Abstract
Robust evidence has accumulated showing that individuals who develop schizophrenia are at elevated risk when compared to the general population to engage in violence towards others. This violence impacts negatively on victims as well as perpetrators and poses a significant financial burden to society. It is posited that among violent offenders with schizophrenia there are three distinct types defined by the age of onset of antisocial and violent behaviour. The early starters display a pattern of antisocial behaviour that emerges in childhood or early adolescence, well before illness onset, and that remains stable across the lifespan. The largest group of violent offenders with schizophrenia show no antisocial behaviour prior to the onset of the illness and then repeatedly engage in aggressive behaviour towards others. A small group of individuals who display a chronic course of schizophrenia show no aggressive behaviour for one or two decades after illness onset and then engage in serious violence, often killing, those who care for them. We hypothesize that both the developmental processes and the proximal factors, such as symptoms of psychosis and drug misuse, associated with violent behaviour differ for the three types of offenders with schizophrenia, as do their needs for treatment.
Keywords: violence, schizophrenia, aggression
1. Violent criminal offending among persons with schizophrenia
There is now robust evidence demonstrating that both men and women with schizophrenia1 are at elevated risk when compared to the general population to be convicted of non-violent criminal offences, at higher risk to be convicted of violent criminal offences, and at even higher risk to be convicted of homicide (Wallace et al. 2004). For example, we examined a birth cohort composed of all the 358 180 persons born in Denmark from 1944 to 1947 followed until they were in their mid-forties. We excluded those who had died or emigrated before the end of the follow-up period. The official criminal records of cohort members who had been admitted to a psychiatric ward at least once with a discharge diagnosis of schizophrenia were compared with those with no psychiatric admissions. The risk of a violent crime was elevated 4.6 (3.8–5.6) times among the men and 23.2 (14.4–37.4) times among the women with schizophrenia when compared with those with no admissions to a psychiatric ward (Brennan et al. 2000). Similar elevations in risk have been documented among persons with schizophrenia identified in other birth and populations cohorts (Hodgins 1992; Tiihonen et al. 1997; Arseneault et al. 2000; Wallace et al. 2004). While fewer women than men, with and without schizophrenia, are convicted of crimes, schizophrenia confers a greater risk for offending among women than among men.
This association between schizophrenia and violent offending is robust: it has been observed by different research teams who recruited samples from countries with different cultures and health and justice systems, and who measured the association of schizophrenia and offending using different experimental designs including longitudinal investigations of birth and population cohorts, comparisons of people with schizophrenia and their neighbours, and diagnostic studies of random samples of convicted offenders. There is no evidence to suggest that the elevated rates of violent offending among persons with schizophrenia when compared to the general population result from discrimination on the part of the criminal justice systems in the different countries where these investigations have been conducted (for a discussion, see Hodgins & Janson 2002). It is important to note that these convictions result from crimes that have been committed in the community and not in psychiatric wards, where aggressive behaviour towards others rarely, if ever, leads to criminal prosecution.
Results of the epidemiological investigations are consistent in showing that the proportions of persons with schizophrenia who commit crimes vary from one study to another, while the elevations in risk among those with schizophrenia when compared to the general population are similar (Hodgins 1998). In countries with high rates of violent crimes, proportionately more individuals with schizophrenia have convictions for violent crimes than in a country with lower rates of violent crimes. This observation suggests that at least some of the factors that contribute to violent crime in the general population also influence violent crime among persons with schizophrenia. The proportions of persons with schizophrenia who acquire convictions for violent crimes also varies by time period, reflecting differences in policies regarding diversion of mentally ill persons accused of crimes from the justice system to the health system (for further discussion, see Hodgins & Janson 2002). Most violent offences committed by persons with schizophrenia are assaults. While homicides attract much attention from the media, they are rare. In some countries, all persons accused of homicide undergo thorough psychiatric evaluations prior to trial. These evaluations have been used to estimate the proportion of homicides that are committed by individuals with schizophrenia and estimates vary from 6 to 28%, indicating substantial variation from one country to another and within countries by time period (Erb et al. 2001). Because the number of homicides varies greatly from one country to another while the prevalence of schizophrenia is relatively stable at just less than 1%, the numbers of persons with schizophrenia who commit homicides differs across countries. Thus, the proportion of persons with schizophrenia who engage in violence varies by place and time period, but evidence shows that it always remains higher than the proportion of offenders in the general population.
2. Why does it matter?
The findings reported above reflect a huge amount of human suffering, on the part of the victims and their families, and on the part of the perpetrators. Schizophrenia is a devastating illness that, in most cases, limits most aspects of functioning through adult life (Mueser & McGurk 2004). The evidence now shows that some of those who are stricken with this brain disorder present a propensity for engaging in aggressive behaviour towards others which leads to further negative consequences. In addition, individuals with schizophrenia are more likely than the general population to be the victims of crime (Teplin et al. 2005), and particularly of assaults, and one of the strongest predictors of physical victimization is their own aggressive behaviour (Walsh et al. 2003; Silver et al. 2005; Hodgins et al. 2007). Violent crimes committed by persons with schizophrenia matter also owing to the associated financial burden they place on society. Studying violence2 among persons with schizophrenia will inform the development of treatments and prevention programmes aimed at reducing such behaviours and, perhaps, further understanding of the brain mechanisms involved in aggressive behaviour.
People with schizophrenia are commonly perceived as unpredictable and dangerous (Crisp et al. 2005), with public fears outweighing the actual risk of being injured by an individual with severe mental illness (Steadman et al. 1998). Public perceptions of dangerousness, regardless of their accuracy, play a central role in fostering stigma (Link et al. 1987). Consequently, violence committed by some individuals with severe mental illness promotes stigmatization and rejection of all persons with severe mental illness. Stigmatization may affect diagnostic decision making and treatment (Walsh & Fahy 2002; Clark & Rowe 2006), pose barriers to recovery and integration in the community, and compromise quality of life (Link & Pelham 2006).
3. Implications of violent offending among persons with schizophrenia
Treatment of persons with schizophrenia which successfully reduced aggressive behaviour would contribute to lowering rates of violent criminality. As noted above, it would reduce not only the homicide rate but also the rate of other forms of violence. For example, in the Danish cohort described above, 2.2% of the men had severe mental illness and they committed 8.4% of the physically aggressive sex offences, 9.0% of the non-physically aggressive sex offences, and in all they comprised 8.1% of the sex offenders (Alden et al. 2007).
Given the numbers of persons with schizophrenia who engage in violent criminal offending, there are important consequences for both the health and criminal justice systems. Adult mental health services provide care for a subgroup of individuals with schizophrenia who present high levels of violent behaviour. For example, we recently assessed a sample of 205 inpatients with severe mental illness from a UK inner city mental health trust, most of whom suffered from schizophrenia. The patients were, on average, in their late thirties and more than 80% had previously required inpatient care. Official criminal records indicated that 46.7% of the men and 16.5% of the women had at least one conviction for a violent crime, and on average the violent offenders had each been convicted of more than two crimes. The 82 men with criminal records had committed 1792 crimes and the 23 female offenders had committed 458 crimes (Hodgins et al. 2007). The risks of conviction in this UK inner city sample of patients when compared to the general UK population were similar to those observed in comparisons of severely mentally ill inpatient and general population samples in Sweden and Denmark. This subgroup of patients with a history of violence presents a challenge to general mental health services. Some of these patients are transferred to forensic inpatient services that have dramatically increased in capacity, not only in the UK, but also in several other European countries (Priebe et al. 2005). Most forensic beds are occupied by men with schizophrenia (Hodgins & Müller-Isberner 2004).
Many persons with schizophrenia are incarcerated (Davies 2004a–c). Rates vary from one country to another, and within countries from one time period to another, depending on policies designed to divert the mentally ill accused or convicted of crimes from the justice system to the health system. In studies of inmate populations, rates of schizophrenia are much higher than rates for age- and sex-matched general population samples (Fazel & Danesh 2002). Within correctional facilities, people with schizophrenia fail to obtain adequate and appropriate treatment for their illness and are frequently physically abused (Wolf et al. 2007).
Also consistent with the epidemiological evidence on the elevated rates of violent offending among persons with schizophrenia is emerging evidence that antisocial behaviour in adolescence is a precursor of schizophrenia. Robins (1966) was the first to note that a disproportionate number of adolescent delinquents subsequently developed schizophrenia. A recent study in Denmark examined a cohort composed of all the offenders aged 15–19 years in 1992. Of the 780 persons who were still alive in Denmark in 2001, 3.3% had developed schizophrenia as compared to the expected 0.7%. The odds of developing schizophrenia among those with a history of violent criminal offending (as compared to those with only non-violent offending) was 4.59 (1.54–13.74) (Gosden et al. 2005). We have compared a sample composed of all the 1992 individuals who as teenagers contacted a clinic for substance misuse in a large metropolitan area of Sweden in the years 1968–1972, and compared them with a randomly selected general population sample matched for sex, age and birthplace. By age 50, four times more males and eight times more females in the clinic than the general population sample had been hospitalized with schizophrenia (Hodgins et al. in preparation). These results are consistent with the epidemiological investigations cited above that identified antisocial behaviour prior to illness onset among a subgroup of offenders with schizophrenia (Hodgins 1992; Wallace et al. 2004).
Thus, individuals who develop schizophrenia contribute disproportionately to violent crime rates. Presently, general adult mental health services fail to assess and manage their risk of violence or to provide them with treatments designed to reduce violent behaviour. More and more of these individuals are being transferred to costly forensic inpatient services (Hodgins & Mu¨ller-Isberner 2004) and are being incarcerated. Among adolescents engaging in antisocial and criminal behaviours, a disproportionate number develop schizophrenia.
4. Schizophrenia is also associated with elevated rates of aggressive behaviour towards others
An interview protocol has been developed specifically to assess aggressive behaviour2 and victimization among persons with mental disorders that combines information from patients and collateral informants (Steadman et al. 1998). Studies have shown that severely mentally ill patients report aggressive incidents at only a slightly lower rate than do collaterals (Steadman et al. 1998). In our study of a sample of UK inpatients with severe mental illness described above, 41.7% of the men and 21.2% of the women reported having engaged in at least one serious assault sometime in their life, 49.2% of the men and 38.8% of the women reported having engaged in at least one act of physical aggression against another person in the previous six months, and 21.7% of the men and 18.8% of the women reported engaging in a life-threatening act of violence against another person in the previous six months. A study of a large sample of outpatients with psychosis found that one in five assaulted another person over a 2-year period (Walsh et al. 2001). Similarly, other studies of samples of outpatients with schizophrenia report rates of any physically aggressive behaviour towards others ranging from 8 to 77% during the previous six months and rates of life-threatening violence towards others ranging from 0 to 40% (Hodgins et al. 2007). As noted previously, rates of convictions for violent crimes are lower among women than men with schizophrenia, but several studies suggest that the prevalence of aggressive behaviour is similar (Walsh et al. 2001; Dean et al. 2006; Hodgins et al. 2007). Importantly, the correlates of violent offending and of physically aggressive behaviour towards others when patients are living in the community are similar.
