Abstract
Patients’ cognitive abilities and verbal expressions of commitment to behavior change predict different aspects of substance abuse treatment outcome, but these two traits have never been examined conjointly. We therefore investigated patients’ cognitive abilities and verbal expressions of commitment to behavior change as predictors of retention and drug use outcomes in an outpatient cognitive behavioral treatment (CBT) of adult cocaine dependent patients. A neuropsychological battery was administered at baseline. Two independent raters used recordings of CBT sessions to code commitment language strength across the temporal segments (e.g. beginning, middle, and end) of one session per patient. Better cognitive abilities predicted treatment retention (p <.01) but not drug use, while mean commitment strength across the session segments predicted reduced drug use (p=.01). Results indicate that while commitment to behavioral changes such as abstinence may occur independently of patient’s cognitive abilities, engagement in the behavioral intervention process appears to depend on cognitive abilities. Future clinical studies should further investigate the relations between cognition and commitment to change and their differential contributions to treatment processes and outcome.
Keywords: Cognition, commitment language, behavioral change, substance abuse treatment
Introduction
Despite advances in evidence-based behavioral treatments for substance dependence, improving the outcome of these treatments requires a better understanding of clinical characteristics and treatment processes that affect outcome. Two areas that are recently attracting increased focus are patients’ levels of cognitive functioning during treatment (Aharonovich et al., 2006), and the language that patients use in their treatment sessions, specifically language expressing commitment to change the target drug use behaviors (Amrhein, Miller, Yahne, Palmer, & Fulcher, 2003; Moyers et al., 2007).
Alcohol and substance abusers frequently show impairments in cognitive functioning. Impairments in such functioning can impact many aspects of treatment, including the learning and retention of new treatment-relevant information concerning behavior change (Roehrich & Goldman, 1993; McCrady & Smith, 1986; Teichner, Horner, Roitzsch, Herron, & Thevos, 2002), and the acquisition of new coping behaviors (Alterman, Holahan, Baughman, & Michels, 1989). Importantly, cognitive impairments predict poor achievement of therapeutic outcomes in alcoholics (Bates, Bowden, & Barry, 2002; Bates, Pawlak, Tonigan, & Buckman, 2006) and in substance abusers (Horner, 1999; Fals-Stewart, 1993), lower retention in residential programs for alcoholics and substance abusers (Fals-Stewart & Shafer, 1992), and lower retention in outpatient treatment for cocaine dependence (Aharonovich, Nunes, & Hasin, 2003; Aharonovich et al., 2006) and marijuana dependence (Aharonovich et al., 2008). The evidence suggests that cognitive deficits affect both treatment process and outcome across substances and treatment modalities.
The importance of motivation to change is well understood in the substance abuse clinical literature, and consequently, improving low levels of motivation or commitment to behavioral change is central to the success of behavioral treatment for substance use (Amrhein et al., 2003). Among patients with low commitment, therapists conducting Motivational Interviewing (MI; (Miller & Rollnick, 1991; Miller & Rollnick, 2002) or Cognitive Behavioral Treatment – Relapse Prevention (CBT-RP; (Carroll, 1998)) attempt to increase motivation to change with various techniques, including the elicitation and reinforcement of patient language indicating a commitment to change behavior (i.e. “change talk”; (Miller et al., 2002). The shifts in patient language from lack of commitment or ambivalence at the beginning of a session to a strong commitment to change by the end of the therapy session can be understood as a reflection of successful engagement in the therapeutic process. This dynamic aspect of the process can be studied empirically through analysis of codes assigned to patient statements in recorded therapy sessions (Amrhein, 2004). In such research, patients’ statements are coded as indicating commitment to change (e.g., “I’ve decided to stop using”, “I am very determined to quit using”), neutrality towards change (e.g., “Occasionally, I think about changing my cocaine use”), or lack of commitment to change (“I will probably use as soon as I get my paycheck”). Further, commitment does not necessarily increase steadily through a successful MI session. Theoretically, a degree of a drop in commitment (“backpedaling”; Amrhein et al., 2003) might be expected among patients engaged in the treatment process when they begin to fully confront the change they need to make, which in MI can begin with the discussion of a behavioral change plan. Consistent with this, Amrhein et al., 2003 studied patient language by decile of the MI therapy session, finding that patients with successful outcomes in terms of abstinence showed a mid-session dip in commitment strength in the 4th decile, when the modal topic was initiation of discussion of the behavioral change plan, with a steady rise after that until the final decile of the session. Thus, to best understand the relationship of commitment language to treatment retention and outcome, both overall commitment strength as well as its dynamic shifts during segments of the therapy session are important to investigate.
