Abstract
OBJECTIVE—The purpose of this study was to determine how patients’ beliefs about antihyperglycemic and antihypertensive medications relate to medication underuse and health status.
RESEARCH DESIGN AND METHODS—In diabetic patients from an economically distressed region, we assessed perceived necessity and harmfulness for antihyperglycemic (n = 803) and antihypertensive (n = 573) medications, past year's medication underuse, A1C, systolic blood pressure (SBP), and diastolic blood pressure (DBP).
RESULTS—After correction for multiple analyses, multivariate models indicated that perceived need for antihyperglycemic medication was associated with being younger, being prescribed insulin, and being prescribed multiple medications. Concern about antihyperglycemic medications was associated with being younger, African American, dissatisfied with information received about medication, and of low health literacy. For antihypertensives, perceived necessity was associated with having numerous medical comorbidities and being dissatisfied with medication information; concern was associated with being younger, dissatisfied with information received about medication, and of low health literacy. Up to one-half of patients underused at least one of the types of medication; many of these patients attributed this underuse to cost. For both types of medications, concern was significantly associated with both cost-related and non–cost-related underuse, and antihypertensive concern was associated with higher SBP and DBP.
CONCLUSIONS—Even after adjustment for economic factors, patients who are younger, African American, or of low health literacy are especially concerned about medication harmfulness, which is in turn associated with medication underuse and higher blood pressure. To enhance adherence and outcomes, interventions should address patients’ underlying concerns about potential adverse treatment effects and focus on both cultural factors and health literacy.
Despite advances in pharmacotherapy and decades of intervention trials to improve diabetes self-management support, adherence to diabetes medication regimens remains suboptimal (1). However, adherence is an “overdetermined” behavior insofar as it is influenced by a diverse variety of demographic, psychosocial, and economic factors. In this study, we focus on one of the least studied of these factors, patients’ personal beliefs about their treatment, because this construct seems to be an adherence determinant in other illnesses and is potentially modifiable through educational and psychosocial interventions.
On both conceptual and empirical bases, treatment beliefs can be subdivided into adherence-increasing beliefs about treatment necessity and advantages and adherence-reducing beliefs about treatment harmfulness, risks, and barriers. Various forms of these constructs seem to explain adherence variation across several prevalent chronic illnesses, including HIV infection (2), depressive disorder (3–5), and cardiovascular disease (6). Although beliefs also appear to play a role in diabetes adherence, this conclusion is based mainly on single items from scales designed to measure other constructs and other nonstandardized measures (7,8).
The nature, intensity, and impact of medication beliefs may vary across sociodemographic subgroups. For example, lower-income patients may be more fatalistic about their likelihood of negative illness outcomes and, as a consequence, be less motivated to pursue aggressive management or “tight control” regimens (9–12). Researchers and clinicians are also increasingly concerned about variation in health care trust, perceived discrimination, and outcomes between African American and Caucasian patients (7). Potential variations in diabetes treatment perceptions may provide an important window into these disparities.
In this current study, we examined diabetic patients’ beliefs about their medication necessity and potential harmfulness in an economically distressed community. Given the importance of hypertension management for diabetes care, we also studied diabetic patients’ beliefs about their antihypertensive medications if applicable. After analyzing covariation in beliefs and sociodemographic characteristics, we modeled multivariate associations among beliefs, nonadherence (due to either cost or other reasons), and key medical outcomes.
RESEARCH DESIGN AND METHODS
This study was conducted in Flint, Michigan, an economically distressed, midsized city. Patients were identified from general medicine clinics of a large safety-net health system (17% of participants), its affiliated diabetes education center (58%), and the local network of federally qualified community health centers (25%). Most (92%) were identified from electronic and paper records using diagnostic codes and recruited via telephone. Additional participants were recruited during outpatient visits. Patients were eligible for the study if they had type 2 diabetes, used antihyperglycemic medication, had not been hospitalized in the prior 3 years for serious psychiatric illness, and received most of their diabetes care in a participating site. Between July 2005 and December 2007, 3,800 patients were identified from medical records and screened by phone, and 322 were identified as outpatients. Of this pool of 4,122 patients contacted for screening and recruitment, 2,516 could not be reached, 450 refused, and 1,116 were screened. Of those contacted, 841 were determined to be eligible and 806 (96%) participated. The study was approved by ethics committees at the University of Michigan and participating health systems.