5. Psychotic symptoms and violence
Recent studies of large population samples indicate that psychotic symptoms are more common than previously thought (Stefanis et al. 2002). One US study revealed that 5.1% of 38132 adults reported psychotic-like experiences. The presence of psychotic-like experiences was associated with a fivefold increase in the risk of assaulting another person (Mojtabai 2006). Yet, the results of studies of the association of positive symptoms of psychosis and violent behaviour among persons with schizophrenia are contradictory (Appelbaum et al. 2000; Bjørkly 2002a,b). The lack of consistency in the evidence results primarily from methodological features of studies including retrospective assessment of symptoms and failure to take account of other factors, such as previous violence, childhood behaviour problems and intoxication, that are known to be associated with violence (Appelbaum et al. 2000; Bjørkly 2002a,b; Hodgins et al. 2003). There is some evidence that when positive symptoms are accompanied by depression or distress, the risk of aggressive behaviour is elevated, even after controlling for a previous history of antisocial behaviour3 and current and past substance misuse (Hodgins et al. 2003; Crocker et al. 2005).
However, the evidence is consistent in showing that the correlates of violent behaviour during acute episodes of psychosis among patients hospitalized on a psychiatric ward differ from the correlates of violent behaviour that occurs in the community. Many acutely psychotic patients who are in most cases admitted involuntarily to psychiatric wards behave aggressively. The aggressive behaviour declines rapidly in the days following admission. Aggressive incidents on an acute psychiatric ward are as common among women as men, and unlike aggressive behaviour that occurs in the community they are strongly associated with confusion and thought disorder (Steinert 2002; Krakowski & Czobor 2004).
Among people with schizophrenia, the lack of association between aggressive behaviour and positive symptoms of psychosis is not surprising if considered in light of evidence that psychosocial functioning generally is not associated with positive symptoms. Aggressive behaviour reflects a lack of interpersonal skills or simply one aspect of psychosocial functioning. Interpersonal skills, community activities and work skills are most strongly associated with performance on neuropsychological tests, negative symptoms and depression, and not with positive symptoms (Bowie et al. 2006). We assessed psychosocial functioning among 248 men with schizophrenia living in the community that we had recruited from forensic and general psychiatric services. Psychosocial functioning was defined to include measures of independent living, occupational functioning, social and leisure activities, and the absence of aggressive behaviour, substance misuse and self-harm. We found that psychosocial functioning was associated with two static predictors—level of education and past diagnoses of substance misuse disorders—and three current predictors—depression, non-compliance with antipsychotic medication and experiences of physical victimization (Hodgins et al. submitted). The results of this study confirmed findings from previous investigations showing that factors other than positive symptoms are most strongly associated with real-life functioning among persons with schizophrenia.
Our study, however, did not include a measure of cognitive impairment. Not only is the level of cognitive impairment a major determinant of psychosocial functioning, it is a core feature of schizophrenia. Deficits in cognitive performance characterize children and adolescents developing the illness, are present at onset of illness, remain stable over time and are largely explained by genetic factors (Cannon & Clarke 2005; Green et al. 2005; Toulopoulou et al. 2007; MacCabe et al. 2007). While individuals developing schizophrenia and those already affected perform more poorly than age-matched healthy persons on all measures of cognitive functioning, among persons with schizophrenia there is wide variation in levels of cognitive performance. Thus, if aggressive behaviour is viewed as one aspect of psychosocial functioning, then like other aspects of psychosocial functioning it too is not strongly, nor consistently, associated with positive symptoms of psychosis.
6. A typology of offenders with schizophrenia
Another reason for the inconsistent results concerning the association of psychotic symptoms and violence is that studies have compared offenders with schizophrenia to non-offenders with schizophrenia, thereby assuming that the offenders constitute a homogeneous group. The evidence, however, does not support this presumption. Among non-mentally ill offenders, findings have accumulated indicating that there are subtypes, defined by age at onset and persistence of antisocial behaviour that differ as to aetiology and response to treatment (Moffitt & Caspi 2001). Among offenders with schizophrenia, subtypes defined by age of onset and persistence of antisocial behaviour are also apparent. Consequently, studies that compare violent and non-violent offenders obscure features that distinguish subtypes of violent offenders with schizophrenia such that findings are difficult to interpret.
We have been conducting a programme of research based on the hypothesis that there are three types of offenders who differ as to the age of onset and persistence of antisocial behaviour. The early starters display a pattern of antisocial behaviour that onsets in childhood or early adolescence and which remains stable across the lifespan. They are usually convicted of crimes prior to illness onset. By contrast, a large group of violent offenders with schizophrenia show no antisocial behaviour prior to the onset of the prodrome or illness, and then repeatedly engage in aggressive behaviour towards others. A small group of individuals who display a chronic course of schizophrenia show no aggressive behaviour prior to their late thirties or early forties, and then engage in serious violence, often killing, those who care for them.
7. Early start offenders with schizophrenia
Early start offenders with schizophrenia have been defined in different ways—those with a conviction for violence prior to illness onset, those with a history of childhood conduct problems, and those who met criteria for conduct disorder (CD) prior to age 15. When compared with other offenders with schizophrenia, those with a childhood history of conduct problems defined in any of these ways are convicted for more non-violent and violent crimes (Fulwiler & Ruthazer 1999; Crocker et al. 2005; Mueser et al. 2006), commit a more diverse array of crimes (Hodgins 2004), and have criminal histories similar to those of non-mentally ill offenders who also have a childhood history of conduct problems (Hodgins & Côté 1993; Schug et al. 2007). In addition, almost all display a pattern of substance misuse going back to early adolescence (Fulwiler et al. 1997; Mueser et al. 1999; Tengström et al. 2001; Moran & Hodgins 2004).
For reasons currently not understood, CD and conduct problems are precursors of schizophrenia. For example, a prospective longitudinal investigation of a large Dutch population sample observed that aggressive behaviour in childhood is associated with thought disorder in adulthood (Ferdinand & Verhulst 1995). Similarly, a prospective investigation of a US population cohort observed that aggressive behaviour in early adolescence is associated with personality disorders that are genetically linked to schizophrenia (Bernstein et al. 1996). The prospective studies of children at risk for schizophrenia by virtue of having a close relative with the disorder, usually the mother, observed that a proportion of the males who developed schizophrenia had displayed conduct problems through childhood. The most direct and robust evidence that CD is a precursor of schizophrenia comes from a prospective investigation that followed a New Zealand birth cohort to age 26. Forty per cent of the cohort members who developed schizophreniform disorders had displayed CD prior to age 15 (Kim-Cohen et al. 2003). In clinical samples of adults with schizophrenia the prevalence of CD is lower. The CD modules of the Structured Clinical Interview for DSM-III-R and IV were designed to diagnose CD prior to age 15 retrospectively. We have used this interview protocol, in some studies supplemented by information from family members, school, social service and justice files, to diagnose CD among adults with schizophrenia. In most samples, the prevalence is approximately 20% among both women and men (Hodgins et al. 1998), but, for example, in the UK sample of inpatients described above, CD prior to age 15 characterized 42.0% of the men and 22.4% of the women (Hodgins et al. 2008). While these samples of patients with schizophrenia were recruited in general psychiatric services, among patients in forensic services the prevalence of CD is higher, and among those incarcerated it is further elevated (Hodgins et al. 1998).
CD and conduct problems are not only precursors of schizophrenia, but they are also more common among people who develop schizophrenia than in the general population. Recent estimates of the prevalence of CD prior to age 15 range from 7.5% among boys and 3.9% among girls in a large UK cohort (Green et al. 2004), to 12.0% among boys and 7.1% among girls in a US sample (Nock et al. 2006). These prevalence rates are much lower than that observed prospectively in the Dunedin study among the cohort members who developed schizophreniform disorders or among clinical samples of adults with schizophrenia. This more recent evidence is consistent with older findings from a US investigation of a population sample of 20 000 adults, in which higher rates of CD were observed among persons with, than without, schizophrenia (Robins et al. 1991), and the number of CD symptoms present prior to age 15 was found to be positively and linearly associated with the likelihood of developing schizophrenia (Robins 1993). The accumulated evidence indicates, then, that the prevalence of CD is higher among people who develop schizophrenia than in the general population, and that the gender difference is less. Thus, not only is the proportion of offenders greater in the population of persons who develop schizophrenia than in the general population, but also is the proportion of offenders who display an early onset and stable pattern of antisocial behaviour.
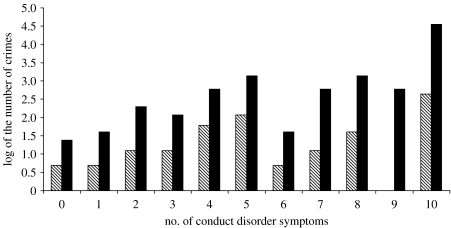
We conducted an investigation to examine the association of CD prior to age 15 and crime and aggressive behaviour among a sample of 248 men with schizophrenia who were, on average, aged 39.8 years at the time of the study (Hodgins et al. 2005). They were assessed in the two weeks prior to discharge from hospital using multiple sources of information including complete criminal records. Of them, 52 (21%) men met criteria for CD prior to age 15. Incident rate ratios (IRR) were calculated to estimate the association between CD and the number of convictions for violent crimes. CD diagnosis was associated with an increase of 2.29 (1.31–4.03) in the number of convictions for violent crimes after controlling for lifetime diagnoses of alcohol and/or drug abuse and/or dependence. Each CD symptom present before age 15 was associated with a 1.15 (1.06–1.25) increase in the number of convictions for violent crimes, again after controlling for diagnoses of substance misuse disorders. CD and CD symptoms were also associated with the number of convictions for non-violent crimes as depicted in figure 1. We have replicated these results in the sample of UK inpatients with severe mental illness described previously (Hodgins et al. 2007). In this study, after controlling for sex, age, current alcohol and drug use, CD prior to age 15 was associated with a twofold (odds ratio: 2.5, 1.17–5.36) increase in the number of convictions for violent crimes. Again, after controlling for sex, age and substance misuse, each CD symptom present before age 15 was associated with a slight increase in the number of violent crimes (odds ratio: 1.16, 1.01–1.35). Both CD diagnosis and the number of CD symptoms were also associated with the number of convictions for non-violent crimes. No sex differences in the associations of CD and later offending were detected. The results of these two studies indicate that among individuals who develop schizophrenia, as among those who do not, CD in childhood is a precursor of criminal offending in adulthood. They concur with the results from other studies that used different definitions of childhood conduct problems (Rice & Harris 1995; Fulwiler & Ruthazer 1999; Tengström et al. 2004).
Figure 1.
Number of non-violent and violent crimes as a function of the number of conduct disorder symptoms among men with schizophrenia. Hatched bars, violent crimes; black bars, non-violent crimes.