Cognitive impairments have the potential to impede engagement in the therapeutic process. This may be reflected by little or no expressed language indicating commitment to reduce substance use throughout a session. Alternatively, cognitive impairments may impede understanding of the session content, as reflected by little evidence of expected shifts in commitment language according to the session decile and the modal topics of discussion that characterize session deciles. However, the relationship of cognitive functioning to commitment language in therapy and its shifts has never been studied. The only related evidence to date comes from a single study in non-patients indicating a relationship between poor verbal memory and lack of readiness to reduce drinking (Blume, Schmaling, & Marlatt, 2005). Since impaired cognitive functioning is common in substance abuse patients and commitment to change is important in the therapeutic process, we investigated the relationship of cognitive functioning to the production of verbal commitment statements. We did this for Cognitive Behavioral Therapy (CBT) sessions for cocaine dependence, since commitment language has not yet been studied in this common and important type of behavioral intervention. Specifically, we investigated the relationship of cognitive functioning to commitment language and its shifts during a CBT session, and the relationship of such commitment language to treatment outcome measures (retention in treatment and drug use). Consistent with our previous research, we studied both mean commitment to change averaged across all segments of a session as well as decile-appropriate shifts towards greater commitment to change by the end of the session. We hypothesized that compared to patients with better cognitive functioning, patients with lower cognitive functioning would show weaker decile-appropriate shifts towards commitment strength across the temporal segments of the CBT session. We also hypothesized that weaker verbal commitment strength to change would predict poorer treatment outcome.
Methods
Procedures
This study was based on a subset of patients participating in a larger study described in detail elsewhere (Aharonovich et al., 2006). All participants were patients in placebo-controlled randomized medication trials for cocaine dependence that included individual 12 CBT-RP weekly sessions. After signing consent for screening, participants were evaluated with the SCID I/P interview [Axis I, DSM IV version; (First, Spitzer, Gibbon, & Williams, 1997)] administered by trained masters- or doctoral-level clinical psychologists, and a physical examination by a physician. Eligible patients signed a consent form for participation in a sub-study of neurocognitive functioning, following procedures approved by the Institutional Review Board at the New York State Psychiatric Institute. A computerized neuropsychological battery was administered at treatment entry to test patients’ neurocognitive functioning, for which patients were paid $20.00. Participants also gave written consent to audiotape their CBT-RP sessions; commitment language expressed during the session was coded using these recordings. Observed urine samples were collected at baseline and weekly during the course of the CBT-RP treatment and quantitatively analyzed for cocaine metabolites.
Sample
Participants were 24 cocaine dependent patients from the larger study with available recorded CBT-RP sessions. Inclusion criteria for the study included meeting DSM-IV criteria for current (last 12 months) cocaine dependence. Exclusion criteria consisted of meeting DSM-IV criteria for bipolar disorder, any psychotic disorder, ADHD, another substance use disorder (except nicotine dependence), having an unstable medical condition, history of seizure disorders, or history of head injury with loss of consciousness >1 hour. The patients’ mean age was 36.67 years (SD=7.06, range 23–51). Mean years of education was 14.90 years (SD = 2.18, range 10–19). 67% (16) of the patients were male, 58% (14) were African American, 8% (2) were White, 17% (4) were married, and 17% (4) were left handed. The mean years of drug use was 11.0 (SD=5.5). Average days of use per week in the 30 days before treatment was 5 (SD =1.2, range 1–7). The breakdown of drug use methods was as follows: 63% (15) smoked crack, 29% (7) snorted cocaine, and 8% (2) used both methods.