Data collection and variable creation
Date were collected by face-to-face research interviews conducted by research staff from various racial backgrounds. Survey items assessed medication use and beliefs, communication with clinicians, health status, and sociodemographic variables. A Bayer 2000 analyzer was used to determine A1C. Blood pressure was measured from each arm with an Omron automatic blood pressure monitor and an appropriately sized cuff and averaged together with a third measure taken 2 min later from the arm with the higher reading.
Medication beliefs
Patients’ treatment beliefs were measured using a well-validated scale, the Beliefs about Medications Questionnaire (BMQ) (13), with versions for antihyperglycemic and antihypertensive medications. The BMQ consists of 11 items tapping either perceived medication necessity (5 items, e.g., “My health, at present, depends on my [diabetes/high blood pressure] medication.”) or concern (6 items, e.g., “I sometimes worry about the long-term effects of my [diabetes/high blood pressure] medicine.”) paired with 5-point Likert scales ranging from “strongly agree” to “strongly disagree.” Item means are computed for the Necessity and Concerns subscales. Internal consistency for our medication-specific adaptations was suggested by respective Cronbach αs of 0.78 and 0.68 for the antihyperglycemic version and 0.81 and 0.73 for the antihypertensive version.
Satisfaction with medication information
Patients’ perception of the adequacy of information about their prescription medication was measured using a modified version of the Satisfaction with Information about Medications Scale (14). This 16-item scale covers satisfaction with information received “from doctors and other people working in the place where I get medical care” on topics such as medication effectiveness. Based on pretesting, the 5-point Likert scale used was replaced with simplified choices (“enough” versus “not enough”). The revised measure had α of 0.89 in this dataset. Higher scores indicate greater satisfaction, and a median split was performed to facilitate interpretation.
Medication underuse
Cost-related underuse was measured using an item that has been used in several prior studies, “In the past 12 months, have you ever taken less of your [diabetes/hypertension] medication than prescribed by your doctor because of the cost?” Non–cost-related underuse was measured using the item “Many people do not take their prescription medication exactly as prescribed by their doctor. In the past year, have you ever taken less of your [diabetes/hypertension] medication prescribed for any reason other than the cost?”
Other variables
Race/ethnicity was self-reported. Functional health literacy (FHL) was measured using three previously validated items (15). As previously validated against a widely accepted standard (16,17), an FHL deficit was indicated by difficulty reading forms or learning about medical conditions. Other self-reported variables were educational attainment, income, insulin prescription, and monthly out-of-pocket medication costs categorized reduced by median split (≤$49 vs. ≥$50).
Statistical analysis
We initially considered bivariate associations between selected patient characteristics (e.g., sociodemographic variables or satisfaction) and medication beliefs, using Spearman's ρ correlation and matched-samples t tests. We then developed four multivariate ordinary least-squares regression models to evaluate the independent effect of patient characteristics on medication beliefs. Next, multinomial logistic models were fitted to examine the impact of perceived necessity and concerns (evaluated simultaneously, i.e., in the same model) on cost-related and non–cost-related medication underuse. Finally, ordinary least-squares regression models were fitted to examine the influence of perceived necessity and concerns (also evaluated simultaneously) on A1C, systolic blood pressure (SBP), and diastolic blood pressure (DBP). Because multivariate analyses involved five outcomes, we applied a Bonferroni correction by interpreting only effects that reached the P < 0.01 (Pcrit = 0.05/5) level of significance.
RESULTS
Descriptive statistics
Sample characteristics are summarized in Table 1. Slightly more than half of the sample was African American and slightly more than half was female. More than one-third had low FHL. Participants showed reasonably good glycemic control (mean = 7.8%) and blood pressure control (mean SBP/DBP = 139/83 mmHg). The majority (71%) were prescribed an antihypertensive medication. The only detected difference between participants who were prescribed antihypertensive medication and those who were not was that the former had higher SBP and DBP than the latter (both P < 0.01). Beliefs about both medications (summarized in Table 1) varied across their entire possible ranges and approximated a normal distribution.