Both in the general population (Moffitt & Caspi 2001) and among people with schizophrenia, not surprisingly, CD is a precursor of aggressive behaviour, as well as violent crime. The same instrument (Steadman et al. 1998) has been used in three studies to assess aggressive behaviour among people with schizophrenia and its association with CD. In the UK sample of men and women with severe illness in their late thirties described previously, we found that after controlling for age, sex and current substance misuse, CD diagnosis prior to age 15 was associated with an increased odds of aggressive behaviour towards others in the previous six months (odds ratio: 2.66, 1.24–5.68), as was each CD symptom (odds ratio: 1.29, 1.11–1.50) (Hodgins et al. 2008).
The 248 men with schizophrenia described previously were studied for 24 months following discharge from hospital (Hodgins et al. 2005). They and an informant were interviewed at six-month intervals to document aggressive behaviour. CD was associated with an increased risk of aggressive behaviour (odds ratio: 2.39, 1.18–4.83) that remained after controlling for current substance misuse and lifetime diagnoses of alcohol abuse/dependence, but fell below significance after controlling for lifetime drug abuse/dependence diagnoses. Each CD symptom present prior to age 15 was associated with an increase in the risk of engaging in aggressive behaviour towards others after controlling for current and past substance misuse (odds ratio: 1.23, 1.09–1.40). We also undertook analyses with this sample to further investigate the role of psychotic symptoms in four six-month periods when patients were living in the community. Symptoms were measured at the beginning of each six-month period, and at the end of the period both collateral informants and patients reported on aggressive behaviour that had occurred in the previous six months. We assessed positive and negative symptoms of psychosis, three paranoid symptoms, as well as depression and anxiety, and changes in levels of these symptoms. In regression models, we first entered the presence or absence of antisocial personality disorder (APD; the adult diagnosis that requires the presence of CD prior to age 15), then current substance misuse measured by both self-report and hair and urine analyses, and then the symptoms and changes in symptoms. In the final model, the risk of aggressive behaviour was increased six times by a diagnosis of APD, and one-and-a-half times by the number of clinically relevant positive symptoms, by the change in the level of positive symptoms and by the presence of anxiety (Hodgins 2008).
Similar findings emerged from analyses of baseline data collected for a large trial of medications in the USA. While this study used the same instrument to assess aggressive behaviour as did our studies, unlike the study above symptoms were not measured prospectively but at the same time as the aggressive behaviour. More than two or more CD symptoms were found to be associated with aggressive behaviour in the previous six months after controlling for numerous confounds, and, as in our studies, there was no association with substance misuse after taking account of childhood conduct problems. While positive symptoms and depression were positively associated with life-threatening violence, negative symptoms were protective. A combination of above median scores for positive symptoms and below median scores for negative symptoms was associated with a threefold increase in risk of life-threatening violence (Swanson et al. 2006).
Thus, the accumulated evidence indicates that CD is a precursor of schizophrenia in a minority of cases, CD is more common among individuals who develop schizophrenia than in the general population, and among adults with schizophrenia, a diagnosis of CD and the number of CD symptoms present prior to age 15 are associated with violent behaviour through adulthood. While some studies do show that positive symptoms are associated with aggressive behaviour even after taking account of CD, the existing evidence indicates that those with CD are not distinguished from other patients with schizophrenia by symptom profiles (Moran & Hodgins 2004). Based on a comparison of the results of a small number of studies, the strength of the association between CD in childhood and violence in adulthood appears to be similar among individuals who develop schizophrenia (Hodgins et al. 2005, 2008; Swanson et al. 2006) as it is among those who do not (Siminoff et al. 2004; Loeber et al. 2005). In addition, the number of CD symptoms prior to age 15 is linearly associated with the development of antisocial personality disorder in adulthood among persons with schizophrenia, as it is in the general population (Robins et al. 1991).
There is little prospective research on individuals who present conduct problems in childhood and who subsequently develop schizophrenia. The lack of prospectively collected data are not surprising given the challenge of identifying the very small number of individuals with conduct problems many years before they develop schizophrenia. An important finding has emerged from the prospective longitudinal investigation of a birth cohort in Dunedin, New Zealand. As previously noted, and consistent with other epidemiological evidence, the risk of violence was elevated among cohort members who developed schizophreniform disorder by age 26. This association was partially explained by the presence of both aggressive behaviour at ages 7, 9 and 11 and psychotic-like experiences at age 11 (Arseneault et al. 2003). Most other relevant findings on the childhood characteristics of individuals with conduct problems who develop schizophrenia derive from studies of clinical samples of adults in which data on childhood are collected retrospectively from multiple sources, some objective—school, social service and juvenile justice records, and some subjective—reports from patients, parents and older siblings. For example, in our sample of 248 men with schizophrenia, we compared those with and without CD prior to age 15. More of those with, than without, CD obtained lower than average marks in elementary school, failed to graduate from secondary school, and prior to age 18 abused substances, experienced physical abuse and were institutionalized (Hodgins et al. 2005). The results of other similar studies concur (Schanda et al. 1992; Fulwiler et al. 1997; Tengström et al. 2001).
Several studies have reported that rates of mental illness among first-degree relatives did not differ for those with and without CD, while rates of criminality and substance misuse were elevated among fathers and brothers (Mueser et al. 1999; Tengström et al. 2001; Hodgins et al. 2005, 2008). Older studies had observed higher rates of criminality among the relatives of persons with schizophrenia when compared to the general population. We had hypothesized that it was the relatives of those with CD prior to illness onset who had relatives that engaged in crime (Hodgins et al. 1996b). Subsequent studies have shown that while greater proportions of parents and siblings of those with, than without, CD prior to illness onset acquired criminal convictions, the differences between the two groups are not always statistically significant. As there are no studies that compare individuals with childhood CD who do and do not develop schizophrenia, it is not possible to compare family liability in the two groups. It is known, however, that among children with CD those who go on to become persistent offenders are distinguished from the others by having more relatives who present externalizing disorders (Odgers et al. 2007).
We and others (Joyal et al. 2003; Stirling et al. 2005) have proposed that among men with schizophrenia, those with early onset persistent antisocial behaviour display fewer brain abnormalities than those without a history of antisocial behaviour. This proposition is based on evidence from studies that compare violent and non-violent patients with schizophrenia–-only a few of which distinguish early starters (for a review see Naudts & Hodgins 2006), and from studies that compare patients with schizophrenia with and without co-occurring substance misuse disorders (for a review, see Potvin et al. 2008). Results suggest that among patients with schizophrenia, those who present an early onset stable pattern of antisocial behaviour perform better on tests tapping specific executive functions (Wisconsin Card Sorting Test, Trail Making Test, WAIS, Trigram Test, Control Oral Word Association Test), more poorly on assessments of orbitofrontal functions, show fewer neurological soft signs, display larger reductions in volume of the amygdala, more structural abnormalities in the orbitofrontal system, more abnormalities of white matter in the amygdala–orbitofrontal system, and smaller reductions of the hippocampus. Thus, early start offenders with schizophrenia may be distinguished by better executive functioning, higher verbal skills and greater impulsivity than other men with schizophrenia. This evidence, however, derives from studies that examined small poorly characterized samples, and that used definitions of violence and measures of brain function and structure that varied markedly. There is only one functional magnetic resonance imaging (fMRI) study that has examined men with schizophrenia and compared those with and without CD (Joyal et al. 2007). The results of this investigation concur with the conclusions of the literature review in showing dysfunction in the orbital prefrontal cortex among those with prior CD. Dysfunction in this brain region has been associated with antisocial behaviour, and specifically with impaired inhibition, attention and lower order executive functions (Damasio 2000). Thus, cognitive impairment—a core feature of schizophrenia that strongly impacts on psychosocial functioning—may distinguish individuals who display an early onset and stable pattern of antisocial behaviour from others with the illness.
We speculate that individuals with CD who are developing schizophrenia may be characterized by lower levels of anxiety, heart rate and cortisol, similar to other children and adolescents with CD (Lorber 2004; Susman 2006; Van Goozen et al. 2007). Consequently, changes in brain function and structure resulting from the toxic effects of chronically elevated levels of cortisol and an overactive hypothalamic–pituitary–adrenal (HPA) axis would be less among those with, than without, CD. Consistent with this notion, one study recently reported that individuals with schizophrenia spectrum disorders and antisocial personality disorder (which requires CD prior to age 15) showed lower skin conductance orienting and arousal than individuals with only antisocial personality disorder or only a schizophrenia spectrum disorder (Schug et al. 2007).
8. Implications for the aetiology of schizophrenia and CD
The accumulated evidence suggests that among persons with schizophrenia, CD is directly associated with criminal offending and substance abuse that begins in adolescence and persists across the lifespan but not with the presentation of the illness. These findings may be interpreted to suggest that among persons with schizophrenia, CD is a distinct co-morbid disorder and not a consequence of abnormalities associated with the developing schizophrenia. Elevated rates of criminality and substance misuse among first-degree relatives would possibly suggest a distinct aetiology for CD. However, the robust finding that the prevalence of CD is higher among people who develop schizophrenia than in the general population indicates that there is a link between the two disorders.
Heritability estimates for schizophrenia are high, usually over 80% (Gottesman 1993). Presently, it is thought that this brain disorder develops as a result of many genes, each of which confers vulnerability, that is further enhanced by untoward events that occur during pregnancy, at birth, in early childhood and adolescence (Mueser & McGurk 2004). We have developed hypotheses to guide future research aimed at furthering understanding of the aetiological processes leading to the development of individuals with CD in childhood and adolescence and schizophrenia in adulthood.
(a) Hypothesis I
Individuals at genetic risk for schizophrenia are at increased risk to be exposed to environmental factors known to contribute to an early onset and stable pattern of antisocial behaviour.
There is robust evidence showing that an early onset and stable pattern of antisocial behaviour is also hereditary, with estimates of heritability at approximately 50% (Krueger et al. 2002; Moffitt 2005). Behavioural genetic studies concur in showing that both shared and non-shared environments contribute to antisocial behaviour, particularly in childhood (Krueger et al. 2002; Moffitt 2005). The non-genetic factors, both of those that characterize families and parents and those that characterize children, that are associated with the development of persistent antisocial behaviour may be more common among children at genetic risk for schizophrenia and their families than in the general population. Consider first factors that are active during pregnancy and at birth. There is considerable evidence indicating that among people who develop schizophrenia, foetal neural development is disrupted in the first trimester, at the end of the second trimester and at birth (Takei et al. 1995; Lane et al. 1997; Ismail et al. 2000; Buka et al. 2001; Cannon et al. 2002b). In studies of general population samples, obstetrical complications coupled with family problems (Hodgins et al. 2001), maternal smoking (Räsänen et al. 1999; Maughan et al. 2004) and drinking (d'Onofrio et al. 2007) during pregnancy have been associated with conduct problems among the offspring. All of these factors are more common among people with schizophrenia than in the general population. Only one study, to our knowledge, has assessed the association between obstetrical complications and an early onset pattern of antisocial behaviour and violence among persons with schizophrenia. In a large birth cohort, complications in the neonatal period were found to be associated with an increased risk (odds ratio: 2.79, 1.71–4.56) for violent criminal offending (Hodgins et al. 2002).
