Abstract
Cholangiocarcinomas are cancers that have poor prognosis and limited treatment options. The noncanonical Wnt pathway is mediated predominantly by Wnt 5a, which activates a Ca2+-dependent pathway involving protein kinase C, or a Ca2+-independent pathway involving the orphan receptor Ror2 and subsequent activation of Jun NH2-terminal kinase (JNK). This pathway is associated with growth-suppressing effects in numerous cell types. We have shown that anandamide decreases cholangiocarcinoma growth in vitro. Therefore, we determined the effects of anandamide on cholangiocarcinoma tumor growth in vivo using a xenograft model and evaluated the effects of anandamide on the noncanonical Wnt signaling pathways. Chronic administration of anandamide decreased tumor growth and was associated with increased Wnt 5a expression in vitro and in vivo. Treatment of cholangiocarcinoma cells with recombinant Wnt 5a decreased cell proliferation in vitro. Neither anandamide nor Wnt 5a affected intracellular calcium release, but both increased the JNK phosphorylation. Stable knockdown of Wnt 5a or Ror2 expression in cholangiocarcinoma cells abolished the effects of anandamide on cell proliferation and JNK activation. Modulation of the endocannabinoid system may be important in cholangiocarcinoma treatment. The antiproliferative actions of the noncanonical Wnt signaling pathway warrants further investigation to dissect the mechanism by which this may occur.
Keywords: biliary tract cancer, receptor tyrosine kinase orphan receptor 2, Jun NH2-terminal kinase
cholangiocarcinomas are devastating cancers of intrahepatic and extrahepatic origin that are increasing in both their worldwide incidence and mortality rate (2, 40). The challenges posed by these often lethal biliary tract cancers are daunting, with conventional treatment options being limited and the only hope for long-term survival being that of complete surgical resection of the tumor (2, 40). Conventional chemotherapy and radiation therapy are not effective in prolonging long-term survival (2); therefore, it is important to understand the cellular mechanisms of cholangiocarcinoma cell growth with a view to develop novel chemopreventive strategies.
Marijuana and its derivatives have been used in medicine for many centuries, and, presently, there is an emerging renaissance in the study of the therapeutic effects of cannabinoids. Ongoing research is determining that regulation of the endocannabinoid system may be effective in the treatment of pain (6, 29), glaucoma (48), and neurodegenerative disorders such as Parkinson's disease (33) and multiple sclerosis (3). In addition, cannabinoids might be effective antitumoral agents because of their ability to inhibit the growth of various types of cancer cell lines in culture (9, 35–37) and in laboratory animals (16). Indeed, we have recently demonstrated that the endocannabinoid anandamide (AEA) has antiproliferative effects on cholangiocarcinoma cell lines in vitro via a cannabinoid receptor-independent pathway involving the stabilization of lipid raft-membrane structures and the recruitment of death-receptor complexes into the lipid rafts (11). Conversely, we have also shown that disruption of lipid raft integrity by the endocannabinoid 2-arachidonoyl glycerol leads to increased cholangiocarcinoma cell proliferation (11). The downstream mechanisms of the antiproliferative effects of AEA on cholangiocarcinoma are unknown.
Wnt signaling proteins are known to exert an effect on a wide variety of developmental and pathological processes (42). They can be divided further into two subclasses: the canonical pathway (Wnt/β-catenin pathway) and the noncanonical pathway (Wnt/Ca2+ or Wnt/JNK pathway) (21). The canonical Wnt signaling pathway involves the inhibition of glycogen synthase kinase-3β and subsequent accumulation and nuclear translocation of β-catenin into the nucleus (30). This pathway is thought to be overactive in various cancers (15). However, the noncanonical pathway, including Wnt 5a, is more complex. Activation of this pathway is thought to trigger the intracytoplasmic release of Ca2+ and the activation of subsequent Ca2+-related signaling (41). Alternatively, Wnt 5a can interact with the receptor tyrosine kinase orphan receptor Ror2 to activate a JNK-mediated pathway (38). The consequences of noncanonical Wnt signaling activation on cell proliferation are unclear. On the one hand, Wnt 5a has tumor-suppressive properties in acute lymphoblastic leukemia (34) and thyroid carcinoma (24). Conversely, Wnt 5a has also been shown to increase endothelial cell proliferation and migration (8).
To date, the effects of the noncanonical Wnt signaling pathway on cholangiocarcinoma growth have not been studied; however, Ca2+ signaling has been shown to have opposing effects on cholangiocyte cell growth (17, 18). Vascular endothelial growth factor (VEGF), for example, stimulates the growth of normal cholangiocytes by activation of the inositol triphosphate (IP3)/Ca2+ signaling pathway with subsequent phosphorylation of Src and ERK1/2 (17), and the hormone gastrin has been shown to inhibit cholangiocyte hyperplasia by activation of the IP3/Ca2+/PKC signaling pathway (18). A role of calcium signaling in the control of neoplastic growth has also been established (1, 12, 22). Increased cytosolic Ca2+ may be responsible for the decrease in cholangiocarcinoma growth observed after administration of tauroursodeoxycholate (1), gastrin (22), and γ-aminobutyric acid (12). The effects of Ror2 activation on cholangiocyte and cholangiocarcinoma cell growth, however, are unknown.
The aims of this study were 1) to demonstrate the antiproliferative effects of anandamide in an in vivo xenograft model of cholangiocarcinoma, 2) to determine the effects of anandamide on the noncanonical Wnt signaling pathway and to identify downstream effectors of this pathway, and 3) to evaluate the role of Wnt signaling on cholangiocarcinoma cell growth.
MATERIALS AND METHODS
Materials.
All reagents were purchased from Sigma Chemical (St Louis, MO) unless otherwise stated. AEA was purchased from Tocris Bioscience (Ellisville, MO), and the recombinant Wnt 5a was purchased from R & D Systems (Minneapolis, MN). All primers for real-time PCR and shRNA plasmids were purchased from SuperArray (Frederick, MD). Antibodies directed against Wnt 5a, VEGF-A, VEGF-C, VEGF-R2, and VEGF-R3 were purchased from Santa Cruz Biotechnology (Santa Cruz, CA). Specific antibodies against phospho JNK and total JNK were purchased from Cell Signaling Technology (Danvers, MA). The inhibitor for JNK (SP 600125) and the calcium chelator BAPTA/AM were purchased from Calbiochem (Gibbstown, NJ).
Nude mice studies.