Table 1.
Sample characteristics
| Medication prescribed |
||
|---|---|---|
| Antihyperglycemic | Antihyperglycemic plus antihypertensive | |
| n | 803 | 573 |
| Age (years) | 55.3 + 11.8 | 57.2 ± 10.7 |
| Sex (% male) | 38.4 | 31.7 |
| African American | 58.3 | 61.9 |
| Level of education (%) | ||
| <12 years | 21.6 | 22.8 |
| 12 years (high school degree) | 35.7 | 36.6 |
| >12 years | 42.7 | 40.6 |
| Household income bracket (%) | ||
| $0–$10,000 | 30.2 | 32.5 |
| $11,000–$20,000 | 23.7 | 24.4 |
| $21,000–$30,000 | 7.4 | 6.9 |
| $31,000–$60,000 | 20.2 | 19.6 |
| >$60,000 | 18.5 | 17.0 |
| No. of medical conditions | 2.7 ± 1.9 | 3.0 ± 1.9 |
| No. of prescription medications | 4.3 ± 1.2 | 4.6 ± 1.0 |
| Prescribed insulin (%) | 39.9 | 41.8 |
| A1C | 7.8 ± 2.0 | 7.7 ± 2.0 |
| SBP (mmHg) | 139.2 ± 21.2 | 142.0 ± 22.5 |
| DBP (mmHg) | 83.1 ± 12.0 | 83.7 ± 12.8 |
| Low health literacy (%) | 37.2 | 39.5 |
| Has a primary care provider (%) | 75.1 | 73.0 |
| Prior diabetes education (%) | 60.2 | 59.8 |
| Medication beliefs | ||
| Necessity | 3.8 ± 0.6 | 3.7 ± 0.6 |
| Concerns | 2.8 ± 0.7 | 2.7 ± 0.6 |
Data are mean ± SD or %.
Univariate associations with medication beliefs
Matched-samples t tests indicated that for both types of medication, perceived necessity was stronger than concern (respective mean differences were 1.0 and 1.1 units on the 5-point BMQ scale [or 1.7 and 1.8 SD units], both P < 0.0001). Participants prescribed both types of medication rated antihyperglycemic medication as more necessary (P = 0.001) and more concerning (P < 0.0001) than antihypertensive medication, although these effect sizes were relatively small (mean differences were both 0.1 BMQ unit or 0.17 SD units).
Bivariate associations between patient characteristics and medication beliefs are listed in Table 2. These were fairly consistent across the two types of medication. Perceived medication necessity tended to be stronger among participants who were younger, female (antihypertensive beliefs only), affected by more comorbid conditions, prescribed a higher number of medications, or prescribed insulin (antihyperglycemic beliefs only). Perceived harmfulness tended to be stronger among participants who were younger, African American, of low income, affected by a greater number of comorbid conditions (antihyperglycemic beliefs only), dissatisfied with medication information, or of low FHL.
Table 2.
Bivariate associations between patient characteristics and medication beliefs
| Medication beliefs |
||||
|---|---|---|---|---|
| Antihyperglycemic |
Antihyperglycemic |
|||
| Necessity | Concerns | Necessity | Concerns | |
| n | 803 | 573 | ||
| Age (years) | −0.11*** | −0.18*** | −0.09* | −0.16*** |
| Sex (male) | −0.03 | −0.07* | −0.11** | 0.02 |
| Ethnic minority | −0.04 | 0.11*** | 0.00 | 0.09* |
| Level of education | −0.02 | 0.01 | −0.07 | 0.02 |
| Household income bracket | −0.08* | −0.09* | −0.05 | −0.14*** |
| Number of prescription medications | 0.22*** | 0.05 | 0.18*** | 0.004 |
| Prescribed insulin | 0.28*** | 0.06 | 0.05 | −0.03 |
| Number of medical conditions | 0.21*** | 0.12*** | 0.18*** | 0.07 |
| Satisfaction with medication information | 0.03 | −0.16*** | 0.10* | −0.17*** |
| Low functional health literacy | 0.01 | 0.14*** | 0.03 | 0.23*** |
| Out-of-pocket prescription costs >$50/month | 0.08* | 0.05 | 0.08 | −0.03 |
Cell entries represent Spearman's ρ values.
