Abstract
Contingency management (CM) is effective in enhancing retention in therapy. After an 8-week baseline, four community-based substance abuse treatment clinics were exposed in random order to 16 weeks of standard care with CM followed by 16 weeks of standard care without CM or vice versa. In total, 75 outpatients participated. Patients who were enrolled in the clinics when the CM treatment phase was in effect attended a significantly greater percentage of therapy sessions than patients who were enrolled in treatment when CM was not in effect. This study is one of the first to investigate CM in community settings implemented entirely by community clinicians, and results suggest that CM is effective in improving therapy attendance.
Keywords: attendance, community settings, contingency management, substance abuse treatment
Many patients in outpatient substance abuse treatment miss therapy sessions and have early attrition from treatment, which may negatively affect outcomes. A recent review of studies of attendance at substance abuse and psychiatric treatment programs reported that between 10% and 60% of scheduled appointments are not attended (Lefforge, Donohue, & Strada, 2007). Patients may miss appointments for several reasons, including treatment barriers such as transportation difficulties, scheduling conflicts, or lack of motivation. Regardless of the reason, missed sessions result in lost opportunities to provide care. Moreover, clinics cannot bill for unattended services, and missed sessions are an inefficient use of therapists' time. Thus, interventions are needed to improve treatment session attendance rates.
One potentially useful method for increasing treatment attendance is contingency management (CM). CM is based on the principles of operant conditioning (Higgins & Petry, 1999). In CM paradigms, a specific target behavior is selected and frequently monitored. When the behavior occurs, the patient is provided with tangible reinforcement (e.g., a voucher or a prize; Glenn & Dallery, 2007). In many CM interventions, the reinforcement magnitude is increased each time the participant satisfies the contingency until it reaches a maximum value. If the contingency is not satisfied, reinforcers are withheld, and the reinforcer magnitude is reset to the starting value. Several reinforcers have been used in studies of substance-abusing patients, including money, vouchers redeemable for merchandise, and the chance to win prizes.
CM interventions have demonstrated efficacy in promoting drug abstinence (e.g., Lussier, Heil, Mongeon, Badger, & Higgins, 2006; Prendergast, Podus, Finney, Greenwell, & Roll, 2006). Relatively few studies, however, have examined the usefulness of CM interventions for enhancing treatment attendance directly. The recent meta-analysis by Lussier et al. reviewed six studies of voucher-based reinforcement for attendance. They found a mean effect size (r) of 0.15, suggesting a relatively small effect of voucher CM on attendance rates. However, the small effect size with respect to CM's impact on attendance may be related to design and reinforcement issues in many of these attendance-specific studies, as noted below.
Two of the studies reviewed by Lussier et al. (2006) examined the efficacy of voucher-based incentives for substance abuse treatment attendance in pregnant substance-dependent women. Svikis, Lee, Haug, and Stitzer (1997) studied voucher incentives for attendance by pregnant women in methadone maintenance and drug-free treatment modalities. They found that patients in drug-free clinics who received higher value incentives (i.e., up to $10.00 per day) for attendance increased their number of treatment days attended. However, incentives were not effective at lower magnitudes (i.e., $1.00 per day) or with methadone-maintained women (who attended a majority of treatment days regardless of reinforcement condition, possibly because methadone itself is a powerful reinforcer). Jones, Haug, Stitzer, and Svikis (2000) randomly assigned substance-abusing pregnant women to a voucher reinforcement condition ($5.00 for attending treatment sessions plus bonuses for consecutive days) or to a control condition with no vouchers. They found that this fairly low magnitude of reinforcement did not affect attendance in drug-free treatment patients, but methadone-maintained patients who received the reinforcement attended more treatment hours and days than patients in the control condition.