All animal experiments were performed in accordance with a protocol approved by the Scott and White Institutional Animal Care and Use Committee and as described previously (12). Male Balb/c 8-wk-old nude (nu/nu) mice were kept in a temperature-controlled environment (20–22°C) with a 12-h/light-dark cycle and with free access to drinking water and standard mouse chow. Mz-ChA-1 cells (5 × 106) were suspended in 0.25 ml of extracellular matrix gel and injected subcutaneously into the back flanks of these animals. After the establishment of tumors, mice received AEA [10 mg/kg ip per day (10, 20, 43, 47) dissolved in 1:4 Tocrisolve: 0.9% NaCl] or vehicle injected three times per week. Tumor parameters were measured twice a week by an electronic caliper, and volume was determined as tumor volume (mm3) = 0.5 × [length (mm) × width (mm) × height (mm)]. After ∼2 mo, mice were anaesthetized with pentobarbital sodium (50 mg/kg ip) and euthanized according to institutional guidelines. Heart, liver, and kidneys were isolated, fixed in formalin, embedded in paraffin, processed for histopathology, and stained with hematoxylin and eosin for the detection of tissue damage. Statistical significance of tumor volumes was assessed using a two-way ANOVA followed by a Bonferroni post hoc analysis.
Histological assessment of tumors.
Small tumor fragments were fixed in 10% buffered formalin for 2 to 4 h and embedded in low-temperature fusion paraffin (55–57°C), and 3- to 4-μm sections were stained with hematoxylin and eosin and Masson's trichrome stains. For immunohistochemistry, sections were mounted on glass slides coated with 0.1% poly-l-lysine. After deparaffination, endogenous peroxidase activity was blocked by a 20-min incubation in methanolic hydrogen peroxide (2.5%). Endogenous biotin was blocked by the Biotin Blocking System (code X0590; DAKO, Copenhagen, Denmark) according to the instructions supplied by the vendor. Sections were hydrated in graded alcohol and rinsed in PBS (pH 7.4) before applying the primary antibody. Sections were incubated overnight at 4°C with antibodies for cytokeratin-7 (sc-23876), PCNA (sc-56), VEGF-A (sc-152), VEGF-C (sc-9047), VEGF-R2 (sc-6251), and VEGF-R3 (sc-321). Samples were then rinsed with PBS for 5 min, incubated for 20 min at room temperature with secondary biotinylated antibody (DAKO LSAB Plus System; HRP, Milan, Italy), incubated with DAKO ABC (DAKO LSAB Plus System), and finally developed with 3–3′diaminobenzidine. For the detection of apoptosis on the single cell, the terminal deoxynucleotide transferase end labeling (TUNEL) method (ApopTag; Oncor, Gaithersburg, MD) was used. For all immunoreactions, negative controls (the primary antibody was replaced with normal serum from the same species) were also included.
Light microscopy and immunohistochemistry observation were taken by BX-51 light microscopy (Olympus, Tokyo, Japan) with a video cam (Spot Insight; Diagnostic Instrument, Sterling Heights, MI) and processed with an image analysis system (Delta Sistemi, Rome, Italy). Light microscopy and immunohistochemical observations were independently performed by three pathologists in a blinded manner.
The numbers of PCNA, cytokeratin-7, VEGF-A, VEGF-C, VEGF-R2, VEGF-R3, and TUNEL-positive tumor cells were assessed in six slides for each group. Positive cells were counted in six nonoverlapping fields (magnification ×20) for each slide and the data expressed as percentage of positive cells.
The degree of fibrosis was evaluated in six randomly nonoverlapping fields (magnification ×20) for each slide using light microscopy of Masson's-stained sections as previously described (7).
Cell culture.
All in vitro experiments were performed in Mz-ChA-1 cells, which is a human cholangiocarcinoma cell line derived from gallbladder (23). These cells were a kind gift from Dr. G. Fitz (University of Texas Southwestern Medical Center, Dallas, TX) and cultured as previously described (11, 12).
Real-time PCR.
RNA was extracted from Mz-ChA-1 cells after treatment with AEA (10−5 M), for various time points and from tumor tissue treated chronically with AEA or vehicle, using the RNeasy Mini Kit (Qiagen, Valencia, CA) according to the instructions provided by the vendor and reverse transcribed using the Reaction Ready First Strand cDNA synthesis kit (SuperArray). These reactions were used as templates for the PCR assays using a SYBR Green PCR master mix (SuperArray) in the real-time thermal cycler (Mx5000P; Agilent Technologies, Santa Clara, CA) using commercially available primers designed against human Wnt 5a, VEGF-A, VEGF-C, VEGF-R2, VEGF-R3, and GAPDH (SuperArray). A ΔΔCt analysis was performed using the control-treated samples as the reference sample. Data are expressed as relative mRNA levels ± SE (n = 3).
Immunoblotting.
Following trypsinization, Mz-ChA-1 cells (1 × 106 cells) were resuspended in lysis buffer as described (22) and sonicated. Immunoblots to detect Wnt 5a, phospho JNK, total JNK, and β-actin were performed as previously described (22) using specific antibodies against each protein. Data are expressed as fold change (mean ± SE) of the relative expression after normalization with β-actin.
Immunofluorescence.
Cells were seeded into six-well dishes containing a sterile coverslip on the bottom of each well. Cells were allowed to adhere overnight, and incubated with AEA (10 μM). Cells were then washed once in cold PBS, fixed to the coverslip with 4% paraformaldehyde (in PBS) at room temperature for 5 min, permeabilized in PBS containing 0.2% Triton X-100 (PBST), and blocked in 4% BSA (in PBST) for 1 h. Wnt 5a antibody was diluted in 1% BSA/PBST, added to the coverslips, and incubated overnight at 4°C. Cells were washed 3 × 10 min in PBST, and a 1:50 dilution (in 1% BSA/PBST) of cy3-conjugated secondary antibodies (Jackson Immunochemicals, West Grove, PA) was added for 2 h at room temperature. Cells were washed again and mounted into microscope slides with Antifade gold containing 4V,6-diamidino-2- phenylindole (DAPI) as a counterstain (Molecular Probes, Eugene, OR). Negative controls were done with the omission of the respective primary antibodies. Sections were visualized using an Olympus IX-71 inverted confocal microscope.
Cell proliferation assays.
