Abstract
A large thrombus entrapped in an atrial septal defect is a rare condition that can lead to life-threatening systemic and pulmonary embolization. The use of thrombolysis may prove dangerous to the patient. Herein, we describe the emergency surgical management that contributed to a successful outcome in a 67-year-old man who was found to have a 23-cm-long thrombus across an atrial septal defect.
Key words: Heart atria; heart septal defects, atrial/complications/surgery; heparin/therapeutic use; pulmonary embolism/etiology/physiopathology/prevention & control; thrombosis/complications/prevention & control/surgery; vena cava filters
Entrapment of a thrombus in an atrial septal defect (ASD) is a very rare condition, and only a few cases have been reported.1–3 The use of thrombolysis to treat a large thrombus that straddles the atrial septum may endanger the patient's life, due to the risk of massive pulmonary and systemic embolization. Herein, we describe our use of emergency surgery and anticoagulation therapy in a 67-year-old man to prevent possible thromboembolism and to remove thrombi that had already embolized into the pulmonary arteries.
Clinical Summary
A 67-year-old retired miner, whose medical history included chronic obstructive pulmonary disease, multiple pulmonary bullae related to smoking and silicosis, and long-standing pulmonary hypertension, developed focal seizures. A computed tomographic scan revealed a large frontal meningioma (4.9 × 6 cm), which was resected. Postoperatively, the patient developed paraplegia. He was given subcutaneous heparin and antithrombotic stockings to avert deep vein thrombosis.
On postoperative day 7, he developed hypoxia, chest pain, hypotension, focal seizures, and unconsciousness. His condition became stable after brief cardiopulmonary resuscitation. An electrocardiogram showed anterior-wall ST-segment elevation. Bedside transthoracic echocardiography showed a large right atrial mass (6 × 2 cm) that prolapsed across the tricuspid valve, together with global hypokinesia and distention of the right ventricle. A subsequent computed tomographic scan revealed a large thrombus in the right atrium that extended across an ASD into the mitral valve (Fig. 1A), along with multiple thrombi in the pulmonary arteries (Figs. 1A and 1B).
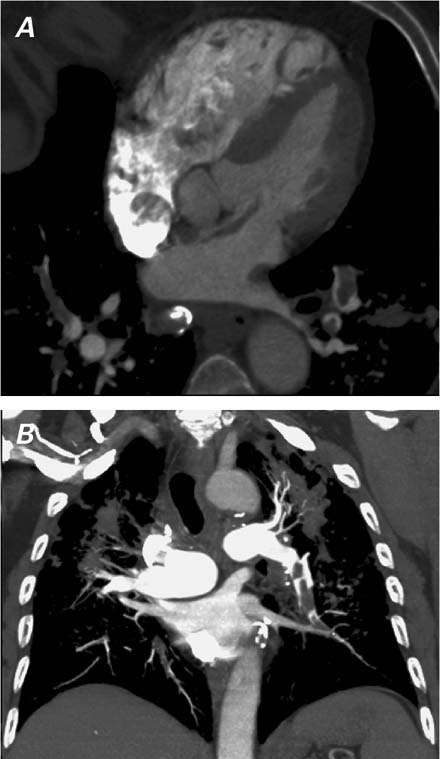
Fig. 1 Computed tomography shows A) a large thrombus that straddles the atrial septum via an atrial septal defect, and B) pulmonary emboli in both pulmonary arteries.
