Abstract
As the HIV epidemic has evolved to become a chronic, treatable condition the focus of HIV care has shifted from the inpatient to the outpatient arena. The optimal structure of HIV care in the outpatient setting is unknown. Using the HIV Research Network (HIVRN), a federally sponsored consortium of 21 sites that provide care to HIV-infected individuals, this study attempted to: (1) document key features of the organization of care in HIVRN adult clinics and (2) estimate variability among clinics in these parameters. A cross-sectional survey of adult clinic directors regarding patient volume, follow-up care, provider characteristics, acute patient care issues, wait times, patient safety procedures, and prophylaxis practices was conducted from July to December 2007. All 15 adult HIVRN clinic sites responded: 9 academic and 6 community-based. The results demonstrate variability in key practice parameters. Median (range) of selected practice characteristics were: (1) annual patient panel size, 1300 (355–5600); (2) appointment no-show rate, 28% (8%–40%); (3) annual loss to follow-up, 15% (5%–25%); (4) wait time for new appointments, 5 days (0.5–22.5), and follow-up appointment, 8 days (0–30). The majority of clinics had an internal mechanism to handle acute patient care issues and provide a number of onsite consultative services. Nurse practitioners and physician assistants were highly utilized. These data will facilitate improvements in chronic care management of persons living with HIV.
Introduction
Highly active antiretroviral theraphy (HAART) has significantly altered the management of HIV infection in the United States. Since its introduction in late 1995, there has been a marked decrease in morbidity due to opportunistic infections, mortality, and hospitalization rates.1–4 Health care expenditures have also shifted from inpatient services to pharmaceuticals and outpatient care.5–8 HIV infection has been transformed from a terminal illness to a chronic disease.9
Experience in the management of HIV infection has been shown to improve clinical outcomes in the outpatient setting.10 While debate still exists on what makes a physician qualified to treat HIV-infected patients, many believe it is a combination of patient experience and continual medical education in HIV care.11 Clinics treating high volumes of HIV-infected patients are more likely to comply with Public Health Services guidelines, including appropriate prophylaxis administration, coinfection testing, and timely measurement of CD4 count and HIV-1 viral load, than clinics with smaller volumes (<100 patients).12 Similar trends have not been experienced in the inpatient setting, with a recent study showing little difference in patient mortality and quality of care outcomes among hosptialist and non-hospitalist physicians.13
The Donabedian structure-process-outcome (SPO) model is a method widely used to assess health care quality. Structure is the materials, human resources, and organizational characteristics utilized in providing health care.14 Processes of care are practitioner-led medical interventions, which include prevention, diagnosis, and treatment of diseases.14 The desired result of these processes of care defines outcome in the SPO model.14
There is little descriptive documentation of the structures of medical care delivered by clinics treating high volumes of HIV-infected patients in the United States. As HIV care becomes increasingly grounded in the outpatient arena and management complicated by expanding therapeutic options, adverse drug reactions, and long-term complications of HIV infection, an understanding of the structures of outpatient HIV care emerges as an important aspect in addressing patient safety and quality of care. Our study aimed at documenting key organizational features of medical care delivered in high volume HIV clinics, with the intent of improving organizational structure and quality of care in outpatient HIV clinics.
Methods
Study design and participants
We conducted a cross-sectional survey of medical directors of adult HIV Research Network (HIVRN) clinics. The HIVRN is a consortium of 21 sites that provide primary and subspecialty care to HIV-infected individuals in 14 cities throughout the United States. It is sponsored by the Agency for Healthcare Research and Quality (AHRQ), Health Resources and Services Administration (HRSA), HIV/AIDS Bureau (HAB), Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment (SAMHSA/CSAT), and Office of AIDS Research, National Institutes of Health (OAR/NIH).
Fifteen HIVRN clinics treat adult (18 years or older) patients. The participating sites are located in the Eastern (5), Midwestern (3), Southern (3), and Western (3) United States. Nine sites have academic affiliation; 6 are community-based.
Data collection
A structured questionnaire was sent to all adult HIVRN medical directors in July 2007 and data were collected from July to December 2007. Medical directors were instructed to answer each question using objective clinical data and to use best estimates if clinical information was not available. After all questionnaires were received and information compiled, a summary worksheet was sent to each medical director to review for accuracy. The survey contained 84 items covering 7 domains. Forty-seven items required a numerical answer, 26 were yes–no questions, and 11 asked for a descriptive statements. This paper focuses on all 7 domains: (1) patient volume, (2) patient follow-up, (3) acute issues, (4) provider characteristics, (5) waiting times, (6) patient safety procedures, and (7) prophylaxis practices.
