Abstract
Eight smokers were randomly assigned to a deposit contract ($50.00) or to a no-deposit group. Using a reversal design, participants could recoup their deposit (deposit group) or earn vouchers (no-deposit group) for smoking reductions and abstinence (breath carbon monoxide [CO] ≤ 4 parts per million) during treatment phases. Treatment was delivered via a novel Internet-based method to monitor smoking status. Although equivalent decreases in breath CO and abstinence were observed during treatment in both groups, $178.50 in vouchers were distributed to participants in the no-deposit group, whereas a small surplus remained in the deposit group. A deposit contract method may represent a cost-effective model to deliver abstinence reinforcement for cigarette smoking.
Keywords: abstinence, cigarette smoking, deposit contract, nicotine, voucher reinforcement
Cigarette smoking is the largest preventable risk factor for morbidity and mortality in developed countries. Although the U.S. Public Health Service endorses various pharmacotherapies and counseling for smoking cessation (Fiore et al., 2000), the majority of patients relapse within 6 months, even when both types of treatments are used together (Ahluwalia, Harris, Catley, Okuyemi, & Mayo, 2002; Fiore, Smith, Jorenby, & Baker, 1994). Several authors have argued that innovative and more intensive behavioral treatments are necessary (Dallery, Glenn, & Raiff, 2007; Sigmon, Lamb, & Dallery, 2008).
We developed an Internet-based abstinence reinforcement intervention (Dallery & Glenn, 2005; Dallery et al., 2007; Glenn & Dallery, 2007). The intervention circumvented several obstacles associated with frequent monitoring of smoking status (e.g., making twice-daily visits to a clinic). Smoking status was verified by employing user-friendly Internet technology to observe participants providing carbon monoxide (CO) samples via a Web camera. Participants could earn voucher reinforcers exchangeable for merchandise available on the Internet for evidence of reductions and abstinence. There was excellent compliance with the treatment; in one study over 97% of the 1,120 scheduled CO samples were collected (Dallery et al.). The treatment also promoted high rates of abstinence in a sample of heavy smokers: Over 65% of the 400 CO samples were negative during treatment.
Another feature of abstinence reinforcement programs that may limit their applicability is their cost. The costs of such programs will vary depending on the delivery setting, but a primary source stems from the vouchers. Although there are a variety of potential solutions that could either mitigate or eliminate these expenses (Amass & Kamien, 2004; Donatelle et al., 2004; Jeffrey, Pheley, Forster, Kramer, & Snell, 1988; Matson, Lee, & Hopp, 1993; Petry et al., 2005; Puska, Korhonen, Korhonen, & McAlister, 1996), a deposit contract method represents a straightforward and potentially effective method to deliver treatment. Consumers are accustomed to paying a fee for health-related treatments in the United States (Busch et al., 2004). Also, there is a long history of using deposit contracting to reduce or eliminate a number of target behaviors, including cigarette smoking (Bowers, Winett, & Frederiksen, 1987; Elliot & Tighe, 1968; Lando, 1977; Paxton, 1980, 1981, 1983; Singh & Leung, 1988; Winett, 1973). Most of these procedures specified that an initial monetary deposit can be recouped based on smoking reductions and abstinence, and the results suggest that deposit contracts are effective. However, deposit reimbursement was typically contingent on self-reports of smoking abstinence rather than biochemical verification of abstinence.
A more rigorous and potentially effective way to reimburse the deposit is to use objective measures of smoking status. To our knowledge, no study has evaluated the effects of contingent reimbursement of a deposit based on objective measures of smoking status. The purpose of the current study was to assess the feasibility and effects of a deposit contract method of delivering abstinence reinforcement using an Internet-based method to objectively verify smoking status.
Method
Participants
Participants were 8 smokers recruited through local print media, flyers, and word of mouth. Interested smokers underwent a brief phone interview to ensure that basic inclusion criteria were met. To meet these criteria, participants were required to be between the ages of 18 and 60, express a desire to quit, smoke a minimum of 10 cigarettes per day, and have at least a 2-year smoking history. Qualified applicants were scheduled for in-person interviews. Table 1 presents participant characteristics.
Table 1.
