Abstract
The Massachusetts eHealth Collaborative (MAeHC) was formed to improve patient safety and quality of care by promoting the use of health information technology through community-based implementation of electronic health records (EHRs) and health information exchange. The Collaborative has recently implemented EHRs in a diverse set of competitively selected communities, encompassing nearly 500 physicians serving over 500,000 patients. Targeting both EHR implementation and health information exchange at the community level has identified numerous challenges and strategies for overcoming them. This article describes the formation and implementation phases of the Collaborative, focusing on barriers identified, lessons learned, and policy issues.
Introduction
Health information technology (HIT) offers an opportunity to improve health care, with the potential to reduce cost and enhance quality, safety, and efficiency. 1,2 To realize this promise, there is growing consensus of the need for large-scale adoption of electronic health records (EHRs) and clinical data exchange. 3 Beginning with pioneering efforts in Santa Barbara 4 and Indiana, 5 more than 250 regions across the country have formed collaborative regional health information organizations (RHIOs) to promote implementation of EHRs and initiation of clinical data exchange. 6 Despite initial enthusiasm, progress has been impeded by challenges ranging from shortages of capital and lack of technical standards to the burdens of converting paper records and concerns about privacy and confidentiality. 3,7–9
To address these issues, Massachusetts health care stakeholders formed a coalition and pooled their resources to pursue community-wide EHR implementation in 3 Massachusetts communities. This report describes the collaborative effort, barriers identified, and lessons learned, and also discusses the policy implications. (For a glossary of key terms, see Appendix 1, available as a JAMIA online-only data supplement at http://www.jamia.org.)
Establishing a Collaborative
The effort originated with the Massachusetts Chapter of the American College of Physicians (MA ACP), which in Fall 2003 designated quality and safety as programmatic priorities. Consultations with experts on patient safety led MA ACP to conclude that promotion of large-scale EHR adoption offered the best approach to promoting quality and safety in clinical practice. With the help of a nationally respected academic HIT research group, 10 a business plan for such an initiative was developed. The plan was presented at a summit of the state's health care stakeholders in March 2004, hosted by MA ACP to explore the collective will for concerted action. The meeting, attended by over 30 of the state's health care leaders, resulted in consensus to explore working collaboratively toward accelerated EHR implementation.
Concurrently, similar discussions about quality and safety were taking place among executives of the state's largest private insurer (Blue Cross Blue Shield of Massachusetts [BCBSMA]). On the recommendation of the state's Secretary of Health and Human Services, BCBSMA responded to the MA ACP challenge for collective action with a pledge of $50M to support a collaborative initiative on an “if you build it successfully we will fund it” basis. The money was designated to establish an all-stakeholder organization that would implement 3 fully funded community-wide EHR demonstration projects across Massachusetts over 3 years. (For more on the motivations of BCBSMA, see Appendix 2, available as a JAMIA online-only data supplement at http://www.jamia.org.)
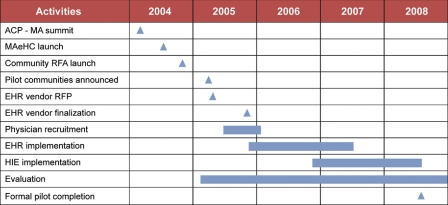
Early meetings of the coalition consolidated the consensus, welcomed additional stakeholder organizations, and formulated an interim organizational structure. Working groups in important functional areas were established, including organizational structure, financing, technical specifications, community implementation, and evaluation. Each was chaired by a stakeholder leader specifically skilled in the area of concentration and charged with formulating specific recommendations. An ambitious time line was set (▶).
Figure 1.
Massachusetts eHealth Collaborative (MAeHC) timeline. ACP = American College of Physicians; EHR = electronic health record; HIE = health information exchange; RFA = request for applications; RFP = request for proposals.
Time and effort were donated by members according to organizational abilities and resources. Specific financial contributions were not required, but there was an expectation of contributions in kind. Members donated office space, information technology support, and legal and business planning services. An Agreement to Participate was drawn up, asking for commitments to: (1) state-wide EHR implementation through collective action, (2) formation of a collaborative organization to carry out the mission, and (3) a cooperative, mission-driven ethic. All participants signed on as founding members (▶). This was followed by release of the first dollars from BCBSMA to support the Collaborative's formal filing for incorporation with the State of Massachusetts as the Massachusetts eHealth Collaborative (MAeHC).