Rhodes et al. (2003) examined the efficacy of a token-based voucher intervention for improving attendance to counseling sessions in methadone-maintained patients in two separate studies. Overall, they found that CM for attendance was effective in increasing attendance by poor attendees, but not by patients who already attended groups regularly. Sinha, Easton, Renee-Aubin, and Carroll (2003) randomly assigned probation-referred marijuana-abusing patients to receive a three-session motivational enhancement treatment (MET) or MET plus voucher CM. Patients could receive up to $120 for attending all three sessions on time, a relatively high magnitude of reinforcement. This study found robust effects of CM, with 65% of patients assigned to the MET plus CM completing all three expected sessions compared to 39% of patients who received MET alone. Helmus, Saules, Schoener, and Roll (2003) provided attendance-contingent incentives to community mental health center patients for attending group therapy sessions in an ABA (4-week baseline, 12-week CM, 4-week baseline) design. They found that attendance increased significantly during the CM phase (from 45% in baseline to 65% in CM) and remained higher during the second baseline phase (68%). Taken together, these studies suggest that voucher-based incentive programs that specifically target attendance can have a positive effect on attendance rates. However, some of the mixed findings may relate to the magnitude of reinforcement available and baseline attendance levels. These parameters have likewise been identified as important in CM studies that target drug abstinence (cf. Lussier et al., 2006; Peirce et al., 2006; Petry, Alessi, Marx, Austin, & Tardif, 2005).
In the current study, we examined a different form of CM applied to treatment attendance. Prize CM, which was developed as an alternative to voucher CM, has also been explored as a behavioral intervention for enhancing attendance. Instead of vouchers, patients earn the opportunity to draw from an urn and possibly win prizes in one of three sizes: small (worth about $1.00), large (worth about $20.00), and jumbo (worth about $100.00). In a variety of studies with numerous patient populations, prize CM decreased drug use (Peirce et al., 2006; Petry, Alessi, Marx, Austin, & Tardif, 2005; Petry, Martin, Cooney, & Kranzler, 2000; Petry, Martin, & Simcic, 2005; Petry, Peirce, et al., 2005).
In terms of increasing attendance, studies also have found favorable effects of this prize-based procedure. In a randomized study with cocaine-dependent methadone maintenance patients (Petry, Martin, & Simcic, 2005), those who received prize-based CM for submission of cocaine-negative urine samples and attendance at group therapy sessions (according to two separate schedules) significantly reduced cocaine use and attended more group therapy sessions (6.6 ± 4.0 sessions) than patients in a standard care condition (3.0 ± 0.5 sessions). However, in a study at community-based drug-free clinics, effects of prize CM were significant for reducing drug use, but CM was only modestly effective for improving attendance (Alessi, Hanson, Wieners, & Petry, 2007). Sigmon and Stitzer (2005) implemented prize CM for therapy attendance in a methadone clinic. Patients enrolled during the CM phase of the study could earn up to $160 for attending all scheduled sessions. Prize CM resulted in a significant increase in attendance from 52% ± 5% in the no-incentive phase to 76% ± 4% during CM. In a reversal design conducted at an HIV drop-in center (Petry, Martin, & Finocche, 2001), we likewise found that provision of prizes for group therapy attendance significantly increased the number of patients attending groups.
Although these investigations have largely demonstrated the efficacy of prize- and voucher-based interventions for improving treatment attendance, few studies have evaluated CM when implemented by community-based clinicians. Most studies relied on research assistants to implement the intervention. Thus, the purpose of the current study was to investigate the effectiveness of CM when applied by clinicians in community-based clinics. Four non-research-based clinics throughout the country participated in this project with only very limited and distal initial training by researchers. We hypothesized that patients who were enrolled in treatment while CM was in effect would attend more sessions than patients who received no CM treatment.
Method
Participants
Participants (N = 75) were patients entering treatment at one of four drug-free (nonmethadone) substance abuse clinics that provided weekly outpatient group therapy. Clinics were located in Maine, Vermont, and Illinois (two clinics). Participants provided written informed consent, and this study received approval from the University of Connecticut School of Medicine Institutional Review Board and other local boards when applicable. Between 10 and 26 participants were recruited at each treatment site (10 at Site A, 23 at Site B, 26 at Site C, and 16 at Site D), and these numbers reflect all attendees at the designated groups over the 40-week study period with the exception of 10 people. All patients who entered the groups were invited to participate in the study, but at two sites, the local IRBs required that any participant who reported gambling problems be excluded, and 2 such individuals were excluded. Eight patients refused to participate, all of whom began treatment during a non-CM phase.
Data Collection
Data were abstracted from patient charts, including sex, race, age, education, employment, marital status, and substance abuse problems for which patients were seeking treatment. In addition, the number and dates of therapy sessions patients were expected to attend and that were actually attended were recorded. From these records, we calculated the percentage of weeks attended for CM and non-CM phases, the primary outcome variable.