The patient was transferred to the operating room. A median sternotomy was performed, and cardiopulmonary bypass (CPB) with bicaval cannulation was instituted. After cardioplegic heart arrest, the right atrium was opened, and the thrombus was removed by means of gentle traction. The thrombus, which was 23 cm long, had a clear indentation at 9 cm where it had been trapped across the ASD (Fig. 2). The removal of the thrombus exposed a secundum ASD (diameter, 1 cm). We enlarged the ASD in order to inspect the mitral valve. No additional intracardiac thrombi were found. The ASD was closed by means of direct suturing, and the aortic cross-clamp was removed. The total aortic cross-clamp time was 31 minutes. The main pulmonary artery was opened, and 3 thrombi were removed from the pulmonary arteries (Fig. 2). Both pleural cavities were opened, and the patient's lungs were massaged in order to dislodge distal thrombi for subsequent removal. The pulmonary arteries were then irrigated and suctioned to remove additional small thrombi. The inferior vena cava (IVC) cannula was temporarily removed, and the IVC was checked for thrombi by means of pump suction and digital palpation. The right atrium was closed, and CPB (total time, 83 min) was discontinued. A Celect® retrievable IVC filter (Cook Medical, Inc.; Bloomington, Ind) was placed immediately after surgery. The patient was anticoagulated, first with heparin and later with warfarin.

Fig. 2 Postoperative photograph shows the 23-cm-long thrombus that was entrapped in the atrial septal defect, and 3 additional smaller thrombi that were removed from the pulmonary arteries.
Postoperatively, the patient required prolonged ventilatory support. Positive pressure ventilation and high pulmonary artery pressure further impeded pulmonary blood flow, and right ventricular failure ensued. The patient developed hepato-renal failure and required hemodialysis. He remained in the intensive care unit for 9 weeks and was then discharged, on warfarin treatment, to a rehabilitation facility. Although paraplegic, he proved able to live a reasonably active life and was doing well at 6 months' follow-up.
Comment
Impending paradoxical thromboembolism threatens the lives of patients who have a large thrombus that is entrapped in an ASD or in a patent foramen ovale. The use of thrombolysis in such patients may be dangerous—if the thrombus breaks spontaneously or as a result of thrombolysis or manipulation, massive pulmonary and systemic thromboembolism can occur. Massive pulmonary embolization is associated with a high mortality rate even in the modern era.4
Prompt diagnosis and surgical management resulted in a successful outcome in our patient. Due to paraplegia, he remained at risk of deep venous thrombosis, so the IVC filter was inserted. We believe that when risk factors for deep vein thrombosis cannot be eliminated, appropriate anticoagulation with warfarin is important after the placement of an IVC filter. Premature discontinuation of the anticoagulation in such a patient may result in IVC-filter clotting and dislodgment.5
Footnotes
Address for reprints: Igor E. Konstantinov, MD, PhD, Department of Cardiothoracic Surgery, Sir Charles Gairdner Hospital, Hospital Avenue, Nedlands, Perth, WA 6009, Australia. E-mail: konstantinov.igor@alumni.mayo.edu
References
- 1.Theologou T, Tewari P, Pointon K, Mitchell IM. Pulmonary thromboembolism with floating thrombus trapped in patent foramen ovale. Ann Thorac Surg 2007;84(6):2104–6. [DOI] [PubMed]
- 2.Rinaldi CA, Stewart AJ, Blauth CI. Intracardiac thrombus traversing a patent foramen ovale: impending paradoxical embolism demonstrated by transoesophageal echocardiography. Int J Clin Pract 2002;56(3):230–1. [PubMed]
- 3.Nellessen U, Daniel WG, Matheis G, Oelert H, Depping K, Lichtlen PR. Impending paradoxical embolism from atrial thrombus: correct diagnosis by transesophageal echocardiography and prevention by surgery. J Am Coll Cardiol 1985;5 (4):1002–4. [DOI] [PubMed]
- 4.Konstantinov IE, Saxena P, Koniuszko MD, Alvarez J, Newman MA. Acute massive pulmonary embolism with cardiopulmonary resuscitation: management and results. Tex Heart Inst J 2007;34(1):41–6. [PMC free article] [PubMed]
- 5.Konstantinov IE, Saxena P, Stewart N, Newman MA. Acute massive pulmonary embolism after migration of an inferior vena cava filter to the right ventricle. Tex Heart Inst J 2006;33 (4):532–3. [PMC free article] [PubMed]