Measures
Patient volume was evaluated by asking the following questions:
How many new patients does your clinic see per year?
How many total patients does your clinic follow per year?
What is the overall no-show rate for routine appointments per day?
What is the no-show rate for new patients?
What is the no-show rates for established patients?
Two questions were devoted to patient follow-up. First, “How do you define loss to follow-up in your clinic?” and second, based on that answer, “What is the loss to follow-up each year?”
The processes of dealing with acute care issues were assessed by asking how clinics handle urgent clinical problems during the day, at night, and on weekends. Also, clinics were asked if they have a walk-in policy and same-day urgent appointments. Responders were asked to describe their walk-in policy and number of same day urgent appointments slots offered per day.
Provider characteristics were ascertained by asking:
How many primary care providers work in your clinic?
What is the distribution of providers (attending levels physicians, physician trainees, nurse practitioners [NPs], physician assistants [PAs], others)?
How many half-day sessions per week does your clinic run?
How many providers operate per half day session?
How many patients is each provider scheduled per half day session?
What is the average panel size per provider?
Respondents were asked the average wait time for new patient appointments and for routine follow-up appointments. Also, they were asked about the length of new patient and routine follow-up appointments according to provider type. The availability of onsite consult services, including case management, clinical pharmacy, psychiatry, substance abuse, gynecology, dermatology, colposcopy, hepatology, neurology, ophthalmology, gastroenterology, dental, oncology, and anoscopy was assessed.
Patient safety practices were determined by inquiring about the presence of a clinic policy/procedure: (1) to inform clinical staff if a patient has been hospitalized; (2) to screen for adverse drug interactions; (3) to promptly identify and respond to critical laboratory results; (4) and to engage patients who have missed appointments. In addition, clinics were asked about procedures used to coordinate care between HIV clinic staff and providers in other specialty areas, the frequency of obtaining outside hospital records, and the ability for other clinics to access medical records of patients cared for in the HIV clinic.
Structures designed to address opportunistic infection prophylaxis were assessed by asking each medical director if a standardized initial medical evaluation form was used; and if so, whether that form prompted providers to give opportunistic illness (OI) prophylaxis when indicated. In addition, clinics were asked if they have a systematic review process to assess if patients receiving ongoing care are on appropriate OI prophylaxis, if they conduct CME lectures on prophylaxis topics, and if they send OI prophylaxis guideline reminders to providers.
Data analysis
Survey responses were tabulated by site. Medians and ranges were calculated for all survey questions requiring a numerical answer, including patient volume, number of providers employed, waiting times to schedule appointments, and annual patient loss to follow-up. Percentages were calculated for all yes–no questions and used to quantify structures in HIVRN clinics, including onsite consultative services, systems in place to handle acute patient care issue, and patient safety procedures. Descriptive statements served to clarify and elaborate on yes–no responses.
Results
Demographic and clinical characteristics of adult HIVRN study participants during the year 2006 are displayed in Table 1. The majority of the sample was males of race/ethnic minority. HIV transmission was secondary to non-injection drug use (IDU) in 81% of the sample. Most study participants had either Medicaid, Ryan White CARE Act funding, or were uninsured. Over 70% of participants were currently receiving HAART during 2006.
Table 1.
Demographic and Clinical Characteristics of Adult HIV Research Network Study Samplea
| Characteristic | 2006 N = 13,833 (%) |
|---|---|
| Gender | |
| Male | 9826 (71) |
| Female | 4007 (29) |
| Age (years) | |
| 18–30 | 1291 (9) |
| 31–49 | 8833 (64) |
| 50+ | 3709 (27) |
| Race/ethnicity | |
| White | 3743 (27) |
| Black | 6422 (46) |
| Hispanic | 3140 (23) |
| Other | 292 (2) |
| Unknown | 236 (2) |
| HIV transmission | |
| Non-IDU | 11148 (81) |
| IDU | 2685 (19) |
| Initial CD4 in Year (cells/mm3) | |
| <51 | 982 (7) |
| 51–200 | 2098 (15) |
| 201–500 | 5972 (43) |
| >500 | 4781 (35) |
| Initial HIV-1 RNA in Year (copies/mL) | |
| < 10,001 | 9280 (67) |
| 10,001–100,000 | 2727 (20) |
| > 100,000 | 1653 (12) |
| Missing | 173 (1) |
| HAART receipt | |
| No | 3727 (27) |
| Yes | 10106 (73) |
| Insurance | |
| Private | 1661 (12) |
| Medicaid | 4760 (34) |
| Medicare | 1628 (12) |
| Medicaid & Medicare | 978 (7) |
| Ryan White/uninsured | 3827 (28) |
| Missing | 979 (7) |
Data represent information from 11 of 15 adult HIVRN sites.
