Abstract
BACKGROUND
The ability to copy and paste text within computerized physician documentation facilitates electronic note writing, but may affect the quality of physician notes and patient care. Little is known about physicians’ collective experience with the copy and paste function (CPF).
OBJECTIVES
To determine physicians’ CPF use, perceptions of its impact on notes and patient care, and opinions regarding its future use.
DESIGN
Cross-sectional survey.
PARTICIPANTS
Resident and faculty physicians within two affiliated academic medical centers currently using a computerized documentation system.
MEASUREMENTS
Responses on a self-administered survey.
RESULTS
A total of 315 (70%) of 451 eligible physicians responded to the survey. Of the 253 (80%) physicians who wrote inpatient notes electronically, 226 (90%) used CPF, and 177 (70%) used it almost always or most of the time when writing daily progress notes. While noting that inconsistencies (71%) and outdated information (71%) were more common in notes containing copy and pasted text, few physicians felt that CPF had a negative impact on patient documentation (19%) or led to mistakes in patient care (24%). The majority of physicians (80%) wanted to continue to use CPF.
CONCLUSIONS
Although recognizing deficits in notes written using CPF, the majority of physicians used CPF to write notes and did not perceive an overall negative impact on physician documentation or patient care. Further studies of the effects of electronic note writing on the quality and safety of patient care are required.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-008-0843-2) contains supplementary material, which is available to authorized users.
KEY WORDS: medical records system, computerized; documentation/mt [methods]; attitude of health personnel; medical staff, hospital; user-computer interface
BACKGROUND
The Institute of Medicine has identified health information technology (IT) as having enormous potential to improve the quality and safety of US health care1,2. Electronic medical records (EMR), in particular, may enhance care by increasing the accessibility of patient information. With this in mind, the National Health Information Coordinator has set a goal that every American should have an electronic medical record within the next 10 years.
Computerized physician documentation, the direct entry of physician notes into electronic health records via computer keyboard and mouse, offers several additional advantages: improved legibility, real time accessibility and decreased costs3. Although potentially cumbersome and time-consuming for physicians, electronic note writing also enables the use of time-saving, computer editing functions, including the copy and paste function (CPF). CPF allows physicians to copy a patient note from a previous time, insert it under a new date and time and alter it, rather than writing an entirely new note each day3. Although physicians have always been able to hand-copy previous patient notes, CPF facilitates this process. Examination of VA electronic medical records from 1990–2002 found evidence of copying in 9–20% of patient notes and 3% of recorded physical exams4–6.
Similar to findings with other health IT applications7–11, however, computerized physician documentation can lead to new types of problems (i.e., unintended consequences), which might mitigate the benefits associated with its use. The VA medical center studies reported that copy and pasted notes could be misleading and present a risk in terms of patient harm, fraud or malpractice claim exposure4–6. In particular, VA investigators found that the copying of the physical exam, especially if copied from a different author or from a prior time period, was “high risk”: more likely to be misleading and have a higher potential for patient harm4,5. Other recent articles also suggest that CPF may have altered the content of patient notes and their use3,12,13. It is unclear, however, whether physicians who use computerized documentation systems share these perceptions of CPF’s impact.
We undertook this study to determine the frequency and pattern of CPF use by resident and faculty physicians in two affiliated academic hospitals, their perceptions of the CPF’s impact on patient notes and patient care and their opinions about the use of CPF in the future.
METHODS
Physicians within three departments (two pediatric, one medicine) of two large, affiliated, academic hospitals were given a self-administered survey over an 8-week study period between June and August 2007.
Survey Sites and Documentation System The three departments of the two academic medical centers included in this study were the pediatric and medicine departments of Hospital A, a 798-bed hospital with 27,500 discharges annually, and the pediatric department of Hospital B, a free-standing children’s hospital with 283 beds and 12,300 discharges annually. The medicine department of Hospital B was not using a computerized documentation system at the time of the survey. The three study departments had inpatient electronic note writing capabilities as part of a commercial electronic medical record system for at least 3 years. The CCHIT (Certification Commission for Health Information Technology) certified vendor system offered preconfigured templates for inpatient note documentation, including admission, progress, procedure and discharge notes. Most information was entered as free text by physicians. Certain vital signs and laboratory values could be imported directly into notes from flow sheets. Each hospital used a different version of the system.
