Abstract
Health literacy is emerging as a key element for successful medication management and empirical support for the efficacy of numeracy in the health context is rising as well. Little is known, however, about their unique effects among women and men. Given the importance of accurate medication management for effective treatment of HIV, the relation of these variables to medication management needs to be assessed. We therefore tested the relation of health literacy (reading comprehension) and numeracy to one's ability to manage a “mock” HIV regimen and whether men and women differed in these abilities. Results showed that women were less able than men to follow medication instructions and answer questions about the mock regimen. Numeracy mediated the relationship between gender and medication management. These findings highlight skills used in managing medication regimens and suggest avenues to target for identification and intervention in medication management among women and men with HIV.
Keywords: Medication management, Health literacy, Numeracy, Gender
Introduction
An important component of successful HIV treatment adherence is medication management capacity (MMC) (MacLaughlin et al. 2005), which has been defined as the “cognitive and functional ability to self-administer a medication regimen as it has been prescribed” (Maddigan et al. 2003, pp. 333). MMC includes functional skills such as correctly identifying medications and selecting the proper dose and timing (MacLaughlin et al. 2005). With the advent of highly active antiretroviral medications to treat HIV/AIDS that require extremely high levels of adherence for maximal viral suppression, the capacity to manage medications effectively over time has critical implications for the health of those living with HIV.
Low health literacy, or an inability “to obtain, process and understand basic health information…needed to make appropriate health decisions” (DHHS 2000), is emerging as an important risk for inadequate antiretroviral (ART) medication taking. In studies by Kalichman and colleagues (Kalichman et al. 2000; Kalichman and Rompa 2000), 18–25% of HIV positive participants were found to have inadequate health literacy and reported poorer adherence to ART regimens, poorer viral response to treatment and poorer immune functioning than those with adequate health literacy. Reasons for missed doses were related to confusion and depression in low health literate HIV positive individuals. These effects were found even after controlling for important potential confounders such as age, gender, ethnicity, income, HIV symptoms, substance abuse, social support, emotional distress and attitudes toward care provider (Kalichman et al. 1999).
The above studies, however, associated low health literacy to adherence to ART, not whether or not the regimens were accurately understood. Recent research has linked poor understanding of medication instructions with low health literacy among adults and older adults in primary care clinics. These studies, using primarily interview formats for assessing medication understanding accuracy, have shown that poor reading skills (as measured by the Rapid Estimate of Adult Literacy in Medicine—REALM) are associated with problems correctly identifying medications (Kripalani et al. 2006), misinterpretations of prescription drug labels (Wolf et al. 2007) and impaired ability to comprehend prescription drug warning labels (Davis et al. 2006).
A relatively recent concept for understanding health behaviors, numeracy, describes the use of quantitative skill in the health context. Because it is a new field, dissemination of research findings in support of health numeracy are only just emerging. Health numeracy is defined as “the degree to which individuals have the capacity to access, process, interpret, communicate, and act on numerical, quantitative, graphical, biostatistical, and probabilistic health information needed to make effective health decisions” (Golbeck et al. 2005, pp. 375) and has been proposed to consist of four categories: basic, computational, analytical, and statistical (Golbeck et al. 2005). Health numeracy has primarily been overshadowed by health literacy, either as a subset of health literacy or completely ignored altogether (Golbeck et al. 2005) and many early studies have focused on risk relationships rather than outcomes. However, a few studies illustrate the effects of low health numeracy on health outcomes. Estrada et al. (2004) found in an anticoagulation control study, that 82.5% of study participants missed one-third or more of items on a numeracy measure and that those with low numeracy scores had poorer anticoagulation control health outcomes. Others have shown that, among diabetic patients, those with statistical numeracy challenges (despite having adequate knowledge of their disease) may be hampered in their attempts to make adequate health decisions regarding their diabetes treatment (Montori et al. 2004). In HIV, Kalichman and colleagues (Kalichman et al. 1999) related health numeracy (understanding directions for taking medicines, monitoring blood glucose, and keeping clinic appointments) to medication adherence. However, no studies known to date have studied how numeracy skills may relate to understanding medication instructions.
Moreover, even less is known about how health literacy and health numeracy may impact health-related outcomes uniquely for men and women. Results from the 2003 National Assessment of Adult Literacy (NAAL) found that women performed slightly better than men on tasks involving reading/comprehending health-related information; however, men scored significantly higher than women on the measure of numeracy skill (National Institute for Literacy 2005). Despite the importance of accurate medication-taking in HIV and the preponderance of studies on risk factors for poor medication adherence among HIV positive patients, comparatively little is known about risks for poor MMC, particularly between men and women.