Measures
Neuropsychological battery
As described previously (Aharonovich et al., 2006), the primary measure of cognitive functioning was the computerized MicroCog (MC) Assessment of Cognitive Functioning (Powell, Kaplan, Whitla, Catlin, & Funkenstein, 1993). This ~ 60 minute battery is normed and standardized for adults. The MC yields cognitive performance scores involving attention, abstract reasoning, memory, spatial processing, reaction time and overall measures of accuracy and information processing speed. Two composite scores indicate general cognitive functioning (GCF), consisting of combined accuracy and speed weighted equally, and global cognitive proficiency (GCP), consisting of combined accuracy and speed, with preferential weight to accuracy. The Wisconsin Card Sort Test [WCST, Computer Version–2 Research Edition,(Heaton, 1999)] was also administered. This ~20 minute non-verbal test assesses cognitive flexibility, the ability to use environmental feedback to accurately shift responses.
Commitment language coding system
The strength and frequency of commitment language during recorded CBT-RP sessions was coded using procedures described by Amrhein et al. (Amrhein et al., 2003). Because the first CBT-RP session is primarily orientation and thus commitment language does not reflect the therapeutic process, the coded CBT session was the 2nd or 3rd session (depending on recording availability or quality). Session length averaged 50 min (range: 30–60 min). To standardize the length of temporal segments within the session, each session was divided into 10 equal temporal segments, or deciles. The length of each decile was the total number of minutes in the session divided by 10. Two independent coders (P.C.A. and a trained research technician), blind to patient characteristics (e.g., severity of drug use, treatment outcome), coded patient commitment statements in the CBT-RP sessions. The coded statements were those made by the patients pertaining to their substance use, either in response to therapist inquiries or in an unsolicited, spontaneous manner. Brief acquiescent replies were excluded (e.g., therapist says, “Sounds like you’re ready for a change”, to which patient replies “Yeah.”). On a scoring sheet, level of strength of patient statements reflecting commitment to change (or lack thereof) were scored with values ranging from −5 (intent to continue drug use) to +5 (intent to reduce or stop drug use). In this sample, inter-rater reliability on these scores as indicated by the intraclass correlation coefficient was .76, indicating excellent reliability consistent with previous reports (Amrhein et al., 2003). For each patient, the data consisted of two 10-decile data files, one reflecting frequencies and the other mean strength values, averaged over coders.
Commitment strength as predictor of outcome
two scores representing commitment strength were computed. The mean commitment strength score for the full session was computed as the average of commitment strength levels across all session deciles for each patient. The second score was the commitment shift. This was computed for each patient by taking the difference between the commitment strength of the 5th decile, or midpoint of the session, and the 10th decile, or session-end. We selected the 5th decile because in this decile, the modal topic was the beginning of the functional analysis, the beginning of the specific confrontation by the patient of what needs to be changed. This is analogous to the 4th-decile discussion in MI of the behavioral change plan that was associated with backpedaling in commitment strength prior to a final shift toward commitment among successful patients shown in Amrhein et al., 2003.
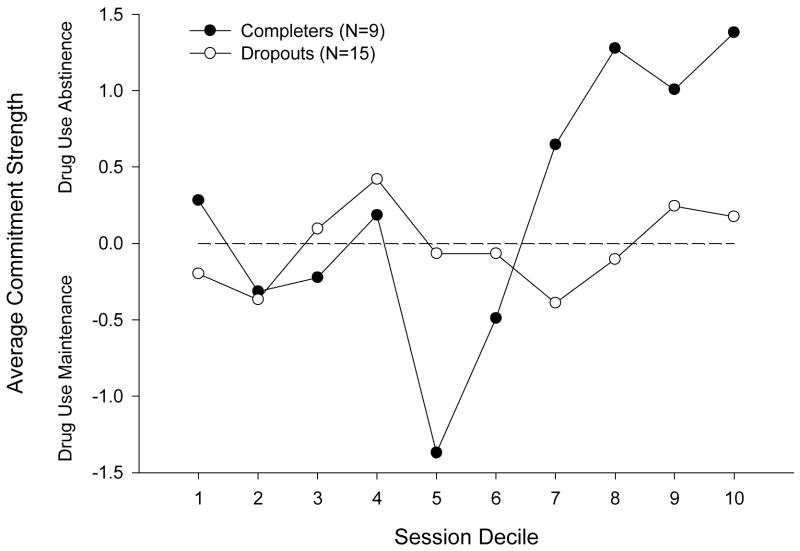
Treatment outcomes
The two main outcomes were retention in treatment and cocaine use. For analytic purposes, retention in treatment was defined as the total number of weeks patients participated in treatment out of the 12 weeks of the CBT-RP. For descriptive purposes (e.g., as in Figure 1), retention was defined as a binary variable, with completers defined as those completing at least 10 weeks of CBT-RP, and dropouts defined as all others. Drug use, the other indicator of treatment outcome, was defined as the proportion of negative urine samples (number of negative urine samples divided by the total number of urine samples collected). To define urine tests as positive or negative for cocaine, we used the standard NIDA cutoff for levels of cocaine metabolites (positive ≥ 300 ng/mL).