In Hospital A’s older version, each templated note was a single free text document. Physicians could copy all or parts of a previous note. Hospital B had switched from this version to a newer version of the documentation system a year prior to survey. In this new version, templated notes were separated into different text boxes or fields (including subjective, past medical history, assessment and plan). The physical exam field could be completed using a checklist or free text. Physicians could use a ‘copy forward’ function in which separate note fields could be individually forwarded into fields of a new note. Physicians could still copy and paste in this system by writing notes as free text documents instead of templated documents, or by copy and pasting each field of the note separately into a new note. Both pediatric departments required all resident and general pediatrician notes to be electronic, while consult service and specialist participation were varied. In the medicine department, writing notes electronically was not mandatory.
Survey Population All resident physicians in the three departments were included in this study. Five faculty divisions of each department were selected for inclusion: the four divisions with the largest inpatient services (general pediatrics or internal medicine, critical care, cardiology and oncology) and one division with primarily inpatient consulting responsibility (infectious disease). The division faculty lists were reviewed by department leaders and division chairs to identify physicians who completed at least 2 weeks of clinical inpatient service in the last academic year.
Survey Instrument We identified important considerations regarding CPF by literature review and key informant interviews. Relevant articles found in Ovid Medline using the key word searches: ‘copy and paste’ and ‘computerized physician documentation’ as well as the subject headings: ‘copying processes,’ ‘user computer interface,’ ‘documentation,’ ‘medical records systems, computerized,’ ‘attitudes to computers’ and ‘attitudes of health personnel’ were reviewed. In addition, 15 semi-structured interviews were conducted with residents, faculty physicians and leaders within the hospital areas of patient safety, legal affairs, billing compliance and clinical informatics. All interviewees reported the ability to distinguish between progress notes written with and without CPF by comparing them to the previous patient notes. Ideas and concepts from these two sources were translated into survey questions and pilot tested for clarity and content validity by an additional 15 residents and faculty.
The 22-question survey incorporated a definition of CPF that included the copy-forward function and excluded the automatic insertion of vital signs and results. Respondents were asked whether they wrote inpatient notes electronically on the hospital documentation system, on paper or a combination of both. Physicians who wrote at least some notes electronically were asked about their comfort level writing notes electronically and the frequency and pattern of their CPF use. All opinions were assessed using five-point Likert scales. Physicians who acknowledged reading electronic notes were asked how frequently they noted flaws in progress notes written using CPF compared to other electronic notes, how CPF affected physician documentation overall and CPF’s effect on the ability of progress notes to serve several purposes (e.g., to communicate a patient’s daily course, to document a patient’s entire course or to document for billing or legal purposes). They were also asked if they have ever made a mistake in patient care that they felt was a result of being confused by a note containing copy and pasted text (yes, no or unsure) and asked their opinion of several proposed changes to CPF use. Demographic information collected included gender, training level, year of birth and year of medical school graduation. A copy of the survey is available online as an appendix.
Data Collection The study protocol and survey were approved by the Institutional Review Boards of the two hospitals before the confidential, self-administered survey was sent to all eligible physicians via e-mail using an online survey tool. Non-respondents were sent two additional e-mail surveys at 2-week intervals and were contacted by phone or page a maximum of two times. In addition, paper copies were brought to resident conferences, and a paper copy was mailed to the offices of all faculty non-respondents. No financial incentives were given for the completion of the survey.
Statistical Analysis Comparisons between (1) survey respondents and non-respondents, (2) electronic note writers (physicians who wrote their inpatient notes electronically on the hospital system) and non-electronic note writers (physicians who wrote paper notes) and (3) CPF users and non-CPF users (including electronic note writers who never used CPF and non-electronic note writers) were performed using chi-square or Fisher exact tests for categorical variables, and t-tests, or ANOVA for continuous variables. Multivariate logistic regression models were used to determine independent predictors associated with (1) electronic note writers versus non-electronic note writers and (2) high (used CPF almost always or most of the time when writing progress notes) versus low CPF use (used CPF sometimes or rarely). All analyses were performed using SAS for PC version 9.1.
RESULTS
A total of 451 physicians were eligible to participate in this study, including all 250 resident physicians (120 pediatric, 130 medicine). Of 438 faculty physicians in the three departments, 297 were within the five selected divisions and 201 had at least 2 weeks inpatient clinical time. The eligible faculty population varied among departments depending on the department size and use of hospitalists. Three hundred fifteen physicians responded to the survey, yielding a response rate of 70%. Three physicians (<1%) began but did not complete the survey. The only significant difference between respondents and non-respondents was that residents earlier in their training were more likely than senior residents to be respondents (p = 0.02, Table 1).
Table 1.