Table 1.
Table 1 Members of the Massachusetts eHealth Collaborative
| Hospitals, Community Health Centers, Integrated Health Care Systems |
|
| Governmental Agencies |
|
| Health Plans and Payer Organizations |
|
| Healthcare Purchaser Organizations |
|
| Non-Voting Members |
|
| Healthcare Professional Associations |
|
| Consumer, Public Interest, and At-Large |
|
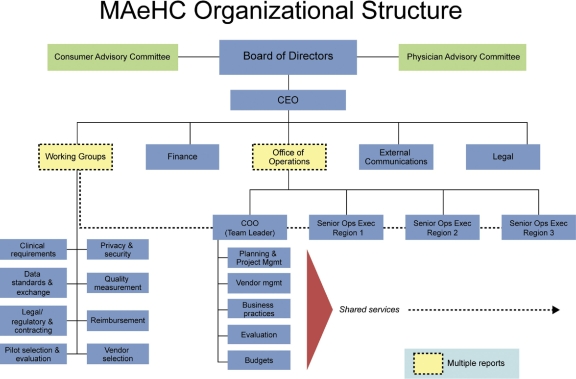
A formal organizational structure was defined (▶). Board seats were assigned to each signatory organization and an executive committee was formed, with representation from each sector of the health care community. In recognition of the importance of physician leadership to the initiative, a physician was elected chair of the MAeHC, followed by the hiring of a nonphysician chief executive officer with experience in clinical data exchange and a chief operating officer physician executive on loan from BCBSMA.
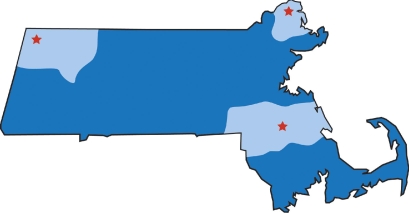
Figure 2.
The 3 communities of the Massachusetts e-Health Collaborative demonstration program.
Initial Actions and Selection of Participating Communities
After incorporation, the board endorsed a strategy of fully funding a limited number of community-wide demonstration projects to concentrate effort, encourage clinical data exchange, facilitate evaluation, and generate potentially important data and experience relevant to large-scale EHR adoption. A Request for Applications was developed and issued to communities throughout the state. 11 The Request for Applications defined “community” broadly (including the “community” of practices relating to one or more local hospitals) and included requirements to recruit at least 80% of community practices, and obtain the participation of the local hospital, other community health facilities, and local leadership (▶). In addition, communities had to establish an organizational structure, designate a local project leader, and commit resources toward implementation. Selection criteria emphasized local physician and community leadership to ensure participation and a coordinated effort.
Table 2.
Table 2 Community Selection ∗
| Description requested of communities |
| Breadth and depth of provider network |
| Organization and commitment of community and stakeholders |
| Description of ongoing participation in other activities |
| Selection criteria |
| A high percentage of each patient's care being done within the applicant community |
| Demonstration of support, commitment, and leadership by health care professionals, health care institutions, and the community at large |
| Existing or planned engagement in electronic health record and/or other technologies supportive of the Collaborative's objectives |
∗ Full description available at www.maehc.org.
Thirty-five of 55 potentially eligible communities in the state submitted first-round applications; 6 were selected as finalists and underwent a second more detailed round that included site visits and town meetings with selection committee members. Three communities (North Adams/Williamstown, Brockton, and Newburyport) were selected as demonstration sites in March 2005, just 12 months after the original summit meeting. All accepted the invitation to proceed.
Establishing Technical Standards and Conducting Vendor Selection
To facilitate EHR selection by communities and practices and encourage best offerings from vendors, a technical standards/vendor selection working group was formed. The working group established 2 key precepts: (1) identify a practical number of qualified vendors from the more than 200 available, and (2) give physicians choices in selection of vendor for their practice. Technical standards were specified to facilitate clinical data exchange, quality/safety initiatives, and evaluation. 12 These included standardized representation of key data, such as use of the Systematized Nomenclature of Medicine (SNOMED) and the International Classification of Diseases (ICD-9-CM).