Many studies have identified characteristics of families and parents which contribute to the initiation and maintenance of antisocial behaviour. These include socioeconomic status of the family, mother's age, level of education and mental health, parenting practices, physical abuse of the child, family conflict and changes in carer (Moffitt & Caspi 2001). These characteristics have all been associated with the development of schizophrenia (Jones et al. 1994; Tienari et al. 1994; Cannon et al. 2002a; Walker et al. 2004; Read et al. 2005; Morgan et al. 2007). Furthermore, studies have shown that both mothers and fathers who themselves display antisocial behaviour engage in parenting practices that contribute to conduct problems among their offspring (Lahey et al. 1988; Frick et al. 1992; Caspi et al. 2004; Jaffee et al. 2004). Largely owing to the difficulty in identifying children who will later develop schizophrenia, there are almost no studies of parenting practices in this population. Thus, although highly speculative at this stage, we propose that individuals with CD prior to the onset of schizophrenia would experience insults in the pre- and perinatal periods resulting from maternal behaviour, and poor attachment to parents, poor parenting especially inadequate and inappropriate supervision, harsh and inconsistent discipline, and a lack of appropriate models for coping with stress.
(b) Hypothesis II
Brain and neuroendocrine abnormalities present among children who are developing schizophrenia render them vulnerable for antisocial and aggressive behaviour.
Adults with schizophrenia display both structural and functional brain abnormalities (Miyamoto et al. 2003; Mueser & McGurk 2004), some of which are observed at illness onset prior to the use of antipsychotic medication (Pantelis et al. 2005). Post-mortem studies of brains of individuals with schizophrenia, studies of obstetrical complications, studies of the consequences of disturbances in utero such as minor physical anomalies, and neurocognitive assessments in childhood of individuals who subsequently developed schizophrenia all suggest that brain abnormalities are present before illness onset (Rapoport et al. 2005). In addition, recent evidence shows that the increase in symptoms of anxiety that precedes onset in most cases is reflected in an overreactive HPA axis as indicated by levels of cortisol and increased pituitary volumes (Garner et al. 2005; Pariante et al. 2005).
Individuals who present an early onset and stable pattern of antisocial behaviour are characterized by deficits in performance in neuropsychological tests and specific features of temperament and behaviour that are observed as early as 3 years of age (Moffitt & Caspi 2001), and lower than average heart rate and cortisol levels (Moffitt & Caspi 2001; Lorber 2004; Loney et al. 2006; Susman 2006; Van Goozen et al. 2007). Children with conduct problems also present marked abnormalities in the recognition of emotions in the faces of others. For example, in one study they reported neutral faces to be hostile, consistent with their behaviour that suggests they constantly feel threatened by others (Dadds et al. 2006; Frick & Marsee 2006). The small subgroup of children with CD who also present callous–unemotional traits fail to recognize fear in the faces and voices of others (Blair et al. 2006).
In a sample of treatment-resistant patients with schizophrenia, a history of arrest was found to be associated with poor recognition of emotions, most particularly fearful faces, after adjusting for age, education, duration of illness and symptom severity. The number of arrests for violent crimes was associated with the misinterpretation of faces as fear or sadness, while aggressive behaviour was associated with misinterpreting faces as angry (Weiss et al. 2006). Adults with schizophrenia display deficits in the recognition of emotions in the faces of others (Schneider et al. 2006) that are present at illness onset and in the prodromal phase (Addington et al. 2008). Studies have also shown that the deficit characterizes many of their healthy siblings leading to the suggestion that it may signal the presence of one or more susceptibility genes for schizophrenia (Bediou et al. 2007). If such a deficit were present in childhood, it might contribute to conduct problems. For example, the failure to recognize anger in the face of adults would deprive the child of information that their behaviour was inappropriate, the failure to recognize fear in others would be associated with a lack of empathy and understanding of others (Blair et al. 2006), and a general failure to recognize emotions would be associated with problems with peers (d'Acremont & Van der Linden 2007).
Longitudinal prospective investigations suggest that children vulnerable for schizophrenia display motor delays, neurological signs, receptive language deficits and lower than average IQ scores (Cannon et al. 2002a; Cannon & Clarke 2005; Laurens et al. 2007a). These characteristics may limit learning not to be aggressive that occurs from toddlerhood through middle childhood (Broidy et al. 2003).
9. Next steps
We hypothesize that there are two distinct developmental trajectories leading to schizophrenia. The first most common pathway is characterized by emotional problems, usually anxiety, and a growing sensitivity to stress through adolescence. The second less common pathway is characterized by conduct problems and a reduced sensitivity to stress. In order to test this hypothesis, we wanted to identify children at risk for schizophrenia. Historically this has always been done by identifying children with an affected relative, usually the parent. Such a strategy, however, is limited in that the majority of adults with schizophrenia do not have an affected relative (Gottesman 1993). Consequently, we have attempted to develop a procedure for identifying at-risk children in the community. Based on a detailed review of the prospective investigations of children with an affected relative and of population cohorts that have identified the childhood characteristics of individuals who developed schizophrenia, we established a list of antecedents that had been replicated. We added to this list psychotic-like experiences that had been found by one prospective study to characterize 11-year-old children who subsequently developed schizophreniform disorder (Poulton et al. 2000). We defined a triad of antecedents of schizophrenia to include the following: (i) a carer report of motor and/or speech delay or abnormality, (ii) a child report in the clinical range for internalizing problems on the Strengths and Difficulties Questionnaire (SDQ) or a carer report in the clinical range for externalizing and peer problems of the SDQ, and (iii) a child report of at least one ‘certain’ psychotic-like experience.
Based on analyses of the first 548 children and carers screened, we found that 9.2% of the boys and 4.1% of the girls met criteria for the triad of antecedents (Laurens et al. 2007a). Furthermore, just as the prevalence of schizophrenia is elevated among persons of African-Caribbean heritage living in the UK, we found that the prevalence of the triad of antecedents was also significantly elevated among children of African-Caribbean heritage (Laurens et al. 2007b). Among the children who presented the triad of antecedents, there are distinct groups. Among the boys, 27.3% obtained scores within the clinical range of the SDQ for emotional problems but not for conduct problems, 36.4% obtained scores within the clinical range of the SDQ for conduct problems but not for emotional problems; 2.3% obtained scores within the clinical range of the SDQ for both emotional and conduct problems; and 34.1% obtained scores within the clinical range of the SDQ on another subscale, most commonly that assessing problems with peers. The comparable figures for the girls are 54.5, 18.2, 12.1 and 15.2%. Until these children pass through the age of risk for schizophrenia, we will not know how many develop the illness.
We have now screened more than 4000 children in the age group of 9–11 years, and the prevalence of the triad of antecedents remains stable. Presently, we are examining a sample of children who present the triad of antecedents, some of whom also have an affected relative and some who do not, children with an affected relative and children who have neither the antecedents of schizophrenia nor an affected relative. The children and their carers complete a diagnostic interview, the carer provides information about the family and carers, and the children complete neuropsychological tests, structural and functional brain imaging and a session to measure event-related potentials.
In addition, we are conducting further studies of adults with schizophrenia who have a history of CD in order to refine our understanding of their distinguishing features, including neurological soft signs, performance on neuropsychological tests, structural brain abnormalities and response to antipsychotic medication.
10. Type II offenders with schizophrenia
Type II offenders with schizophrenia present no history of antisocial or aggressive behaviour prior to illness onset. Thereafter, they repeatedly engage in aggressive behaviour towards others. Such a pattern of aggressive behaviour that onsets in adulthood is very rare, as almost all persistently violent offenders have a long history of antisocial and aggressive behaviour stretching back into childhood (Loeber et al. 2005; Moffitt 2006). When a pattern of aggressive behaviour onsets in adulthood, it is usually associated with some form of brain disorder (see for example, Hodgins et al. 1996a). In the sample of 248 men with schizophrenia, which we recruited from forensic and general psychiatric hospitals, we compared the offenders who did not have a childhood history of antisocial behaviour, i.e. our Types II and III, with those who did, Type I. Those without antisocial behaviour prior to illness onset, compared with those with prior CD, included similar proportions with at least one conviction for a violent crime, but, on average, they had acquired fewer convictions for violent crimes and many fewer convictions for non-violent crimes. Importantly, however, a greater proportion of patients without antisocial behaviour prior to illness onset had been convicted for a homicide (23.9%) when compared with patients with prior CD (10.4%) (X2(N=186)=3.99, p=.046). As would be expected, patients with no history of antisocial behaviour prior to illness onset were significantly older at first conviction for a violent crime than were those with prior CD.
There are few studies of patients with schizophrenia, no history of antisocial behaviour prior to illness onset, who repeatedly engage in aggressive behaviour towards others. Some evidence (Mueser et al. 1999, 2006) suggests that they may be particularly vulnerable to illicit drug use and that drug use may be directly associated with their violent behaviour. In the study described above, we found no differences in the prevalence of lifetime diagnoses of alcohol abuse and/or dependence or drug abuse and/or dependence among patients with and without antisocial behaviour prior to illness onset. Similarly, in our study of the UK inpatient sample, we found no difference in levels of substance misuse between those with and without a CD prior to age 15. Although half of the patients in this study presented a substance misuse problem, in the subsequent 2 years, 3% of the men and 5% of the women received a treatment targeting this problem. Yet, there are effective treatments for substance misuse among persons with schizophrenia (Green et al. 2007). Drug use by patients with schizophrenia puts them at risk for violence in several different ways. With impaired social cognition, such patients make contact with antisocial offenders who congregate in high-crime areas with high levels of violence in order to purchase illicit drugs and use up their limited financial resources that may subsequently impact on nutrition. The use of either alcohol and/or illicit drugs further contributes to limiting their psychosocial functioning generally and to increasing their cognitive impairments. It usually also limits their engagement with services and their compliance with medication. Furthermore, the consequences of different substances on an already malfunctioning brain, and most specifically on the fragile dopaminergic and serotonergic systems, may lower the threshold for engaging in aggressive behaviour. Understanding of the links between substance misuse and violence among persons with schizophrenia with no history of antisocial behaviour prior to illness onset is a priority for future research.
While substance use by persons with schizophrenia has attracted a great deal of attention, no studies to our knowledge have examined the links between the progressive brain changes that characterize the illness and aggressive behaviour. Furthermore, studies have not been undertaken to understand if individual reactions to these brain changes, and/or to illness onset, are linked to violence. Patients with schizophrenia who repeatedly engage in aggressive behaviour in the absence of a prior history of such behaviour represent a distinct subgroup. Further research is needed to identify the processes leading to the aggressive behaviour and treatments to end it.