Study Population and Comparisons Between Respondents and Non-respondents
| Characteristic* | Study population | All respondents | Non-respondents | p-value |
|---|---|---|---|---|
| All physicians | N = 451 | N = 315 | N = 136 | |
| Female gender | 270 (60) | 187 (59) | 83 (61) | 0.74 |
| Hospital A | 287 (64) | 196 (62) | 91 (67) | 0.34 |
| Pediatricians | 256 (57) | 186 (59) | 70(51) | 0.14 |
| Residents | 250 (55) | 167 (53) | 83 (61) | 0.12 |
| Residents only | N = 250 | N = 167 | N = 83 | |
| Residency year† | ||||
| First | 83 (33) | 63 (38) | 20 (24) | 0.02 |
| Second | 77 (31) | 54 (32) | 23 (28) | |
| Third | 89 (36) | 50 (30) | 39 (48) | |
| Faculty only | N = 201 | N = 148 | N = 53 | |
| Years since graduation (mean, SD)‡ | 20 (9.5) | 19.8 (9.7) | 20.5 (8.7) | 0.67 |
| Primary care | 50 (25) | 40 (27) | 10 (19) | 0.24 |
| Subspecialists only | N = 151 | N = 108 | N = 43 | |
| Subspecialty | ||||
| Cardiology | 42 (28) | 23 (21) | 19 (44) | 0.07 |
| Critical care | 27 (18) | 23 (21) | 4 (9) | |
| Oncology | 38 (25) | 28 (26) | 10 (23) | |
| Infectious disease | 21 (14) | 16 (15) | 5 (12) | |
| Neonatology | 23 (15) | 18 (17) | 5 (12) |
*N (%) unless otherwise indicated
†One observation missing for residency year
‡Two observations missing for years since graduation
Use of Computerized Documentation System As shown in Figure 1, 253 (80%) of the 315 respondents wrote their inpatient notes electronically, including 193 who wrote all of their notes electronically and 60 who used a combination of electronic and paper notes. Ninety-seven percent of residents were electronic note writers compared to 61% of faculty. Resident physicians, physicians at hospital A with the older documentation system and younger physicians were independently more likely to be electronic note writers (Table 2). Among faculty, primary care physicians and physicians working at hospital A were independently more likely to be electronic note writers.
Figure 1.
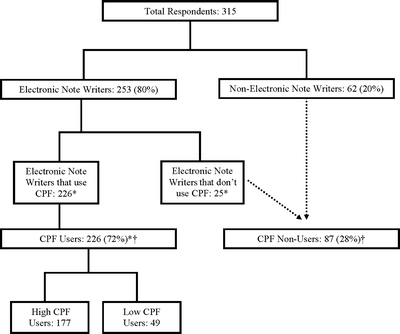
Flow diagram of respondents. *Two electronic note writers did not indicate whether they use CPF, total respondents = 313. †Of the 313 respondents, 304 (97%) reported reading electronic patient notes (223 CPF users and 81 CPF non-users).
Table 2.
Univariate and Multivariate Associations of Writing Notes Electronically
| All respondents (n = 315) | Faculty respondents only (n = 148) | |||
|---|---|---|---|---|
| Characteristic | Univariate odds ratio (95% CI) | Multivariate odds ratio (95% CI) | Univariate odds ratio (95% CI) | Multivariate odds ratio (95% CI) |
| Female gender | 1.7 (1.0, 3.0) * | 1.2 (0.6, 2.4) | 1.3 (0.7, 2.5) | — |
| Age (per 1-year increase) | 0.9 (0.9, 0.9)* | 1.1 (1.0, 1.1) † | 1.0 (0.9, 1.0)* | 1.0 (0.9, 1.0) |
| Hospital A | 3.7 (2.1, 6.5)* | 2.6 (1.3, 4.9) † | 3.6 (1.8, 7.3)* | 4.3 (2.0, 9.4) † |
| Pediatricians | 0.8 (0.5, 1,5) | — | 0.8 (0.4, 1.6) | — |
| Residents | 20.3 (7.9, 52.5)* | 7.6 (2.3, 24.7) † | — | — |
| Primary care physician | — | — | 8.7 (2.9, 26.0)* | 9.9 (3.2, 31.6) † |
| Inpatient service time | ||||
| <3 months/year | Reference | |||
| 3 to 6 months/year | 0.9 (0.4, 1.9) | |||
| >6 months/year | 0.7 (0.3, 1.7) | |||
*Variables in which p ≤ 0.1 were included in the multivariate model
†p < 0.05 in multivariate model
Use of the Copy and Paste Function Ninety percent of the 253 electronic note writers reported they used CPF when writing daily progress notes (Fig. 1). Among these 226 CPF users, 177 (78%) were high CPF users (used CPF almost always or most of the time when writing progress notes). Residents were almost three times more likely to be high rather than low CPF users compared with faculty physicians (OR = 2.9, 95% CI = 1.5, 5.7), while age, gender, hospital, specialty and comfort writing notes electronically were not independently related to frequency of use.