P < 0.05;
P < 0.01;
P < 0.005.
Multivariate models of medication beliefs
Antihyperglycemic medication beliefs.
After adjustment for sociodemographic covariates (age, sex, ethnicity, and income), perceived need for antihyperglycemic medications was independently associated with having a greater number of prescriptions and being prescribed insulin (Table 3). In contrast, concern about antihyperglycemic medications was associated with dissatisfaction with medication information, low FHL, and high out-of-pocket prescription costs.
Table 3.
Multivariate associations between beliefs, adherence, and health status
| Independent variables predicting medication beliefs | Medication beliefs (as dependent variables)† |
|||
|---|---|---|---|---|
| Antihyperglycemic |
Antihypertensive |
|||
| Necessity | Concerns | Necessity | Concerns | |
| n | 803 | 573 | ||
| Age (years) | −0.12*** | −0.17*** | −0.08 | −0.17*** |
| Sex (male) | −0.02 | −0.05 | −0.10* | 0.05 |
| Ethnic minority | −0.03 | 0.12*** | 0.03 | 0.09* |
| Household income bracket | −0.08* | −0.05 | −0.04 | −0.07 |
| Number of prescription medications | 0.12** | −0.02 | 0.07 | −0.06 |
| Whether prescribed insulin | 0.23*** | 0.03 | −0.06 | −0.04 |
| No. of medical conditions | 0.09 | 0.11* | 0.14** | 0.08 |
| Satisfaction with medication information | 0.05 | −0.15*** | 0.11*** | −0.14*** |
| Low functional health literacy | −0.02 | 0.12*** | 0.01 | 0.22*** |
| Out-of-pocket prescription costs >$50/month | 0.05 | 0.09* | 0.07 | 0.04 |
| Binary dependent variables (medication underuse)‡ | Medication beliefs (as independent variables)§ |
|||
|---|---|---|---|---|
| Antihyperglycemic |
Antihypertensive |
|||
| Necessity | Concerns | Necessity | Concerns | |
| Cost-related underuse vs. no underuse | 1.4 | 2.8*** | 1.2 | 2.6*** |
| Noncost-related underuse vs. no underuse | 1.0 | 1.7*** | 1.2 | 1.9*** |
| Cost-related underuse vs. non-cost-related underuse | 1.4 | 1.7*** | 1.0 | 1.3 |
| Continuous dependent variables (health status)‖ | ||||
| A1C (%) | 0.03 | 0.08* | — | — |
| SBP (mmHg) | — | — | 0.09* | 0.16*** |
| DBP (mmHg) | — | — | 0.07 | 0.12** |
P < 0.05 (NS with Bonferroni correction).
P < 0.01.
P < 0.005.
Each column represents a separate ordinary least-squares regression model, with dependent variables listed as column headers and independent variables listed in rows. Cell entries represent standardized regression coefficients.
Cell entries are odds ratios (P value) of adjusted association between medication beliefs (independent variable, in columns) and underuse of the corresponding medication (dependent variable, in rows), with the second type of underuse as the reference group.
All models adjusted for age, sex, ethnic minority status, household income, number of prescription medications, insulin use, number of comorbid conditions, out-of-pocket prescription costs, and FHL.
Cell entries are standardized β coefficients (P value) of adjusted association between medication beliefs and the medical outcome variable.
Antihypertensive medication beliefs.
After covariate adjustments, perceived need for antihypertensive medications was associated with having a greater number of comorbid conditions and being satisfied with medication information. Concern about antihypertensive medications was associated with being dissatisfied with medication information and having a low FHL.
Multivariate models of adherence and health status
Antihyperglycemic medication underuse.
