruction of LA confirming MAP catheter in the LSPV antrum (NavX, St Jude Medical, CA). (C) Segmented 64-slice computed tomogram imported into NavX for positional reference.
Pacing Protocol
The protocol was performed before ablation. Patients presenting in AF were electrically cardioverted to sinus rhythm; those who could not complete the protocol with 2 cardioversions were excluded. After ensuring stable MAP catheter positions, the protocol commenced after 18±5 minutes. Pacing was applied at the proximal poles of the MAP catheter at twice diastolic threshold, and APs were recorded from distal poles (12). A drive train of 10 beats at cycle length 500 ms was followed by single PACs coupled at 450 ms, 400 ms, reduced in 20 ms steps to 300 ms, then in 10 ms steps to the effective refractory period (ERP).
MAPs were filtered at 0.05–500 Hz and intracardiac signals between 30–500 Hz. Signals were digitized at 1 kHz to 16-bit resolution and exported from the recorder (Bard Pro, Billerica, MA) for analysis using custom PC software written by SMN in Labview (National Instruments, Austin, TX). Recordings showing excessive baseline wander, artifact or noise were excluded.
Measurement of PAC-Related APD Restitution
We measured APD using validated software (12) (figure 2). AP onset was defined as the calculated maximal upstroke dV/dt. Phase II was defined after the AP peak, and phase IV (diastolic) voltage as the mean of voltages preceding and following the beat. APD at 90 % repolarization (APD90) extends from AP onset to 90% voltage recovery from phase II. Diastolic interval (DI) extends from APD90 of the prior beat to the current AP onset (figure 2C). When an AP was contaminated, e.g. pacing artifact in the last drive beat (figures 3–6), we used mean APD90 of 2 prior beats. Early PACs have negative DI if ERP is shorter than APD90 (12).
Figure 2.
Left Atrial Action Potentials During Constant Pacing (S1) and PACs (S2) in patients with (A) Paroxysmal AF; and (B) Persistent AF. For each PAC, stimulus artifact (“Stim”) and phases 1, 2 and 3 of the AP are labeled. Activation time (AT) spans the time from the stimulus artifact to the computed dV/dt maximum of phase 0 (not labeled), and is 25 ms for A and 50 ms in B. Bipolar atrial electrograms are labeled “A” in the coronary sinus (CS). (C) APD90 measurement, calculated as 90% repolarization from phase II voltage to the baseline.
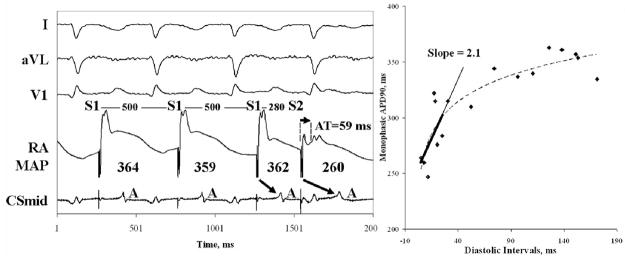
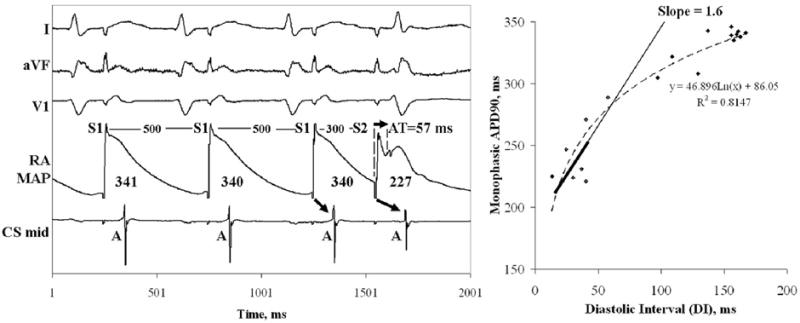
Figure 3. Steep Left Atrial APD Restitution in Paroxysmal AF.
This PAC is delivered just outside the ERP (500/320 ms) and results in DI 6 ms and APD restitution slope = 1.8 (same patient as figure 2A). The thickened line represents the DI range for which slope was calculated.