Participant Characteristics
| Age (Years) | Sex | Ethnicity | Income per week ($) | Cigarettes per day | Years smoking | |
| Deposit | ||||||
| H0079 | 34 | F | W | 401–500 | 20 | 20 |
| M0096 | 54 | F | W | > $700 | 20 | 27 |
| D0102 | 20 | M | W | 201–300 | 20 | 5 |
| A0104 | 27 | F | W | 100–200 | 20 | 10 |
| No deposit | ||||||
| D0089 | 55 | F | W | < 100 | 40 | 40 |
| G0095 | 21 | F | H | 301–400 | 20 | 4 |
| P0096 | 34 | F | W | 301–400 | 25 | 11 |
| M0100 | 27 | M | W | 401–500 | 25 | 10 |
Interview
Participants read and signed an informed consent that described in detail all the phases and procedures in the study. A CO reading of less than 10 parts per million (ppm) resulted in disqualification from the study. Qualified participants were randomly divided into two groups (4 per group).
Participants assigned to the deposit group were asked to pay researchers a $50.00 deposit. Participants were able to earn back this deposit, in cash, over the course of the study as well as an additional $28.80 in vouchers if all of the study requirements were met (see Experimental Design below). (For convenience, the term vouchers will be used hereafter to refer to both cash reimbursements of the deposit and voucher earnings.) We set the deposit at $50.00 so that it would not be unduly prohibitive and to be consistent with the relatively low amounts required in previous studies that have used a deposit contract (e.g., Elliot & Tighe, 1968; Paxton, 1980, 1981, 1983; Winett, 1973). Participants assigned to the no-deposit group were not asked to pay an initial deposit; these participants were able to earn a total of $78.80 in vouchers if all study requirements were met. Participants were informed about these potential earnings.
Materials
Most of the materials and methods are described in detail elsewhere (Dallery et al., 2007). We loaned each participant a CO monitor and a Web camera. If participants did not own their own computer, we loaned them laptops. CO levels were displayed on the CO monitor (in parts per million) by illumination of a series of light-emitting diodes (LEDs) on the front panel of the monitor.
CO Monitoring
CO levels were measured twice daily with at least 8-hr intervals between samples (Dallery & Glenn, 2005; Dallery et al., 2007; Glenn & Dallery, 2007). Participants were compliant with the 8-hr intersample interval requirement. To leave a sample, each participant logged on to the University of Florida Smoking Lab and Clinic (UF-SLC) Web site. A Web page appeared with a code consisting of 10 randomly generated numbers and letters. The Web camera was positioned to face the participant, the computer monitor displaying the random code, and the CO monitoring device held by the participant. Thus, it was easy to detect that the CO monitor was reset (i.e., a reading of zero was displayed) and ready for operation. After the CO monitor was reset, the participant inhaled deeply, started the CO monitor countdown, and held his or her breath while 15 LEDs on the monitor were consecutively extinguished over 15 s. A single LED then flashed, at which point the participant exhaled fully into the CO monitor. An audible hiss resulted from exhaling into the CO monitor and was easily detectable from video samples. After exhaling into the CO monitoring device, LEDs illuminated to correspond to the amount of CO in the participant's breath. At this point, the participant stopped the video recording and e-mailed it to researchers. Because the computer monitors displaying the randomly generated codes were included in each video sample, researchers could later access the Web site to determine when each sample was taken (i.e., after the code was generated and before the video was sent via e-mail). Consequently, researchers could confirm that CO samples were taken at the times corresponding with participants' self-reports.
Experimental Design
The experiment was a single-subject reversal design (ABCA) consisting of the following four phases: baseline (A), shaping (B), abstinence induction (C), and return to baseline (A). The experiment lasted for 24 consecutive days. Vouchers could be earned only during the shaping and abstinence induction phases. In the deposit group, the first $50.00 earned by participants represented reimbursement for the initial deposit. The reimbursement was in the form of cash delivered at the end of the treatment period. The remaining vouchers earned by the deposit group (up to $28.80) and all vouchers earned by the no-deposit group were exchangeable for goods on the Internet. Brief counseling sessions were held at the start of each condition. The first session was in person, and the rest were phone based. Each session lasted approximately 10 min and focused on practical cessation tips and problem-solving strategies (e.g., removing all cigarettes and lighters from the home, coping with craving).