IDU, injection drug use; HAART, highly active antiretroviral therapy.
The total number of patients followed per year at each site ranges from 355 to 5600, with a median of 1300 patients. Eight sites (53%) follow more than 1000 patients per year. HIVRN adult clinics enrolled 60 to 730 new patients per year, with a median of 250 patients per year.
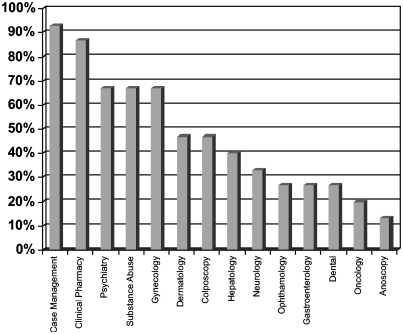
The number of total providers working in HIVRN adult clinic varies, ranging from 2 to 72, with a median of 15 providers per clinic. The majority of providers are attending physicians (51%), with the remaining consisting of physician trainees (34%), NPs (11%), and PAs (4%). Nearly all clinics (87%) employ midlevel providers, defined as NPs and PAs, and 80% utilize physician trainees. HIVRN clinics vary in the type of onsite services offered, ranging from high-resolution anoscopy (13%) to case management (93%; Fig. 1).
FIG. 1.
Onsite services available in HIVRN Adult Cinics.
Attending physicians, NPs, and PAs have similar patient panel size, patient volume per half-day clinic session, and appointment length (Table 2). Specifically, for these three groups, the median panel size is 129 to 142 patients (range, 10.5–300), median patient volume per half-day session is 8.5 to 9 (range, 5–15), median new patient appointment length is 40 to 50 minutes (range, 15–60), and median established patient appointment length is 20 minutes (range, 15–45). Full time clinicians typically work a median of 8 half-day sessions per week (range, 1–1).
Table 2.
Panel Size and Appointment Length by Provider Type
| |
|
|
Median appointment length in minutes (range) |
|
|---|---|---|---|---|
| Provider | Median panel size (range) | Median patient volume per 1/2 day session (range) | New patients | Established patients |
| MD/DO (attending) | 135 (70–300) | 8.5 (5–15) | 40 (15–60) | 20 (15–45) |
| MD (trainee) | 30 (19–80) | 5 (2–9.5) | 60 (40–60) | 20 (15–60) |
| NP | 129 (10.5–175) | 9 (5–14) | 50 (15–60) | 20 (15–30) |
| PA | 142 (100–159) | 9 (5–11.5) | 42.5 (35–60) | 20 (17.5–45) |
MD, doctor of medicine; DO, doctor of osteopathic medicine; NP, nurse practitioners; PA, physician assistants.
The median wait time to schedule a clinic appointment was 5 days (range, 0–22.5) for new patient visits and 8 days (range, 0–30) for established patient visits (Table 3). The median no-show rate for clinic appointments was 28% (range, 8%–40%), with median no-show rates for new patients at 30% (range, 8%–50%) and median no-show rate for established patients at 28% (range, 2%–40%). Clinics define loss to follow up differently. Most (87%) classify loss to follow-up as missing clinic visits for 1 year, while others (13%) use a 6-month cutoff. The median annual loss to follow up, calculated individually using each HIVRN clinic's definition, was 15% (range, 5%–25%).
Table 3.