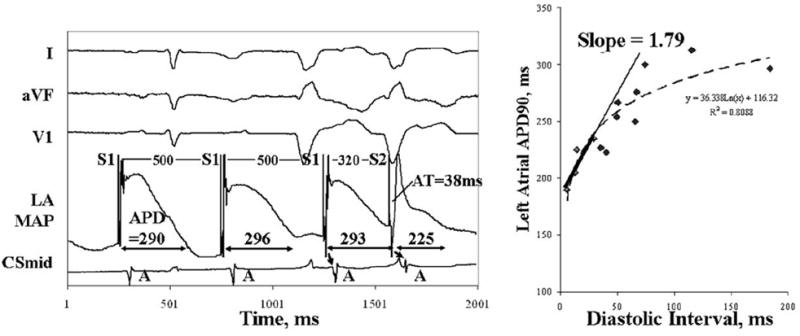
Figure 6. Right Atrial APD restitution has slope > 1 Without AT Prolongation.
In (A) Paroxysmal AF, PACs and APD restitution for a 74 year old man with LA diameter 45 mm and AF for 3 years; (B) Persistent AF, in the same patient as figure 5B. Compared to left atrial data in this patient, ERP (280 ms vs 200 ms) and APD90 (346 ms vs 275 ms) were longer, and AT delay (57 ms vs 106 ms) and minimum DI (13 vs 23 ms) were shorter. See table II.
We constructed standard APD restitution curves from (DI, APD90) pairs. Maximum slope was determined from linear fits of 30-ms DI segments containing data (i.e., from 0 to 30 ms, 10 to 40 ms and so on) without extrapolation as reported (13,14).
Analysis of Activation Time Restitution
We measured activation time (AT) from the pacing stimulus to AP upstroke of each PAC. We used (DI, AT) pairs to plot standard restitution (14) as best-fit straight lines where (a) AT lengthened (at short DI), and (b) flat restitution. We report the longest DI where AT began to prolong (7).
Statistical Analysis
Continuous data are represented as mean ± standard deviation (SD). The two-tailed t-test was used to compare continuous clinical variables. Paired clinical variables were compared using linear regression and the paired t-test. The Mann-Whitney U-test was used to compare repolarization and conduction parameters. The Fisher exact test was applied to contingency tables. An additional 4 patients recruited after phase I of the analysis did not appreciably alter the statistics, that are presented for the entire population. A p-value < 5 % was considered statistically significant.
Results
Clinical characteristics are shown in Table 1. Patients with paroxysmal AF had smaller left atria than those with persistent AF.
I. Left Atrial APD Dynamics in Paroxysmal AF
Left atrial APD restitution had slope > 1 in paroxysmal AF. Figure 3 shows left atrial APs near the RSPV in a 61 year old man with LA diameter 42 mm and paroxysmal AF for 2.5 years. For this PAC just outside ERP, activation time (AT) is short and APD90 is markedly shortened. APD restitution (for all PACs) has maximal slope 1.79.
For patients with paroxysmal AF, maximum left atrial APD restitution slope was 1.5±0.4, and 12/13 had maximum slope > 1. Of these patients, the DI range for which slope > 1 was 27±9 ms. Two patients presented in AF. After cardioversion, maximal left atrial APD restitution slopes were > 1 (1.9 and 1.5) and other parameters were similar to patients presenting in sinus rhythm.
II. Relevance of APD Restitution Slope > 1 to AF Initiation
A single PAC initiated AF in 5 patients with paroxysmal AF, all with maximum restitution slope > 1. In each case, the PAC was followed by marked APD oscillations predicted by APD restitution, then AF (i.e. without rapid automatic firings). Figure 4A shows APs near the left superior PV in a 65 year old gentleman with LA diameter 38 mm and maximum APD restitution slope 1.2. The very early PAC was followed by a pause to the next beat, then a short-coupled beat then AF. In figure 4A, steep APD restitution predicted that this long-short-long sequence would cause extreme APD oscillations (221-139-224-158 ms for S1-S2-F1-F2), then AF (F1-F7) that continued to track APD restitution.
Figure 4. PAC Induces Paroxysmal AF In a Patient with Steep APD Restitution.