11. Type III offenders with schizophrenia
These are men in their late thirties with chronic schizophrenia and no history of antisocial or aggressive behaviour who kill, or try to kill, someone, often a carer. Among men with schizophrenia, the number of convictions for violent offences decreases with the age at first conviction (Hodgins 2004). But this is not true of homicide. Homicides are often committed by patients with schizophrenia who have no history of violence or of antisocial behaviour (Beaudoin et al. 1993; Erb et al. 2001). We know of only one study that has examined this type of offender. It was based on the large amount of research showing that callousness is associated with aggressive behaviour. Using the sample of 248 men with schizophrenia described above, we found that clinical ratings of deficient affective experience (shallow affect, callousness, lack of remorse and a failure to accept responsibility for one's own actions) was associated with violent offending and with negative symptoms, but not with CD or substance misuse (Sunak 2006). Similarly, in a study of persistently aggressive inpatients, three distinct groups were identified, one of which was characterized by a lack of remorse (Nolan et al. 2003). We hypothesize that among patients with schizophrenia, deficient affective experience may be a state that fluctuates as do psychotic symptoms, and that when present it increases the vulnerability for aggressive behaviour towards others.
12. Conclusion
The available evidence indicates that schizophrenia is associated with an increased risk for non-violent and violent crime and for aggressive behaviour towards others. Offenders with schizophrenia constitute a heterogeneous population. Developing a typology of offenders with schizophrenia that is relevant to aetiology and treatment will provide a framework for investigating causal mechanisms and for studies of the effectiveness of treatment packages that address the characteristics of each type of offender.
Acknowledgments
The author would like to thank the many collaborators from around the world who contributed to the studies reported here and M. Rutter and J. Veverra who commented on earlier versions of this paper. He would also like to thank many patients and families who gave generously of their time to provide with the data.
The author acknowledges financial support from the European Union, agencies in Canada, Finland, Germany and Sweden, the trustees and R&D funds of the South London and Maudsley NHS Foundation Trust, and the Department of Health via the National Institute for Health Research (NIHR) Specialist Biomedical Research Centre for Mental Health award to South London and Maudsley NHS Foundation Trust (SLaM) and the Institute of Psychiatry at King's College, London.
One contribution of 11 to a Discussion Meeting Issue ‘The neurobiology of violence: implications for prevention and treatment’.
Endnotes
The term schizophrenia is used to refer to both schizophrenia and schizoaffective disorder.
The term violence is used to refer to physical aggression towards another person that may or may not lead to criminal prosecution. The terms violence and aggressive behaviour are used interchangeably.
The term antisocial behaviour is used to refer to a wide array of behaviours that break social norms, rules and laws, and that by definition includes substance misuse.
References
- Addington J, Penn D, Woods S.W, Addington D, Perkins D.O. Facial affect recognition in individuals at clinical high risk for psychosis. Br. J. Psychiatry. 2008;192:67–68. doi: 10.1192/bjp.bp.107.039784. doi:10.1192/bjp.bp.107.039784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alden A, Brennan P, Hodgins S, Mednick S. Psychotic disorders and sex offending in a Danish birth cohort. Arch. Gen. Psychiatry. 2007;64:1251–1258. doi: 10.1001/archpsyc.64.11.1251. doi:10.1001/archpsyc.64.11.1251 [DOI] [PubMed] [Google Scholar]
- Appelbaum P.S, Robbins P.C, Monahan J. Violence and delusions: data from the MacArthur violence risk assessment study. Am. J. Psychiatry. 2000;157:566–572. doi: 10.1176/appi.ajp.157.4.566. doi:10.1176/appi.ajp.157.4.566 [DOI] [PubMed] [Google Scholar]
- Arseneault L, Moffitt T.E, Caspi A, Taylor P.J, Silva P.A. Mental disorders and violence in a total birth cohort: results from the Dunedin study. Arch. Gen. Psychiatry. 2000;57:979–986. doi: 10.1001/archpsyc.57.10.979. doi:10.1001/archpsyc.57.10.979 [DOI] [PubMed] [Google Scholar]
- Arseneault L, Cannon M, Murray R, Poulton R, Caspi A, Moffitt T.E. Childhood origins of violent behaviour in adults with schizophreniform disorder. Br. J. Psychiatry. 2003;183:520–525. doi: 10.1192/bjp.183.6.520. doi:10.1192/bjp.183.6.520 [DOI] [PubMed] [Google Scholar]
- Beaudoin M.N, Hodgins S, Lavoie F. Homicide, schizophrenia, and substance abuse or dependency. Can. J. Psychiatry. 1993;38:541–546. doi: 10.1177/070674379303800803. [DOI] [PubMed] [Google Scholar]
- Bediou B, Asri F, Brunelin J, Krolak-Salmon P, D'amato T, Saoud M, Tazi I. Emotion recognition and genetic vulnerability to schizophrenia. Br. J. Psychiatry. 2007;191:126–130. doi: 10.1192/bjp.bp.106.028829. doi:10.1192/bjp.bp.106.028829 [DOI] [PubMed] [Google Scholar]
- Bernstein D.P, Cohen P, Skodol A, Bezirganian S, Brook J.S. Childhood antecedents of adolescent personality disorders. Am. J. Psychiatry. 1996;153:907–913. doi: 10.1176/ajp.153.7.907. [DOI] [PubMed] [Google Scholar]
- Bjørkly S. Psychotic symptoms and violence towards others—a literature review of some preliminary findings: part 1. Delusions. Aggress. Violent Behav. 2002a;7:617–631. doi:10.1016/S1359-1789(01)00049-0 [Google Scholar]
- Bjørkly S. Psychotic symptoms and violence towards others—a literature review of some preliminary findings: part 2. Hallucinations. Aggress. Violent Behav. 2002b;7:605–615. doi:10.1016/S1359-1789(01)00050-7 [Google Scholar]
- Blair R.J.R, Peschardt K.S, Budhani S, Mitchell D.G.V, Pine D.S. The development of psychopathy. J. Child Psychol. Psychiatry. 2006;47:262–275. doi: 10.1111/j.1469-7610.2006.01596.x. doi:10.1111/j.1469-7610.2006.01596.x [DOI] [PubMed] [Google Scholar]
- Bowie C.R, Reichenberg A, Patterson T.L, Heaton R.K, Harvey P.D. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am. J. Psychiatry. 2006;163:418–425. doi: 10.1176/appi.ajp.163.3.418. doi:10.1176/appi.ajp.163.3.418 [DOI] [PubMed] [Google Scholar]
- Brennan P, Mednick S.A, Hodgins S. Major mental disorders and criminal violence in a Danish birth cohort. Arch. Gen. Psychiatry. 2000;57:494–500. doi: 10.1001/archpsyc.57.5.494. doi:10.1001/archpsyc.57.5.494 [DOI] [PubMed] [Google Scholar]
- Broidy L.M, et al. Developmental trajectories of childhood disruptive behaviors and adolescent delinquency: a six-site, cross-national study. Dev. Psychol. 2003;39:222–245. doi: 10.1037//0012-1649.39.2.222. doi:10.1037/0012-1649.39.2.222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buka S.L, Tsuang M.T, Torrey E.F, Klebanoff M.A, Bernstein D, Yolken R.H. Maternal infections and subsequent psychosis among offspring. Arch. Gen. Psychiatry. 2001;58:1032–1037. doi: 10.1001/archpsyc.58.11.1032. doi:10.1001/archpsyc.58.11.1032 [DOI] [PubMed] [Google Scholar]
- Cannon M, Clarke M.C. Risk for schizophrenia— broadening the concepts, pushing back the boundaries. Schizophr. Res. 2005;79:5–13. doi: 10.1016/j.schres.2005.05.027. doi:10.1016/j.schres.2005.05.027 [DOI] [PubMed] [Google Scholar]
- Cannon M, Caspi A, Moffitt T.E, Harrington H, Taylor A, Murray R.M, Poulton R. Evidence for early-childhood, pan-developmental impairment: specific to schizophreniform disorder. Arch. Gen. Psychiatry. 2002a;59:449–456. doi: 10.1001/archpsyc.59.5.449. doi:10.1001/archpsyc.59.5.449 [DOI] [PubMed] [Google Scholar]
- Cannon M, Jones P.B, Murray R.M. Obstetric complications and schizophrenia: historical and meta-analytic review. Am. J. Psychiatry. 2002b;159:1080–1092. doi: 10.1176/appi.ajp.159.7.1080. doi:10.1176/appi.ajp.159.7.1080 [DOI] [PubMed] [Google Scholar]
- Caspi A, et al. Maternal expressed emotion predicts children's anti-social behaviour problems: using monozygotic-twin differences to identify environmental effects on behavioural development. Dev. Psychol. 2004;40:149–161. doi: 10.1037/0012-1649.40.2.149. doi:10.1037/0012-1649.40.2.149 [DOI] [PubMed] [Google Scholar]
- Clark T, Rowe R. Violence, stigma and psychiatric diagnosis: the effects of a history of violence on psychiatric diagnosis. Psychiatry Bull. 2006;30:254–256. doi:10.1192/pb.30.7.254 [Google Scholar]
- Crisp A, Gelder M, Goddard E, Meltzer H. Stigmatisation of people with mental illnesses: a follow-up study wihtin the changing minds campaign of the Royal college of Psychiatrists. World Psychiatry. 2005;4:106–113. [PMC free article] [PubMed] [Google Scholar]
- Crocker A.G, Mueser K.T, Drake R.E, Clark R.E, McHugo G.J, Ackerson T.H, Alterman A.I. Antisocial personality, psychopathy, and violence in persons with dual disorders. Crim. Justice Behav. 2005;32:452–476. doi:10.1177/0093854805276407 [Google Scholar]
- d'Acremont M, Van der Linden M. Memory for angry faces, impulsivity, and problematic behavior in adolescence. J. Abnorm. Child Psychol. 2007;35:313–324. doi: 10.1007/s10802-006-9092-1. doi:10.1007/s10802-006-9092-1 [DOI] [PubMed] [Google Scholar]
- d'Onofrio B.M, Van Hulle C.A, Waldman I.D, Rodgers J.L, Rathouz P.J, Lahey B.B. Casual inferences regarding prenatal alcohol exposure and childhood externalizing problems. Arch. Gen. Psychiatry. 2007;64:1296–1304. doi: 10.1001/archpsyc.64.11.1296. doi:10.1001/archpsyc.64.11.1296 [DOI] [PubMed] [Google Scholar]
- Dadds M.R, Perry Y, Hawes D.J, Merz S, Riddell A.C, Haines D.J, Solak E, Abeygunawardane A.I. Attention to the eyes reverses fear-recognition deficits in child psychopathy. Br. J. Psychiatry. 2006;189:280–281. doi: 10.1192/bjp.bp.105.018150. doi:10.1192/bjp.bp.105.018150 [DOI] [PubMed] [Google Scholar]
- Damasio A.R. A neural basis for sociopathy. Arch. Gen. Psychiatry. 2000;57:128–129. doi:10.1001/archpsyc.57.2.128 [Google Scholar]
- Davies, N. 2004a Scandal of society's misfits dumped in jail. The Guardian, 6 December 2004.