Figure 1.
The relations between commitment strength and retention in treatment
Data Analysis
Preliminary analyses included T-tests and Chi-square tests to verify that there were no significant differences between the completer (n=9) and dropout (n=15) groups on baseline demographic, depression, and drug use variables. These tests indicated that treatment completers and dropouts did not significantly differ in age, gender, race, marital status, years of drug use, method of cocaine use, baseline drug use frequency or education (p-values > 0.10).
The primary predictors for the main analyses were: 1) commitment strength, i.e., the mean across all session deciles, and 2) commitment shift: the difference between the midpoint (5th decile) to the session’s last decile. First, we calculated Pearson correlation coefficients to indicate the association between cognitive and commitment strength measures; the alpha for statistical significance was set at p<0.05. Normality was checked and to better meet normality assumptions, the raw scores for Perseverative Errors (PE) and Perseverative Responses (PR) were transformed to standard scores with a mean = 100 and standard deviation = 15; higher scores reflect lower PE and PR. Second, we regressed commitment strength measures on treatment outcome measures (retention and cocaine use) using linear regression. We first used unadjusted models, testing each of the two commitment strength variables as predictors of the two treatment outcome variables. We then conducted models controlling for sex, race (black vs. other), age (a three-level variable, coded as <29, 30–45, >45), and education (high school or more versus less than high school). Education and age were defined as categorical variables, using common and conceptually relevant definitions of the categories.
Results
Relationship between cognitive functioning and commitment language during CBT session
Cognitive functioning included attention, spatial processing, reaction time, accuracy of response, and general cognitive abilities. As shown in Table 1, cognitive functioning measured with the MC scales and the WCST was not significantly related to mean commitment strength. However, a statistically significant relationship was found between cognitive functioning and the shift towards greater commitment to change from the mid-point to the end of the treatment session. All scores on the WCST were significantly related to a shift towards greater commitment language from the mid-point to the end of the treatment session, as were three scores on the MC. These results suggest a relation between better cognitive executive abilities, such as mental flexibility, and abilities to produce greater shifts in commitment language.
Table 1.
Relationship between cognitive measures and commitment language
| 1. Commitment Strength: mean across all session deciles | 2. Commitment Strength: shift-midpoint to final session decilea | |
|---|---|---|
| Cognition Scores (MC) | ||
| Attention | −.04 | .59** |
| Abstract Reasoning | −.15 | .35 |
| Memory | −.08 | .15 |
| Spatial Processing | −.22 | .54** |
| Reaction Time | .03 | .57** |
| Accuracy | .10 | .46* |
| General Cognitive Function (GFC) | −.14 | .45* |
| Functional Cognitive Proficiency(FCP) | −.19 | .38 |
| Wisconsin Card Sort Test (WCST) | ||
| Perseverative Errors | .01 | .69** |
| Perseverative Responses | .00 | .65** |
| Categories Completed | .06 | .71** |
| Failure to Maintain Set | .04 | −.53** |
(10th Decile–5th Decile);
p < .01
p < .05, df=22
Association between Commitment Language Strength and treatment outcome
As shown in Table 2, mean commitment strength across deciles was unrelated to total weeks in CBT-RP, but was significantly related to proportion of negative urines. In contrast, shift from mid-session to the end of the session was significantly related to treatment retention (total weeks in treatment) but unrelated to the proportion of negative urines.
Table 2.