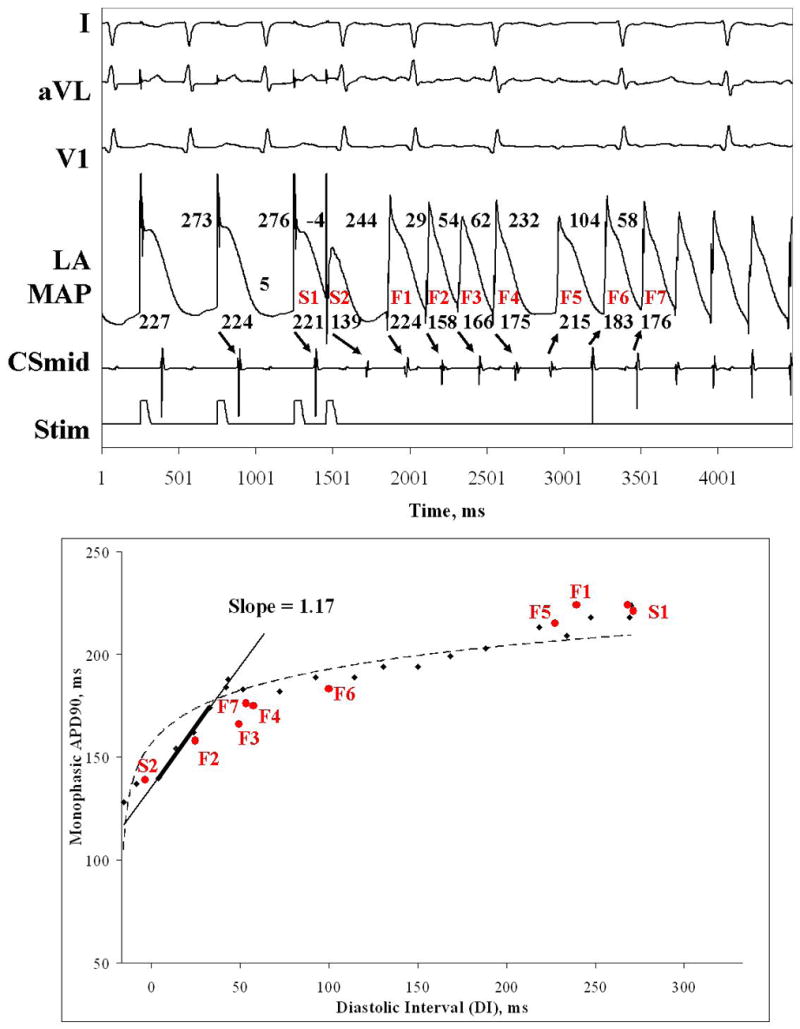
(A) Very early PAC (DI -4 ms) followed by a pause then AF. (B) Steep Restitution May Explain PAC-Induced AF (in red). S1, S2, F1 and F2 show marked APD oscillations, because of steep APD restitution (slope = 1.2; slope > 3 by monoexponential fit), then AF onset. AF cycles continue to track restitution, even though wavelets meander (altered activation sequence after F4).
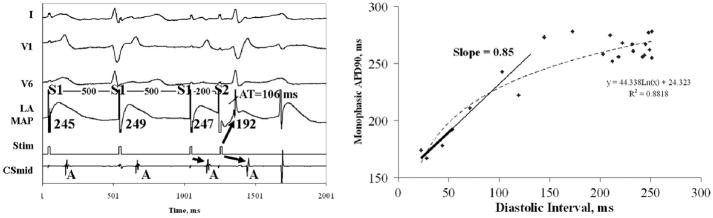
III. Left Atrial APD Dynamics in Persistent AF
Patients with persistent AF had shorter peri-PV baseline APD90 (p<0.001) and shorter ERP (p=0.01) than patients with paroxysmal AF (table II). Maximum APD90 restitution slope, however, was less steep than in patients with paroxysmal AF. Single PACs from the PVs did not induce AF in any patient with persistent AF.
Table II.
Bi-Atrial Repolarization Dynamics
| Characteristic | Paroxysmal AF | Persistent AF | P |
|---|---|---|---|
| Left Atrial, n | 13 | 11 | |
| APD90 (drive train), ms | 295±44 | 237±35 | <0.001 |
| APD90 range, ms | 104±27 | 68±35 | 0.01 |
| Effective Refractory Period (ERP), ms | 242±34 | 204±28 | 0.01 |
| Functional Refractory Period (FRP), ms | 285±39 | 261±25 | 0.06 |
| ERP/FRP, % | 85±7 | 78±8 | <0.05 |
| FRP/APD90, % | 97±6 | 112±14 | <0.001 |
| Maximum APD90 Restitution Slope | 1.5±0.4 | 0.7±0.2 | <0.001 |
| Shortest Diastolic Interval, ms | 5±21 | 20±21 | 0.10 |
| Right Atrial, n | 6 | 8 | |
| APD90 (drive train), ms | 315±36 | 271±33 | 0.01 |
| APD90 range, ms | 124±31 | 121±27** | 0.65 |
| Effective Refractory Period, ms | 252±41 | 224±37 | 0.24 |
| Functional Refractory Period, ms | 282±54 | 264±44 | 0.61 |
| ERP/FRP, % | 90±9 | 85±7+ | 0.25 |
| FRP/APD90, % | 89±12 | 97±10* | 0.24 |
| Maximum APD90 Restitution Slope | 1.3±0.4 | 1.5±0.3† | 0.52 |
| Shortest Diastolic Interval, ms | −5±16 | 2±15* | 0.61 |
Compared to left atrium: + p=0.06;
p<0.05;
p<0.01;
p<0.001.