- Davies, N. 2004b Trapped in a cycle of self-harm and despair for want of a psychiatric bed. The Guardian, 7 December 2004.
- Davies, N. 2004c Wasted lives of the young let down by jail system. The Guardian, 8 December 2004.
- Dean K, Walsh E, Moran P, Tyler P, Creed F, Byford S, Burns T, Murray R, Fahy T. Violence in women with psychosis in the community: prospective study. Br. J. Psychiatry. 2006;188:264–270. doi: 10.1192/bjp.bp.104.008052. doi:10.1192/bjp.bp.104.008052 [DOI] [PubMed] [Google Scholar]
- Erb M, Hodgins S, Freese R, Müller-Isberner R, Jöckel D. Homicide and schizophrenia: maybe treatment does have a preventive effect. Crim. Behav. Ment. Health. 2001;11:6–26. doi: 10.1002/cbm.366. doi:10.1002/cbm.366 [DOI] [PubMed] [Google Scholar]
- Fazel S, Danesh J. Serious mental disorder in 23000 prisoners: a systematic review of 62 surveys. Lancet. 2002;259:545–550. doi: 10.1016/S0140-6736(02)07740-1. doi:10.1016/S0140-6736(02)07740-1 [DOI] [PubMed] [Google Scholar]
- Ferdinand R.F, Verhulst F.C. Psychopathology from adolescence into young adulthood: an 8-year follow- up study. Am. J. Psychiatry. 1995;152:1586–1594. doi: 10.1176/ajp.152.11.1586. [DOI] [PubMed] [Google Scholar]
- Frick P.J, Marsee M.A. Psychopathy and developmental pathways to antisocial behavior in youth. In: Patrick C.J, editor. Handbook of psychopathy. Guilford Press; New York, NY: 2006. pp. 353–374. [Google Scholar]
- Frick P.J, Lahey B.B, Loeber R, Stouthamer-Loeber M, Christ M.A.G, Hanson K. Familial risk factors to oppositional defiant disorder and conduct disorder: parental psychopathology and maternal parenting. J. Consult. Clin. Psychol. 1992;60:49–55. doi: 10.1037//0022-006x.60.1.49. doi:10.1037/0022-006X.60.1.49 [DOI] [PubMed] [Google Scholar]
- Fulwiler C, Ruthazer R. Premorbid risk factors for violence in adult mental illness. Compr. Psychiatry. 1999;40:96–100. doi: 10.1016/s0010-440x(99)90112-8. doi:10.1016/S0010-440X(99)90112-8 [DOI] [PubMed] [Google Scholar]
- Fulwiler C, Grossman H, Forbes C, Ruthazer R. Early-onset substance abuse and community violence by outpatients with chronic mental illness. Psychiatr. Serv. 1997;48:1181–1185. doi: 10.1176/ps.48.9.1181. [DOI] [PubMed] [Google Scholar]
- Garner B, et al. Pituitary volume predicts future transition to psychosis in individuals at ultra-high risk of developing psychosis. Biol. Psychiatry. 2005;58:417–423. doi: 10.1016/j.biopsych.2005.04.018. doi:10.1016/j.biopsych.2005.04.018 [DOI] [PubMed] [Google Scholar]
- Gosden N.P, Kramp P, Gabrielsen G, Andersen T.F, Sestoft D. Violence of young criminals predicts schizophrenia: a 9-year register-based followup of 15- to 19-year-old criminals. Schizophr. Bull. 2005;31:759–768. doi: 10.1093/schbul/sbi015. doi:10.1093/schbul/sbi015 [DOI] [PubMed] [Google Scholar]
- Gottesman, I. I. 1993 Origins of schizophrenia: past as prologue. In Nature, nurture and psychology (eds R. Plomin & G. E. McClean), pp. 231–244. Washington, DC: American Psychological Association.
- Green, H., McGinnity, A., Meltzer, H., Ford, T. & Goodman, R. 2004 Mental health of children and young people in Great Britain 2004. Summary report. Office for National Statistics.
- Green E.K, et al. Operation of the schizophrenia susceptibility gene, neuregulin 1, across traditional diagnostic boundaries to increase risk for bipolar disorder. Arch. Gen. Psychiatry. 2005;62:642–648. doi: 10.1001/archpsyc.62.6.642. doi:10.1001/archpsyc.62.6.642 [DOI] [PubMed] [Google Scholar]
- Green A.I, Drake R.E, Brunette M.F, Noordsy D.L. Schizophrenia and co-occurring substance use disorder. Am. J. Psychiatry. 2007;164:402–408. doi: 10.1176/ajp.2007.164.3.402. doi:10.1176/appi.ajp.164.3.402 [DOI] [PubMed] [Google Scholar]
- Hodgins S. Mental disorder, intellectual deficiency and crime: evidence from a birth cohort. Arch. Gen. Psychiatry. 1992;49:476–483. doi: 10.1001/archpsyc.1992.01820060056009. [DOI] [PubMed] [Google Scholar]
- Hodgins S. Epidemiological investigations of the associations between major mental disorders and crime: methodological limitations and validity of the conclusions. Soc. Psychiatry Psychiatr. Epidemiol. 1998;33:29–37. doi: 10.1007/s001270050207. doi:10.1007/S001270050207 [DOI] [PubMed] [Google Scholar]
- Hodgins S. Criminal and antisocial behaviours and schizophrenia: a neglected topic. In: Gattaz W.F, Häfner H, editors. Search for the causes of schizophrenia. vol. V. Steinkopff Verlag; Darmstadt, Germany: 2004. pp. 315–341. [Google Scholar]
- Hodgins S. Criminality among persons with severe mental illness. In: Soothill K, Dolan M, Rogers P, editors. Handbook of forensic mental health. Willan Publishing; Devon, UK: 2008. ch. 16. [Google Scholar]
- Hodgins S, Côté G. Major mental disorder and APD: a criminal combination. Bull. Am. Acad. Psychiatry Law. 1993;21:155–160. [PubMed] [Google Scholar]
- Hodgins S, Janson C.G. Cambridge University Press; Cambridge, UK: 2002. Criminality and violence among the mentally disordered: the Stockholm metropolitan project. [Google Scholar]
- Hodgins S, Müller-Isberner R. Preventing crime by people with schizophrenic disorders: the role of psychiatric services. Br. J. Psychiatry. 2004;185:245–250. doi: 10.1192/bjp.185.3.245. doi:10.1192/bjp.185.3.245 [DOI] [PubMed] [Google Scholar]
- Hodgins S, Mednick S.A, Brennan P, Schulsinger F, Engberg M. Mental disorder and crime: evidence from a danish birth cohort. Arch. Gen. Psychiatry. 1996a;53:489–496. doi: 10.1001/archpsyc.1996.01830060031004. [DOI] [PubMed] [Google Scholar]
- Hodgins S, Toupin J, Côté G. Schizophrenia and antisocial personality disorder: a criminal combination. In: Schlesinger L.B, editor. Explorations in criminal psychopathology. Charles C Thomas Publisher; Springfield, IL: 1996b. pp. 217–237. [Google Scholar]
- Hodgins S, Côté G, Toupin J. Major mental disorders and crime: an etiological hypothesis. In: Cooke D, Forth A, Hare R.D, editors. Psychopathy: theory, research and implications for society. Kluwer Academic Publishers; Dordrecht, The Netherlands: 1998. pp. 231–256. [Google Scholar]
- Hodgins S, Kratzer L, McNeil T.D. Obstetric complications, parenting, and risk of criminal behavior. Arch. Gen. Psychiatry. 2001;58:746–752. doi: 10.1001/archpsyc.58.8.746. doi:10.1001/archpsyc.58.8.746 [DOI] [PubMed] [Google Scholar]
- Hodgins S, Kratzer L, McNeil T.F. Obstetrical complications, parenting practices and risk of criminal behavior among persons who develop major mental disorders. Acta Psychiatr. Scand. 2002;105:179–188. doi: 10.1034/j.1600-0447.2002.1o109.x. doi:10.1034/j.1600-0447.2002.1o109.x [DOI] [PubMed] [Google Scholar]
- Hodgins S, Hiscoke U.L, Freese R. The antecedents of aggressive behavior among men with schizophrenia: a prospective investigation of patients in community treatment. Behav. Sci. Law. 2003;21:523–546. doi: 10.1002/bsl.540. doi:10.1002/bsl.540 [DOI] [PubMed] [Google Scholar]
- Hodgins S, Tiihonen J, Ross D. The consequences of conduct disorder for males who develop schizophrenia: associations with criminality, aggressive behavior, substance use, and psychiatric services. Schizophr. Res. 2005;78:323–335. doi: 10.1016/j.schres.2005.05.021. doi:10.1016/j.schres.2005.05.021 [DOI] [PubMed] [Google Scholar]
- Hodgins S, Alderton J, Cree A, Aboud A, Mak T. Aggressive behaviour, victimisation, and crime among severely mentally ill patients requiring hospitalisation. Br. J. Psychiatry. 2007;191:343–350. doi: 10.1192/bjp.bp.106.06.029587. doi:10.1192/bjp.bp.106.06.029587 [DOI] [PubMed] [Google Scholar]
- Hodgins, S., Cree, A., Alderton, J. & Mark, T. 2008 Conduct disorder to severe mental illness: associations with aggressive behaviour, crime and victimization. Psychol. Med.38, 975–987. (doi:10.1017/S0033291707002164). [DOI] [PubMed]
- Hodgins, S., Lincoln, T. & Mak, T. Submitted. Functional outcome in schizophrenia: a novel definition and predictors.
- Hodgins, S., Larsson, G. & Larm, P. In preparation. Developing schizophrenia among adolescents with substance misuse problems.