Median Wait for Appointments and No-Show Rates by Site
| |
Average wait for appointments |
No-show rates |
|||
|---|---|---|---|---|---|
| Clinic | New patients (days) | Established patients (days) | Overall | New patients | Established patients |
| A | 0.5 | 0.5 | 10% | 17% | 5% |
| B | 21 | 21 | 36% | 36% | 36% |
| C | 17.5 | 17.5 | 20% | 25% | 18% |
| D | 0 | 0.5 | 25% | 5% | 25% |
| E | 2.5 | 2.5 | 15% | 10% | 20% |
| F | 14 | 8 | 8% | 8% | 2% |
| G | 22.5 | 22.5 | 40% | 40% | 40% |
| H | 2.5 | 30 | 28% | 28% | 28% |
| I | 21 | 8 | 31% | 54% | 30% |
| J | 5 | 15 | 22% | 30% | 22% |
| K | 3 | 4.5 | 27% | 30% | 26% |
| L | 10 | 0 | 40% | 50% | 40% |
| M | 1.5 | 2 | 30% | 33% | 29% |
| N | 10 | 7 | 40% | 40% | 40% |
| O | 3 | 10 | 32% | 50% | 31% |
Acute patient care issues are handled by clinics in a variety of manners, including same-day appointments, walk-in appointments, referral to emergency departments, and by on-call providers. During the day, 87% of clinics provide same-day appointments and 80% have a walk-in policy. At night and on weekends, 87% of clinics utilize an on-call provider, with the remaining clinics referring patients to emergency departments.
HIVRN clinics have established a number of patient safety procedures: 93% have a clinic policy to identify and respond to critical laboratory results, 73% have a policy to engage patients lost to follow-up, and 47% have a policy to screen for adverse drug interactions. In addition, 53% of clinics routinely obtain hospital records for patients hospitalized at outside institutions and 67% of clinics share their medical records with providers in other general and specialty clinics.
Eighty percent of HIVRN clinics utilize a standardized initial medical evaluation form. Of those with standardized intake forms, 33% of the forms prompt providers to administer OI prophylaxis medications when indicated. Furthermore, 67% of clinics send prophylaxis guideline reminders to providers and 60% conduct continued medical education lectures on prophylaxis indications. Over half, 53%, of HIVRN clinics conduct a systematic review of patients with CD4 counts less than 200 cells/mm3 to assess if they are on appropriate OI prophylaxis. All clinics conducting such a review provide feedback to their providers, and 63% of clinics give information comparing individual providers to other providers in the clinic.
Discussion
HIV management and health care expenditures are shifting from the inpatient to the outpatient arena.5–8 This study highlights the variability in the structures of medical care delivery by experienced providers in high-volume, adult HIV clinics.
Care by midlevel providers, NPs and PAs, is increasing at a rapid pace.15,16 Our provider characteristics are similar to those of Ryan White Comprehensive AIDS Resources Emergency (CARE) Act Title III funded sites, where midlevel providers constitute 20% of all primary HIV providers in the outpatient setting,17 with nearly all HIVRN clinics employing midlevel providers. This differs from the Department of Veteran Affairs (VA) HIV outpatient clinics, where 52% of all clinics are staffed solely by attending physicians and multidisciplinary provider teams (e.g., attending physicians, midlevel providers, and trainees) are utilized in only 13% of clinics.18
Among general patients, short-term health outcomes and quality of care measures seem equivalent between NPs and physicians in the primary care setting.19 Patient satisfaction is higher19 and health services cost is 12.5% lower for NPs compared to primary care physicians.20 In regards to HIV outpatient care, a recent cross-sectional analysis compared the quality of care provided by NPs and PAs to those of infectious diseases-trained physicians, general medicine HIV experts, and general medicine non-HIV experts.17 Eight quality measures were identified: prescribing HAART, HIV-1 RNA suppression, Pneumocystis jiroveci pneumonia (PCP) prophylaxis, purified protein derivative (PPD) testing rate, hepatitis C testing, papanicolaou smear, influenza vaccination, and outpatient visits during three of four quarters.17 NPs and PAs performed similarly on six of the eight quality measures as infectious diseases-trained physicians and general medicine HIV-experts and were superior in two measures (PPD testing rate and papanicolaou smear).17 Further research is needed to determine how NPs and PAs perform when faced with more complex HIV health care decisions, such as OI treatment, HAART treatment failure, drug–drug interactions, and adverse medication side effects.