Figure 5A shows APs near the LSPV in an 82 year old man with LA diameter 44 mm and AF for 5 years. This very early PAC (coupled at 180 ms, versus APD90 ≈230 ms) captured due to marked AT delay (93 ms) that is evident after the pacing artifact (compare against the artifact from the blocked stimulus in the inset). This AT delay prolonged DI (18 ms) to truncate the leftmost portions of APD restitution, giving maximum slope 0.52 (i.e. < 1). Figure 5B shows APs near the RSPV in a 62 year old man with LA diameter 50mm and AF diagnosed 5 years ago. Again, this early PAC (coupled at 200 ms, versus APD90≈250 ms) captures because of AT delay (106 ms) that prolonged DI. Maximal APD restitution slope is 0.45 (i.e. <1).
Figure 5. Left Atrial APD Restitution Is Less Steep in Persistent AF.
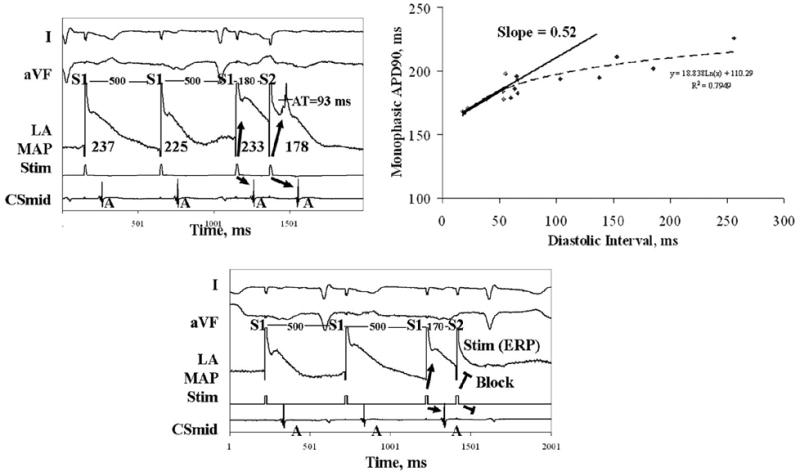
(A) This PAC is early (coupling interval 180 ms), yet significant AT delay (93 ms) enables capture (see blocked stimulus artifact at ERP, 170 ms). This prolongs DI and flattens APD restitution. (B) This early PAC also encounters AT delay (106ms). APD restitution has maximum slope 0.85 (i.e. also not steep; same patient as fig 2B). In both patients, FRP (minimum interval from prior beat to PAC) is longer than ERP (minimum distance between stimuli). See table II.
Such results were typical for patients with persistent AF (table II), in whom maximal APD restitution slope was significantly lower (0.7±0.2) than in paroxysmal AF (p<0.001), and no patient had slope > 1. Accordingly, APD90 range was compressed compared to patients with paroxysmal AF (p=0.01; table II). One persistent AF patient who presented in sinus rhythm had APD restitution slope < 1 (0.64) and similar APD indices to patients presenting in AF (who were cardioverted).
IV. Right Atrial APD Dynamics
Right atrial APD restitution showed maximum slopes > 1 in patients with paroxysmal and persistent AF (table II, figure 6), confirming a previous report (9).
For all patients, right atrial APD restitution slope was 1.4±0.4 (table II) and 13/14 patients had slope > 1 (the exception had persistent AF). In persistent AF patients, APD restitution slope was higher in right than left atrium (1.5±0.3 vs 0.7±0.2; p<0.001; table II).
V. Left Atrial Activation Time and APD Restitution
Because dynamic conduction slowing may alter APD restitution (7), we measured AT restitution in both groups. Left atrial AT prolongation arose more easily (i.e. for later coupled PACs) in persistent than paroxysmal AF. This prolonged DI for early PACs and truncated the steepest portion of APD restitution.
Figure 7A shows left atrial AT restitution for a patient with paroxysmal AF. AT for PACs prolongs only when DI < 21 ms (i.e. very early beats). In contrast, left atrial AT for a patient with persistent AF prolongs for a wide PAC range (DI < 98 ms) causing “broad restitution” (fig. 7B) (7).
Figure 7. Left Atrial Activation Prolongs for a Wider Range of Beats in Persistent than Paroxysmal AF.