We, therefore, tested the relation of health literacy and numeracy to MMC among HIV positive men and women. We first tested for differences between men and women in MMC. Second, we assessed the relationship of health literacy and numeracy to MMC and third, we tested whether health literacy and/or numeracy mediated effects of gender on MMC in this group.
Methods
Participants
Participants for this study were recruited from HIV care clinics affiliated with the University of Miami, Jackson Memorial Hospital or Florida Department of Health pharmacies serving individuals enrolled in the AIDS Drug Assistance Program (ADAP) in Miami-Dade County, Florida. Participants were primarily referred by their HIV care providers or otherwise learned of the study from flyers posted in the clinics and pharmacies. Interested persons were either screened in person by the study recruiter in a private clinic room or were screened over the telephone by the study coordinator. Those eligible for the study were 18 years of age, currently receiving antiretroviral treatment (ART) or medically “in-process” for their first course of ART, had no history of head injury or loss of consciousness lasting more than 30 minutes and no presence of psychotic symptoms at the time of enrollment. Additionally, eligible individuals had not used heroin, cocaine or marijuana in the past 12 months. Both English and Spanish-speaking individuals were enrolled and the study was conducted in the preferred language of the individual. HIV diagnosis was verified via medical record abstraction.
Informed consent was obtained from each participant prior to initiation of study procedures. Due to the likelihood of limited literacy levels in a number of participants (our earlier research with a similar population identified average reading ability at the fifth grade level; Waldrop-Valverde and Valverde 2005), an informed consent post-test was given to ensure persons understood the procedures and risk/benefits of the study. All study procedures were completed in one session lasting no more than 2 h and participants were compensated US $50 upon completion.
Measures
Demographics
Participants answered basic demographic questions about age, education, race/ethnicity, and history of HIV infection.
Reading Comprehension for Health-Related Information
The Reading Comprehension subtest of the Test of Functional Health Literacy (TOFHLA) (Parker et al. 1995) was used to measure reading literacy. This test consists of 50 items that assess text comprehension using the modified cloze procedure. Every fifth to seventh word in a health-oriented text passage is omitted and the reader selects the appropriate word from a list of four possible choices. The passages were selected from instructions for an upper gastrointestinal series, the patient rights and responsibilities section of the Medicaid application form and a standard hospital informed consent form. Scores range from 0 to 50 and the percent correct was calculated. Although a short version of the test is available (36 items) the test developers recommend use of the full version in research studies.
Numeracy
The Applied Problems subtest of the Woodcock Johnson—III Tests of Achievement (Woodcock et al. 2001) was used to assess quantitative skills involving analyzing and solving math problems. To solve the problems, the person must listen to the problem (the test items are read aloud by the examiner), recognize the procedure to be followed, and then perform relatively simple calculations. Because many of the problems include extraneous information, the individual must decide not only the appropriate mathematical operations to use but also which numbers to include in the calculation. Applied problems are a measure of quantitative reasoning, math achievement and math knowledge. According to the test developers, low performance on this test may be a function of limited math skills, comprehension difficulties or poor mathematical reasoning abilities. This test was selected since it tapped abilities identified at “face value” to be similar to skills required for MMC, including those identified in “document literacy” that require calculation problems and inference of the correct mathematical operation when it is not provided (Ancker and Kaufman 2007).
Any test item may be repeated and the person is given a pencil and paper on which to make calculations. Although the test contains a total of 63 items, all items may not be administered. This test has a ceiling criterion to determine discontinuation of the test. The ceiling is met when the subject responds incorrectly to the last six consecutively administered items or when the final item is administered. Scores on this test are converted to demographically corrected z-scores with a mean of 0 and a standard deviation of 1.