Treatment Phases
The study was conducted in three phases at four clinics. Prior to initiating the study, one of the authors provided a 3-hr training session on CM and research consent procedures to therapists at each site. Therapists were instructed on how to monitor attendance and conduct the CM procedure. Training in CM consisted of a didactic lecture that addressed current research in CM, details on providing prize CM in a group setting, instruction on implementation of the current protocol, procedures for record keeping and completing the forms used in the study, and role-play practice of CM scenarios. Specifically, during the initial didactic presentation, the presenter conducted a PowerPoint presentation that lasted approximately 1 to 1.5 hr. The presenter began the presentation by describing the basic behavioral principles of CM and the theoretical rationale behind this intervention. The presenter then discussed several classic studies in which CM was applied as an intervention to reduce substance use. In most cases, the presenter then conducted a mock demonstration CM session for the therapists. Depending on the size of the training group, the presenter then led the therapists in role-play scenarios, and the therapists practiced CM scenarios while the presenter provided feedback. The therapists also received instruction in completing recording forms during the practice session. Finally, the presenter met with the group to address any questions or concerns that arose during the role-play sessions. In addition, researchers provided funds ($1,200.00 per clinic) for therapists to purchase prizes in CM phases described below, and research staff provided some assistance in purchasing prizes by shopping for the first batch of prizes to be used during the CM phase.
The first 8 weeks of the study consisted of standard treatment. During this baseline phase, all patients beginning groups were asked to participate in the study at the time they initiated treatment, and investigators reviewed consent and attendance tracking procedures on a weekly basis to ensure appropriate study implementation. This first baseline phase was followed by two 16-week treatment phases. One 16-week phase was a standard treatment phase, and the other 16-week phase was a standard treatment plus CM phase. Both phases were presented in a random order (i.e., by flip of a coin) at each of the four clinics. Clinics A, C, and D received the standard treatment phase first followed by the CM phase, whereas Clinic B received conditions in the reverse order.
Standard Treatment Plus Monitoring
During this phase, patients received standard treatment as usual at the clinic. This included weekly group sessions addressing relapse prevention, substance use, HIV risk, relationship issues, and cognitive behavioral therapy.
Contingency Management
Patients received standard treatment as usual at the clinic during the CM phase. However, patients in treatment during this phase also received chances to win prizes for coming to treatment. Patients' names were written on a piece of paper and placed in a bowl during the group session held each week, if they attended. Participants had one opportunity each week to attend a group meeting in which they could win prizes. Names of each attendee went into the bowl once, plus a bonus number of times that depended on how many weeks in a row they had attended. For example, a patient's name went into the bowl a total of two times for 2 weeks in a row of attendance, three times for 3 weeks in a row of attendance, and so on, up to a maximum of 16 times for patients who were enrolled in Week 1 of the CM phase and attended all 16 weeks. Unexcused absences resulted in a reset to one bonus slip for the next week of full attendance. Excused absences (sickness, court appearances) that were approved by the counselor did not reset the bonus slips earned for the next group session.
During the group session, five names were drawn from the bowl. The first 4 patients whose names were drawn were allowed to draw once from a prize bowl. The 5th patient whose name was drawn was allowed to draw from the bowl five times. Patients could have their names pulled more than once during the group session if they attended more than 1 week in a row. The bowl from which winners drew contained 100 slips of paper. Of these slips, 69 stated “small prize!” A small prize was worth about $1.00 and included items such as bus tokens, gift certificates to fast food restaurants, socks, toiletries, and so on. Thirty of the slips stated “large prize!” and consisted of items worth about $20.00. Examples included watches, portable stereos, sweatshirts, pot and pan sets, coffee makers, and gift certificates to movie theaters, popular clothing stores, and so on. One slip stated “jumbo prize!” and was worth about $80.00 to $100.00. It included prizes such as TVs, boom boxes, or DVD players. The counselor who conducted drawings brought a stock of popular small, large, and jumbo items to each group session. If a patient did not like the items brought, he or she was allowed to exchange the item with the counselor after the session.
Patients were required to be in the group room on time to be eligible for drawings. That is, if they entered the room after all the other names were placed in the bowl, they were not eligible to win the draw that day (but lateness did not reset their bonuses for the next week's group session, even if they were too late to draw for prizes on that day). One week before the CM phase was due to stop, all patients were informed of the ending of CM.