- Ismail B, Cantor-Graae E, McNeil T. Minor physical anomalies in schizophrenia: cognitive, neurological, and other clinical correlates. J. Psychiatr. Res. 2000;34:45–56. doi: 10.1016/s0022-3956(99)00034-5. doi:10.1016/S0022-3956(99)00034-5 [DOI] [PubMed] [Google Scholar]
- Jaffee S.R, Caspi A, Moffitt T.E, Taylor A. Physical maltreatment victim to antisocial child: evidence of an environmentally mediated process. J. Abnorm. Psychol. 2004;113:44–55. doi: 10.1037/0021-843X.113.1.44. doi:10.1037/0021-843X.113.1.44 [DOI] [PubMed] [Google Scholar]
- Jones P, Rodgers B, Murray R, Marmot M. Child developmental risk factors for adult schizophrenia in the British 1946 birth cohort. Lancet. 1994;344:1398–1401. doi: 10.1016/s0140-6736(94)90569-x. doi:10.1016/S0140-6736(94)90569-X [DOI] [PubMed] [Google Scholar]
- Joyal C, Hallé P, Hodgins S, Lapierre D. Letter to the editor: drug abuse and/or dependence and better neuropsychological performance in patients with schizophrenia. Schizophr. Res. 2003;63:297–299. doi: 10.1016/s0920-9964(02)00387-0. doi:10.1016/S0920-9964(02)00387-0 [DOI] [PubMed] [Google Scholar]
- Joyal C.C, et al. Violent persons with schizophrenia and comorbid disorders: a functional magnetic resonance imaging study. Schizophr. Res. 2007;91:97–102. doi: 10.1016/j.schres.2006.12.014. doi:10.1016/j.schres.2006.12.014 [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt T.E, Harrington H.L, Milne B.J, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective longitudinal cohort. Arch. Gen. Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. doi:10.1001/archpsyc.60.7.709 [DOI] [PubMed] [Google Scholar]
- Krakowski M, Czobor P. Gender differences in violent behaviours: relationship to clinical symptoms and psychosocial factors. Am. J. Psychiatry. 2004;161:459–465. doi: 10.1176/appi.ajp.161.3.459. doi:10.1176/appi.ajp.161.3.459 [DOI] [PubMed] [Google Scholar]
- Krueger R.F, Hicks B.M, Patrick C.J, Carlson S.R, Iacono W.G, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J. Abnorm. Psychol. 2002;111:411–424. doi:10.1037/0021-843X.111.3.411 [PubMed] [Google Scholar]
- Lahey B.B, Piacentini J.C, McBurnett K, Stone P, Hartidagen S, Hynd G. Psychopathology in the parents of children with conduct disorder and hyperactivity. Am. Acad. Child Adolesc. Psychiatry. 1988;27:163–170. doi: 10.1097/00004583-198803000-00005. [DOI] [PubMed] [Google Scholar]
- Lane A, et al. The anthropometric assessment of dysmorphic features in schizophrenia as an index of its developmental origins. Psychol. Med. 1997;27:1155–1164. doi: 10.1017/s0033291797005503. doi:10.1017/S0033291797005503 [DOI] [PubMed] [Google Scholar]
- Laurens K.R, Hodgins S, Maughan B, Murray R.M, Rutter M.L, Taylor E.A. Community screening for psychotic-like experiences and other putative antecedents of schizophrenia in children aged 9–12 years. Schizophr. Res. 2007a;90:130–146. doi: 10.1016/j.schres.2006.11.006. doi:10.1016/j.schres.2006.11.006 [DOI] [PubMed] [Google Scholar]
- Laurens, K. R., West, S. A., Murray, R. M. & Hodgins, S. 2007b Psychotic-like experiences and other antecedents of schizophrenia in children aged 9–12 years: a comparison of ethnic and migrant groups in the United Kingdom. Psychol. Med (doi:10.1017/S0033291707002048) [DOI] [PubMed]
- Link B.G, Pelham J.C. Stigma and its public health implications. Lancet. 2006;11:528–529. doi: 10.1016/S0140-6736(06)68184-1. doi:10.1016/S0140-6736(06)68184-1 [DOI] [PubMed] [Google Scholar]
- Link B.G, Cullen F.T, Frank J, Wozniak J.F. The social rejection of former mental patients: understanding why labels matter. Am. J. Sociol. 1987;92:1461–1500. doi:10.1086/228672 [Google Scholar]
- Loeber R, et al. The prediction of violence and homicide in young men. J. Consult. Clin. Psychol. 2005;73:1074–1088. doi: 10.1037/0022-006X.73.6.1074. doi:10.1037/0022-006X.73.6.1074 [DOI] [PubMed] [Google Scholar]
- Loney B.R, Butler M.A, Lima E.N, Counts C.A, Eckel L.A. The relation between salivary cortisol, callour-unemotional traits, and conduct problems in an adolescent non-referred sample. J. Child Psychol. Psychiatry. 2006;47:30–36. doi: 10.1111/j.1469-7610.2005.01444.x. doi:10.1111/j.1469-7610.2005.01444.x [DOI] [PubMed] [Google Scholar]
- Lorber M.F. Psychophysiology of aggression, psychopathy, and conduct problems: a meta-analysis. Psychol. Bull. 2004;130:531–552. doi: 10.1037/0033-2909.130.4.531. doi:10.1037/0033-2909.130.4.531 [DOI] [PubMed] [Google Scholar]
- MacCabe, J. H. et al 2007 Scholastic achievement at age 16 and risk of schizophrenia and other psychoses: a national cohort study. Psychol. Med (doi:10.1017/S0033291707002048) [DOI] [PubMed]
- Maughan B, Taylor A, Caspi A, Moffitt T.E. Parental smoking and early childhood conduct problems: testing genetic and environmental explanations of the association. Arch. Gen. Psychiatry. 2004;61:836–843. doi: 10.1001/archpsyc.61.8.836. doi:10.1001/archpsyc.61.8.836 [DOI] [PubMed] [Google Scholar]
- Miyamoto S, LaMantia A.S, Duncan G.E, Sullivan P, Gilmore J.H, Lieberman J.A. Recent advances in the neurobiology of schizophrenia. Mol. Interv. 2003;3:27–39. doi: 10.1124/mi.3.1.27. doi:10.1124/mi.3.1.27 [DOI] [PubMed] [Google Scholar]
- Moffitt T.E. Genetic and environmental influences on antisocial behaviors: evidence from behavioral-genetic research. Adv. Genet. 2005;55:41–104. doi: 10.1016/S0065-2660(05)55003-X. doi:10.1016/S0065-2660(05)55003-x [DOI] [PubMed] [Google Scholar]
- Moffitt, T. E. 2006 Life-course-persistent versus adolescence-limited antisocial behaviour. In Developmental psychopathology (eds D. Cicchetti & D. Cohen). Risk, disorder, and adaptation, pp. 570–598, 2nd edn. Hoboken, NJ: Wiley. Also see xvi, 944 pp.
- Moffitt T.E, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Dev. Psychopathol. 2001;13:355–375. doi: 10.1017/s0954579401002097. doi:10.1017/S0954579401002097 [DOI] [PubMed] [Google Scholar]
- Mojtabai R. Psychotic-like experiences and interpersonal violence in the general population. Soc. Psychiatry Psychiatr. Epidemiol. 2006;40:1–8. doi: 10.1007/s00127-005-0020-4. [DOI] [PubMed] [Google Scholar]
- Moran P, Hodgins S. The correlates of co-morbid antisocial personality disorder in schizophrenia. Schizophr. Bull. 2004;30:791–802. doi: 10.1093/oxfordjournals.schbul.a007132. [DOI] [PubMed] [Google Scholar]
- Morgan C, et al. Parental separation, loss and psychosis in different ethnic groups: A case-control study. Psychol. Med. 2007;37:495–503. doi: 10.1017/S0033291706009330. doi:10.1017/S0033291706009330 [DOI] [PubMed] [Google Scholar]
- Mueser K.T, McGurk S.R. Schizophrenia. Lancet. 2004;363:2063–2072. doi: 10.1016/S0140-6736(04)16458-1. doi:10.1016/S0140-6736(04)16458-1 [DOI] [PubMed] [Google Scholar]
- Mueser K.T, Rosenberg S.D, Drake R.E, Miles K.M, Wolford G, Vidaver R, Carrieri K. Conduct disorder, antisocial personality disorder and substance use disorders in schizophrenia and major affective disorders. J. Stud. Alcohol. 1999;60:278–284. doi: 10.15288/jsa.1999.60.278. [DOI] [PubMed] [Google Scholar]
- Mueser K.T, Crocker A.G, Frisman L.B, Drake R.E, Covell N.H, Essock S.M. Conduct disorder and antisocial personality disorder in persons with severe psychiatric and substance use disorders. Schizophr. Bull. 2006;32:626–636. doi: 10.1093/schbul/sbj068. doi:10.1093/schbul/sbj068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naudts K.H, Hodgins S. Schizophrenia and violence. A search for neurobiological correlates. Curr. Opin. Psychiatry. 2006;19:533–538. doi: 10.1097/01.yco.0000238484.12023.aa. doi:10.1097/01.yco.0000238484.12023.aa [DOI] [PubMed] [Google Scholar]
- Nock M.K, Kazdin A.E, Hiripi E, Kessler R.C. Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the national comorbidity survey replication. Psychol. Med. 2006;36:699–710. doi: 10.1017/S0033291706007082. doi:10.1017/S0033291706007082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolan K.A, Czobor P, Roy B.B, Platt M.M, Shope C.B, Citrome L.L, Volavka J. Characteristics of assaultive behavior among psychiatric inpatients. Psychiatr. Serv. 2003;54:1012–1016. doi: 10.1176/appi.ps.54.7.1012. doi:10.1176/appi.ps.54.7.1012 [DOI] [PubMed] [Google Scholar]
- Odgers C.L, Milne B.J, Caspi A, Crump R, Poulton R, Moffitt T.E. Predicting prognosis for the conduct-problem boy: can family history help? J. Am. Acad. Child Adolesc. Psychiatry. 2007;46:1240–1249. doi: 10.1097/chi.0b013e31813c6c8d. doi:10.1097/chi.0b013e31813c6c8d [DOI] [PubMed] [Google Scholar]
- Pantelis C, et al. Structural brain imaging evidence for multiple pathological processes at different stages of brain development in schizophrenia. Schizophr. Bull. 2005;31:672–696. doi: 10.1093/schbul/sbi034. doi:10.1093/schbul/sbi034 [DOI] [PubMed] [Google Scholar]
- Pariante C.M, et al. Increased pituitary volume in antipsychotic-free and antipsychotic-treated patients of the AESOP First-Onset Psychosis Study. Neuropsychopharmacology. 2005;30:1923–1931. doi: 10.1038/sj.npp.1300766. doi:10.1038/sj.npp.1300766 [DOI] [PubMed] [Google Scholar]
- Potvin S, Joyal C.C, Pelletier J, Stip E. Contradictory cognitive capacities among substance-abusing patients with schizophrenia: a meta-analysis. Schizophr. Res. 2008;100:242–251. doi: 10.1016/j.schres.2007.04.022. doi:10.1016/j.schres.2007.04.022 [DOI] [PubMed] [Google Scholar]