Understanding Antiretroviral Medication Instructions
Understanding of ART medication instructions was assessed using the medication management test (MMT) (Albert et al. 1999). The test was developed in response to provider's seeming lack of awareness of the cognitive basis for patients' inability to adhere to HIV regimens and in order to identify “…mistakes in dispensing prescriptions and [assess] how well patients can calculate when a new prescription is needed, determine if pills have been missed over the prior week, and identify which medicines need to be taken with food or might make one drowsy.” (Albert et al. 1999, pp. 122). The test consists of eight items with a total of 16 points. There are five “mock” HIV medications with labels (created for the test) based on typical ART medications and dosing schedules (e.g., zidovudine, lamivudine, and saquinavir) (Over-the-counter medications such as acetaminophen and vitamins were used in place of actual antiretroviral medications). An example of a medication label is “Take one tablet two times a day— Medication B 150 mg tablet 30 tablets.” Another is “Take two tablets three times a day.” The MMT also has a medication insert for Loperamide, an anti-diarrheal, which contains indications, contraindications, dosing instructions side effects, and warnings.
The test score is then based on answers to questions about the medication labels, the loperamide insert, the ability to correctly count out and place a week's supply of pills in a medication organizer and to determine missed doses and refills. Example questions include “The next few questions are about Medication A. Assume that when you started taking Medication A, you had a seven day supply and that you've been taking the medication for three days now. In other words, you should have taken the medication as prescribed for the last three days. Now show me what you would do to determine if you've missed any pills so far” & “For medication B, how many days will a new prescription last?” & “Please answer the following questions based on this package insert information for a common diarrhea medication. If you were suddenly experiencing diarrhea and began taking this medication, what's the maximum number of capsules you should take over a two-day period?” The total percent correct was used in analyses.
Data Analysis
Characteristics of study participants were compared by gender (male = 0, female = 1) and assessed using t-tests and chi-square where appropriate. Pearson and Spearman correlations were used to test the association of participant characteristics with performance on the MMT. Only those variables significantly related to each outcome variable (P < 0.05) were included as covariates. Hierarchical multiple regression was used to test the relative contribution of gender, health literacy (TOFHLA) and quantitative literacy (Applied Problems) to scores on the MMT. Gender and covariates were entered into the first step, followed by health literacy, then third, by quantitative literacy. Mediation effects were then tested using path analytic techniques.
Results
A total of 155 participants, 90 men and 65 women, completed this study. Demographic characteristics by gender are presented in Table 1. No statistically significant differences were noted between men and women in age, education, or current employment. Men and women performed similarly on the TOFHLA reading comprehension measure (men = 78% correct; women = 73% correct; t(154) = 1.30, P > .05). However, women were more likely than men to be black (X2 = 5.72, P < .05) (versus non-black), have a regular place to stay (X2 = 7.17, P < .01), to have been diagnosed with HIV for significantly longer than men (t(142) = −2.24, P < .05), to have lower scores on the numeracy measure (Applied Problems test; t(147) = 5.50, P < 0.001), and significantly lower scores on the outcome measure of understanding medication instructions assessed by the MMT (t(153) = 2.91, P < .01). Women correctly answered an average of only 50% of questions on the Applied Problems test while men correctly answered 63%.
Table 1.
Demographic characteristics of study participants by gender
| Men (n = 90) | Women (n = 65) | Test statistic | |
|---|---|---|---|
| Race/Ethnicity | X2 = 5.724* | ||
| Black | 73 | 62 | |
| Non-black | 22 | 6 | |
| Regular place to stay (yes) | 76 | 64 | X2 = 7.171* |
| Mean (SD) years of education | 11.7 (2.6) | 11.3 (1.8) | t = 1.073 |
| Mean (SD) years since HIV diagnosis | 8.6 (7.0) | 11.1 (6.2) | t = −2.275 |
| TOFHLA % correct | 78% | 73% | t = 1.299 |
| Applied problems z-score | −.81 | −1.32 | t = 5.466* |
| MMT % correct | 65% | 58% | t = 2.912 |
Note: MMT-R = medication management test; TOFHLA = Test of functional health literacy in adults
P < .05
Results of Spearman and Pearson correlations of demographic characteristics and MMT scores showed that education and time since HIV diagnosis were significantly associated with MMT scores at an alpha <.05 and were therefore included in the regression analysis.
The hierarchical multiple regression analysis testing the association of gender, health literacy, and numeracy with the MMT scores is presented in Table 2. The first step of the model that included years of education, time since HIV diagnosis and gender explained 14% of the variance in MMT performance (R2 = 0.144, P < 0.001). Both gender and education were significantly related to the MMT in the first step. After inclusion of reading comprehension (TOFHLA) in step two, education and gender were no longer significant. In the second step, only reading comprehension scores were significantly related to MMT. The addition of reading comprehension to the model accounted for an additional 21% of the variance (R2Δ = 0.211, P < 0.001). In the third and final step, both reading comprehension and numeracy as well as time since HIV diagnosis were significantly associated with medication inference and accounted for an additional 12% of variance in the model (R2Δ = 0.125, P < 0.000). The final model with all variables explained 48% of the variance in MMT scores.