Data Analysis
Analyses were conducted on an intent-to-treat basis using all patients who consented to participate in the study. Because an open group design was used, some patients who began treatment during a non-CM phase went on to receive CM when the CM phase went into effect, others started during a CM phase but may have only had a few CM groups before the phase switched to non-CM; thus, in both cases they were exposed to both phases. Other participants were exposed to only the CM or the non-CM phase. Similar to Sigmon and Stitzer (2005), who used an analogous open group design, our primary analysis focused on data from participants who were exposed to only one treatment type (i.e., CM only vs. non-CM only) in a between-participants analysis. We initially compared participants who received no CM and those who received only CM on demographic and substance use characteristics using independent sample t tests or chi-square tests. Analysis of variance (ANOVA) compared groups with respect to the primary dependent variable—percentage of sessions attended relative to the number of sessions the patient could have attended (i.e., based on treatment discharge date). Any session not attended by the patient was considered missed, unless the session was cancelled by the therapist (a rare event that occurred in less than 7% of expected attendances, e.g., on holidays). The attendance variable was square root transformed to correct for skewness, and treatment site was included as a fixed factor in the analysis. Because one site (A) had only 1 patient who was exposed to only the non-CM phase and no patients exposed to CM only, data from this site were not included in these analyses.
We separately examined data from participants who were exposed to both treatment phases (n = 24) using a within-participant ANOVA, again with treatment site as a fixed factor. Using the full sample of 75 participants, we also compared the number of patients in groups during CM and non-CM conditions to see if this variable differed by phase and by site. Finally, we calculated the total number of draws each patient received and the total dollar amount of prizes received for each patient who attended at least one CM session. One site (Site C) mistakenly provided $5.00 small prizes instead of $1.00 prizes. However, this site was retained in the analyses, because this error appears to have had limited impact on group comparisons.
Results
In total, 75 patients participated in this study, consisting of 45.3% (n = 34) men and 54.7% (n = 41) women. The mean age (SD) was 38.0 ± 12.0 years. Most (93%, n = 67) were Caucasian, 5.5% (n = 4) were African American, and 1.4% (n = 1) was Native American. Twenty-three percent (n = 16) were married or cohabiting, and about one third were employed full time. Mean (SD) years of education were 12.6 ± 1.8. Most patients were seeking treatment for alcohol problems, although other drug use was also common. Most baseline variables did not differ between those who attended only during the CM phase and those who only attended during the non-CM phase (Table 1). Even though patients who received CM only were more likely to present with cocaine problems, those presenting with cocaine problems did not differ from those presenting with noncocaine problems with respect to treatment attendance, t(51) = 0.41, p = .53. Thus, this variable was not included as a covariate in subsequent analyses.
Table 1.
Demographic and Substance Use Variables
| Variable | Both CM and non-CM (n = 24) | CM treatment onlya (n = 25) | No CM treatment onlya (n = 26) | No CM vs. CM only |
| Age M (SD) | 42.9 (13.9) | 37.0 (9.5) | 34.2 (11.0) | t (49) = −0.93, p = .33 |