Mz-ChA-1 cells were seeded into 96-well plates (10,000 cells/well) in a final volume of 200 μl of growth medium and allowed to adhere to the plate overnight. Because serum binds to and sequesters AEA (5), cells were then changed to serum-free media immediately before the addition of either AEA (10−5 M), or recombinant Wnt 5a (rWnt 5a; 50 ng/ml) for 48 h. Where appropriate, cells were pretreated with the Ca2+ chelator, BAPTA/AM (0.5 μM) (46) or an inhibitor for JNK (30 μM) (39) for 1 h before the addition of AEA or rWnt 5a as described above. Cell proliferation was assessed using a colorimetric cell proliferation assay (CellTiter 96AQueous; Promega, Madison, WI) and absorbance measured at 490 nm by a microplate spectrophotometer (Versamax; Molecular Devices, Sunnyvale, CA). In all cases, data are expressed as the fold change of treated cells compared with vehicle-treated controls.
Bromodeoxyuridine staining.
Bromodeoxyuridine (BrdU) assays were performed as described previously (11) using Mz-ChA-1 cells stimulated with AEA (10 μM) and rWnt 5a (50 ng/ml) for 48 h. The number of BrdU-positive nuclei was counted and expressed as a percentage of total cells in five random fields for each treatment group. Data are averages ± SE of five fields in three independent experiments.
Stable transfected cell lines.
The role of Wnt 5a and Ror2 expression in the antiproliferative actions of AEA were demonstrated using cells that have the expression of each of these genes stably knocked down. These cell lines were established using SureSilencing shRNA (SuperArray) plasmids for human Wnt 5a and Ror2, containing a marker for either neomycin resistance (Wnt 5a) or puromycin resistance (Ror2) for the selection of stably transfected cells, according to the instructions provided by the vendor. Briefly, Mz-ChA-1 were transfected with the shRNA-containing vectors or the control vector in a six-well plate with Mirus TransIT-LT1 Transfection Reagent (Madison, WI). Transfected cells were selected by the addition of 250 μg/ml of geneticin or 0.25 μg/ml puromycin into the media, and the selection process was allowed to continue for 3–4 days. Surviving cells were then split to a lower density in a 12-well plate so that each clone stems from only 5–10 cells. A total of 24 clones was then assessed for the relative knockdown of each specific gene, as well as related genes using real-time PCR, and a single clone with the greatest degree of knockdown was selected for subsequent experiments.
Intracellular calcium imaging.
Changes in intracellular calcium were assessed using a modification of the method by Long et al. (26). Briefly, Mz-ChA-1 cells were loaded with Fura-2 AM (10 μmol/l) diluted in calcium-free Hanks' buffered saline (HBS) and were imaged on a Nikon Eclipse microscope with a Photometrics camera. Cells were then placed in calcium-free HBS and alternatively excited at 340 and 380 nm. The ratio of 340/380 nm was continuously monitored in at least 10 cells per treatment. After a 5-min baseline, cells were treated with either AEA (10−5 M) or rWnt 5a (50 ng/ml) for 10 min followed by the addition of ionomycin (10 μM) to induce intracellular calcium release for 5 min.
RESULTS
AEA decreased cholangiocarcinoma tumor growth in vivo.
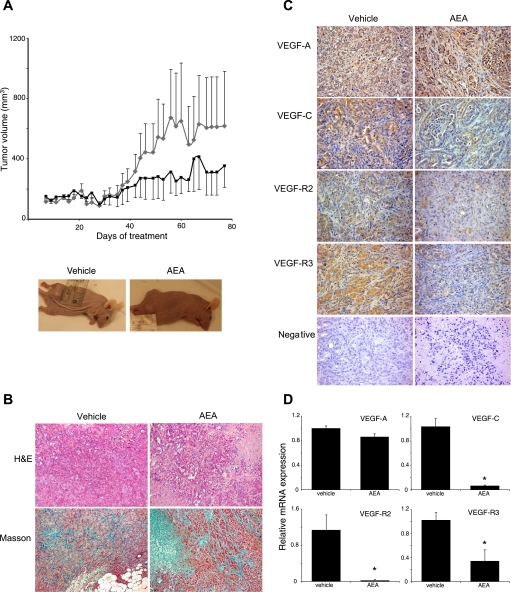
Treatment of cholangiocarcinoma tumors with AEA for 72 days significantly suppressed tumor growth from day 41 of treatment (P = 0.0086; Fig. 1A). Histological analysis of liver, heart, and kidney indicated no significant organ damage caused by the chronic AEA treatment (data not shown), suggesting that the AEA treatment was well tolerated.
Fig. 1.
Chronic anandamide (AEA) treatment decreases tumor growth in an in vivo xenograft model of cholangiocarcinoma. A: Mz-ChA-1 cells were injected into the flank of athymic mice. After tumors were established, mice were treated with 10 mg/kg per day intraperitoneal AEA (black) or vehicle (grey) 3 days per wk for 80 days, and tumor volume was assessed by triaxial measurements. Data are average tumor volumes ± SE. B: histological assessment of tumors from vehicle- and AEA-treated mice was performed by hematoxylin and eosin (H & E) staining and Masson's trichrome stain. H & E staining demonstrated that AEA treatment decreased the areas of tumor necrosis, whereas analysis of the Masson's trichrome staining showed that AEA increased the collagen content as an indicator of fibrosis. Magnification ×10. Expression of various members of the vascular endothelial growth factor (VEGF) family was assessed in tumor tissue by immunohistochemistry (C) and real-time PCR (D). Chronic AEA treatment decreased the immunoreactivity and mRNA expression of VEGF-C, VEGF-R2, and VEGF-R3 with no effect on the expression of VEGF-A. Data are expressed as average mRNA expressions ± SE after correction for GAPDH expression; *P < 0.05.
Histological analysis of the excised tumors revealed that all cells within tumors from AEA-treated and vehicle-treated animals were CK-7 positive, indicating cholangiocyte phenotype (data not shown). AEA treatment significantly decreased the area of tumor necrosis (Fig. 1B), and semi-quantitative analysis of collagen content as a marker of fibrosis showed that AEA increased fibrosis within the tumor (Fig. 1B).
We then analyzed the expression of the angiogenic factors of the VEGF family within the tumors. Chronic treatment with AEA decreased VEGF-C, VEGF-R2, and VEGF-R3 immunoreactivity, without any affect on VEGF-A immunoreactivity (Fig. 1C). These data were confirmed by real-time PCR analysis of RNA extracted from the AEA-treated and vehicle-treated tumor tissue. Once again, no significant effect of AEA on VEGF-A was observed; however, there was a dramatic decline in VEGF-C, VEGF-R2, and VEGF-R3 mRNA expression (Fig. 1D).