Table 2.
Hierarchical multiple regression of medication management test (MMT) scores on gender, reading comprehension and numeracy
| B | SE B | β | |
|---|---|---|---|
| Step 1 | |||
| Gender | −9.243 | 4.447 | −.169* |
| Education | 3.441 | 1.011 | .278** |
| Time since HIV diagnosis | −.033 | .028 | −.099 |
| Step 2 | |||
| Gender | −7.298 | 3.886 | −.133 |
| Education | .738 | .971 | .060 |
| Time since HIV diagnosis | −.040 | .024 | −.118 |
| Health literacy (TOFHLA) | .687 | .104 | .510** |
| Step 3 | |||
| Gender | 3.106 | 3.959 | .057 |
| Education | −.190 | .891 | −.015 |
| Time since HIV diagnosis | −.068 | .022 | −.200* |
| Health literacy (TOFHLA) | .283 | .118 | .210* |
| Numeracy (Applied Problems) | 25.11 | 4.448 | .538** |
Note: R2 = .14 for Step 1; ΔR2 = .211 for Step 2; ΔR2 = .125 for Step 3 (P < .05)
P < 0.05
P < 0.01
Since our findings showed that women scored lower on the MMT and on our measure of numeracy, we further tested whether numeracy skills mediated differences between men and women in performance on the MMT using path analytic techniques. Mediation analysis tests whether the effects of one variable on another (e.g., the effects of variable A on variable C) go through a third variable, the mediator (e.g., the effects of variable A on variable C, go through or are mediated by the effects of variable B). In perfect mediation, the relationship between variables A and C should be negated when variable B is entered into the model (Baron and Kenny 1986).
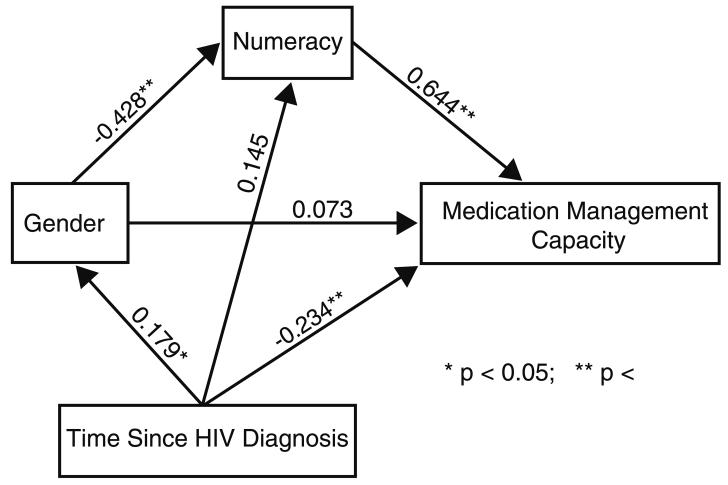
In the path analysis, we first evaluated the relation of gender to MMT performance while controlling for time since HIV diagnosis. Consistent with results of the hierarchical multiple regression analysis, gender was a significant predictor of MMT performance. When numeracy was added to the model and paths were constructed between gender and numeracy and numeracy and MMT performance, however, this situation changed. Gender was significantly related to numeracy, and numeracy in turn was a significant predictor of MMT scores. The direct relation between gender and MMT score, however, was no longer significant. It thus appears that the relation between gender and MMT performance is largely due to gender differences in numeracy. Figure 1 provides a graphical depiction of the final path model.
Fig. 1.
Path analysis of mediation effect of numeracy on MMT and gender adjusted for years since HIV diagnosis
Discussion
The purpose of this study was to test whether HIV positive men and women differed in their MMC. We also tested the independent effects of reading comprehension and numeracy on MMC and potential mediation effects.
Our findings showed that men and women had similar skill in reading comprehension and that reading comprehension skills were important for medication management. However, women had significantly lower numeracy scores than men. Numeracy was strongly related to MMC and was shown to mediate the relationship between women's lower scores on the MMT. That is to say, our findings indicate that women had more difficulty with our measure of MMC because of their poorer numeracy skills.
