Abstract
An air embolism in the arterial system is a rare but serious sequela of lung biopsy. We describe the case of a patient who presented with acute cardiac and cerebral air embolism, including simultaneous acute ST-segment elevation myocardial infarction, atrial fibrillation, unresponsiveness, seizure, and stroke. Computed tomographic imaging revealed air pockets in the right coronary artery and aorta. The patient made a full recovery after aggressive medical treatment and hyperbaric oxygen therapy.
Key words: Biopsy, needle/adverse effects; embolism, air/complications/etiology/radiography/therapy; hyperbaric oxygenation; postoperative complications; radiography, interventional; tomography, X-ray computed
An air embolism in the arterial system is a rare but serious sequela of lung biopsy. We describe the case of a patient who presented with acute cardiac and cerebral air embolism, simultaneous acute ST-segment elevation myocardial infarction, atrial fibrillation, unresponsiveness, seizure, and stroke. Multislice computed tomographic (CT) imaging revealed air pockets in the right coronary artery and aorta. The patient made a full recovery after aggressive medical treatment and hyperbaric oxygen therapy.
Percutaneous lung biopsy guided by CT is a common clinical procedure that enables tissue diagnosis of pulmonary diseases of various causes. The most frequent sequela is pneumothorax.1 Rarely, fatal or nonfatal systemic air embolism occurs, which can cause rapid deterioration of patients' cardiac and neurologic conditions and which requires prompt and sometimes specialized treatment.
Case Report
In November 2007, a 67-year-old man presented at our hospital due to recurrent fever and joint infection, after left-hip replacement surgery. Chest radiography revealed multiple pulmonary infiltrates suggestive of bronchiolitis fibrosa obliterans with organizing pneumonia.
The patient was referred for core needle biopsy of the right lung under the guidance of multislice CT. The needle trajectory was planned on the basis of the CT images. A coaxial 17/18-gauge needle system was used to enter the lung, and 2 core biopsy samples were obtained. The patient did not cough during the procedure. However, he developed seizures and became unresponsive immediately after the biopsy. Electrocardiography showed acute atrial fibrillation, substantial ST-segment elevation in leads II, III, aVF, and V2 through V4, and ST-segment depression in leads I and aVL (Fig. 1)—consistent with acute myocardial injury involving the distributions of more than 1 coronary artery.
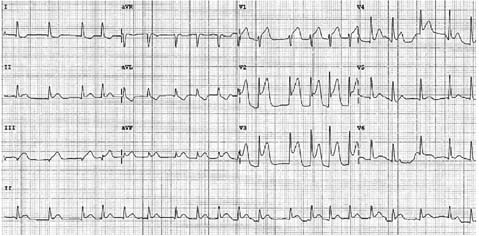
Fig. 1 Electrocardiogram shows atrial fibrillation and diffuse ST-segment elevation in the inferior and anterior leads.
The patient maintained a systolic blood pressure of 140 to 160 mmHg. Review of the multislice CT images showed air bubbles in the entire right coronary artery (Fig. 2) and the ascending aorta, diagnostic of an air embolism of the arterial system.
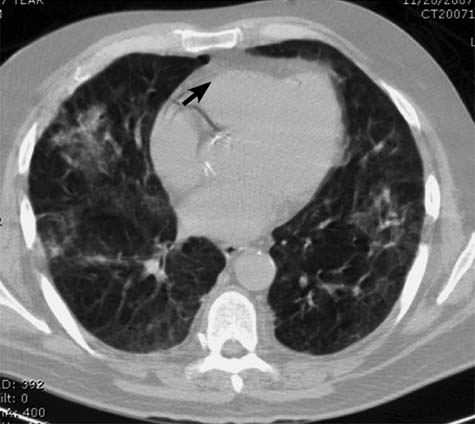
Fig. 2 Multislice computed tomography shows that the right coronary artery is entirely filled with air (arrow).
Rapid images of the head were of limited use because of the patient's motion artifact but showed no obvious air bubbles in the brain. He was placed in a mild Trendelenberg position and was administered 100%, high-flow, non-rebreathing oxygen. He was given nitropaste and intravenous diltiazem to achieve some vasodilation and heart-rate control. Intravenous normal saline solution with glucose was also given to avoid hypotension and hypoglycemia. The patient regained consciousness after about 15 minutes. The seizures stopped spontaneously. He had persistent left-arm and left-hand weakness. Electrocardiography pertformed 47 minutes later showed persistent atrial fibrillation but complete resolution of the ST-segment elevation. Anticoagulation therapy was not initiated, due to the acute neurologic symptoms. Within 2 hours, the patient was transferred to a nearby medical center for hyperbaric oxygen therapy, which he received over 2 days in accordance with U.S. Navy Protocol 6. He was mechanically ventilated for airway protection. A subsequent blood test showed cardiac troponin I elevation to 4.8 ng/dL, consistent with acute myocardial infarction. The patient eventually experienced complete cardiac and neurologic recovery. The biopsy findings confirmed the clinical diagnosis of bronchiolitis fibrosa obliterans with organizing pneumonia. The patient underwent surgery to remove the original hip-joint replacement without any problem, and eventually underwent successful new hip-replacement surgery.