AEA treatment increases the expression of Wnt 5a in vitro and in vivo.
Treatment of the human cholangiocarcinoma cell line, Mz-ChA-1, with AEA for various time points increased the mRNA expression of Wnt 5a from 30 min up to 8 h (Fig. 2A). In addition, the protein expression of Wnt 5a was also increased up to 8 h after AEA treatment in vitro (Fig. 2B). These data were confirmed by immunofluorescent analysis of Wnt 5a expression, which showed an increase in Wnt 5a immunoreactivity predominantly in the cytoplasmic/membrane compartment of the cell (Fig. 2C). Examination of the AEA-treated tumor tissue also demonstrated an increase in Wnt 5a mRNA and immunoreactivity compared with vehicle-treated tissue (Fig. 2D and 2E).
Fig. 2.
AEA treatment increases the expression of Wnt 5a in cholangiocarcinoma cells. Mz-ChA-1 cells were treated with AEA (10 μM) for various time points. Wnt 5a expression was assessed by real-time PCR (A), immunoblotting (B), and immunofluorescence (C) in vitro and by real-time PCR (D) and immunohistochemistry (E) in tumors after AEA treatment in vivo. Where appropriate, data are expressed as average expressions ± SE after correction for GAPDH (A and D) or β-Actin (B), and * denotes significance (P < 0.05). Scale bar = 10 μM.
Wnt 5a decreases cholangiocyte proliferation to a similar degree as AEA.
We have previously shown that AEA decreases cholangiocyte proliferation in vitro (11). Given that AEA also increases Wnt 5a expression, we wanted to determine whether Wnt 5a could also decrease cholangiocyte proliferation. Indeed, treatment of Mz-ChA-1 cells with rWnt 5a decreased cell proliferation to a similar degree as AEA as shown by 3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS) assay (Fig. 3A). Furthermore, both AEA and rWnt 5a decreased the rate of BrdU incorporation compared with control-treated cells (Fig. 3B), suggesting that both AEA and Wnt 5a decreased the rate of cell cycle progression.
Fig. 3.
Treatment of cholangiocarcinoma cells with AEA or recombinant Wnt 5a in vitro decreased cell proliferation. Mz-ChA-1 cells were treated with AEA (10 μM) or recombinant Wnt (rWnt 5a) (50 ng/ml) for 48 h. Cell proliferation was assessed by 3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS) cell proliferation assays (A), and data are expressed as fold change in proliferation (average ± SE, n = 7); *P < 0.05 compared with basal treatment. Cell cycle progression was assessed by bromodeoxyuridine (BrdU) incorporation assays (B). The number of BrdU-positive cells was expressed as a percentage of total cells. Data are expressed as the averages ± SE from 5 random fields from 3 independent experiments; * denotes significance (P < 0.05) compared with basal treatment.
To definitively prove that Wnt 5a is involved in the antiproliferative effects of AEA, we specifically knocked down the expression of Wnt 5a in Mz-ChA-1 cells to 5% of the parental cell line (Fig. 4A) by stably transfecting a Wnt 5a shRNA construct. This had no effect on the expression of Wnt 5b (Fig. 4A). By using these cell lines we could clearly demonstrate that AEA decreased cell proliferation in the mock-transfected cell line (Mz-neo neg) to a similar degree as the parental Mz-ChA-1 cells (Fig. 4B). However, the antiproliferative effects of AEA were abolished by the absence of Wnt 5a expression in the Mz-Wnt 5a cell line (Fig. 4B), suggesting that Wnt 5a is required for the antiproliferative effects of AEA.
Fig. 4.
Specific knockdown of Wnt 5a expression abolished the antiproliferative effects of AEA. Mz-ChA-1 cells were stably transfected with Wnt 5a shRNA vectors. The expression of Wnt 5a and Wnt 5b were assessed in the parental cell line (Mz-ChA-1), the mock-transfected cell line (Mz-neo neg), and the cell line containing the Wnt 5a shRNA (Mz-Wnt 5a) by real-time PCR and immunoblotting (A). Data are expressed as averages ± SE after correction for GAPDH expression. The effect of AEA treatment on cell proliferation was assessed by MTS assays (B). The 3 cell lines were treated with AEA (10 μM) for 48 h, and data are expressed as fold change in proliferation (average ± SE, n = 7); *P < 0.05 compared with basal treatment within each cell line.
The downstream consequences of Wnt 5a activation are calcium independent and require the activation of Ror2 and JNK.
The noncanonical Wnt pathway can be calcium dependent or independent (21). We wanted to determine which molecular pathway AEA and Wnt 5a were functioning through to exert their antiproliferative effects. Using Fura AM as a fluorescent indicator of intracellular calcium release, it was evident that neither AEA or rWnt 5a had any effect on calcium release, but subsequent ionomycin administration increased intracellular calcium (data not shown). In addition, pretreatment of Mz-ChA-1 cells with the calcium chelator BAPTA/AM before the administration of AEA or rWnt 5a failed to inhibit the antiproliferative effects exerted by these agents (data not shown).
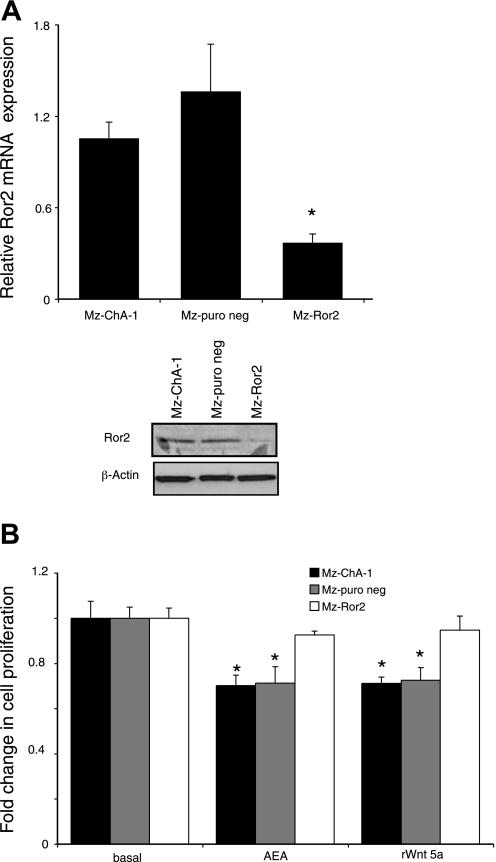
The calcium-independent pathway that is activated by Wnt 5a involves the activation of the orphan receptor Ror2. We generated a stable transfected cell line using a specific shRNA construct against human Ror2. This cell line had Ror2 expression levels ∼24% of the mock-transfected cell line (Fig. 5A). Once again, AEA and rWnt 5a decreased cell proliferation in the mock-transfected cell line (Mz-puro neg; Fig. 5B), whereas, in the Ror2 shRNA cell line (Mz-Ror2), AEA and rWnt 5a had no effect on cell proliferation (Fig. 5B), suggesting that indeed AEA and rWnt 5a exert their antiproliferative effects through the activation of Ror2.