The National Committee for Quality Assurance (NCQA) is currently developing HIV/AIDS performance measures.21 Nine categories have been established addressing measures on both the provider and system level, these include: (1) medical visits; (2) CD4 count measurement; (3) prescribing PCP prophylaxis; (4) adolescent and adult clients with HIV/AIDS who are prescribed HAART and who achieve HIV-1 RNA suppression; (5) tuberculosis screening; (6) sexually transmitted disease screening; (7) hepatitis B and C screening; (8) immunizations and vaccinations; and (9) high-risk behavior screening.21 The NCQA HIV/AIDS measures focus on processes of care and do not emphasize clinical outcomes and structure of health care delivery. Our study highlights important clinic structures that can serve as a point of reference for outpatient HIV care, including patient safety procedures, how acute patient care issues are addressed, and availability of onsite consultation services. In addition, we describe and quantify certain clinic operational parameters such as annual loss to follow up, appointment no-show rates, time to schedule clinic visits, and length of medical appointments. These data can serve as a baseline for future clinic structure research. Using the seven domains addressed in this study (patient volume, patient follow-up, acute issues, provider characteristics, waiting times, patient safety procedures, and prophylaxis practices) new research should focus on linking these structures to outcomes and in identifying the ideal components of an outpatient HIV clinic.
High no-show rates in many of our clinics for both new and follow-up visits may limit access to care and compromise provider productivity. A recent study of accelerated or open access scheduling systems, characterized by limiting the lead time to schedule appointments allowing patients to schedule visits soon after making an appointment request, may be a promising intervention that could be studied as part of quality and access improvement programs.22,23 Same-day and walk-in appointments, which are highly utilized in HIVRN clinics, may serve as an alternate mechanism to increase health care access and provider productivity.
The majority of HIVRN clinics utilize an on-call provider system to address acute patient care issues. Health Resources and Services Administration (HRSA) funded programs providing HIV care used a similar structure, at nearly all sites, to increase medical service accessibility.24 Physician on-call programs and evening or weekend clinic hours are associated with a reduction in the likelihood of repeat emergency department use.25 The utilization of internal clinic mechanisms to handle acute patient issues could potentially decrease emergency department visits and hospitalizations. Furthermore, if emergency department referral or hospitalization is required, providers can communicate medical information to the hospital or emergency department staff more efficiently. Improved communication between emergency department staff and primary physicians leads to better patient management.26
With the introduction of new antiretroviral drugs and an increase in available drug combinations, adverse drug side effects and interactions are frequently observed.27,28 In our study, 47% of clinics had a formalized policy to screen for adverse drug interactions. The majority of these policies included the participation of a pharmacist in reviewing medication lists and counseling patients on potential side effects. The use of clinical pharmacists can have an important impact on the delivery of outpatient HIV care. A study by Geletko et al.29 examining pharmacist interventions demonstrated that 62% of pharmacist interventions resulted in enhanced treatment efficacy, 14% resulted in the prevention of an adverse drug interaction or medication error, and 2% resulted in cost avoidance. Another study demonstrated that pharmacists decreased use of nonscheduled health services, number of specialty physician visits, and the number and cost of drugs.30 Screening for adverse events and interactions should be expanded in the outpatient setting, and clinical pharmacists should continue to be utilized.
HIVRN clinics provide a variety of onsite services. More than half of clinics offered on-site case management, clinical pharmacy, psychiatry, substance abuse, and gynecology services. This compares to HRSA-funded HIV care programs, which documented the presence of HIV medical care, mental health, and substance abuse treatment capabilities in 38% of programs.24 Most VA clinics treating HIV-infected patients have on-site pharmacy, substance abuse treatment, and mental health services.18 In a recent study, documenting the presence of on-site service in HIV clinics after a quality improvement intervention, it was noted that social work services were present in 84% of clinics and substance abuse counseling in 51%.31 Given the increased morbidity and mortality associated with illicit drug use32 and mental illness, more clinics are providing on-site substance abuse and mental health treatment. Data suggest that HIV-infected individuals are more likely to receive health maintenance interventions, such as vaccinations, if they are conducted in their primary care clinic as compared to outside clinics or sites requiring referral.33 The number and variety of onsite services provided in HIVRN clinics increases the likelihood that patients will attend appointments and receive appropriate follow-up.
There are several potential limitations to this study. First, although respondents used objective data when available, some responses were best estimates and could be affected by recall or good performance biases. Our study sites are not nationally representative and may not generalize to all HIV providers. The majority of HIVRN sites were large clinics in urban areas, and the data reported may not generalize well to smaller clinics and more rural locales. However, clinics treating high volumes of HIV infected patients likely face similar organizational issues as those identified in the HIVRN, allowing our findings to generalize more broadly to larger HIV clinics. In addition providers at these sites are highly experienced in HIV care with high rates of HAART usage and OI prophylaxis.34 Therefore, our results may serve as a model for patients receiving care from providers with less HIV experience. Comparison of NPs and PAs to attending physicians was limited since patient panel size was not adjusted for the number of half-day clinic sessions conducted per week. In addition, 30% of survey questions were yes–no, which could lead to both under reporting and over reporting of certain measures. A descriptive statement was required for some of these questions to further clarify responses.