Discussion
Computed-tomographic–guided needle biopsy of the lungs is a commonly performed procedure that aids in the diagnosis of pulmonary lesions. It is generally well tolerated by patients. Tomiyama and associates1 reviewed the results of 9,783 biopsies in Japan and reported pneumothorax as the most common complication (35%). Severe complications occurred rarely—in 0.75% of patients, including 0.061% who experienced air embolisms; 0.1%, hemothorax; and 0.07%, death related to the sequelae of major events. Among the patients with air embolisms, no further details were available in this series. Mokhlesi and co-authors,2 in 2002, reported a case of coronary artery embolism in a patient who experienced cardiac arrest during lung biopsy; air was revealed in the left anterior descending artery by CT imaging. Those investigators proposed 3 possible mechanisms of the air embolism: the needle in the pulmonary vein, bronchovenous fistula, and air in the pulmonary arterial circulation reaching the pulmonary veins by traversing the microvasculature.2 Recently, Hiraki and colleagues3 reported 4 cases of air embolisms in 1,010 CT-guided lung biopsies from a single-institutional experience. All patients had paroxysms of coughing during or immediately after the procedure. One patient had a neurologic deficit, and another 3 patients did not have cardiac or cerebral symptoms in spite of the presence of air in the systemic circulation. The authors recommended immediate therapy with 100% oxygen and hyperbaric oxygen treatment, if available.
Our patient had very unusual simultaneous presentation of seizure and unresponsiveness, atrial fibrillation, acute ST-segment elevation myocardial infarction, and documentation of air in the coronary circulation and aorta. The above findings were consistent with cardiac and cerebral air embolism. Our review of the multislice CT imaging of the right coronary artery quickly confirmed the underlying cause of the patient's acute clinical deterioration and facilitated prompt intervention. The cardiac problems mimicked coronary spasm and seemed to be self limiting.4 The neurologic deficit lasted a few days, which indicated the more protracted nature of terminal cerebral vessel air embolism and the importance of ongoing care—especially the need for repeated hyperbaric oxygen therapy in an effort to maximally reduce the gas-bubble size, to replace nitrogen with oxygen, and to restore circulation and tissue oxygenation. Our patient had a favorable response to repeated hyperbaric oxygen treatment up to 2 days after his initial presentation; this confirms similar observations by other investigators.5
Interventional radiology services should consider having a clinical protocol of CT-guided lung biopsy in place to handle the very rare but life-threatening complications of arterial air embolism in order to achieve the best possible outcome.
Acknowledgement
The authors thank Dr. Nathan Ritter for his review of the cardiac computed-tomographic images.
Footnotes
Address for reprints: David H. Hsi, MD, FACC, 1561 Long Pond Road, Suite 401, Rochester, NY 14626. E-mail: dhsi@unityhealth.org
References
- 1.Tomiyama N, Yasuhara Y, Nakajima Y, Adachi S, Arai Y, Kusumoto M, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol 2006;59(1):60–4. [DOI] [PubMed]
- 2.Mokhlesi B, Ansaarie I, Bader M, Tareen M, Boatman J. Coronary artery air embolism complicating a CT-guided transthoracic needle biopsy of the lung. Chest 2002;121(3):993–6. [DOI] [PubMed]
- 3.Hiraki T, Fujiwara H, Sakurai J, Iguchi T, Gobara H, Tajiri N, et al. Nonfatal systemic air embolism complicating percutaneous CT-guided transthoracic needle biopsy: four cases from a single institution. Chest 2007;132(2):684–90. [DOI] [PubMed]
- 4.Heupler FA Jr, Ferrario CM, Averill DB, Bott-Silverman C. Initial coronary air embolus in the differential diagnosis of coronary artery spasm. Am J Cardiol 1985;55(6):657–61. [DOI] [PubMed]
- 5.Lattin G Jr, O'Brien W Sr, McCrary B, Kearney P, Gover D. Massive systemic air embolism treated with hyperbaric oxygen therapy following CT-guided transthoracic needle biopsy of a pulmonary nodule. J Vasc Interv Radiol 2006;17(8):1355–8. [DOI] [PubMed]