Linear regression of commitment strength on treatment outcome measure (N=24)
| Proportion Negative Urines | Weeks in treatment | |||
|---|---|---|---|---|
| Unadjusted β | Adjusted+β | Unadjusted β | Adjusted+β | |
| Commitment Language aspects | ||||
| Commitment Strength: mean across all session deciles | 19.61* (p=0.01) | 16.95* (p=0.01) | 0.48 (p=0.64) | 0.29 (p=0.73) |
| Commitment Strength: shift- midpoint to final session decilea | −0.87 (p=0.78) | −0.11 (p=0.97) | 0.80* (p=0.02) | 0.84* (p=0.001) |
Adjusted for age, sex, race, and education
p<0.05
Relations between commitment shift, cognition and treatment outcome
We found no significant correlation between weeks in treatment and proportion of negative urines during treatment (r=.34). Based on our previous findings on the association between impaired cognition and low retention (Aharonovich et al., 2006) we explored the associations of commitment language strength to the retention groups (dropouts and completers). Commitment language strength values were plotted by session decile, averaged over patients within the retention groups. Commitment strength below the dashed zero line indicates commitment toward continued drug use; commitment strength above this line indicates commitment toward change (i.e., reduced use). Means on or near the dashed “zero” line indicate a noncommittal stance or ambivalence. As Figure 1 illustrates, commitment strength hovered around the ambivalent level throughout the session for patients that dropped out of treatment. In contrast, for completers commitment strength shifted considerably across the deciles of the session. Analyses of the strength of commitment language expressed during the session revealed systematic commitment strength differences between the completers and dropouts. Overall, there was an increase in participants’ commitment strength over the course of the CBT session (F(9,198) = 2.87, MSe = 1.791, p < .005). However, dropouts did not shift significantly in their commitment strength across the session deciles (F(9,126) = .57, MSe = 1.809 p >.82). The variation of shifts in commitment strength from the noncommittal threshold was not statistically significant for the dropouts F(1,14) = .02, MSe = 4.914 p >.89 (see Figure 1). Thus, not only did the dropouts fail to exhibit a systematic pattern in commitment strength across their deciles, the level of this strength varied randomly from 0, i.e., the noncommittal level. In contrast, the completers produced significant variations in shift in their verbal expression of commitment strength across the session deciles. The first significant shift in strength was a drop in commitment expressed at mid session, the 5th decile (F(1,18) = 20.21, MSe=.836, p <.002,) followed by a significant increase in commitment statements toward and through the end of the session (across 7th through 10th deciles, F(1,8) = 10.28, MSe = 4.076, p < .02).
Discussion
The main findings of this study were significant associations between the three main variables: cognitive functioning, commitment language, and treatment outcome. Our results indicate that for the commitment strength predictor, only shifts in the strength of commitment statements during a cognitive behavioral treatment (CBT) session were positively and significantly related to participants’ baseline level of cognitive functioning. These shifts in commitment strength also significantly predicted treatment retention, although they were not significantly related to drug use during the treatment. At the same time, overall mean commitment levels throughout the session were predictive of reduction in drug use during cocaine dependence treatment. This is the first time these clinically relevant factors have been studied together in the same patients.
Our two hypotheses were partially supported by the findings. The first hypothesis concerned level of cognitive abilities and strength of commitment to change. Ability to making shifts in commitment strength was associated with mental flexibility as measured by the WCST, while commitment strength across deciles of the session was unrelated to cognitive abilities. The positive association between mental flexibility (WCST scores) and shifts in commitment during the session may reflect the dynamics of an engagement process. Conversely, rigidity and perseveration (reflecting lack of mental flexibility) may impede therapy by blocking a patient’s exploration of different options to reduce drug use, as well as hampering expressions of commitment to change.
Our second hypothesis concerned strength of commitment language and treatment outcome. The ability to make a commitment shift as indicated by the commitment strength scores predicted treatment retention. This suggests that the abilities for shifts or changes in commitment may positively interact with treatment engagement and eventually improve retention, although cognitive impairments may not negatively affect drug use outcome. The finding that overall mean commitment scores predicted decreased drug use, independent of cognitive abilities, suggests that patients entering the CBT session with strong, stable commitment to abstinence do reduce their drug use, regardless of their cognitive levels. Consistent with these results, another study of cocaine users showed that written endorsement of a strong commitment to abstinence predicted decreased risk for relapse to cocaine (Hall, Havassy and Wasserman, 1991) during 12 weeks of follow-up. However, Hall et al., 1991, did not assess the relationship of cognitive functioning to commitment strength and its changes, which was done in this report.