In conclusion, surveyed clinics highly utilized midlevel providers, had an internal mechanism to respond to acute patient care issues, and instituted a number of patient safety and prophylaxis administration programs. HIVRN clinics treat high volumes of HIV infected persons and prescribe HAART and OI prophylaxis more frequently than national norms.34,35 Structures and operations of clinics in this network can serve as a model for the delivery of outpatient HIV health care.
Appendix.
| Participating Sites |
| Alameda County Medical Center, Oakland, California (Silver Sisneros, D.O.) |
| Children's Hospital of Philadelphia, Philadelphia, Pennsylvania (Richard Rutstein, M.D.) |
| Community Health Network, Rochester, New York (Roberto Corales, D.O.) |
| Community Medical Alliance, Boston, Massachusetts (James Hellinger, M.D.) |
| Drexel University, Philadelphia, Pennsylvania (Sara Allen, C.R.N.P., Peter Sklar, M.D.) |
| Henry Ford Hospital, Detroit, Michigan (Norman Markowitz, M.D.) |
| Johns Hopkins University, Baltimore, Maryland (Kelly Gebo, M.D., Richard Moore, M.D) |
| Montefiore Medical Group, Bronx, New York (Robert Beil, M.D.) |
| Montefiore Medical Center, Bronx, New York (Lawrence Hanau, M.D.) |
| Nemechek Health Renewal, Kansas City, Missouri (Patrick Nemechek, D.O.) |
| Oregon Health and Science University, Portland, Oregon (P. Todd Korthuis, M.D.) |
| Parkland Health and Hospital System, Dallas, Texas (Philip Keiser, M.D.) |
| St. Jude's Children's Hospital and University of Tennessee, Memphis, Tennessee (Aditya Gaur, M.D.) |
| St. Luke's Roosevelt Hospital Center, New York, New York (Victoria Sharp, M.D.) |
| Tampa General Health Care, Tampa, Florida (Charurut Somboonwit, M.D.) |
| University of California, San Diego, La Jolla, California (Stephen Spector, M.D.) |
| University of California, San Diego, California (W. Christopher Mathews, M.D.) |
| Wayne State University, Detroit, Michigan (Jonathan Cohn, M.D.) |
| Sponsoring Agencies |
| Agency for Healthcare Research and Quality, Rockville, Maryland (Fred Hellinger, Ph.D., John Fleishman, Ph.D., Irene Fraser, Ph.D.) |
| Health Resources and Services Administration, Rockville, Maryland (Alice Kroliczak, Ph.D., Robert Mills, Ph.D.) |
| Substance Abuse and Mental Health Services Administration, Rockville, Maryland (Kevin Mulvey, Ph.D., Pat Roth) |
| Data Coordinating Center |
| Johns Hopkins University, Baltimore, Maryland (Richard Moore, M.D., Jeanne Keruly, C.R.N.P., Kelly Gebo, M.D., Perrin Hicks, M.P.H., Michelande Ridoré, B.A.) |
Acknowledgments
Supported by the Agency for Healthcare Research and Quality (290-01-0012), the National Institute of Aging (R01 AG026250), and the National Institute on Drug Abuse (K23DA019809). Dr. Gebo also received support from the Johns Hopkins University Richard S. Ross Clinician Scientist Award.