Baseline (A)
The baseline phase lasted for 5 days. During this phase, CO samples were collected twice per day. No scheduled consequences were in effect.
Shaping (B)
The shaping phase lasted for 4 days. During this phase, vouchers were contingent on specified reductions in CO level. The reductions were determined as follows: First, the mean CO during baseline was determined. Then, progressively lower CO values were calculated such that over eight samples the last CO level would be ≤ 4 ppm (our criterion for abstinence). Participants earned $0.50 for the first submission with a CO level that met the criterion for specified reductions in CO. Each consecutive sample submission that met the necessary criterion resulted in a $0.10 increase in the value of the voucher earned. Every third consecutive sample submission that met the schedule criterion resulted in an additional $3.00 bonus voucher. If participants failed to submit a sample or submitted a sample that did not meet the specified criterion, no vouchers were earned and the value of the next voucher earned was reset to $0.50. Following a reset, the voucher value returned to the highest value previously obtained if three consecutive samples were submitted that met the necessary criteria for CO reduction.
Abstinence Induction (C)
The abstinence induction phase lasted for 10 days. The schedule of reinforcement simply continued from the shaping phase. However, during abstinence induction, participants were required to demonstrate abstinence by submitting CO samples at or below 4 ppm (designated as negative samples) to earn vouchers.
Return to Baseline (A)
This phase was identical to the baseline phase.
Participants were encouraged to visit the UF-SLC Web site throughout the study. A graph of CO results, a statement of cumulative voucher earnings, a statement of remaining voucher earnings if a purchase had been made, and a link to a Web page that listed Internet vendors at which the vouchers could be redeemed were available on the Web site. The site also provided a list of links to smoking-cessation sites and other health-related information.
Participants notified research staff when they wished to purchase an item with the vouchers. If they had enough vouchers, research staff ordered and delivered the item. Delivery usually occurred within 1 to 3 weeks of the initial request. Participants could not buy firearms, weapons, drugs, or alcohol. Following sample submissions, participants also received e-mails from researchers that stated total voucher earnings.
Results and Discussion
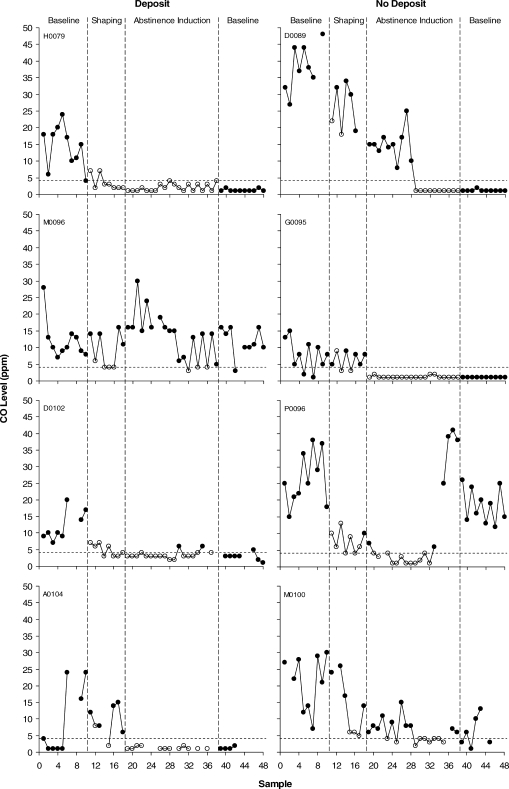
Figure 1 shows CO levels across all phases of the study for all individuals. Relative to baseline, CO levels decreased during the shaping and abstinence induction phases for 7 of the 8 participants. Missing samples are indicated by missing data points (26 in the deposit group and 13 in the no-deposit group). One participant (A0104) accounted for 17 of the missing samples in the deposit group. One participant (M0096) did not show clear reductions in CO during the intervention phases. All other participants showed evidence of sustained abstinence (i.e., four or more consecutive negative COs). Only 1 participant (P0096) who decreased CO levels during abstinence showed a clear return to baseline in CO levels after achieving sustained abstinence. Another participant (M0100) who decreased CO levels during abstinence resumed some smoking during the return-to-baseline phase, albeit at lower levels than the first baseline phase. All other participants showed sustained abstinence even after the vouchers were withdrawn.