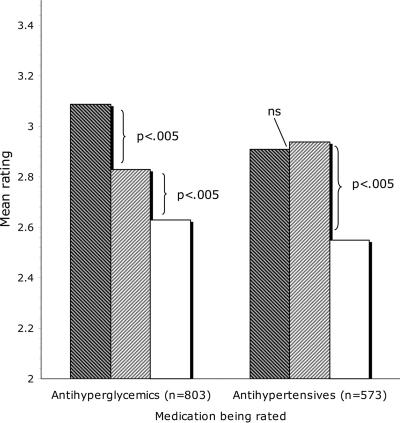
Almost half (46.6%) of participants reported antihyperglycemic underuse, about one-third of whom (16.5% of all participants) reported cost-related underuse. Adjusted logistic regression models indicated that greater concern was associated with antihyperglycemic medication underuse (Table 3). Specifically, each 1-point increase on the 5-point Concerns scale was associated with a 2.8 times increase in the risk of cost-related antihyperglycemic medication underuse and also with a 1.7 times increase in the risk of antihyperglycemic medication underuse for other reasons (each compared with no underuse). Antihyperglycemic medication concern was furthermore associated with whether a patient reported reduced adherence because of cost problems or other reasons. Specifically, each 1-point Concerns scale increase was associated with a 1.7 times increase in the risk of underuse because of cost versus other reasons. Figure 1 (left panel) depicts this set of differences.
Figure 1.
Concern ratings by medication and type of underuse.
Diabetes outcomes.
Neither antihyperglycemic medication necessity nor concern was significantly associated with A1C. However, the regression coefficient for antihyperglycemic medication concern nearly reached the Bonferroni-adjusted significance level (β = 0.08, P = 0.034) (Table 3).
Antihypertensive medication underuse.
Of participants prescribed antihypertensive medications, 31.1% reported underuse, with cost being a reason for underuse for about half (i.e., 15.3% of those prescribed antihypertensive medications). As found for antihyperglycemic medications, concern was significantly associated with each type of underuse (versus no underuse), but perceived necessity was not (Table 3). Specifically, each 1-point increase in Concerns was associated with a 2.6 times increase in risk of cost-related antihypertensive medication underuse and with a 1.9 times increase in risk of antihypertensive medication underuse for other reasons, each versus no underuse (Fig. 1, right panel). However, among those with one or the other form of antihypertensive medication underuse, concern was not associated with type of underuse.
Hypertension outcomes.
Perceived antihypertensive medication necessity was not significantly associated with either SBP or DBP. However, concern was significantly associated with both SBP and DBP (Table 3). Extrapolating from β coefficients and SDs obtained, each 1-point increase in the Concerns score was associated with a 5.7-mmHg increase in SBP and with a 2.5-mmHg increase in DBP. To examine whether this effect of concern was mediated by underuse, we added to the model a variable reflecting the presence of any underuse. Although underuse was significantly associated with SBP (β = 0.14, P = 0.002), β (concerns) did not decrease appreciably reduce (Preduction in β = 0.21). The same pattern was found when DBP was analyzed as the dependent variable and also when adjustment for each type of underuse was coded individually.
CONCLUSIONS
In this study conducted in an economically vulnerable community, diabetic patients reported significant concerns about the necessity and safety of their antihyperglycemic and antihypertensive medications. Those with the strongest concerns about medication harmfulness tended to underuse both types of medication because of both cost and other reasons. Concern was furthermore associated with blood pressure control among patients prescribed antihypertensive medications. These associations persisted after statistical adjustment for multiple sociodemographic factors, including key economic variables such as household income, total out-of-pocket prescription costs, and total number of prescriptions.
It is interesting to note that perceived necessity and harmfulness had different determinants, as has also been demonstrated outside of diabetes (5). Specifically, perceived necessity was related to medical factors such as number of comorbidities, number of medications, and insulin use. In contrast, perceived medication harmfulness was related to psychosocial factors, namely FHL and dissatisfaction with medication information received. Because only the latter belief relates to adherence and outcomes, it seems far more important to address key psychosocial factors in nonadherent patients, rather than assume that they fail to grasp the medical necessity of treatment.