| Gender: Women % | 62.5 (15 of 24) | 56.0 (14 of 25) | 46.1 (12 of 26) | χ2 (1, N = 51) = 0.49, p = .48 |
| Race % | χ2 (2, N = 48) = 2.83, p = .24 | |||
| Caucasian | 100 (24 of 24) | 81.8 (18 of 22) | 96.2 (25 of 26) | |
| African American | 0 (0 of 24) | 13.6 (3 of 22) | 3.8 (1 of 26) | |
| Native American | 0 (0 of 24) | 4.5 (1 of 22) | 0 (0 of 26) | |
| Marital % | χ2 (2, N = 47) = 5.56, p = .06 | |||
| Married or cohabiting | 25.0 (6 of 24) | 9.5 (2 of 21) | 38.5 (10 of 26) | |
| Single or never married | 29.2 (7 of 24) | 52.4 (11 of 21) | 42.3 (11 of 26) | |
| Separated or divorced | 45.8 (11 of 24) | 38.1 (8 of 21) | 19.2 (5 of 26) | |
| Employed full time % | 33.3 (8 of 24) | 32.0 (8 of 25) | 38.5 (10 of 26) | χ2 (1, N = 51) = 0.23, p = .63 |
| Years of education M (SD) | 12.3 (2.4) | 12.7 (1.8) | 12.8 (1.4) | t (49) = 0.20, p = .84 |
| Substance use problemb % | ||||
| Alcohol | 100 (16 of 16) | 87.5 (21 of 24) | 79.2 (19 of 24) | χ2 (1, N = 48) = 0.60, p = .44 |
| Cocaine | 18.1 (2 of 11) | 50 (11 of 22) | 15 (3 of 20) | χ2 (1, N = 42) = 5.78, p < .05 |
| Opioid | 8.3 (1 of 12) | 14.3 (3 of 21) | 21.1 (4 of 19) | χ2 (1, N = 40) = 0.32, p = .57 |
| Cannabis | 27.3 (3 of 11) | 47.6 (10 of 21) | 31.6 (6 of 19) | χ2 (1, N = 40) = 1.07, p = .30 |
| Other drug | 0 (0 of 11) | 14.3 (3 of 21) | 10.5 (2 of 19) | χ2 (1, N = 40) = 0.13, p = .72 |
| More than one substance | 44.4 (4 of 9) | 61.9 (13 of 21) | 36.8 (7 of 19) | χ2 (1, N = 40) = 2.51, p = .11 |
Note. Numbers in parentheses include the total number (data available from chart review) from which percentage values were calculated.
Comparisons are between participants who received no CM and those who received CM only.
Due to interclinic differences in charting, some data on substance use problems are not available.
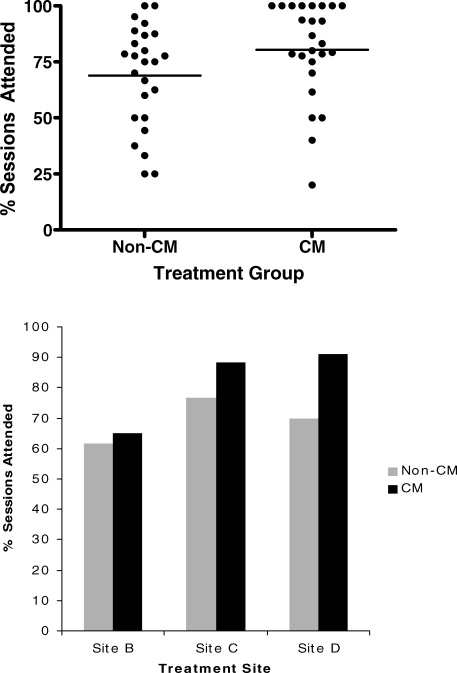
Patients who were enrolled in treatment only during the CM phase attended a significantly greater percentage of sessions (M = 80.4%, SD = 21.7%) than patients who were enrolled only during the non-CM phases (M = 68.9%, SD = 22.8%), F (1, 44) = 5.26, p ≤ .05. Individual data are presented in the top panel of Figure 1. Site effects, F (2, 44) = 4.50, p ≤ .05, were also statistically significant and are presented in the bottom panel of Figure 1, showing that some sites (e.g., C and D) had better overall attendance rates than others. The Site by CM Exposure interaction term was not significant, F (2, 44) = 1.15, p = .33, indicating that effects of CM did not differ by site.
Figure 1.
Percentage of sessions attended for patients who were exposed to either non-CM or CM treatment phases across treatment site. Top: Dots represent individual data points and horizontal lines represent means. Bottom: group data across sites. Note that Site A is not included because only 1 participant was exposed to only one of the treatment phases only.
The within-participant analysis that examined patients who were enrolled in both CM and non-CM phases (n = 24) did not find a significant main effect for treatment phase, F (1, 20) = 0.0, p = .96. However, the Site by Phase effect interaction fell just short of significance, F (3, 20) = 2.79, p = .067. Individual data are presented in the top panel of Figure 2. The bottom panel of Figure 2 shows that participants at one treatment site with relatively high treatment attendance during the non-CM phase (Site D) experienced a trend toward lower attendance during the CM phase. By contrast, participants in a clinic with relatively lower attendance during non-CM (Site A) evidenced a trend toward greater attendance during the CM phase.