Figure 1.
CO levels across all phases of the study. The dashed horizontal line indicates the abstinence criterion of 4 ppm. Open data points indicate that the sample met the shaping or abstinence criterion during the shaping and abstinence induction phases, respectively. Missing data points indicate when samples were not submitted.
There were no clear differences in rates of abstinence between the deposit and no-deposit groups (Figure 1). In the deposit group, 65% of the samples were negative during the abstinence induction phase, and in the no-deposit group, 63% of the samples were negative in the abstinence induction phase (missing samples were considered positive). Despite several procedural differences, these numbers are consistent with the 65% of negative samples in our previous and largest study (Dallery et al., 2007).
The total amount distributed in voucher earnings in the deposit and no-deposit groups was $156.90 and $178.50, respectively. However, because participants in the deposit group paid $200.00 in deposits, a $43.10 surplus remained for this group; researchers used this surplus to supplement experimental costs (e.g., vouchers earned by participants in the no-deposit group). By assigning individuals to groups after the informed consent process, we attempted to equate the groups in terms of willingness to provide a deposit (and possibly in terms of motivation to quit and financial means). We should note that several participants declined to participate or did not attend the screening after learning about the study. It is not clear, however, if the deposit per se affected their decision. We did not query participants about their reasons for not participating. No one withdrew from the study after assignment to the deposit group.
The present study demonstrated that a deposit contract method of delivering abstinence reinforcement is feasible. There are clearly several practical issues that would have to be addressed should a treatment of this sort be promoted to community providers. For instance, it will be necessary to find some balance between the amount of the deposit, treatment acceptability, and treatment effectiveness (Paxton, 1981, 1983). The most cost-effective approach may require larger incentives (Sindelar, Elbel, & Petry, 2007). It would not be desirable, however, if the cost of the treatment unduly discouraged participation for lower income smokers. One solution would be to use a sliding deposit scale and corresponding earnings rate based on income. We should emphasize that the amount deposited was less than a typical smoker would pay for cigarettes during the same period.
More work is necessary to evaluate the acceptability and effectiveness of a deposit contract. The present study used a small sample size, and we did not evaluate reasons why some participants declined to participate or did not attend screening appointments after our initial contact. If a deposit contract method could be integrated with an Internet-based delivery model, it could promote both the sustainability and the dissemination of the intervention.
Acknowledgments
This research was supported by NIH Grant R21DA015289. We thank Matthew Locey, Julie Marusich, and Bethany Raiff for their helpful suggestions on a previous version of this manuscript.
References
- Ahluwalia J.S, Harris K.J, Catley D, Okuyemi K.S, Mayo M.S. Sustained release bupropion for smoking cessation in African Americans. Journal of the American Medical Association. 2002;288:468–474. doi: 10.1001/jama.288.4.468. [DOI] [PubMed] [Google Scholar]
- Amass L, Kamien J. A tale of two cities: Financing two voucher programs for substance abusers through community donations. Experimental and Clinical Psychopharmacology. 2004;12:147–155. doi: 10.1037/1064-1297.12.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers T.G, Winett R.A, Frederiksen L.W. Nicotine fading, behavioral contracting, and extended treatment: Effects on smoking cessation. Addictive Behaviors. 1987;12:181–184. doi: 10.1016/0306-4603(87)90024-4. [DOI] [PubMed] [Google Scholar]
- Busch S.H, Falba T.A, Duchovny N, Jofre-Bonet M, O'Malley S.S, Sindelar J.L. Value to smokers of improved cessation products: Evidence from a willingness-to-pay survey. Nicotine and Tobacco Research. 2004;6:631–639. doi: 10.1080/14622200410001727885. [DOI] [PubMed] [Google Scholar]