Among patients with more variable commitment (including ambivalence at the beginning of the session), better cognitive functioning and mental flexibly was important in producing such shifts towards commitment. Intuitively, these results are not surprising. To actively engage in the therapeutic process (which includes participating in a meaningful dialogue with the therapist) requires concentration and the ability to sustain attention, allowing for information encoding and processing, as well as mental flexibility to explore and move between new and different concepts. Impaired attention and cognitive rigidity may impede the therapeutic process, leading to frustration and eventually to dropout. Cognitive impairments in substance abusers have long been hypothesized to interfere with treatment processes, negatively impacting outcome (Aharonovich et al., 2006; Aharonovich et al., 2003; Horner, Harvey, & Denier, 1999; Becker & Jaffe, 1984). For these patients, with variable commitment, active engagement in the treatment process, indicated by their significant shift strength, was important in improving their retention in treatment, although reduction in drug use was not apparent by the end of the study. While we did not find a significant relationship between treatment retention and proportion of positive urines in this study, numerous previous studies showed positive associations between length of stay in cocaine use treatment and drug use outcome (e.g., Simpson et al., 1999) and if we had followed the patients for a longer period of time, such a relationships might have become apparent. In general, the longer patient retains in treatment, allowing time for the process to unfold, the greater the likelihood of better outcomes. A future study with post-treatment follow-up would allow investigation of whether better cognitive functioning, stronger commitment language and retention in treatment result in better abstinence for patients that were initially ambivalent at the beginning of treatment.
A limitation of the study is that the sample was not large enough for a multivariate mediational analysis, where we could investigate whether commitment variables would mediate the effects of cognitive functioning on treatment outcome. However, the present paper is important because the significant relationships found among the main variables support the need for a larger study that can address the issues in a more refined statistical analysis that can only be done with a larger sample.
Conclusion
This is the first study to examine patients’ verbal commitment to change, cognitive abilities and treatment outcome among drug dependent patients. Results indicate that while commitment to behavioral changes such as abstinence is not necessarily dependent on patient’s cognitive abilities, engagement in the process of the behavioral intervention (e.g., CBT), depends on cognitive abilities. Clinicians should not feel discouraged if a patient’s commitment language drops or starts to ‘back peddle” during a session, as this might indicate active engagement in the therapeutic process. Rather, clinicians should listen carefully to this language, and based on what they hear, assist the patient to express strong commitment statements as these were found to be good predictors of outcome. Future clinical studies need to further investigate the relations between cognition and verbal commitment to change and their differential contributions to treatment processes and outcome.
Acknowledgments
Support was provided by NIDA grants K23 DA016743; K02 DA000288; PI50 DA09236 and NIAAA grant K05 AA014223.
References
- Aharonovich E, Brooks A, Nunes E, Hasin D. Cognitive deficits in marijuana users: Effects on motivational enhancement therapy plus cognitive behavioral therapy treatment outcome. Drug and Alcohol Dependence. 2008;95:279–283. doi: 10.1016/j.drugalcdep.2008.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aharonovich E, Hasin DS, Brooks AC, Liu X, Bisaga A, Nunes EV. Cognitive deficits predict low treatment retention in cocaine dependent patients. Drug and Alcohol Dependence. 2006;81:313–322. doi: 10.1016/j.drugalcdep.2005.08.003. [DOI] [PubMed] [Google Scholar]
- Aharonovich E, Nunes E, Hasin D. Cognitive impairment, retention and abstinence among cocaine abusers in cognitive-behavioral treatment. Drug and Alcohol Dependence. 2003;71:207–211. doi: 10.1016/s0376-8716(03)00092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alterman AI, Holahan JM, Baughman TG, Michels S. Predictors of alcoholics’ acquisition of treatment-related knowledge. Journal of Substance Treatment. 1989;6:49–53. doi: 10.1016/0740-5472(89)90021-4. [DOI] [PubMed] [Google Scholar]