The findings highlight multiple possible opportunities for clinicians and health systems. Because cost-related underuse was explained by factors other than income and costs, approaches in addition to direct financial assistance might be effective (18). Prescribing clinicians should address patients’ preferences for information about side effects and other potential consequences of pharmacotherapy, especially among patients with poor FHL. This strategy may build trust and enhance adherence and outcomes (19). Because medication underuse related to perceived medication harmfulness but not perceived necessity, we speculate that patients may view their prescribed medication as relatively more necessary than safe. If so, then it would be most productive to address patients’ worries about side effects and the personal meanings of taking medication (20).
Notably, African Americans were generally more concerned about medication harmfulness than their Caucasian counterparts. Moreover, this pattern exists regardless of income, medication costs, and FHL. Given that perceived discrimination and distrust in health care have been documented in African Americans with diabetes (21), the most culturally sensitive interventions will be those that deal directly and skillfully with medication fears.
Screening for nonadherence using archival data is increasingly feasible, as health systems transition to integrated electronic medical record and pharmacy systems. Nevertheless, educators and prescribers might consider direct screening for medication concerns, especially worry about requiring medication, likely side effects, dependence potential, and lifestyle disruption. Such information may be a useful basis for patient-centered medication decision making, ultimately improving health outcomes.
Study limitations include self-report assessment methods, which can inflate adherence estimates. However, our detected rates of nonadherence were similar to those we found in a prior study using refill data (22), our measurement approach was prevalidated, and a recent literature review concluded that standardized self-report adherence measures correspond adequately with objective measures (23). Our cross-sectional design precludes the examination of whether the detected associations persist across time, making causal inference impossible. Medication concerns might simply reflect actual adverse effects that prevent the regimen intensification required to improve outcomes. Finally, the single study site might not resemble other regions because of geographical variation in community, cultural, clinical, and economic factors. Therefore, the results should only be generalized after careful consideration of the sample characteristics and any unmeasured factors.
We conclude that diabetic patients with significant treatment-related concerns are more likely to underuse their diabetes and (if applicable) antihypertensive medication. This pattern occurs whether the underuse is cost-related or not, consistent with growing evidence that patients’ adherence in the context of cost pressures is jointly influenced by economic and diverse noneconomic factors (23). This is a key point, because clinicians in economically challenged communities may feel powerless about improving patients’ ability to afford medication. Because medication concerns may directly influence cost-related underuse, improved illness outcome may be achievable by simultaneously addressing attitudinal and economic issues.
Acknowledgments
This study was funded by the Clinical Research Program of the American Diabetes Association, the Michigan Diabetes Research and Training Center, and the Michigan Institute for Clinical and Health Research (National Institutes of Health Grant UL1RR024986). J.D.P. is a VA Senior Research Career Scientist.
No potential conflicts of interest relevant to this article were reported.
Sarah Lim, Shimia Isaac, and Mary Jane Eicher were responsible for patient recruitment and data collection. Dana Striplin provided overall project management. Basim Tofiq, MD, FRCP, FACP, and Michael Giacalone, MD, provided invaluable support for data collection.
Published ahead of print at http://care.diabetesjournals.org on 13 October 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C Section 1734 solely to indicate this fact.