- Dallery J, Glenn I.M. Effects of an Internet-based voucher reinforcement program for smoking abstinence: A feasibility study. Journal of Applied Behavior Analysis. 2005;38:349–357. doi: 10.1901/jaba.2005.150-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Glenn I.M, Raiff B.R. An Internet-based abstinence reinforcement treatment for cigarette smoking. Drug and Alcohol Dependence. 2007;86:230–238. doi: 10.1016/j.drugalcdep.2006.06.013. [DOI] [PubMed] [Google Scholar]
- Donatelle R, Hudson D, Dobie S, Goodall A, Hunsberger M, Oswald K. Incentives in smoking cessation: Status of the field and implications for research and practice with pregnant smokers. Nicotine and Tobacco Research. 2004;6:S163–S179. doi: 10.1080/14622200410001669196. [DOI] [PubMed] [Google Scholar]
- Elliot R, Tighe T. Breaking the cigarette habit: Effects of a technique involving threatened loss of money. The Psychological Record. 1968;18:503–513. [Google Scholar]
- Fiore M.C, Bailey W.C, Cohen S.J, Dorfman S.F, Goldstein M.G, Gritz E.R, et al. Treating tobacco use and dependence. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; 2000. [Google Scholar]
- Fiore M.C, Smith S.S, Jorenby D.E, Baker T.B. The effectiveness of nicotine patch for smoking cessation: A meta-analysis. Journal of the American Medical Association. 1994;271:1940–1947. [PubMed] [Google Scholar]
- Glenn I.M, Dallery J. Effects of Internet-based voucher reinforcement and a transdermal nicotine patch on cigarette smoking. Journal of Applied Behavior Analysis. 2007;40:1–13. doi: 10.1901/jaba.2007.40-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffrey R.W, Pheley A.M, Forster J.L, Kramer F.M, Snell M.K. Payroll contracting for smoking cessation: A worksite pilot study. American Journal of Preventive Medicine. 1988;4:83–86. [PubMed] [Google Scholar]
- Lando H.A. Successful treatment of smokers with a broad-spectrum behavioral approach. Journal of Consulting and Clinical Psychology. 1977;45:361–366. doi: 10.1037//0022-006x.45.3.361. [DOI] [PubMed] [Google Scholar]
- Matson D.M, Lee J.W, Hopp J.W. The impact of incentives and competitions on participation and quit rates in worksite smoking cessation programs. American Journal of Health Promotion. 1993;7:270–280. doi: 10.4278/0890-1171-7.4.270. [DOI] [PubMed] [Google Scholar]
- Paxton R. The effects of a deposit contract as a component in a behavioral programme for stopping smoking. Behaviour Research and Therapy. 1980;18:45–50. doi: 10.1016/0005-7967(80)90068-6. [DOI] [PubMed] [Google Scholar]
- Paxton R. Deposit contracts with smokers: Varying frequency and amount of repayments. Behaviour Research and Therapy. 1981;19:117–123. doi: 10.1016/0005-7967(81)90035-8. [DOI] [PubMed] [Google Scholar]
- Paxton R. Prolonging the effect of deposit contracts with smokers. Behaviour Research and Therapy. 1983;21:425–433. doi: 10.1016/0005-7967(83)90012-8. [DOI] [PubMed] [Google Scholar]
- Petry N.M, Peirce J.M, Stitzer M.L, Blaine J, Roll J.M, Cohen A, et al. Effect of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs: A National Drug Abuse Treatment Clinical Trials Network study. Archives of General Psychiatry. 2005;62:1148–1156. doi: 10.1001/archpsyc.62.10.1148. [DOI] [PubMed] [Google Scholar]
- Puska P, Korhonen H, Korhonen T, McAlister A. International quit and win '96: A global campaign to promote smoking cessation. Tobacco Control. 1996;5:342. doi: 10.1136/tc.5.4.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigmon S.C, Lamb R.J, Dallery J. Tobacco. In: Higgins S.T, Silverman K, Heil S.H, editors. Contingency management in substance abuse treatment. New York: Guilford; 2008. pp. 99–119. [Google Scholar]
- Sindelar J, Elbel B, Petry N.M. What do we get for our money? Cost-effectiveness of adding contingency management. Addiction. 2007;102:309–316. doi: 10.1111/j.1360-0443.2006.01689.x. [DOI] [PubMed] [Google Scholar]
- Singh N.N, Leung J. Smoking cessation through cigarette-fading, self-recording, and contracting: Treatment, maintenance and long-term follow-up. Addictive Behaviors. 1988;13:101–105. doi: 10.1016/0306-4603(88)90033-0. [DOI] [PubMed] [Google Scholar]
- Winett R.A. Parameters of deposit contracts in the modification of smoking. The Psychological Record. 1973;23:49–60. [Google Scholar]