Figure 2.
Percentage of sessions attended for patients who were exposed to both non-CM and CM treatment phases across treatment site. Top: Dots represent individual data points and horizontal lines represent means. Bottom: group data across sites.
Sites differed significantly in terms of the mean (SD) number of patients attending each week during the CM phase: Site A was 7.5 ± 0.9, Site B was 4.9 ± 1.8, Site C was 6.1 ± 1.5, and Site D was 5.4 ± 1.3 patients each week; F (3, 60) = 10.58, p = .001. Specifically, Site A had significantly larger groups than Sites B and D (for both Scheffe post hoc p ≤ .05). However, this site, as noted in the bottom panel of Figure 2, was the site that showed the largest difference in attendance rates across treatment phases in the between-participants analyses. Thus, it is unlikely that larger group size adversely affected patients' perceived chances of winning prizes during CM. Indeed, the cross-site differences in group size were likely inherent regardless of the implementation of CM, in that this site also had the largest mean (SD) group size during non-CM: Site A was 5.5 ± 1.5, Site B was 1.8 ± 1.3, Site C was 5.1 ± 1.3, Site D was 5.1 ± 1.7; F (3, 56) = 22.95, p = .001. Site B had significantly lower attendance rates than Sites A, C, and D per Scheffe post hoc analyses, ps ≤ .05.
CM-treated patients received a mean of 11.9 draws from the bowl, resulting in 8.5 smalls, 3.4 larges, and 0.1 jumbos. Patients selected a mean of $82.78 worth of prizes in total. Prize amounts differed by treatment site, with mean prize amounts ranging from $56.10 per person to $122.33 per person, but this difference did not reach statistical significance, F (3, 45) = 1.66, p = .19. The overall cost of the 16-week CM intervention ranged from $739.35 to $1,120.71 per clinic, with a mean cost of $1,016.52 ± $184.98.
Discussion
Patients enrolled in substance abuse treatment only during the time prize CM was in effect attended a greater percentage of their weekly sessions than patients who were engaged in treatment only while CM was not available. This finding is consistent with many studies of prize (Petry et al., 2001; Petry, Martin, & Simcic, 2005; Sigmon & Stitzer, 2005) and voucher CM for attendance (Lussier et al., 2006). However, as we noted earlier, not all investigations have found that CM significantly improves attendance (Alessi et al., 2007; Jones et al., 2000; Rhodes et al., 2003; Svikis et al., 1997), and in our subset of 24 patients who were exposed to both CM and non-CM conditions, we did not find a main effect for CM on attendance. Nonsignificant findings may be due to small sample sizes, low magnitudes of reinforcement available, high baseline attendance rates, or a combination of these factors. Results from our between-participants analyses, nevertheless, showed that prize CM can have a moderate effect on improving attendance rates.
This study also demonstrates that community-based substance abuse clinicians can effectively implement prize CM for attendance. Only minimal training (one training session approximately 3 hr in duration) was provided prior to initial implementation. Research staff reviewed all prize drawing records at the end of the study, and no deviations from protocol were noted with respect to number of slips provided or draws given. Further, the expected proportions of small, large, and jumbo slips were drawn and prizes awarded. Thus, this CM procedure was easy to train and implement correctly, with the exception that one clinic mistakenly purchased small prizes at a larger than intended magnitude.
Even though CM for attendance may be relatively easy to train and implement, it is rarely used in community-based settings (e.g., McGovern, Fox, Xie, & Drake, 2004). Willenbring et al. (2004) found that clinicians reported several barriers to implementing CM, including lack of skills or knowledge (57.5%), lack of staff time (54.8%), low demand or priority (50.9%), lack of administrative support (39.9%), and lack of confidence in the effectiveness of CM (35.1%). Thus, there is a need for greater transfer of efficacious substance abuse treatment technologies such as CM to community providers. Dissemination studies such as this one, showing the benefits of CM in real-world clinics, may assist in bridging the gap between clinical service and research.
In this study, a research grant provided the training and the prizes free of charge to the clinics. Further adaptation and integration of the approach in community settings are needed. Cost-effectiveness evaluations are also beginning to address economic aspects of CM (Olmstead, Sindelar, & Petry, 2007; Sindelar, Olmstead, & Peirce, 2007). Data from the current study suggest that fairly low-cost CM interventions can increase attendance, which in turn, may increase reimbursement rates to the clinics. Moreover, some prizes could be solicited via donations, further reducing the up-front costs of the procedures (e.g., Amass & Kamien, 2004).