References
- 1.Briesacher BA. Andrade SE. Fouayzi H. Chan KA: Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy 28:437–443, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horne R, Buick D, Fisher M, Leake H, Cooper V, Weinman J: Doubts about necessity and concerns about adverse effects: identifying the types of beliefs that are associated with non-adherence to HAART. Int J STD AIDS 15:38–44, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Clatworthy J, Bowskill R, Rank T, Parham R, Horne R: Adherence to medication in bipolar disorder: a qualitative study exploring the role of patients’ beliefs about the condition and its treatment. Bipolar Disord 9:656–664, 2007 [DOI] [PubMed] [Google Scholar]
- 4.Aikens JE, Nease DE Jr, Nau DP, Klinkman MS, Schwenk TL: Adherence to maintenance-phase antidepressant medication as a function of patient beliefs about medication. Ann Fam Med 3:23–30, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aikens JE, Nease DE Jr, Klinkman MS: Explaining patient beliefs about the necessity and harmfulness of antidepressants. Ann Fam Med 6:23–29, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petrie KJ, Weinman J, Sharpe N, Buckley J: Role of patients view of their illness in predicting return to work and functioning after myocardial infarction: longitudinal study. BMJ 312:1191–1194, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hill-Briggs F, Gary TL, Bone LR, Hill MN, Levine DM, Brancati FL: Medication adherence and diabetes control in urban African Americans with type 2 diabetes. Health Psychol 24:349–357, 2005 [DOI] [PubMed] [Google Scholar]
- 8.Chao J, Nau DP, Aikens JE, Taylor SD: The mediating role of health beliefs in the relationship between depressive symptoms and medication adherence in persons with diabetes. Res Soc Adm Pharm 1:508–525, 2005 [DOI] [PubMed] [Google Scholar]
- 9.Neame R, Hammond A: Beliefs about medications: a questionnaire survey of people with rheumatoid arthritis. Rheumatology 44:762–767, 2005 [DOI] [PubMed] [Google Scholar]
- 10.Lange LJ, Piette JD: Personal models for diabetes in the context of patients’ health status. J Behav Med 29:239–253, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez JS, Penedo FJ, Llabre MM, Duran RE, Antoni MH, Schneiderman N, Horn R: Physical symptoms, beliefs about medications, negative mood, and long-term HIV medication adherence. Ann Behav Med 34:46–55, 2007 [DOI] [PubMed] [Google Scholar]
- 12.Egede LE, Bonadonna RJ: Diabetes self-management in African Americans: an exploration of the role of fatalism. Diabetes Educ 29:105–115, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Horne R, Weinman J: Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic illness. J Psychosom Res 47:555–567, 1999 [DOI] [PubMed] [Google Scholar]
- 14.Horne R, Hankins M, Jenkins R: The Satisfaction with Information about Medications Scale (SIMS): a new measurement tool for audit and research. Qual Health Care 10:135–140, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chew LD, Bradley KA, Boyko EJ: Brief questions to identify patients with inadequate health literacy. Fam Med 36:588–594, 2004 [PubMed] [Google Scholar]
- 16.Sarkar U, Lessler D, Reilly B, Regenstein M, Piette JD, Johnson J, Brunt M, Huang J, Chew L, Gonzalez R, Schillinger D: Innovative diabetes self-management approaches for patients in safety net health care systems. Patient Educ Couns 70:102–110, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nurss JR, Parker R, Williams M, Baker D: STOFHLA Teaching Edition. Snow Camp, NC, Peppercorn Books
- 18.Piette JD, Heisler M: Horne R. Caleb Alexander G: A conceptually based approach to understanding chronically ill patients’ responses to medication cost pressures Soc Sci Med 62:846–857, 2006 [DOI] [PubMed] [Google Scholar]
- 19.Thrasher AD, Earp JAL, Golin CE, Zimmer CR: Discrimination, distrust, and racial/ethnic disparities in antiretroviral therapy adherence among a national sample of HIV-infected patients. J Acquir Immune Defic Syndr 49:84–93, 2008 [DOI] [PubMed] [Google Scholar]
- 20.Polonsky WH, Fisher L, Guzman S, Villa-Caballero L, Edelman SV: Psychological insulin resistance in patients with type 2 diabetes: the scope of the problem. Diabetes Care 28:2543–2545, 2005 [DOI] [PubMed] [Google Scholar]
- 21.Piette JD, Bibbins-Domingo K, Schillinger D: Health care discrimination, processes of care, and diabetes patients’ health status. Patient Educ Couns 60:41–48, 2006 [DOI] [PubMed] [Google Scholar]
- 22.Nau DP, Chao JD, Aikens JE: The relationship between guideline-concordant depression treatment and patient adherence to oral diabetes medications. Res Soc Adm Pharm 1:378–388, 2005 [DOI] [PubMed] [Google Scholar]
- 23.Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB: The concordance of self-report with other measures of medication adherence: a summary of the literature. Med Care 42:649–652, 2004 [DOI] [PubMed] [Google Scholar]