In (A) Paroxysmal AF, AT prolongs only at very early DI (<20 ms; i.e. preserved conduction restitution), seen in actual and normalized plots. (B) Persistent AF, AT prolongs at longer DI (< 108 ms; i.e. broad conduction restitution) in both plots. See table III.
Compared to paroxysmal AF, patients with persistent AF showed broader left atrial AT restitution (p=0.01; table III). In persistent AF, the FRP/APD90 ratio was >1 (1.12) because of delay for earliest PACs. Thus, the earliest PV-PAC was separated from the last drive beat (i.e. FRP) by APD90 + 28 ms (12 % of 237 ms). In paroxysmal AF, left atrial FRP/APD90 ratio ≈1 (p<0.01 vs persistent AF; table II).
Table III.
Atrial Conduction Dynamics
| Conduction Parameter | Paroxysmal AF | Persistent AF | P |
|---|---|---|---|
| Left Atrial | |||
| Baseline AT (in drive cycle), ms | 23±11 | 20±7 | 0.84 |
| Maximal AT, ms | 76±35 | 91±28 | 0.17 |
| DI where Prolongation starts, ms | 11±55 | 71±30 | 0.01 |
| Right Atrial | |||
| Baseline AT (in drive cycle), ms | 14±6 | 15±7 | 0.70 |
| Maximal AT, ms | 39±45 | 62±29 | 0.12 |
| DI where Prolongation starts, ms | 14±28 | 18±32 | 0.60 |
The clinically measurable parameter left atrial ERP/FRP was smaller in persistent than paroxysmal AF (p<0.05, table II).
VI. Relationship of Activation Time and APD Indices with Demographic Variables
For all patients, neither the minimum DI at which AT prolonged (p=0.17) nor maximum APD restitution slope (p=0.10) significantly related to LA diameter.
Discussion
This study shows that patients with paroxysmal AF exhibit APD restitution slope > 1 near pulmonary veins. This enables single PACs to cause exaggerated APD oscillations that may lead to wavebreak and AF. Conversely, in patients with persistent AF, early PV-PACs experience markedly prolonged activation time that flattened APD restitution (slope < 1). The initiation of persistent AF may thus reflect broad conduction restitution or mechanisms unrelated to APD oscillations. Notably, differences were more marked in left than right atrium, and may reflect progressive atrial electrical remodeling.
APD Restitution as a Potential Mechanism for Human AF
This is the first human study to link the restitution hypothesis (6,7,15) with AF. In this population, single PACs induced AF in one fifth of patients, all of whom had APD restitution slope > 1 (i.e. paroxysmal AF) enabling marked APD oscillations. Furthermore, because extreme APD oscillations may enable a tachycardia to terminate abruptly (16), APD restitution slope > 1 may also explain why paroxysmal AF is more likely to self-terminate than persistent AF.
This mechanism may contribute to the focal source hypothesis for AF, in which rapid regular regions activate too quickly for the remaining atrium, causing AF via “fibrillatory” conduction (17,18). APD restitution slope > 1 could potentially amplify slight cycle fluctuations to cause APD alternans, wavebreak and AF. We have previously reported that APD alternans heralds the disorganization from atrial flutter to AF (11), although the short pacing sequences in the current protocol prevented an analysis of alternans.
Notably, these data do not explain episodic AF that is, why AF does not follow every early PAC. This may result from sympathovagal activity, that may variably steepen APD restitution, as in canine atria (19), or create pro-arrhythmic APD heterogeneity (20). These data also do not explain initiation of persistent AF. This could be explained by spatial heterogeneity: persistent AF initiates in regions where APD restitution slope is > 1. Spatial factors are likely to be central; for example, Kim et al. reported right atrial APD restitution slope > 1 in AF patients (9), yet very early PACs and rapid pacing (cycle length 180 ms) at these sites did not induce AF.
Dynamic Left Atrial Activation Delay and Mechanisms for Persistent AF
AT prolongation was greater in persistent than paroxysmal AF, and in left compared to right atrium. The magnitude of this delay (≈100 ms) suggests that it represents dynamic conduction slowing, supported by similar delay to distant electrodes (e.g. coronary sinus), rather than intracellular mechanisms that may explain shorter right atrial latency (≈28 ms) in patients with structurally normal atria (21).
In the ventricle, dynamic slowing enables fibrillation even if APD restitution slope < 1 (7,22). In canine atria, conduction slowing from cellular uncoupling increases AF vulnerability independent of cellular electrophysiology (APD dynamics) (23). Speculatively, therefore, broad left atrial conduction restitution in patients with persistent AF may enable rapid tachycardias to cause APD alternans and wavebreak, a mechanism that we suggested in the right atrium in patients in whom typical atrial flutter disorganizes to AF (11). Recent studies confirm left atrial conduction slowing in patients with structural disease (24), although this requires study in patients with AF.