Despite these positive effects, our study has several limitations. We implemented CM in treatment groups in the community with open enrollment, in which random assignment of patients was not possible because the clinics did not have sufficient patient enrollment, therapists, or space to conduct simultaneous groups that varied only with respect to CM. Thus, we cannot make definitive conclusions about the efficacy of CM for attendance. Further, aside from inspection of attendance and prize record keeping by the treatment providers, we did not include any fidelity measures to examine how well CM was presented and implemented by the clinicians. Given that CM does appear to be associated with greater attendance, it seems logical that greater scrutiny may result in even better outcomes.
Regardless of these limitations, this study also has some important strengths. Patients were recruited from several treatment settings across the country, and they all received group-based substance abuse treatment, both standard and CM, from community providers. This study, therefore, has high external validity. Implementation of this relatively low-cost ($60.00 per week) prize-based CM intervention into group therapy in non-research-based clinics is associated with improved attendance. These results call for further adoption and implementation of CM in community-based substance abuse treatment settings.
Acknowledgments
This study and preparation of this report were supported by Grants R01-DA16855, R01-DA018883, R01-DA14618, R01-DA13444, P50-DA09241, and P50-AA03510 from the National Institutes of Health and Joe Young Sr. funds from the state of Michigan. We especially thank Michael Boyle, Gail Bowlin, Dee Coon, Glen Covert, Kathy Duhamel, Barbara Haynes, Lora McManus, Kathy Nelson, Margaret O'Hagan-Lynch, Fred Savinelli, William Shakespeare, Heather Wilkin, Barb Worsfold, and Kelli Wright for their support and assistance on this project. We are also grateful to the clinics that participated in the study.
References
- Alessi S.M, Hanson T, Wieners M, Petry N.M. Low-cost contingency management in community clinics: Delivering incentives partially in group therapy. Experimental and Clinical Psychopharmacology. 2007;15:293–300. doi: 10.1037/1064-1297.15.3.293. [DOI] [PubMed] [Google Scholar]
- Amass L, Kamien J. A tale of two cities: Financing two voucher programs for substance abusers through community donations. Experimental and Clinical Psychopharmacology. 2004;12:147–155. doi: 10.1037/1064-1297.12.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn I.M, Dallery J. Effects of internet-based voucher reinforcement and a transdermal nicotine patch on cigarette smoking. Journal of Applied Behavior Analysis. 2007;40:1–13. doi: 10.1901/jaba.2007.40-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmus T.C, Saules K.K, Schoener E.P, Roll J.M. Reinforcement of counseling attendance and alcohol abstinence in a community-based dual-diagnosis treatment program: A feasibility study. Psychology of Addictive Behaviors. 2003;17:249–251. doi: 10.1037/0893-164X.17.3.249. [DOI] [PubMed] [Google Scholar]
- Higgins S.T, Petry N.M. Contingency management: Incentives for sobriety. Alcohol Research & Health. 1999;23:122–127. [PMC free article] [PubMed] [Google Scholar]
- Jones H.E, Haug N.A, Stitzer M.L, Svikis D.S. Improving treatment outcome for pregnant drug-dependent women using low-magnitude voucher incentives. Addictive Behaviors. 2000;25:263–267. doi: 10.1016/s0306-4603(98)00119-1. [DOI] [PubMed] [Google Scholar]
- Lefforge N.L, Donohue B, Strada M.J. Improving session attendance in mental health and substance abuse settings: A review of controlled studies. Behavior Therapy. 2007;38:1–22. doi: 10.1016/j.beth.2006.02.009. [DOI] [PubMed] [Google Scholar]