System features assessed by the working group included user friendliness, functionality, clinical decision support capability, interoperability, security, reliability, and affordability (▶). Over 20 vendors responded to the selection committee's request for proposals, and 7 were eventually chosen and recommended to the 3 pilot communities. The selected vendors held community fairs and conducted other informational activities to enable practices to choose the systems and companies best suited to their needs.
Table 3.
Table 3 Vendor Request for Proposals—Key Areas Covered
| Corporate Background | Reason for Focus on Item |
|---|---|
| Company information, financial information, Massachusetts installations, client references | Intended to ensure that companies selected would be those with strong track records, which would be likely to remain in business |
| Product information | |
| Current product offering, products in development, product development | Life cycle for these products is short |
| Software requirements | To ensure compatibility with existing systems |
| Technical requirements | To ensure compatibility with existing systems and to budget for potential postimplementation expenses |
| Hardware platform, software platform, client devices supported | To ensure compatibility with existing systems and to budget for potential postimplementation expenses |
| Integration and interface requirements | To ensure compatibility with existing systems and to budget for potential postimplementation expenses |
| Integration checklist, exchange standards checklist | Key aim of collaborative is to enable clinical data exchange, extraction of quality data |
| Implementation requirements | To avoid any hidden costs associated with implementation or maintenance |
| HIPAA Standards | To ensure patient privacy and security |
| Pricing | Key aim of the collaborative is to obtain good prices for providers |
HIPAA = Health Insurance Portability and Accountability Act.
Contracting
Once incorporated, the Collaborative moved from donated legal services to retaining independent legal counsel to support the conduct of its business, particularly for contracting, both with vendors and communities. Hundreds of hours were required for crafting and negotiating the contracts for communities and practices. Goals were to ensure proper participation by practices and hospitals (e.g., to comply with data protection rules and reporting requirements) while providing the necessary legal protections that would facilitate participation. Two of the 3 communities and some individual practices retained their own counsel to collectively review the contracts for participating practices and ensure that liability and financial responsibilities were reasonable.
Contracting with vendors was more routine. Negotiations focused on obtaining the best terms for service, price, reliability, and customer responsiveness. The Collaborative performed these negotiations for all participating communities, enabling the latter to simply choose the vendor(s) that best met their specific needs and not have to spend time and effort in vendor selection and contracting, which can be problematic for most practices. 13
Evaluation
Because it is a demonstration project, the MAeHC initiative received detailed evaluation. Coalition experts developed an evaluation plan that specified 6 areas of study: (1) use of technology, (2) barriers to and facilitators of adoption, (3) implementation tactics, (4) impact on safety (e.g., medication errors), (5) impact on quality, and (6) economic issues. The evaluation proposal was approved and budgeted at $3.5M (nearly 7% of the project's total expenses). Grant support was obtained, offsetting about 40% of the expense. Evaluation methods include automated record reviews, manual chart reviews, and questionnaires.
Finalizing Plans with Practices and Establishing Confidentiality/Security Standards
Each prospective practice completed a detailed survey and underwent a site visit by project staff to help plan EHR implementation. The Collaborative assembled a team of individuals with expertise in practice organization and information technology to perform the initial consultative site visits and to subsequently work with practices in converting to electronic records and reorganizing workflow and operations.
Data security practices and privacy/confidentiality standards were developed through a process of extensive discussion and debate both within the Collaborative and with the communities. The sensitive issue of patient control over data exchange was resolved by implementing an “opt in” model, in which patients are specifically asked to agree to as-needed electronic exchange of their clinical data between clinical sites (no permission is sought to have data stored in the practice's EHR).
Contract language with each community was drawn up, and individual practices formally signed on to the project, committing to: (1) full conversion from paper records to EHRs, (2) full participation in all evaluation and community data-sharing activities, and (3) upholding data-security and privacy standards. In return, full funding of their office EHR purchase, implementation, and operations (exclusive of practice staff time and opportunity costs) was guaranteed through June 2008 (with all necessary upgrades and technical support).