On average, women were able to answer correctly only a little over 50% of the mathematical reasoning test items, whereas men answered 63% correctly; therefore, neither group was highly skilled in this area. However, our results suggest that women were more adversely affected by their low numeracy skills as indicated by their MMC. Controversy has long existed as to the evidence for a male advantage in math performance. A meta-analysis (Hyde et al. 1990) showed that across studies with a wide range of ages and abilities, no gender differences in math abilities were noted. The study also pointed out that during the elementary school years girls even had a slight mathematical advantage over boys in computational skills. However, as math competencies shift in high school, boys show a slight advantage over girls, particularly in geometry and problem solving skills (Hyde et al. 1990). In an attempt to understand the basis for such gender differences, Casey et al. (1997) found that both math self-confidence and mental rotation abilities mediated the relationship between gender and Mathematics Scholastic Aptitude Test (SAT-M) scores. Others found that male high school students utilized greater strategy flexibility than females which affected performance on the SAT-M and Graduate Record Examination—GRE problem solving tests (Gallagher et al. 2000). It appears then that reasoning, problem solving and self-confidence may be essential for women when performing mathematically.
As in previous research (Davis et al. 2006; Kripalani et al. 2006; Wolf et al. 2007), the present study also found a significant relationship between health literacy for verbal information and understanding of medication instructions. The ability to accurately read, understand and draw conclusions from verbal information is critically important for effective medication management. In a summary report developed by the Agency for Healthcare Research and Quality (AHRQ) (Berkman et al. 2004), a limited number of interventions to address low health literacy were identified. All of the studies attempted to improve presentation and understanding of verbal material and were largely successful. However, as results from the present study illustrate, further research to determine the mix of abilities required to be successful in the patient role are needed so that the essential skills for particular behaviors can be identified and intervened.
Several limits of the present study must be noted. We used an antiretroviral regimen that contained five mock HIV medications. Many contemporary ART regimens consist of once and twice daily doses which may alleviate some of the burden imposed by more complex regimens as that used in this study. However, in addition to antiretroviral medications, most HIV positive patients are also prescribed prophylactic medications, vitamins, etc. Although non-adherence to these other medications does not result in the same detrimental consequences as non-adherence to ART, effective medical management of HIV infection requires overall adherence to a number of health behaviors and is the best “prescription” for HIV treatment. These findings would therefore continue to be relevant even for today's more contemporary, less complex HIV treatment regimens and whether the difficulties in MMC and numeracy displayed on average by women in this study persist with less complex regimens warrants further study.
Since this was not a randomly selected sample, the characteristics of this particular study sample may have influenced these findings. Women in this sample were over 90% African American and nearly all participants were from a low socioeconomic background. Previous studies among socioeconomically disadvantaged children have shown that low SES children are at a disadvantage overall in academic achievement which is largely driven by limited economic resources in poor communities, schools and families (Arnold and Doctoroff 2003). Non-white elementary and middle school students have been found to have significantly poorer mathematical conceptual skills (Hall et al. 1999) and studies have also shown that minority women in particular are vastly underrepresented in mathematical fields (National Science Foundation 2001). Such deficiencies in opportunity and resources may have influenced the findings in the present study and as such, the generalizability of our findings is limited.
Moreover, as discussed previously, the empirical use of numeracy in relation to health behaviors is in its early stages. Few measures exist to date to assess numeracy in general as well as its various subcomponents. To our knowledge, no other studies have used the Applied Problems subtest of the Woodcock Johnson—III Tests of Achievement in relation to health behaviors. We chose this measure rather than, for instance, the numeracy scale of the TOFHLA, because it better represented at face value, the fundamental basic and computation numeracy skills presumed needed to manage a medication regimen. The TOFHLA numeracy measure more accurately represents a measure of our outcome (i.e., understanding medication instructions) rather than the underlying numeracy skills needed to manage medications. The utility of this measure for explaining or predicting relevant health behaviors including medication management must be further examined and replicated.
Despite the above caveats, the present findings have implications for both future research and clinical practice. We hope that this study increases awareness of the skills needed to successfully manage medication regimens so that efforts to identify persons with these skill deficits can be implemented. Although remediation of poor reading comprehension and numeracy skills is likely beyond the scope of most clinical care providers, identification of specific skill deficits that can impede successful medication management can help care providers gauge the level of training and assistance a given patient may need when starting or changing a regimen. The tests used herein, however, are time consuming. Future research should be directed at developing brief screening tools to identify patients at risk for poor health literacy and numeracy.