Fig. 5.
Specific knockdown of Ror2 expression abolished the antiproliferative effects of AEA and rWnt 5a. Mz-ChA-1 cells were stably transfected with Ror2 shRNA vectors. The expression of Ror2 was assessed in the parental cell line (Mz-ChA-1), the mock-transfected cell line (Mz-puro neg), and the cell line containing the Ror2 shRNA (Mz-Ror2) by real-time PCR and immunoblotting (A). Data are expressed as averages ± SE after correction for GAPDH expression. The effect of AEA and rWnt 5a treatment on cell proliferation was assessed by MTS assays (B). The 3 cell lines were treated with AEA (10 μM) or rWnt 5a (50 ng/ml) for 48 h, and data are expressed as fold change in proliferation (average ± SE, n = 7); *P < 0.05 compared with basal treatment within each cell line.
A downstream consequence of Wnt 5a activation of Ror2 may be the activation of JNK (38). Indeed, treatment of Mz-ChA-1 cells or the mock-transfected cell lines by AEA and rWnt 5a increased phospho JNK by up to twofold (Fig. 6A and data not shown). However, AEA stimulation of the Wnt 5a shRNA cell line (Mz-Wnt 5a) failed to activate JNK (Fig. 6A), and stimulation of the Ror2 shRNA cell line (Mz-Ror2) with AEA or rWnt 5a also failed to increase phospho JNK (Fig. 6A), suggesting that AEA activates JNK by a mechanism requiring Wnt 5a and Ror2. Furthermore, pretreatment of the Mz-ChA-1 cell line with the JNK inhibitor (SP600125) prevented the antiproliferative effects of AEA and rWnt 5a (Fig. 6B).
Fig. 6.
Activation of JNK is necessary for the antiproliferative effects of AEA and rWnt 5a in cholangiocarcinoma cells. A: JNK activation was assessed by immunoblotting using phosphospecific antibodies in Mz-ChA-1 cells after AEA (10 μM) or rWnt5a (50 ng/ml) treatment. Data are expressed as an average ratio of phospho-JNK (pJNK) to total JNK expression (± SE, n = 4), and * denotes significance (P < 0.05). This JNK activation was abolished by the specific knockdown of Wnt 5a (Mz-Wnt 5a) or Ror2 (Mz-Ror2) expression. B: involvement of JNK activation in the antiproliferative effects of AEA and Wnt 5a was assessed by MTS assay. Mz-ChA-1 cells were pretreated with the JNK inhibitor (JNK Inh.) (SP 600125; 30 μM) for 30 min before the addition of AEA (10 μM) or rWnt 5a (50 ng/m) for 48 h, and data are expressed as fold change in proliferation (average ± SE, n = 7); *P < 0.05 compared with basal treatment.
DISCUSSION
The findings of this study relate to the endocannabinoid system and subsequent downstream cell signaling events as potential therapeutic targets regulating cholangiocarcinoma cell growth. By using an in vivo xenograft model of cholangiocarcinoma, we showed that AEA exerts tumor growth-suppressing effects, which was coupled to increased fibrosis and decreased expression of certain members of the VEGF family of angiogenic factors. The antiproliferative effects of AEA occurred via the upregulation of Wnt 5a expression and subsequent involvement of Ror2-mediated JNK activation. These data suggest that therapies aimed at either modulating the endogenous levels of AEA in vivo, or activating the Wnt 5a/Ror2/JNK pathway may prove beneficial in the treatment of cholangiocarcinoma.
We have previously shown the antiproliferative effects of AEA in cholangiocarcinoma cells in vitro (11). This effect was via a Cb1- and Cb2-independent mechanism involving the stabilization of lipid rafts in the plasma membrane and the recruitment of death receptor complexes into these membrane microdomains (11). Furthermore, we have demonstrated an antiproliferative action of AEA on hyperplastic cholangiocyte proliferation via a Cb2-dependent mechanism (10). The novel data presented here extend our findings to include the effects of chronic AEA treatment to cholangiocarcinoma tumor growth in vivo. Consistent with our findings, cannabinoids of various origins (endogenous, plant-derived, or synthetic analogs) have been shown to suppress cancer cell growth in vitro (9, 35–37) as well as in vivo (16). Indeed, a recent clinical pilot study to determine the safety of intracranial administration of delta-9-tetrahydrocannabinol in patients with glioblastoma demonstrated a marked reduction in Ki67 staining within the tumor (19). This observation, together with the very promising results observed in cell cultures and laboratory animals (9, 16, 35–37), suggests that administering cannabinoids alone or in conjunction with existing chemotherapeutic agents may be a promising treatment strategy for aggressive cancers of various origins.
Our in vivo data demonstrated that AEA also decreases tumor progression by reducing the expression of trophic factors such as VEGF-C, and their receptors VEGF-R2 and VEGF-R3. These factors are necessary for the vascularization of the tumors (13, 14) and contribute to the development and growth of cholangiocarcinoma tumors. We have previously shown that γ-amino butyric acid also exerts its tumor growth-suppressing effects in part via decreased VEGF expression (12). Indeed, treatment of cholangiocarcinoma cells with recombinant VEGF-A increased proliferation and was shown to be responsible for the proliferative effects of estrogen (28). Data presented here clearly show a role for the noncanonical, Wnt 5a-mediated signal transduction pathway in the antiproliferative effects of AEA. To our knowledge, this is the first demonstration of regulation of the noncanonical Wnt signaling pathway by cannabinoids. In support of our data, Wnt 5a has also been shown to have tumor-suppressive properties in other forms of cancer (24, 25, 34, 51, 52). One possible mechanism by which Wnt 5a may exert its tumor-suppressive properties is by the antagonism of the canonical Wnt signaling pathway via downregulation of the intracellular β-catenin protein levels and concomitant decrease in β-catenin activity (52). The subsequent activity of the canonical Wnt pathways after AEA treatment in cholangiocarcinoma has not yet been studied.