The views expressed in this paper are those of the authors. No official endorsement by DHHS, the National Institutes of Health, or the Agency for Healthcare Research and Quality is intended or should be inferred.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Palella FJ., Jr Delaney KM. Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853–860. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- 2.Moore RD. Chaisson RE. Natural history of HIV infection in the era of combination antiretroviral therapy. AIDS. 1999;13:1933–1942. doi: 10.1097/00002030-199910010-00017. [DOI] [PubMed] [Google Scholar]
- 3.Mouton Y. Alfandari S. Valette M, et al. Impact of protease inhibitors on AIDS-defining events and hospitalizations in 10 French AIDS reference centres. Federation National des Centres de Lutte contre le SIDA. AIDS. 1997;11:F101–105. doi: 10.1097/00002030-199712000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Torres RA. Barr M. Impact of combination therapy for HIV infection on inpatient census. N Engl J Med. 1997;336:1531–1532. doi: 10.1056/nejm199705223362118. [DOI] [PubMed] [Google Scholar]
- 5.Bozzette SA. Berry SH. Duan N, et al. The care of HIV-infected adults in the United States. HIV Cost and Services Utilization Study Consortium. N Engl J Med. 1998;339:1897–1904. doi: 10.1056/NEJM199812243392606. [DOI] [PubMed] [Google Scholar]
- 6.Bozzette SA. Joyce G. McCaffrey DF, et al. Expenditures for the care of HIV-infected patients in the era of highly active antiretroviral therapy. N Engl J Med. 2001;344:817–823. doi: 10.1056/NEJM200103153441107. [DOI] [PubMed] [Google Scholar]
- 7.Fleishman JA. Gebo KA. Reilly ED, et al. Hospital and outpatient health services utilization among HIV-infected adults in care 2000–2002. Med Care. 2005;43(9 Suppl):III40–52. doi: 10.1097/01.mlr.0000175621.65005.c6. [DOI] [PubMed] [Google Scholar]
- 8.Hellinger FJ. The lifetime cost of treating a person with HIV. JAMA. 1993;270:474–478. [PubMed] [Google Scholar]
- 9.Gifford AL. Groessl EJ. Chronic disease self-management and adherence to HIV medications. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S163–166. doi: 10.1097/00126334-200212153-00016. [DOI] [PubMed] [Google Scholar]
- 10.Kitahata MM. Koepsell TD. Deyo RA. Maxwell CL. Dodge WT. Wagner EH. Physicians' experience with the acquired immunodeficiency syndrome as a factor in patients' survival. N Engl J Med. 1996;334:701–706. doi: 10.1056/NEJM199603143341106. [DOI] [PubMed] [Google Scholar]
- 11.HIV Medicine Association. HIVMA's Definition of an Experienced HIV Provider. 2007. www.hivma.org/Content.aspx?id=1782. [Oct 17;2007 ]. www.hivma.org/Content.aspx?id=1782
- 12.Solomon L. Flynn C. Lavetsky G. Managed care for AIDS patients: Is bigger better? J Acquir Immune Defic Syndr. 2005;38:342–347. [PubMed] [Google Scholar]
- 13.Schneider JA. Zhang Q. Auerbach A, et al. Do hospitalists or physicians with greater inpatient HIV experience improve HIV care in the era of highly active antiretroviral therapy? Results from a multicenter trial of academic hospitalists. Clin Infect Dis. 2008;46:1085–1092. doi: 10.1086/529200. [DOI] [PubMed] [Google Scholar]
- 14.Donabedian A. The Definition of Quality and Approaches to Its Assessment. Ann Arbor, MI: Health Administration Press; 1980. Explorations in Quality Assessment and Monitoring Vol. 1. [Google Scholar]
- 15.Cooper RA. Perspectives on the physician workforce to the year 2020. JAMA. 1995;274:1534–1543. [PubMed] [Google Scholar]
- 16.Cooper RA. Laud P. Dietrich CL. Current and projected workforce of nonphysician clinicians. JAMA. 1998;280:788–794. doi: 10.1001/jama.280.9.788. [DOI] [PubMed] [Google Scholar]
- 17.Wilson IB. Landon BE. Hirschhorn LR, et al. Quality of HIV care provided by nurse practitioners, physician assistants, and physicians. Ann Intern Med. 2005;143:729–736. doi: 10.7326/0003-4819-143-10-200511150-00010. [DOI] [PubMed] [Google Scholar]
- 18.Yano EM. Asch SM. Phillips B, et al. Organization and management of care for military veterans with human immunodeficiency virus/acquired immunodeficiency syndrome in Department of Veterans Affairs Medical Centers. Mil Med. 2005;170:952–959. doi: 10.7205/milmed.170.11.952. [DOI] [PubMed] [Google Scholar]
- 19.Horrocks S. Anderson E. Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324:819–823. doi: 10.1136/bmj.324.7341.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Venning P. Durie A. Roland M. Roberts C. Leese B. Randomised controlled trial comparing cost effectiveness of general practitioners and nurse practitioners in primary care. BMJ. 2000;320:1048–1053. doi: 10.1136/bmj.320.7241.1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Committee for Quality Assurance American Medical Association (AMA), AMA-Convened Physician Consortium for Performance Improvement® Health Resources Services Administration Infectious Diseases Society of America/HIV Medicine Association. HIV/AIDS Performance Measures Specifications for Public Comment. 2007.