Current Status: Recruitment, Adoption, Implementation, and “Opting In” by Patients
Physician recruitment and retention have been strong. Of 561 physicians in 167 practices originally invited to participate in the program, 548 (98%) physicians in 159 (95%) practices accepted the offer. Since accepting the offer, 53 physicians in 18 practices have withdrawn from the program, leaving 141 participating practices, yielding an overall participation rate of 84% of all physicians and 88% of all practices in the pilot communities. Offsetting these withdrawals, approximately 75 physicians have joined the program since the recruitment effort, mostly through organic growth of practices already participating in the project. The main reasons for withdrawal from the project were: (1) EHR provided through another program, (2) dissatisfaction with choice of EHR vendors, (3) EHR not suited to their specialty, and (4) in one instance, physician death.
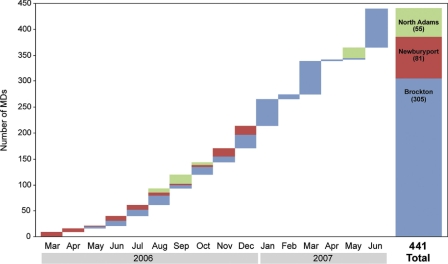
Implementation has been nearly complete (▶). Of the 141 initially participating practices, 138 (98%) have fully implemented their EHR as of September 2008. One of the remaining practices is scheduled to “go live” in November 2008; 2 practices have failed implementation. Early data show that levels of provider utilization of key functionalities such as electronic prescribing are very high. Duration of time to implementation has ranged from 4 months to 9 months, with 4 months being typical for a small office practice (1 month of preparation work and 3 months of work with the vendor).
Figure 4.
Distribution of practices and adoption rates among the 3 communities as of July 1, 2007.
The approach to clinical data exchange has varied by community, ranging from all providers electing to use the same vendor (making data exchange technically easier) to use of a central architecture by multiple vendors. In the first community to “go live,” 94% of patients are “opting in” for clinical data exchange.
Budget and Resources
The overall budget for the MAeHC collaborative and its pilot programs is approximately $50 million, with the greatest proportion (approximately 42%) allocated to purchase and implementation of EHRs in the offices of the 495 physicians. About 11% was dedicated to clinical data exchange. Program staff and direct overhead expenses were limited to approximately 21% of the total budget, although the preponderance of personnel effort was dedicated to on-site support of the participating practices. Legal fees accounted for 5% of the budget. There has been no strict accounting of the enormous amount of time and other in-kind contributions by member organizations since project inception, but estimated economic value likely totals in the hundreds of thousands of dollars, given the thousands of hours of work donated by highly skilled professionals.
Discussion
The MAeHC's demonstration effort achieved widespread adoption of EHRs in 3 Massachusetts communities. Adoption rates in excess of 90% are rare in the United States except in integrated delivery systems. 14 This effort helped identify and highlight factors essential to successful large-scale EHR adoption as well as underscore important barriers.
Factors Essential to Large-scale EHR Adoption
Factors essential to this initial success included strong financial backing, intensive practice support, commitment to collective action, clear goals, leadership from the physician community, governmental support, and a community-based focus.
Financial underwriting from the Massachusetts nonprofit payer community (i.e., BCBSMA) was critical to the high rates of adoption and implementation. The challenge of “you build it, we'll fund it” derived from enlightened self-interest and realization on the part of BCBSMA that the financial return from an interoperable EHR with decision support and clinical data exchange could be substantial if efficiency is improved, waste reduced, and health outcomes improved. 3 Absent the availability of financial resources from the payer community and the willingness to expend them, funding EHR adoption becomes much more problematic, especially for small primary care practices that do not have the necessary capital. Payment reform will be essential to widespread EHR adoption.
Moving more rapidly to large-scale EHR adoption requires that those who will benefit most financially (i.e., payers and purchasers 15 ) put up the necessary capital, either directly or through enhanced reimbursement. Most small- to medium-sized practices, especially those delivering primary care, find themselves unable to afford electronic medical records and may not derive much return from any such investment. 8,13 Since the bulk of patient care in the United States is delivered by such practices, their lack of funding contributes to the United States lagging far behind most other industrialized nations in EHR implementation. 10 The “skin-in-the-game” argument for substantial physician investment ignores the major costs in time and effort that even a “free” EHR implementation program such as this one entails.