Our data indicate a role for the tyrosine kinase orphan receptor Ror2 and subsequent JNK activation in the activated noncanonical Wnt pathway. Wnt 5a activation of Ror2 has been established as an alternative noncanonical pathway to the Wnt/Ca2+ pathway (32, 38), and it may regulate various biological functions such as filopodia formation (31) and cell polarity (50). An antiproliferative effect of the Wnt 5a/Ror2/JNK pathway has previously been shown in colon cancer cells, which ultimately resulted in the suppression of the defective canonical Wnt signaling pathway in these cells (27). Furthermore, increased nuclear staining of β-catenin, indicative of canonical Wnt signaling activation, has been demonstrated in cholangiocarcinoma biopsy samples (44).
The effects of JNK activation on cholangiocarcinoma cell growth has previously been studied (49). Treatment of cholangiocarcinoma cells with tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) triggered an apoptotic pathway that involved JNK-dependent events (49). The data presented here demonstrate that JNK activation is also required for the antiproliferative effects of AEA. We have previously shown that AEA treatment facilitates death receptor complex formation (11), an event that is also necessary for TRAIL-induced apoptosis (45). Taken together, these data support our findings of an AEA-stimulated activation of JNK and its subsequent role in the antiproliferative effects.
We have previously shown that AEA exerts its antiproliferative effects by stabilizing the lipid raft structures (11). Whether the activation of the Wnt 5a-dependent pathway by AEA shown here is directly associated with lipid rafts or is a downstream consequence of a lipid raft-mediated event is unknown. However, there is evidence to suggest that Wnt signaling molecules can be targeted to lipid raft structures (53). The role of lipid rafts in the activation of Wnt 5a-mediated signaling is a topic of ongoing research in our laboratory.
In conclusion, we have demonstrated antiproliferative effects of AEA in an in vivo xenograft model of cholangiocarcinoma, and this occurs via the upregulation of Wnt 5a expression and subsequent activation of Ror2 and JNK. We propose that the development of novel therapeutic strategies aimed at modulating the endocannabinoid system, or mimicking the mode of action of AEA, would prove beneficial for the treatment of this devastating disease.
GRANTS
This work was supported by an NIH K01 grant award (DK078532) to Dr. DeMorrow and by a Veterans Affairs Merit Award, a Veterans Affairs Research Scholar Award, and the NIH grants DK062975 and DK58411 to Dr. Alpini. Dr. Gaudio was supported by Ministero Istruzione Universitá e Ricerca grants (PRIN 2005) and Faculty funds.
Acknowledgments
We acknowledge Glen Cryer of the Scott & White Hospital, Grants Administration Office for assistance with proofreading and the Scott & White Hospital animal facility staff for assistance with animal surgical models. We also acknowledge the Texas A & M Health Science Center Microscopy Imaging Center for assistance with the confocal microscopy imaging.
The costs of publication of this article were defrayed in part by the payment of page charges. The article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Alpini G, Kanno N, Phinizy JL, Glaser S, Francis H, Taffetani S, LeSage G. Tauroursodeoxycholate inhibits human cholangiocarcinoma growth via Ca2+-, PKC-, and MAPK-dependent pathways. Am J Physiol Gastrointest Liver Physiol 286: G973–G982, 2004. [DOI] [PubMed] [Google Scholar]
- 2.Alpini G, Prall R, LaRusso N. The pathobiology of biliary epithelia. In: The Liver: Biology And Pathobiology, (4th ed.), edited by Arias IM. Philadelphia, PA: Lippincott Williams and Wilkins, 2001, pp. 4E 421–435.
- 3.Baker D, Pryce G, Croxford JL, Brown P, Pertwee RG, Huffman JW, Layward L. Cannabinoids control spasticity and tremor in a multiple sclerosis model. Nature 404: 84–87, 2000. [DOI] [PubMed] [Google Scholar]
- 4.Bifulco M, Laezza C, Valenti M, Ligresti A, Portella G, VDIM. A new strategy to block tumor growth by inhibiting endocannabinoid inactivation. FASEB J 18: 1606–1608, 2004. [DOI] [PubMed] [Google Scholar]
- 5.Bojesen IN, Hansen HS. Binding of anandamide to bovine serum albumin. J Lipid Res 44: 1790–1794, 2003. [DOI] [PubMed] [Google Scholar]
- 6.Calignano A, La Rana G, Giuffrida A, Piomelli D. Control of pain initiation by endogenous cannabinoids. Nature 394: 277–281, 1998. [DOI] [PubMed] [Google Scholar]
- 7.Carpino G, Morini S, Ginanni Corradini S, Franchitto A, Merli M, Siciliano M, Gentili F, Onetti Muda A, Berloco P, Rossi M, Attili AF, Gaudio E. Alpha-SMA expression in hepatic stellate cells and quantitative analysis of hepatic fibrosis in cirrhosis and in recurrent chronic hepatitis after liver transplantation. Dig Liver Dis 37: 349–356, 2005. [DOI] [PubMed] [Google Scholar]
- 8.Cheng CW, Yeh JC, Fan TP, Smith SK, Charnock-Jones DS. Wnt5a-mediated non-canonical Wnt signalling regulates human endothelial cell proliferation and migration. Biochem Biophys Res Commun 365: 285–290, 2008. [DOI] [PubMed] [Google Scholar]