Atrial Remodeling, Dynamic Prolongation of Activation Time and APD Restitution
It is unclear whether observed differences between persistent and paroxysmal AF reflect electrical or structural atrial remodeling. It is tempting to conclude that structural remodeling and fibrosis (25) explain broad left atrial AT restitution in persistent AF. However, the DI for AT prolongation (table III) associated weakly with increased age or left atrial size, and did not differ between groups in the right atrium that typically dilates in tandem with the left atrium.
In the absence of structural remodeling, conduction slowing is an inconsistent feature of electrical remodeling; for example, it is seen in dogs and sheep but not goats (25). Conduction slowing also may not fully explain flattened APD restitution in persistent AF, because minimum DI did not differ significantly from paroxysmal AF. Thus, electrical remodeling may explain these observations. In canine atria, electrical remodeling causes greater IKr current in left than right atrium, that compresses APD range and shortens ERP (26). Future studies must therefore examine atrial cellular electrophysiology in patients with persistent and paroxysmal AF (27).
Clinical Implications
APD restitution slope > 1 provides a mechanistic rationale to isolate PVs and other trigger sites (10). On the other hand, APD restitution slope < 1 and substantial AT delay suggest a reduced dependence on triggers, and the need for additional ablation even in patients labeled paroxysmal AF. Clinically, this may be revealed by a shorter ERP/FRP ratio (table II). Trials should study whether conduction slowing adds to dominant frequency or fractionation mapping (10) in guiding ablation.
Limitations
One major limitation is lack of spatial sampling. Because of the challenges of recording stable MAPs for prolonged periods, particularly in left atrium, we studied APD restitution near putative trigger sources, i.e. the superior PVs and superior vena cava. Future work should study if persistent AF patients show APD restitution slope>1 remote from PVs or exaggerated APD dispersion. We recorded right atrial MAPs only in a patient subset, yet our findings of APD restitution slope > 1 without marked AT delay in either group agrees with a prior report (9). Second, we have no control group, yet comparing APD restitution to induced AF in controls (i.e. without clinical AF) would be of unclear significance. Third, it is possible that APD restitution may be flattened in persistent AF patients who were more likely to present in AF than paroxysmal AF patients. However, paroxysmal AF patients presenting in AF still had APD restitution slope > 1, while the persistent AF patient presenting in sinus rhythm had APD restitution slope < 1, somewhat reducing this concern. In addition, persistent AF patients showed right atrial APD restitution slope > 1 despite longstanding AF (likely with right atrial remodeling). To minimize the impact of cardioversion, we waited > 15 minutes as in prior reports (12). Fourth, these data may not apply to patients who could not remain in sinus rhythm long enough to complete this protocol. Fifth, although MAPs could theoretically be influenced by movement, we feel that this is unlikely given the consistency of MAP morphology before and after PACs (e.g. fig 5B). Sixth, higher spatial resolution is needed to determine if AT delay reflects conduction restitution or intracellular mechanisms (e.g. reduced excitability). Although AT delay also occurred to the coronary sinus (figs. 2–6), we did not quantify this because activation paths likely vary with PAC prematurity over this distance. In addition, our sample is too small to study whether APD or activation slowing predict the response to AF ablation. Finally, our study lacked women, reflecting our Veterans’ Affairs patient population. Although sex differences in AF are not clear, studies in both genders are required.
Conclusions
Human left atrial APD restitution has slope > 1 near the pulmonary veins in patients with paroxymal AF. Through this mechanism, early PACs may cause exaggerated APD oscillations to initiate AF. In patients with persistent AF, PACs encounter prolonged activation times and flattened APD restitution. The initiation of persistent AF may thus reflect broad conduction restitution or mechanisms unrelated to APD oscillations. Therapeutically, steep APD restitution provides a mechanistic rationale to isolate triggers, while further studies should define how regional conduction slowing may impact the substrates for persistent AF and approaches to ablation.
Acknowledgments
Supported by grants to SMN from the National Institutes of Health (HL70529, HL83359) and the Doris Duke Charitable Foundation, and to DEK by an ACC-Merck Fellowship.
We are indebted to Kathleen Mills, BA for coordinating this study and to Elizabeth Greer, RN, Stephanie Yoakum, RNP and Stanley Keys, RCVT for helping with clinical data collection.