Practice support emerged as an essential ingredient. Conversion from paper to electronic records represents a fundamental change in practice organization and operation. For smaller practices, such transformation can be nearly impossible without external support. Setting up a team of practice operation facilitators to work with individual practices proved essential, as did having continued information technology support. Support was provided at all phases, from planning the implementation and redesigning the workflow, through installation and training, and with ongoing support. This model acknowledges an important potential pitfall: divorcing system implementation from workflow design can lead to adoption failure. Budgeting for such support needs to be generous—typically about one-third of total expenses. Only one practice failed implementation in the MAeHC (<1% rate), while the failure rate with typical vendor implementations anecdotally approaches 33%. 16
Collective/collaborative action also proved critical. From the outset, all members of the health care community were welcomed, based on the view that the proposed mission required a pooling of resources and the active participation of all stakeholders. This imparted to the project a mission-focused ethic and culture that transcended any particular organization and encouraged contributions of necessary financial resources, expertise, and political support. It also promoted efficient, effective utilization of scarce resources and helped leverage and focus the enormous capabilities and talent scattered throughout the state. In tapping collectively into the aspirations of individuals and organizations in the health care community, the project provided opportunities to carry out ideas on a large scale and encouraged much pro bono work and many in-kind contributions. Organizing on a larger scale also facilitated contracting and minimized the financial and operational risks to individual practices, many of which cannot otherwise afford to convert to EHRs. The Massachusetts HIT community has an especially robust history of such collaborative work. 17–20
A collaborative approach and consistent vision for HIT also facilitated implementing quality, safety, and efficiency measures such as decision-support, clinical data exchange, and standards for confidentiality and privacy. The HIT vision of this project derives from available evidence suggesting that EHRs need to be coupled to decision-support tools and clinical data exchange to realize desired health outcomes and adequate return on investment. 2,3,13
Another central feature of this HIT initiative was physician leadership. The project originated with a medical professional organization (MA ACP) interested in promoting the quality and safety of medical care. The Collaborative called upon recognized physician leaders and experts in quality and safety to help set the agenda and facilitate the process. Such leadership underscores the message that health care quality and safety are recognized responsibilities and valued missions of the medical profession. By taking the lead, the physician community can seize the opportunity to effect constructive change.
Governmental support also played a pivotal role. Even though no state or federal funding was sought for this demonstration project, efforts by local, state, and federal officials helped bring parties together, encouraged community participation, and allayed public privacy and confidentiality concerns; in addition, they sponsored legislation to promote standards and adoption of EHRs in clinical practice; EHR adoption can be a win-win proposition for all, as evidenced by the project's bipartisan political support.
An unexpected benefit was community building. At the local level, community organizing efforts sprang up, stimulated by the application process and later proving instrumental to collective decision making, clinical data exchange, and privacy/confidentiality agreements. We learned that if the entire community is not engaged, individual physicians/practices will implement EHRs without regard to what their “trading partners” (i.e., hospitals, referring network, etc.) are doing and thereby forego an opportunity for shared social benefit. “Community” appears to be a highly effective unit of intervention for EHR implementation.
Important Barriers
Several major impediments were encountered, including inadequate standards for data representation and vocabulary, concerns about vendor instability and system obsolescence, system limitations, privacy and security issues, contracting demands, and practice inertia. The lack of universal standards for vocabulary and data representation poses a major impediment to data sharing and interoperability. Multiple vocabularies exist across health care entities, complicating the exchange of health information between providers. The problem is well recognized, 8 and the Collaborative asked all vendors to adhere to basic existing standards for data representation and vocabulary. Nonetheless, the magnitude of the problem proved greater than expected and necessitated considerable time and resources to ensure that individual systems adequately communicated with each other.
Despite extremely positive national activity in the areas of vender certification and systems standards (e.g., the Certification Commission for Healthcare Information Technology and the Health Information Technology Standards Panel), 20 the current rudimentary state of standards means that they are still insufficiently specific for routine everyday use by practices and communities, especially in regard to ensuring interoperability and ease of use in reviews for quality of care. Absent additional major progress in the nation's approach to EHR standards, any community attempting to establish interoperability among competing vendor systems will need to commit considerable technical and organizational effort to achieve even rudimentary clinical data exchange.
A dynamic business climate and rapid technology change are important factors making practices reluctant to commit to EHR systems, fearing they may be left stranded with an obsolete system. Many vendors are start-up companies; others are large companies with varying degrees of commitment to EHR development and support. To help mitigate risk to the practices, the Collaborative vetted vendors for corporate commitment and financial stability and wrote into contracts the need to adhere to basic interoperability standards that would enable transfer of data to a vendor's new system or to a new vendor's system.