- Poulton R, Caspi A, Moffitt T.E, Cannon M, Murray R, Harrington H.L. Children's self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch. Gen. Psychiatry. 2000;57:1053–1058. doi: 10.1001/archpsyc.57.11.1053. doi:10.1001/archpsyc.57.11.1053 [DOI] [PubMed] [Google Scholar]
- Priebe S, Badesconyi A, Fioritti A, Hansson L, Kilian R, Torres-Gonzales F, Turner F, Wiersma D. Reinstitutionalisation in mental health care: comparison of data on service provision from six European countries. Br. Med. J. 2005;330:123–126. doi: 10.1136/bmj.38296.611215.AE. doi:10.1136/bmj.38296.611215.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapoport, J. C., Addington, A. M., Frangou, S. 2005 The neurodevelopmental model of schizophrenia: update 2005 Mol. Psychiatry10, 614. (Correcting 10, 439–449.) (doi:10.1038/sj.mp.4001673) [DOI] [PubMed]
- Räsänen P, Hakko H, Isohanni M, Hodgins S, Järvelin M.-R, Tiihonen J. Maternal smoking during pregnancy and risk of criminal behavior in the Northern Finland 1966 birth cohort. Am. J. Psychiatry. 1999;156:857–862. doi: 10.1176/ajp.156.6.857. [DOI] [PubMed] [Google Scholar]
- Read J, van Os J, Morrison A.P, Ross C.A. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr. Scand. 2005;112:330–350. doi: 10.1111/j.1600-0447.2005.00634.x. doi:10.1111/j.1600-0447.2005.00634.x [DOI] [PubMed] [Google Scholar]
- Rice M.E, Harris G.T. Psychopathy, schizophrenia, alcohol abuse, and violent recidivism. Int. J. Law Psychiatry. 1995;18:333–342. doi: 10.1016/0160-2527(95)00015-a. doi:10.1016/0160-2527(95)00015-A [DOI] [PubMed] [Google Scholar]
- Robins L. Williams and Williams; Baltimore, MD: 1966. Deviant children grown up. [Google Scholar]
- Robins L.N. Childhood conduct problems, adult psychopathology, and crime. In: Hodgins S, editor. Mental disorder and crime. Sage Publications Inc; Newbury Park, CA: 1993. pp. 173–207. [Google Scholar]
- Robins L.N, Tipp J, Przybeck T. Antisocial personality. In: Robins L.N, Regier D, editors. Psychiatric disorders in America: the epidemiologic catchment area study. Macmillan/Free Press; New York, NY: 1991. pp. 258–290. [Google Scholar]
- Schanda H, Földes P, Topitz A, Fliedl R, Knecht G. Premorbid adjustment of schizophrenic criminal offenders. Acta Psychiatr. Scand. 1992;86:121–126. doi: 10.1111/j.1600-0447.1992.tb03239.x. doi:10.1111/j.1600-0447.1992.tb03239.x [DOI] [PubMed] [Google Scholar]
- Schneider F, Gur R.C, Koch K, Backes V, Amunts K, Shah J, Bilker W, Gur R.E, Habel U. Impairment in the specificity of emotion processing in schizophrenia. Am. J. Psychiatry. 2006;163:442–447. doi: 10.1176/appi.ajp.163.3.442. doi:10.1176/appi.ajp.163.3.442 [DOI] [PubMed] [Google Scholar]
- Schug R.A, Raine A, Wilcox R.R. Psychophysiological and behavioural characteristics of individuals comorbid for antisocial personality disorder and schizophrenia-spectrum personality disorder. Br. J. Psychiatry. 2007;191:408–414. doi: 10.1192/bjp.bp.106.034801. doi:10.1192/bjp.bp.106.034801 [DOI] [PubMed] [Google Scholar]
- Silver E, Arseneault L, Langley J, Caspi A, Moffitt T.E. Mental disorder and violent victimization in a total birth cohort. Am. J. Public Health. 2005;95:2015–2021. doi: 10.2105/AJPH.2003.021436. doi:10.2105/AJPH.2003.021436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siminoff E, Elander J, Holmshaw J, Pickles A, Murray R, Rutter M. Predictors of antisocial personality. Continuities from childhood to adult life. Br. J. Psychiatry. 2004;184:118–127. doi: 10.1192/bjp.184.2.118. doi:10.1192/bjp.184.2.118 [DOI] [PubMed] [Google Scholar]
- Steadman H.J, Mulvey E.P, Monahan J, Robbbins P.C, Applebaum P.S, Grisso T, Roth L.H, Silver E. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch. Gen. Psychiatry. 1998;55:393–401. doi: 10.1001/archpsyc.55.5.393. doi:10.1001/archpsyc.55.5.393 [DOI] [PubMed] [Google Scholar]
- Stefanis N.C, Hanssen M, Smirnis N.K, Avramopoulos D.A, Evdokimidis I.K, Stefanis C.N, Verdoux H, Van Os J. Evidence that three dimensions of psychosis have a distribution in the general population. Psychol. Med. 2002;32:347–358. doi: 10.1017/s0033291701005141. [DOI] [PubMed] [Google Scholar]
- Steinert T. Prediction of inpatient violence. Acta Psychiatr. Scand. 2002;106:133–141. doi: 10.1034/j.1600-0447.106.s412.29.x. doi:10.1034/j.1600-0447.106.s412.29.x [DOI] [PubMed] [Google Scholar]
- Stirling J, Lewis S, Hopkins R, White C. Cannabis use prior to first onset psychosis predicts spared neurocognition at 10-year follow-up. Schizophr. Res. 2005;75:135–137. doi: 10.1016/j.schres.2004.10.006. doi:10.1016/j.schres.2004.10.006 [DOI] [PubMed] [Google Scholar]
- Sunak, S. 2006 Deficient effective experience and violence in schizophrenia. MSc thesis, Department of Forensic Mental Health Science, Institute of Psychiatry, King's College London.
- Susman E.J. Psychobiology of persistent antisocial behavior: Stress, early vulnerabilities and the attenuation hypothesis. Neurosci. Biobehav. Rev. 2006;30:376–389. doi: 10.1016/j.neubiorev.2005.08.002. doi:10.1016/j.neubiorev.2005.08.002 [DOI] [PubMed] [Google Scholar]
- Swanson J.W, Swartz M.S, Van Dorn R.A, Elbogen E.B, Wagner H.R, Rosenbeck R.A, Stroup T.S, McEvoy J.P, Lieberman J.A. A national study of violent behavior in persons with schizophrenia. Arch. Gen. Psychiatry. 2006;63:490–499. doi: 10.1001/archpsyc.63.5.490. doi:10.1001/archpsyc.63.5.490 [DOI] [PubMed] [Google Scholar]
- Takei N, Sham P.C, O'Callaghan E.O, Glover G, Murray R.M. Early risk factors in schizophrenia: place and season of birth. Eur. Psychiatry. 1995;10:165–170. doi: 10.1016/0767-399X(96)80059-9. doi:10.1016/0767-399X(96)80059-9 [DOI] [PubMed] [Google Scholar]
- Tengström A, Hodgins S, Kullgren G. Men with schizophrenia who behave violently: the usefulness of an early versus late starters typology. Schizophr. Bull. 2001;27:205–218. doi: 10.1093/oxfordjournals.schbul.a006867. [DOI] [PubMed] [Google Scholar]
- Tengström A, Hodgins S, Grann M, Långström N, Kullgren G. Schizophrenia and criminal offending: the role of psychopathy and substance misuse. Crim. Justice Behav. 2004;31:1–25. doi:10.1177/0093854804265173 [Google Scholar]
- Teplin L, McClelland G.M, Abram K.M, Weiner D.A. Crime victimization in adults with severe mental illness: comparison with the national crime victimization survey. Arch. Gen. Psychiatry. 2005;62:911–921. doi: 10.1001/archpsyc.62.8.911. doi:10.1001/archpsyc.62.8.911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tienari P, et al. The Finnish adoptive family study of schizophrenia. Implications for family research. Br. J. Psychiatry. 1994;164:20–26. [PubMed] [Google Scholar]
- Tiihonen J, Isohanni M, Rasanen P, Koiranen M, Moring J. Specific major mental disorders and criminality: a 26-year prospective study of the 1966 Northern Finland birth cohort. Am. J. Psychiatry. 1997;154:840–845. doi: 10.1176/ajp.154.6.840. [DOI] [PubMed] [Google Scholar]
- Toulopoulou T, Picchioni M, Rijsdijk F, Hua-Hall M, Ettinger U, Sham P, Murray R. Substantial genetic overlap between neurocognition and schizophrenia: genetic modeling in twin samples. Arch. Gen. Psychiatry. 2007;64:1348–1355. doi: 10.1001/archpsyc.64.12.1348. doi:10.1001/archpsyc.64.12.1348 [DOI] [PubMed] [Google Scholar]
- Van Goozen S.J.M, Fairchild G, Snoek H, Harold G.T. The evidence for a neurobiological model of childhood antisocial behaviour. Psychol. Bull. 2007;133:149–182. doi: 10.1037/0033-2909.133.1.149. doi:10.1037/0033-2909.133.1.149 [DOI] [PubMed] [Google Scholar]
- Walker E, Kestler L, Bollini A, Hochman K.M. Schizophrenia: etiology and course. Annu. Rev. Psychol. 2004;55:401–430. doi: 10.1146/annurev.psych.55.090902.141950. doi:10.1146/annurev.psych.55.090902.141950 [DOI] [PubMed] [Google Scholar]
- Wallace C, Mullen P.E, Burgess P. Criminal offending in schizophrenia over a 25-year period marked by deinstitutionalization and increasing prevalence of comorbid substance use disorders. Am. J. Psychiatry. 2004;161:716–727. doi: 10.1176/appi.ajp.161.4.716. doi:10.1176/appi.ajp.161.4.716 [DOI] [PubMed] [Google Scholar]
- Walsh E, Fahy T. Voilence in society. Br. Med. J. 2002;325:507–508. doi: 10.1136/bmj.325.7363.507. doi:10.1136/bmj.325.7363.507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh E, Gilvarry C, Samele C, Harvey K, Manley C, Tyrer P, Creed F, Murray R, Fahy T. Reducing violence in severe mental illness: randomized controlled trial of intensive case management compared with standard care. Br. Med. J. 2001;323:1093–1097. doi: 10.1136/bmj.323.7321.1093. doi:10.1136/bmj.323.7321.1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh E, Moran P, Scott C, McKenzie K, Burns T, Creed F, Tyrer P, Murray R.M, Fahy T. UK700 Group. Prevalence of violent victimisation in severe mental illness. Br. J. Psychiatry. 2003;183:233–238. doi: 10.1192/bjp.183.3.233. doi:10.1192/bjp.183.3.233 [DOI] [PubMed] [Google Scholar]
- Weiss E.M, et al. The relationship between history of violent and criminal behavior and recognition of facial expression of emotions in men with schizophrenia and schozoaffective disorder. Aggress. Behav. 2006;32:187–194. doi:10.1002/ab.20120 [Google Scholar]
- Wolf N, litz C, Shi J. Rates of sexual victimization in prison for inmates with and without mental disorders. Psychiatr. Serv. 2007;58:1087–1094. doi: 10.1176/appi.ps.58.8.1087. doi:10.1176/appi.ps.58.8.1087 [DOI] [PMC free article] [PubMed] [Google Scholar]