- 9.De Petrocellis L, Melck D, Palmisano A, Bisogno T, Laezza C, Bifulco M, Di Marzo V. The endogenous cannabinoid anandamide inhibits human breast cancer cell proliferation. Proc Natl Acad Sci USA 95: 8375–8380, 1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeMorrow S, Francis H, Gaudio E, Ueno Y, Venter J, Onori P, Franchitto A, Vaculin B, Vaculin S, Alpini G. Anandamide inhibits cholangiocyte hyperplastic proliferation via activation of thioredoxin 1/redox factor 1 and AP-1 activation. Am J Physiol Gastrointest Liver Physiol 294: G506–G519, 2008. [DOI] [PubMed] [Google Scholar]
- 11.DeMorrow S, Glaser S, Francis H, Venter J, Vaculin B, Vaculin S, Alpini G. Opposing actions of endocannabinoids on cholangiocarcinoma growth: recruitment of fas and fas ligand to lipid rafts. J Biol Chem 282: 13098–13113, 2007. [DOI] [PubMed] [Google Scholar]
- 12.Fava G, Marucci L, Glaser S, Francis H, De Morrow S, Benedetti A, Alvaro D, Venter J, Meininger C, Patel T, Taffetani S, Marzioni M, Summers R, Reichenbach R, Alpini G. gamma-Aminobutyric acid inhibits cholangiocarcinoma growth by cyclic AMP-dependent regulation of the protein kinase A/extracellular signal-regulated kinase 1/2 pathway. Cancer Res 65: 11437–11446, 2005. [DOI] [PubMed] [Google Scholar]
- 13.Ferrara N VEGF as a therapeutic target in cancer. Oncology 69, Suppl 3: 11–16, 2005. [DOI] [PubMed] [Google Scholar]
- 14.Ferrara N, Kerbel RS. Angiogenesis as a therapeutic target. Nature 438: 967–974, 2005. [DOI] [PubMed] [Google Scholar]
- 15.Fodde R, Brabletz T. Wnt/beta-catenin signaling in cancer stemness and malignant behavior. Curr Opin Cell Biol 19: 150–158, 2007. [DOI] [PubMed] [Google Scholar]
- 16.Galve-Roperh I, Sanchez C, Cortes ML, del Pulgar TG, Izquierdo M, Guzman M. Anti-tumoral action of cannabinoids: involvement of sustained ceramide accumulation and extracellular signal-regulated kinase activation. Nat Med 6: 313–319, 2000. [DOI] [PubMed] [Google Scholar]
- 17.Gaudio E, Barbaro B, Alvaro D, Glaser S, Francis H, Ueno Y, Meininger CJ, Franchitto A, Onori P, Marzioni M, Taffetani S, Fava G, Stoica G, Venter J, Reichenbach R, DeMorrow S, Summers R, Alpini G. Vascular endothelial growth factor stimulates rat cholangiocyte proliferation via an autocrine mechanism. Gastroenterology 130: 1270–1282, 2006. [DOI] [PubMed] [Google Scholar]
- 18.Glaser S, Benedetti A, Marucci L, Alvaro D, Baiocchi L, Kanno N, Caligiuri A, Phinizy JL, Chowdhury U, Papa E, LeSage G, Alpini G. Gastrin inhibits cholangiocyte growth in bile duct-ligated rats by interaction with cholecystokinin-B/Gastrin receptors via d-myo-inositol 1,4,5-triphosphate-, Ca(2+)-, and protein kinase C alpha-dependent mechanisms. Hepatology 32: 17–25, 2000. [DOI] [PubMed] [Google Scholar]
- 19.Guzman M, Duarte MJ, Blazquez C, Ravina J, Rosa MC, Galve-Roperh I, Sanchez C, Velasco G, Gonzalez-Feria L. A pilot clinical study of Delta(9)-tetrahydrocannabinol in patients with recurrent glioblastoma multiforme. Br J Cancer 95: 197–203, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hayase T, Yamamoto Y, Yamamoto K. Protective effects of cannabinoid receptor ligands analogous to anandamide against cocaine toxicity. Nihon Arukoru Yakubutsu Igakkai Zasshi 36: 596–608, 2001. [PubMed] [Google Scholar]
- 21.Johnson ML, Rajamannan N. Diseases of Wnt signaling. Rev Endocr Metab Disord 7: 41–49, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kanno N, Glaser S, Chowdhury U, Phinizy JL, Baiocchi L, Francis H, LeSage G, Alpini G. Gastrin inhibits cholangiocarcinoma growth through increased apoptosis by activation of Ca2+-dependent protein kinase C-alpha. J Hepatol 34: 284–291, 2001. [DOI] [PubMed] [Google Scholar]
- 23.Knuth A, Gabbert H, Dippold W, Klein O, Sachsse W, Bitter-Suermann D, Prellwitz W, Meyer zum Buschenfelde KH. Biliary adenocarcinoma. Characterisation of three new human tumor cell lines. J Hepatol 1: 579–596, 1985. [DOI] [PubMed] [Google Scholar]
- 24.Kremenevskaja N, von Wasielewski R, Rao AS, Schofl C, Andersson T, Brabant G. Wnt-5a has tumor suppressor activity in thyroid carcinoma. Oncogene 24: 2144–2154, 2005. [DOI] [PubMed] [Google Scholar]
- 25.Liang H, Chen Q, Coles AH, Anderson SJ, Pihan G, Bradley A, Gerstein R, Jurecic R, Jones SN. Wnt5a inhibits B cell proliferation and functions as a tumor suppressor in hematopoietic tissue. Cancer Cell 4: 349–360, 2003. [DOI] [PubMed] [Google Scholar]
- 26.Long C, Cook LG, Hamilton SL, Wu GY, Mitchell BM. FK506 binding protein 12/12.6 depletion increases endothelial nitric oxide synthase threonine 495 phosphorylation and blood pressure. Hypertension 49: 569–576, 2007. [DOI] [PubMed] [Google Scholar]
- 27.MacLeod RJ, Hayes M, Pacheco I. Wnt5a secretion stimulated by the extracellular calcium-sensing receptor inhibits defective Wnt signaling in colon cancer cells. Am J Physiol Gastrointest Liver Physiol 293: G403–G411, 2007. [DOI] [PubMed] [Google Scholar]
- 28.Mancino A, Mancino MG, Glaser SS, Alpini G, Bolognese A, Izzo L, Francis H, Onori P, Franchitto A, Ginanni-Corradini S, Gaudio E, Alvaro D. Estrogens stimulate the proliferation of human cholangiocarcinoma by inducing the expression and secretion of vascular endothelial growth factor. Dig Liver Dis. In press. [DOI] [PMC free article] [PubMed]
- 29.Manzanares J, Corchero J, Romero J, Fernandez-Ruiz JJ, Ramos JA, Fuentes JA. Pharmacological and biochemical interactions between opioids and cannabinoids. Trends Pharmacol Sci 20: 287–294, 1999. [DOI] [PubMed] [Google Scholar]
- 30.Moon RT Wnt/beta-catenin pathway. Sci STKE 271: cm1, 2005. [DOI] [PubMed]