Despite careful vetting, system limitations often became evident. Some systems failed to meet expectations, necessitating considerable system modification to establish required functionalities, sometimes at the expense of the Collaborative; in some instances the expected functionality has not yet been delivered. Those undertaking large-scale HIT adoption need to demand from prospective vendors evidence of ability to meet technical specifications and have project and technical managers with the expertise, experience, and diligence to ensure that vendors live up to these requirements.
Privacy and security concerns represent another challenge, especially important to effecting clinical data exchange. As noted, the community approach has been extremely valuable in helping to elicit privacy concerns and implement local solutions that ensure the security of patient data. Details of the privacy/confidentiality solutions worked out by communities are beyond the scope of this article, but “opting in” by patients was selected by communities as the preferred approach and was highly effective.
Contracting costs and efforts can be formidable. The real cost of contracting lay in the enormous amount of time required to negotiate and finalize contracts with the large number of project participants. Initial plans did not adequately account for the necessary time. The Collaborative spent approximately 5% ($2M) on contracting and associated legal services. The contracting agenda included practice and vendor contracts; privacy and security practice rules for individual practices, community data exchange, and data warehousing; research contracts; institutional review board management; and patient consent and education (over 500,000 patients). No organization that we are aware of has undertaken such a broad set of technical, organizational, legal, and social issues in this area on such a large scale; limiting legal expenses to less than 5% of budget has required diligence and close oversight.
Even with financial backing and practice support, practices frequently attempted to delay their “go live” dates. While no specific pattern emerged, there simply seems to be no good time to undergo practice transformation; it is common for physicians and practices to delay the pain of transition as long as possible. Nonetheless, the project will have implemented EHRs for over 500 physicians in 200 locations across 3 communities in a span of 21 months, a feat that clearly could not have been accomplished without the financial, operational, legal, and political support provided by the Collaborative.
Policy Implications
We believe that policies that enable community efforts such as this one may be beneficial. However, this collaborative had a number of components that may be difficult to achieve elsewhere, most notably a major financial commitment by the payer community. If such efforts are to be successful, it will be important for regional and local government to play a convening role.
Payment reform that rewards providers for either adopting electronic records, improving quality, or even reporting quality data on a regular basis would be expected to have a major catalytic impact if the incentives are sufficient, 8 and Medicare's recent steps along these lines represent a step in the right direction, albeit a small one. 21 Electronic health records represent a key piece of infrastructure for the patient-centered medical home, so that payment reform that supports this approach should be complementary. 22 Programs that target physician adoption should include not only support for purchasing hardware and software, but also enable practice support, or they are likely to be associated with high failure rates. The standards in use need additional refinement and vetting, and the conformance testing that is now being taken on by Certification Commission for Healthcare Information Technology is absolutely essential in this evolution and deserves public support. 20 Finally, the government may need to play a role in enabling the sharing of clinical decision support, as the full value of electronic records is unlikely to be achieved in the near term if it is not available. 23
Conclusion
The Collaborative's long-range goal is to expand EHR adoption to the rest of the state and link community data exchanges to a statewide exchange system. Discussions are underway with all of the key stakeholders to develop a business model to support widespread EHR adoption. Contribution of capital for the initial investment is being proposed on a “fair share” basis, according to expected financial return for individual parties.
Development of this collaborative represents one approach to accelerating implementation of HIT, with potential benefits in quality, safety, and efficiency. Although substantial early progress has been realized, the organization is still young, and the benefits still need to be demonstrated. Nonetheless, the barriers encountered and strategies to overcome them should be applicable to others considering similar initiatives. (▶).
Figure 3.
Organizational structure of the Massachusetts eHealth Collaborative. CEO = chief executive officer; COO = chief operating officer; MAeHC = Massachusetts eHealth Collaborative.
References
- 1.Johnston D, Pan E, Middleton B. Finding the values in healthcare information technologieshttp://www.citl.org/findingTheValue.pdfAccessed June 11, 2008.
- 2.Hillestad R, Bigelow JH. Health information technology: can HIT lower costs and improve quality?http://rand.org/pubs/research_briefs/RB9136/RAND_RB9136.pdfAccessed June 11, 2008.