List of Abbreviations
- AP
Action Potential
- APD
Action Potential Duration
- AT
Activation Time
- DI
Diastolic Interval
- ERP
Effective Refractory Period
- FRP
Functional Refractory Period
- LA
Left Atrium
- LSPV
Left superior pulmonary vein
- PV
Pulmonary Vein
- RSPV
Right Superior Pulmonary Vein
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Haissaguerre M, Jais P, Shah DC, et al. Spontaneous Initiation of Atrial Fibrillation by Ectopic Beats Originating in the Pulmonary Veins. N Engl J Med. 1998;339:659–666. doi: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 2.Haissaguerre M, Sanders P, Hocini M, et al. Changes in Atrial Fibrillation Cycle Length and Inducibility During Catheter Ablation and Their Relation to Outcome. Circulation. 2004;109:3007–3013. doi: 10.1161/01.CIR.0000130645.95357.97. [DOI] [PubMed] [Google Scholar]
- 3.Gerstenfeld EP, Sauer W, Callans DJ, et al. Predictors of success after selective pulmonary vein isolation of arrhythmogenic pulmonary veins for treatment of atrial fibrillation. Heart Rhythm. 2006;3:165–170. doi: 10.1016/j.hrthm.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 4.Haissaguerre M, Sanders P, Hocini M, et al. Catheter Ablation of Long-Lasting Persistent Atrial Fibrillation: Critical Structures for Termination. Journal of Cardiovascular Electrophysiology. 2005a;16:1125–1137. doi: 10.1111/j.1540-8167.2005.00307.x. [DOI] [PubMed] [Google Scholar]
- 5.Gong Y, Xie F, Stein K, et al. Mechanism underlying initiation of paroxysmal atrial flutter/atrial fibrillation by ectopic foci: a simulation study. Circulation. 2007;115:2094–102. doi: 10.1161/CIRCULATIONAHA.106.656504. [DOI] [PubMed] [Google Scholar]
- 6.Franz MR. The electrical restitution curve revisited: steep or flat slope--which is better? J Cardiovasc Electrophysiol. 2003;14:S140–7. doi: 10.1046/j.1540.8167.90303.x. [DOI] [PubMed] [Google Scholar]
- 7.Weiss JN, Karma A, Shiferaw Y, Chen P-S, Garfinkel A, Qu Z. From Pulsus to Pulseless: The Saga of Cardiac Alternans (Review) Circ Res. 2006;98:1244. doi: 10.1161/01.RES.0000224540.97431.f0. [DOI] [PubMed] [Google Scholar]
- 8.Koller ML, Maier SKG, Gelzer AR, Bauer WR, Meesmann M, Gilmour RF., Jr Altered Dynamics of Action Potential Restitution and Alternans in Humans With Structural Heart Disease. Circulation. 2005;112:1542–1548. doi: 10.1161/CIRCULATIONAHA.104.502831. [DOI] [PubMed] [Google Scholar]
- 9.Kim B-S, Kim Y-H, Hwang G-S, et al. Action potential duration restitution kinetics in human atrial fibrillation. J Am Coll Cardiol. 2002;39:1329–1336. doi: 10.1016/s0735-1097(02)01760-6. [DOI] [PubMed] [Google Scholar]
- 10.Calkins H, Brugada J, Packer D, et al. HRS/EHRA/ECAS expert Consensus Statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on catheter and surgical ablation of atrial fibrillation. European Heart Rhythm Association (EHRA); European Cardiac Arrhythmia Scoiety (ECAS); American College of Cardiology (ACC); American Heart Association (AHA); Society of Thoracic Surgeons (STS) Heart Rhythm. 2007;4:816–61. doi: 10.1016/j.hrthm.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 11.Narayan SM, Bode F, Karasik PL, Franz MR. Alternans Of Atrial Action Potentials As A Precursor Of Atrial Fibrillation. Circulation. 2002b;106:1968–1973. doi: 10.1161/01.cir.0000037062.35762.b4. [DOI] [PubMed] [Google Scholar]
- 12.Franz MR, Karasik PL, Li C, Moubarak J, Chavez M. Electrical Remodeling of the Human Atrium: Similar Effects in Patients with Chronic Atrial Fibrillation and Atrial Flutter. J Am Coll Cardiol. 1997;30:1785–1792. doi: 10.1016/s0735-1097(97)00385-9. [DOI] [PubMed] [Google Scholar]