- 22.Kopach R. DeLaurentis PC. Lawley M, et al. Effects of clinical characteristics on successful open access scheduling. Health Care Manage Sci. 2007;10:111–124. doi: 10.1007/s10729-007-9008-9. [DOI] [PubMed] [Google Scholar]
- 23.Valenti WM. Bookhardt-Murray J. Advanced-access scheduling increases quality, productivity, and revenue. AIDS Read. 2004;14:220–224. [PubMed] [Google Scholar]
- 24.Tobias C. Drainoni ML. Wood S. Analysis of Human Resources and Services Administration-funded services for HIV-positive substance users: A study of Ryan White CARE Act Title III, Title IV, and Special Projects of National Significance providers. AIDS Patient Care STDs. 2004;18:604–613. doi: 10.1089/apc.2004.18.604. [DOI] [PubMed] [Google Scholar]
- 25.Markson LE. Houchens R. Fanning TR. Turner BJ. Repeated emergency department use by HIV-infected persons: Effect of clinic accessibility and expertise in HIV care. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;17:35–41. doi: 10.1097/00042560-199801010-00005. [DOI] [PubMed] [Google Scholar]
- 26.Afilalo M. Lang E. Leger R, et al. Impact of a standardized communication system on continuity of care between family physicians and the emergency department. CJEM. 2007;9:79–86. doi: 10.1017/s1481803500014834. [DOI] [PubMed] [Google Scholar]
- 27.Hellinger FJ. Encinosa WE. Inappropriate drug combinations among privately insured patients with HIV disease. Med Care. 2005;43(9 Suppl):III53–62. doi: 10.1097/01.mlr.0000175630.68791.cd. [DOI] [PubMed] [Google Scholar]
- 28.Fellay J. Boubaker K. Ledergerber B, et al. Prevalence of adverse events associated with potent antiretroviral treatment: Swiss HIV Cohort Study. Lancet. 2001;358(9290):1322–1327. doi: 10.1016/s0140-6736(01)06413-3. [DOI] [PubMed] [Google Scholar]
- 29.Geletko SM. Poulakos MN. Pharmaceutical services in an HIV clinic. Am J Health Syst Pharm. 2002;59:709–713. doi: 10.1093/ajhp/59.8.709. [DOI] [PubMed] [Google Scholar]
- 30.Beney J. Bero LA. Bond C. Expanding the roles of outpatient pharmacists: effects on health services utilisation, costs, and patient outcomes. Cochrane Database Syst Rev. 2000. p. CD000336. [DOI] [PubMed]
- 31.McInnes DK. Landon BE. Wilson IB, et al. The impact of a quality improvement program on systems, processes, and structures in medical clinics. Med Care. 2007;45:463–471. doi: 10.1097/01.mlr.0000256965.94471.c2. [DOI] [PubMed] [Google Scholar]
- 32.Lucas GM. Griswold M. Gebo KA. Keruly J. Chaisson RE. Moore RD. Illicit drug use and HIV-1 disease progression: A longitudinal study in the era of highly active antiretroviral therapy. Am J Epidemiol. 2006;163:412–420. doi: 10.1093/aje/kwj059. [DOI] [PubMed] [Google Scholar]
- 33.Sheth AN. Moore RD. Gebo KA. Provision of general and HIV-specific health maintenance in middle aged and older patients in an urban HIV clinic. AIDS Patient Care STDs. 2006;20:318–325. doi: 10.1089/apc.2006.20.318. [DOI] [PubMed] [Google Scholar]
- 34.Gebo KA. Fleishman JA. Reilly ED. Moore RD. High rates of primary Mycobacterium avium complex and Pneumocystis jiroveci prophylaxis in the United States. Med Care. 2005;43(9 Suppl):III23–30. doi: 10.1097/01.mlr.0000175631.34438.1e. [DOI] [PubMed] [Google Scholar]
- 35.Gebo KA. Fleishman JA. Conviser R, et al. Racial and gender disparities in receipt of highly active antiretroviral therapy persist in a multistate sample of HIV patients in 2001. J Acquir Immune Defic Syndr. 2005;38:96–103. doi: 10.1097/00126334-200501010-00017. [DOI] [PubMed] [Google Scholar]