- 3.Walker J, Pan E, Johnston D, Adler-Milstein J, Bates DW, Middleton B. The value of health care information exchange and interoperability Health Aff (Millwood) 2005. Suppl Web Exclusives:W5-10-W5-18. [DOI] [PubMed]
- 4.California HealthCare Foundation The Santa Barbara County care data exchangehttp://www.chcf.org/documents/ihealth/SantaBarbarafsweb.pdf 2005. Accessed June 11, 2008.
- 5.IHIE Indiana health information exchangehttp://www.ihie.com/ 2005. Accessed June 11, 2008.
- 6.eHealth Initiative Description of eHealth Initiative's programshttp://www.ehealthinitiative.org/initiatives/programs/ 2005. Accessed June 11, 2008.
- 7.Miller RH, West C, Brown TM, Sim I, Ganchoff C. The value of electronic health records in solo or small group practices Health Aff (Millwood) 2005;24:11277. [DOI] [PubMed] [Google Scholar]
- 8.Bates DW. Physicians and ambulatory electronic health records Health Aff (Millwood) 2005;24:1180-1189. [DOI] [PubMed] [Google Scholar]
- 9.Kaushal R, Bates DW, Poon EG, Jha AK, Blumenthal D. Functional gaps in attaining a national health information network Health Aff (Millwood) 2005;24:1281-1289. [DOI] [PubMed] [Google Scholar]
- 10.Bates DW, Ebell M, Gotlieb E, Zapp J, Mullins HC. A proposal for electronic medical records in U.S. primary care J Am Med Inform Assoc 2003;10:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Massachusetts eHealth Collaborative Expanding the use of electronic health records and establishing a regional health information infrastructure in Massachusetts. Request for applications. http://www.maehc.org/documents/MAeHCRequestforApplications-6Dec04_000.pdf 2003. Accessed June 11, 2008.
- 12.Massachusetts eHealth Collaborative Electronic health record. Request for proposal. http://www.maehc.org/documents/MAeHC_EHR_RFP_000.pdf 2003. Accessed June 11, 2008.
- 13.Simon SR, Kaushal R, Cleary PD, et al. Correlates of electronic health record adoption in office practices: a statewide survey J Am Med Inform Assoc 2007;14:110-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jha AK, Ferris TG, Donelan K, et al. How common are electronic health records in the United States?. A summary of the evidence. Health Aff (Millwood) 2006;25:w496-w507. [DOI] [PubMed] [Google Scholar]
- 15.Wang SJ, Middleton B, Prosser LA, et al. A cost-benefit analysis of electronic medical records in primary care Am J Med 2003;114:397-403. [DOI] [PubMed] [Google Scholar]
- 16.Connolly C. Cedars-Sinai doctors cling to pen and paperhttp://www.washingtonpost.com/wp-dyn/articles/A52384-2005Mar20.html 2003. Accessed June 11, 2008.
- 17.Glaser JP, DeBor G, Stuntz L. The New England Healthcare EDI Network J Healthc Inf Manag 2003;17:42-50. [PubMed] [Google Scholar]
- 18.Halamka J, Aranow M, Ascenzo C, et al. Health care IT collaboration in Massachusetts: the experience of creating regional connectivity J Am Med Inform Assoc 2005;12:596-601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Center for Information Technology Leadership HIEI: Healthcare information exchange and interoperabilityhttp://www.citl.org/research/HIEI.htm 2005. Accessed June 11, 2008.
- 20. Certification Commission for Healthcare Information Technologyhttp://www.cchit.org/ 2005. Accessed June 11, 2008.
- 21.Centers for Medicare and Medicaid Services Physician Quality Reporting Initiative Overviewhttp://www.cms.hhs.gov/pqri/ 2005. Accessed June 11, 2008.
- 22.Goroll AH, Berenson RA, Schoenbaum SC, Gardner LB. Fundamental reform of payment for adult primary care: comprehensive payment for comprehensive care J Gen Intern Med 2007;22:410-415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Osheroff JA, Teich JM, Middleton B, Steen EB, Wright A, Detmer DE. A roadmap for national action on clinical decision support J Am Med Inform Assoc 2007;14:141-145. [DOI] [PMC free article] [PubMed] [Google Scholar]