Since several studies have already indicated that low health literacy is associated with poor adherence (Kalichman et al. 2000; Kalichman and Rompa 2000), it would be important to test whether improvements in MMC then lead to improvements in adherence. Training in medication management, particularly at the outset of ART, could potentially circumvent some instances of early non-adherence that are related to poor understanding of medication regimen instructions. Such training could incorporate strategies and tools/devices to limit reliance on reading and numeracy skills.
Acknowledgements
The authors would like to thank Michael Stirratt for his thoughtful review and helpful suggestions in the preparation of this manuscript. We would also like to thank Jesline Jean-Simon for her invaluable recruitment skills. This study was supported by funding from the National Institute of Mental Health grant number MH74664 to the lead author, D. Waldrop-Valverde.
Contributor Information
Drenna Waldrop-Valverde, Department of Psychiatry & Behavioral Sciences, Miller School of Medicine, University of Miami, P.O. Box 016960 (M817), Miami, FL 33101, USA.
Deborah L. Jones, Department of Psychiatry & Behavioral Sciences, Miller School of Medicine, University of Miami, P.O. Box 016960 (M817), Miami, FL 33101, USA
Dushyantha Jayaweera, Department of Medicine, Miller School of Medicine, University of Miami, Miami, FL, USA.
Peggy Gonzalez, Department of Psychiatry & Behavioral Sciences, Miller School of Medicine, University of Miami, P.O. Box 016960 (M817), Miami, FL 33101, USA.
Javier Romero, Miami-Dade County Health Department, Office of HIV/AIDS, Miami, FL, USA.
Raymond L. Ownby, Department of Psychiatry & Behavioral Sciences, Miller School of Medicine, University of Miami, P.O. Box 016960 (M817), Miami, FL 33101, USA
References
- Albert SM, Weber CM, Todak G, Polanco C, Clouse R, McElhiney M, et al. An observed performance test of medication management ability in HIV: Relation to neuropsychological status and medication adherence outcomes. AIDS and Behavior. 1999;3:121–128. [Google Scholar]
- Ancker JS, Kaufman D. Rethinking health numeracy: A multidisciplinary literature review. Journal of the American Medical Informatics Association. 2007;14:713–721. doi: 10.1197/jamia.M2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold DH, Doctoroff GL. The early education of socioeconomically disadvantaged children. Annual Review of Psychology. 2003;54:517–545. doi: 10.1146/annurev.psych.54.111301.145442. doi:10.1146/annurev.psych.54.111301.145442. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. doi:10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Berkman ND, DeWalt DA, Pignone MP, Sheridan SL, Lohr KN, Lux L, et al. Literacy and health outcomes. Evidence report/technology assessment no. 87 (Prepared by RTI International—University of North Carolina evidence-based practice center under contract no. 290-02-0016) Agency for Healthcare Research and Quality; Rockville, MD: 2004. (AHRQ Publication No. 04-E007-2). [Google Scholar]
- Casey MB, Nuttall RL, Pezaris E. Mediators of gender differences in mathematics college entrance test scores: A comparison of spatial skills with internalized beliefs and anxieties. Developmental Psychology. 1997;33:669–680. doi: 10.1037//0012-1649.33.4.669. doi:10.1037/0012-1649.33.4.669. [DOI] [PubMed] [Google Scholar]
- Davis TC, Wolf MS, Bass PF, Middlebrooks M, Kennen E, Baker DW, et al. Low literacy impairs comprehension of prescription drug warning labels. Journal of General Internal Medicine. 2006;21:847–851. doi: 10.1111/j.1525-1497.2006.00529.x. doi:10.1111/j.1525-1497.2006.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DHHS Healthy people 2010. 2000 Available online http://www.healthypeople.gov.