- 13.Yue AM, Franz MR, Roberts PR, Morgan JM. Global Endocardial Electrical Restitution in Human Right and Left Ventricles Determined by Noncontact Mapping. J Am Coll Cardiol. 2005a;46:1067–1075. doi: 10.1016/j.jacc.2005.05.074. [DOI] [PubMed] [Google Scholar]
- 14.Narayan SM, Franz MR, Kim J, Lalani G, Sastry A. T-wave Alternans, Restitution of Ventricular Action Potential Duration and Outcome. J Am Coll Cardiol. 2007f;50:2385–2392. doi: 10.1016/j.jacc.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 15.Walker ML, Rosenbaum DS. Cellular alternans as mechanism of cardiac arrhythmogenesis. Heart Rhythm. 2005;2:1383–1386. doi: 10.1016/j.hrthm.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 16.Frame LH, Simson MB. Oscillations of Conduction, Action Potential Duration and refractoriness. A mechanism for spontaneous termination of re-entrant tachycardias. Circulation. 1988;78:1277–1287. doi: 10.1161/01.cir.78.5.1277. [DOI] [PubMed] [Google Scholar]
- 17.Skanes AC, Mandapati R, Berenfeld O, Davidenko JM, Jalife J. Spatiotemporal Periodicity During Atrial Fibrillation in the Isolated Sheep Heart. Circulation. 1998;98:1236–1248. doi: 10.1161/01.cir.98.12.1236. [DOI] [PubMed] [Google Scholar]
- 18.Waldo AL, Feld GK. Inter-relationships of atrial fibrillation and atrial flutter mechanisms and clinical implications. J Am Coll Cardiol. 2008;51:779–86. doi: 10.1016/j.jacc.2007.08.066. [DOI] [PubMed] [Google Scholar]
- 19.Patterson E, Lazzara R, Szabo B, et al. Sodium-calcium exchange initiated by the Ca2+ transient: an arrhythmia trigger within pulmonary veins. J Am Coll Cardiol. 2006;47:1196–206. doi: 10.1016/j.jacc.2005.12.023. [DOI] [PubMed] [Google Scholar]
- 20.Miyauchi Y, Zhou S, Okuyama Y, et al. Altered atrial electrical restitution and heterogeneous sympathetic hyperinnervation in hearts with chronic left ventricular myocardial infarction: implications for atrial fibrillation. Circulation. 2003;108:360–6. doi: 10.1161/01.CIR.0000080327.32573.7C. [DOI] [PubMed] [Google Scholar]
- 21.Koller B, Karasik PL, Solomon AJ, Franz MR. Prolongation of conduction time during premature stimulation in the human atrium is primarily caused by local stimulus response latency. Eur H J. 1995;16:1920–1924. doi: 10.1093/oxfordjournals.eurheartj.a060848. [DOI] [PubMed] [Google Scholar]
- 22.Banville I, Gray RA. Effect of Action Potential Duration and Conduction Velocity Restitution and Their Spatial Dispersion on Alternans and the Stability of Arrhythmias. J Cardiovasc Electrophysiol. 2002;13:1141 – 1149. doi: 10.1046/j.1540-8167.2002.01141.x. [DOI] [PubMed] [Google Scholar]
- 23.Ohara T, Qu Z, Lee MH, et al. Increased vulnerability to inducible atrial fibrillation caused by partial cellular uncoupling with heptanol. Am J Physiol Heart Circ Physiol. 2002;283:H1116–22. doi: 10.1152/ajpheart.00927.2001. [DOI] [PubMed] [Google Scholar]
- 24.Roberts-Thomson KC, Stevenson IH, Kistler PM, et al. Anatomically determined functional conduction delay in the posterior left atrium relationship to structural heart disease. J Am Coll Cardiol. 2008;51:856–62. doi: 10.1016/j.jacc.2007.11.037. [DOI] [PubMed] [Google Scholar]
- 25.Allessie MA, Ausma J, Schotten U. Electrical, Contractile and Structural Remodeling during Atrial Fibrillation. Cardiovasc Res. 2002;54:230–246. doi: 10.1016/s0008-6363(02)00258-4. [DOI] [PubMed] [Google Scholar]
- 26.Li D, Zhang L, Kneller J, Nattel S. Potential Ionic Mechanism for Repolarization Differences Between Canine Right and Left Atrium. Circ Res. 2001;88:1168–1175. doi: 10.1161/hh1101.091266. [DOI] [PubMed] [Google Scholar]
- 27.Workman AJ, Kane KA, Rankin AC. Characterisation of the Na, K pump current in atrial cells from patients with and without chronic atrial fibrillation. Cardiovasc Res. 2003;59:593–602. doi: 10.1016/s0008-6363(03)00466-8. [DOI] [PubMed] [Google Scholar]