- 31.Nishita M, Yoo SK, Nomachi A, Kani S, Sougawa N, Ohta Y, Takada S, Kikuchi A, Minami Y. Filopodia formation mediated by receptor tyrosine kinase Ror2 is required for Wnt5a-induced cell migration. J Cell Biol 175: 555–562, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oishi I, Suzuki H, Onishi N, Takada R, Kani S, Ohkawara B, Koshida I, Suzuki K, Yamada G, Schwabe GC, Mundlos S, Shibuya H, Takada S, Minami Y. The receptor tyrosine kinase Ror2 is involved in non-canonical Wnt5a/JNK signalling pathway. Genes Cells 8: 645–654, 2003. [DOI] [PubMed] [Google Scholar]
- 33.Piomelli D, Giuffrida A, Calignano A, Rodriguez de Fonseca F. The endocannabinoid system as a target for therapeutic drugs. Trends Pharmacol Sci 21: 218–224, 2000. [DOI] [PubMed] [Google Scholar]
- 34.Roman-Gomez J, Jimenez-Velasco A, Cordeu L, Vilas-Zornoza A, San Jose-Eneriz E, Garate L, Castillejo JA, Martin V, Prosper F, Heiniger A, Torres A, Agirre X. WNT5A, a putative tumour suppressor of lymphoid malignancies, is inactivated by aberrant methylation in acute lymphoblastic leukaemia. Eur J Cancer 43: 2736–2746, 2007. [DOI] [PubMed] [Google Scholar]
- 35.Ruiz L, Miguel A, Diaz-Laviada I. Delta9-tetrahydrocannabinol induces apoptosis in human prostate PC-3 cells via a receptor-independent mechanism. FEBS Lett 458: 400–404, 1999. [DOI] [PubMed] [Google Scholar]
- 36.Sanchez C, de Ceballos ML, del Pulgar TG, Rueda D, Corbacho C, Velasco G, Galve-Roperh I, Huffman JW, Ramon y Cajal S, Guzman M. Inhibition of glioma growth in vivo by selective activation of the CB(2) cannabinoid receptor. Cancer Res 61: 5784–5789, 2001. [PubMed] [Google Scholar]
- 37.Sanchez C, Galve-Roperh I, Canova C, Brachet P, Guzman M. Delta9-tetrahydrocannabinol induces apoptosis in C6 glioma cells. FEBS Lett 436: 6–10, 1998. [DOI] [PubMed] [Google Scholar]
- 38.Schambony A, Wedlich D. Wnt-5A/Ror2 regulate expression of XPAPC through an alternative noncanonical signaling pathway. Dev Cell 12: 779–792, 2007. [DOI] [PubMed] [Google Scholar]
- 39.Shin M, Yan C, Boyd D. An inhibitor of c-jun aminoterminal kinase (SP600125) represses c-Jun activation, DNA-binding and PMA-inducible 92-kDa type IV collagenase expression. Biochim Biophys Acta 1589: 311–316, 2002. [DOI] [PubMed] [Google Scholar]
- 40.Sirica AE Cholangiocarcinoma: molecular targeting strategies for chemoprevention and therapy. Hepatology 41: 5–15, 2005. [DOI] [PubMed] [Google Scholar]
- 41.Slusarski DC, Yang-Snyder J, Busa WB, Moon RT. Modulation of embryonic intracellular Ca2+ signaling by Wnt-5A. Dev Biol 182: 114–120, 1997. [DOI] [PubMed] [Google Scholar]
- 42.Smalley MJ, Dale TC. Wnt signalling in mammalian development and cancer. Cancer Metastasis Rev 18: 215–230, 1999. [DOI] [PubMed] [Google Scholar]
- 43.Smith PB, Compton DR, Welch SP, Razdan RK, Mechoulam R, Martin BR. The pharmacological activity of anandamide, a putative endogenous cannabinoid, in mice. J Pharmacol Exp Ther 270: 219–227, 1994. [PubMed] [Google Scholar]
- 44.Sugimachi K, Taguchi K, Aishima S, Tanaka S, Shimada M, Kajiyama K, Sugimachi K, Tsuneyoshi M. Altered expression of beta-catenin without genetic mutation in intrahepatic cholangiocarcinoma. Mod Pathol 14: 900–905, 2001. [DOI] [PubMed] [Google Scholar]
- 45.Thorburn A Death receptor-induced cell killing. Cell Signal 16: 139–144, 2004. [DOI] [PubMed] [Google Scholar]
- 46.Tsien RY New calcium indicators and buffers with high selectivity against magnesium and protons: design, synthesis, and properties of prototype structures. Biochemistry 19: 2396–2404, 1980. [DOI] [PubMed] [Google Scholar]
- 47.van der Stelt M, Veldhuis WB, van Haaften GW, Fezza F, Bisogno T, Bar PR, Veldink GA, Vliegenthart JF, Di Marzo V, Nicolay K. Exogenous anandamide protects rat brain against acute neuronal injury in vivo. J Neurosci 21: 8765–8771, 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Voth EA, Schwartz RH. Medicinal applications of delta-9-tetrahydrocannabinol and marijuana. Ann Intern Med 126: 791–798, 1997. [DOI] [PubMed] [Google Scholar]
- 49.Werneburg NW, Guicciardi ME, Bronk SF, Kaufmann SH, Gores GJ. Tumor necrosis factor-related apoptosis-inducing ligand activates a lysosomal pathway of apoptosis that is regulated by Bcl-2 proteins. J Biol Chem 282: 28960–28970, 2007. [DOI] [PubMed] [Google Scholar]
- 50.Yamanaka H, Moriguchi T, Masuyama N, Kusakabe M, Hanafusa H, Takada R, Takada S, Nishida E. JNK functions in the non-canonical Wnt pathway to regulate convergent extension movements in vertebrates. EMBO Rep 3: 69–75, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ying J, Li H, Chen YW, Srivastava G, Gao Z, Tao Q. WNT5A is epigenetically silenced in hematologic malignancies and inhibits leukemia cell growth as a tumor suppressor. Blood 110: 4130–4132, 2007. [DOI] [PubMed] [Google Scholar]
- 52.Ying J, Li H, Yu J, Ng KM, Poon FF, Wong SC, Chan AT, Sung JJ, Tao Q. WNT5A exhibits tumor-suppressive activity through antagonizing the Wnt/beta-catenin signaling, and is frequently methylated in colorectal cancer. Clin Cancer Res 14: 55–61, 2008. [DOI] [PubMed] [Google Scholar]
- 53.Zhai L, Chaturvedi D, Cumberledge S. Drosophila wnt-1 undergoes a hydrophobic modification and is targeted to lipid rafts, a process that requires porcupine. J Biol Chem 279: 33220–33227, 2004. [DOI] [PubMed] [Google Scholar]