- Estrada CA, Martin-Hryniewicz M, Peek BT, Collins C, Byrd JC. Literacy and numeracy skills and anticoagulation control. American Journal of Medical Science. 2004;328:705–710. doi: 10.1097/00000441-200408000-00004. [DOI] [PubMed] [Google Scholar]
- Gallagher AM, De Lisi R, Holst PC, McGillicuddy-De Lisi AV, Morely M, Calahan C. Gender differences in advanced mathematical problem solving. Journal of Experimental Child Psychology. 2000;75:165–190. doi: 10.1006/jecp.1999.2532. doi:10.1006/jecp. 1999.2532. [DOI] [PubMed] [Google Scholar]
- Golbeck AL, Ahlers-Schmidt CR, Paschal AM, Dismuke SE. A definition and operational framework for health numeracy. American Journal of Preventive Medicine. 2005;29:375–376. doi: 10.1016/j.amepre.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Hall CW, Davis NB, Bolen LM, Chia R. Gender and racial differences in mathematical performance. The Journal of Social Psychology. 1999;139:677–689. doi: 10.1080/00224549909598248. [DOI] [PubMed] [Google Scholar]
- Hyde JS, Fennema E, Lamon SJ. Gender differences in mathematics performance: A meta-analysis. Psychological Bulletin. 1990;107:139–155. doi: 10.1037/0033-2909.107.2.139. doi:10.1037/0033-2909.107.2.139. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Benotsch E, Suarez T, Catz S, Miller J, Rompa D. Health literacy and health-related knowledge among persons living with HIV/AIDS. American Journal of Preventive Medicine. 2000;18:325–331. doi: 10.1016/s0749-3797(00)00121-5. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Ramachandran B, Catz S. Adherence to combination antiretroviral therapies in HIV patients of low health literacy. Journal of General Internal Medicine. 1999;14:267–273. doi: 10.1046/j.1525-1497.1999.00334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D. Functional health literacy is associated with health status and health-related knowledge in people living with HIV/AIDS. Journal of Acquired Immune Deficiency Syndromes. 2000;25:337–344. doi: 10.1097/00042560-200012010-00007. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Henderson LE, Chiu EY, Robertson R, Kolm P, Jacobson TA. Predictors of medication self-management skill in a low literacy population. Journal of General Internal Medicine. 2006;21:852–856. doi: 10.1111/j.1525-1497.2006.00536.x. doi:10.1111/j.1525-1497.2006.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddigan SL, Farris KB, Keating N, Wiens CA, Johnson JA. Predictors of older adults' capacity for medication management in a self-medication program. Journal of Aging and Health. 2003;15:332–335. doi: 10.1177/0898264303251893. doi:10.1177/0898264303251893. [DOI] [PubMed] [Google Scholar]
- MacLaughlin EJ, Raehl CL, Treadway AK, Sterling TL, Zoller DP, Bond CA. Assessing medication adherence in the elderly which tools to use in clinical practice? Drugs & Aging. 2005;22:231–255. doi: 10.2165/00002512-200522030-00005. doi:10.2165/00002512-200522030-00005. [DOI] [PubMed] [Google Scholar]
- Montori V, Leung T, Thompson C, Chung J, Capes S, Smith S. Choice of risk representation to enable diabetes decision-making. Diabetes. 2004;53(S2):A225. [Google Scholar]
- National Institute for Literacy 2003 National Assessment of Adult Literacy: A first look at the literacy of America's adults in the 21st century. National Center for Educational Statistics. 2005 http://nces.ed.gov/naal/health_results.asp#GenderHealthLiteracy, http://nces.ed.gov/surveys/all/ib_performance.asp.
- National Science Foundation . Science and engineering degrees by race/ethnicity of recipients 1990–1998. National Science Foundation; Arlington, VA, USA: 2001. [Google Scholar]
- Parker RM, Baker D, Williams MV. The test of functional health literacy: A new instrument for measuring patients' literacy skills. Journal of General Internal Medicine. 1995;10:537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- Waldrop-Valverde D, Valverde E. Homelessness and psychological distress as contributors to antiretroviral non-adherence in HIV positive injecting drug users. AIDS Patient Care and STDs. 2005;19:326–334. doi: 10.1089/apc.2005.19.326. doi:10.1089/apc.2005.19.326. [DOI] [PubMed] [Google Scholar]
- Wolf MS, Davis TC, Shrank W, Rapp DN, Bass PF, Connor UM, et al. To err is human: Patient misinterpretations of prescription drug label instructions. Patient Education and Counseling. 2007;67:293–300. doi: 10.1016/j.pec.2007.03.024. doi:10.1016/j.pec.2007.03.024. [DOI] [PubMed] [Google Scholar]
- Woodcock RW, McGrew KS, Mather N. Woodcock Johnson III Tests of Achievement. Riverside Publishing; Itasca, IL: 2001. [Google Scholar]