- Lussier J.P, Heil S.H, Mongeon J.A, Badger G.J, Higgins S.T. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- McGovern M.P, Fox T.S, Xie H, Drake R.E. A survey of clinical practices and readiness to adopt evidence-based practices: Dissemination research in an addiction treatment system. Journal of Substance Abuse Treatment. 2004;26:305–312. doi: 10.1016/j.jsat.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Olmstead T.A, Sindelar J.L, Petry N.M. Cost-effectiveness of prize-based incentives for stimulant abusers in outpatient psychosocial treatment programs. Drug and Alcohol Dependence. 2007;87:175–182. doi: 10.1016/j.drugalcdep.2006.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peirce J.M, Petry N.M, Stitzer M.L, Blaine J, Kellogg S, Satterfield F, et al. Effects of lower-cost incentives on stimulant abstinence in methadone maintenance treatment: A National Drug Abuse Treatment Clinical Trials Network study. Archives of General Psychiatry. 2006;63:201–208. doi: 10.1001/archpsyc.63.2.201. [DOI] [PubMed] [Google Scholar]
- Petry N.M, Alessi S.M, Marx J, Austin M, Tardif M. Vouchers versus prizes: Contingency management for treatment of substance abusers in community settings. Journal of Consulting and Clinical Psychology. 2005;73:1005–1014. doi: 10.1037/0022-006X.73.6.1005. [DOI] [PubMed] [Google Scholar]
- Petry N.M, Martin B, Cooney J.L, Kranzler H.R. Give them prizes and they will come: Contingency management for treatment of alcohol dependence. Journal of Consulting and Clinical Psychology. 2000;68:250–257. doi: 10.1037//0022-006x.68.2.250. [DOI] [PubMed] [Google Scholar]
- Petry N.M, Martin B, Finocche C. Contingency management in group treatment: A demonstration project in an HIV drop-in center. Journal of Substance Abuse Treatment. 2001;21:89–96. doi: 10.1016/s0740-5472(01)00184-2. [DOI] [PubMed] [Google Scholar]
- Petry N.M, Martin B, Simcic F. Prize reinforcement contingency management for cocaine dependence: Integration with group therapy in a methadone clinic. Journal of Consulting and Clinical Psychology. 2005;73:354–359. doi: 10.1037/0022-006X.73.2.354. [DOI] [PubMed] [Google Scholar]
- Petry N.M, Peirce J, Stitzer M, Blaine J, Roll J.M, Cohen A, et al. Effects of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs: A National Drug Abuse Treatment Clinical Trials Network study. Archives of General Psychiatry. 2005;62:1148–1156. doi: 10.1001/archpsyc.62.10.1148. [DOI] [PubMed] [Google Scholar]
- Prendergast M, Podus D, Finney J, Greenwell L, Roll J.M. Contingency management for treatment of substance use disorders: A meta-analysis. Addiction. 2006;101:1546–1560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- Rhodes G.L, Saules K.K, Helmus T.C, Roll J, BeShears R.S, Ledgerwood D.M, et al. Improving on-time counseling attendance in a methadone maintenance program: A contingency management approach. American Journal of Drug and Alcohol Abuse. 2003;29:759–773. doi: 10.1081/ada-120026259. [DOI] [PubMed] [Google Scholar]
- Sigmon S.C, Stitzer M.L. Use of a low-cost incentive intervention to improve counseling attendance among methadone-maintained patients. Journal of Substance Abuse Treatment. 2005;229:253–258. doi: 10.1016/j.jsat.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Sindelar J.L, Olmstead T.A, Peirce J.M. Cost-effectiveness of prize-based contingency management in methadone maintenance treatment programs. Addiction. 2007;102:1463–1471. doi: 10.1111/j.1360-0443.2007.01913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Easton C, Renee-Aubin L, Carroll K.M. Engaging young probation referred marijuana-abusing individuals in treatment: A pilot trial. American Journal on Addictions. 2003;12:314–323. [PubMed] [Google Scholar]
- Svikis D.S, Lee J.H, Haug N.A, Stitzer M.L. Attendance incentives for outpatient treatment: Effects in methadone- and nonmethadone-maintained pregnant drug dependent women. Drug and Alcohol Dependence. 1997;48:33–41. doi: 10.1016/s0376-8716(97)00101-4. [DOI] [PubMed] [Google Scholar]
- Willenbring M.L, Kivlahan D, Kenny M, Grillo M, Hagedorn H, Postier A. Beliefs about evidence-based practices in addiction treatment: A survey of Veterans Administration program leaders. Journal of Substance Abuse Treatment. 2004;26:79–85. doi: 10.1016/S0740-5472(03)00161-2. [DOI] [PubMed] [Google Scholar]