- Amrhein PC. How does motivational interviewing work? What client talk reveals. Journal of Cognitive Psychotherapy. 2004;184:323–336. [Google Scholar]
- Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. Journal of Consulting and Clinical Psychology. 2003;71:862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- Bates ME, Bowden SC, Barry D. Neurocognitive impairment associated with alcohol use disorders: implications for treatment. Experimental Clinical Psychopharmacology. 2002;10:193–212. doi: 10.1037//1064-1297.10.3.193. [DOI] [PubMed] [Google Scholar]
- Bates ME, Pawlak AP, Tonigan JS, Buckman JF. Cognitive impairment influences drinking outcome by altering therapeutic mechanisms of change. Psychology of Addictive Behaviors. 2006;20:241–253. doi: 10.1037/0893-164X.20.3.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker JT, Jaffe HH. Impaired memory for treatment-relevant information in inpatient men alcoholics. Journal of Studies on Alcohol. 1984;45:339–343. doi: 10.15288/jsa.1984.45.339. [DOI] [PubMed] [Google Scholar]
- Blume AW, Schmaling KB, Marlatt GA. Memory, executive cognitive function, and readiness to change drinking behavior. Addictive Behaviors. 2005;30:301–314. doi: 10.1016/j.addbeh.2004.05.019. [DOI] [PubMed] [Google Scholar]
- Carroll KM. A Cognitive-Behavioral Approach: Treating Cocaine Addiction. Therapy manuals for drug addiction. Rockville, MD: National Institute of Drug Abuse; 1998. [Google Scholar]
- Fals-Stewart W. Neurocognitive defects and their impact on substance abuse treatment. Journal of Addiction and Offender Counseling. 1993;13:46–57. [Google Scholar]
- Fals-Stewart W, Shafer J. The relationship between length of stay in drug-free therapeutic communities and neurocognitive functioning. Journal of Clinical Psychology. 1992;48:539–543. doi: 10.1002/1097-4679(199207)48:4<539::aid-jclp2270480416>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis Disorders--Patient Edition. New York: New York State Psychiatric Institute; 1997. [Google Scholar]
- Hall SM, Havassy BE, Wasserman DA. Effects of commitment to abstinence, positive moods, stress and comping on relapse to cocaine use. Journal of Consulting Clinical Psychology. 1991;59:526–532. doi: 10.1037//0022-006x.59.4.526. [DOI] [PubMed] [Google Scholar]
- Heaton RK. Wisconsin Card Sorting Test: Computer Version 3 for Windows-Research Edition. Odessa, FL: Psychological Assessment Resources, Inc; 1999. [Google Scholar]
- Horner MD. Attentional functioning in abstinent cocaine abusers. Drug and Alcohol Dependence. 1999;54:19–33. doi: 10.1016/s0376-8716(98)00141-0. [DOI] [PubMed] [Google Scholar]
- Horner MD, Harvey RT, Denier CA. Self-report and objective measures of cognitive deficit in patients entering substance abuse treatment. Psychiatry Research. 1999;86:155–161. doi: 10.1016/s0165-1781(99)00031-1. [DOI] [PubMed] [Google Scholar]
- McCrady BS, Smith DE. Implications of cognitive impairment for the treatment of alcoholism. Alcoholism Clinical and Experimental Research. 1986;10:145–149. doi: 10.1111/j.1530-0277.1986.tb05061.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People To Change Addictive Behavior. New York: Guilford Press; 1991. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2. New York: The Guilford Press; 2002. [Google Scholar]
- Moyers TB, Martin T, Christopher PJ, Houck JM, Tonigan S, Amrhein PC. Client Language as a Mediator of Motivational Interviewing Efficacy: Where Is the Evidence? Alcoholism: Clinical and Experimental Research. 2007;31:40s–47s. doi: 10.1111/j.1530-0277.2007.00492.x. [DOI] [PubMed] [Google Scholar]
- Powell DH, Kaplan EF, Whitla D, Catlin R, Funkenstein HH. MicroCog: Assessment of Cognitive Functioning Version 2.1. San Antonio, TX: The Psychological Corporation; 1993. [Google Scholar]
- Roehrich L, Goldman MS. Experience-dependent neuropsychological recovery and the treatment of alcoholism. Journal of Consulting and Clinical Psychology. 1993;61:812–821. doi: 10.1037//0022-006x.61.5.812. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Fletcher BW, Hubbard RL, Anglin MD. A national evaluation of treatment outcomes for cocaine dependence. Archives of General Psychiatry. 1999;56:507–514. doi: 10.1001/archpsyc.56.6.507. [DOI] [PubMed] [Google Scholar]
- Teichner G, Horner MD, Roitzsch JC, Herron J, Thevos A. Substance abuse treatment outcomes for cognitively impaired and intact outpatients. Addictive Behaviors. 2002;27:751–763. doi: 10.1016/s0306-4603(01)00207-6. [DOI] [PubMed] [Google Scholar]