CPF users frequently copied notes written by other physicians (81%) and notes written during past visits or admissions (72%). Forty-seven percent of CPF users at Hospital B with the copy forward function and 69% at Hospital A (p = 0.002) copied either the entire note or part of the note, including the physical exam.
Impact of CPF Use Three hundred and four of the 315 respondents reported reading electronic patient notes, including 223 CPF users and 81 non-users. Although CPF non-users were more likely to recognize flaws in notes created with CPF compared to electronic notes written without CPF, the majority of both users and non-users agreed CPF notes contained more outdated and inconsistent information and were more difficult to find new information within (Table 3). CPF non-users were also more likely than users to agree CPF notes led to confusion or mistakes in patient care (Table 3), but only a quarter of all electronic note readers agreed and only eight physicians (3%) reported they made a mistake in patient care resulting from being confused by a note that contained copy and pasted text. Fifty-six (19%) were unsure. Many resident respondents explained they used other methods to keep track of patient data: “No (I have not made a mistake) - only because we carry around handwritten notes (residents’ sheets) at all times and those are usually trustworthy.” Most CPF users felt that CPF had improved physician documentation overall and the ability of progress notes to communicate a patient’s daily course and document for legal purposes, while most non-users disagreed (Table 3). The majority of both users and non-users, however, thought CPF improved the documentation of a patient’s entire hospital course, and approximately half of both users and non-users thought that CPF improved billing documentation.
Table 3.
Attitudes Towards CPF Use Among CPF Users and CPF Non-users (Non-users Include 25 Electronic Note Writers Who Do Not Use CPF and 62 Non-Electronic Note Writers)
| Characteristic* | All respondents N = 302† | CPF users N = 226 | CPF non-users N = 87 | p-value |
|---|---|---|---|---|
| CPF impact on notes: Physicians who agree that electronic notes written using CPF compared to other electronic notes (are): | ||||
| More trustworthy | 32 (11) | 27 (12) | 5 (6) | 0.13 |
| More difficult to find new information within | 183 (61) | 116 (52) | 67 (83) | <0.001 |
| Contain more outdated information | 215 (71) | 146 (66) | 69 (85) | 0.001 |
| Contain more inconsistent information | 214 (71) | 152 (69) | 62 (77) | 0.18 |
| Lack documented justification for clinical decisions | 74 (23) | 35 (16) | 35 (43) | <0.001 |
| Lead to more confusion in patient status or course | 83 (27) | 40 (18) | 43 (53) | <0.001 |
| More likely to lead to a mistake in patient care | 74 (25) | 47 (21) | 27 (33) | 0.03 |
| CPF impact on note use: Physicians who feel CPF has improved: | ||||
| Communication of patient’s daily course | 165 (55) | 146 (66) | 19 (24) | <0.001 |
| Documentation of entire hospital course | 238 (79) | 193 (87) | 45 (56) | <0.001 |
| Documentation for legal purposes | 120 (40) | 105 (48) | 15 (19) | <0.001 |
| Documentation for billing | 138 (46) | 100 (46) | 38 (49) | 0.64 |
| Physician documentation overall | 168 (56) | 153 (69) | 15 (19) | <0.001 |
| Future CPF use: Physicians who agree: | ||||
| CPF use should be continued | 246 (82) | 199 (91) | 47 (58) | <0.001 |
| CPF Education needed | 272 (91) | 198 (90) | 74 (91) | 0.80 |
| CPF text should be identifiable | 133 (44) | 80 (37) | 53 (65) | <0.001 |
| Alerts should indicate notes too similar | 113 (38) | 70 (32) | 43 (53) | <0.001 |
| Should not allow copying all types of notes | 139 (46) | 91 (42) | 48 (59) | 0.006 |
| Should not allow copying from another author | 70 (23) | 35 (16) | 35 (44) | <0.001 |
| Should not allow copying certain types of notes | 51 (17) | 18 (8) | 33 (41) | <0.001 |
*N (%) unless otherwise indicated
†Three missing
Future CPF Use Most physicians agreed that the CPF should be continued in future documentation systems, and more than 90% believed education on using CPF responsibly should be provided to physicians (Table 3). CPF users were significantly less supportive than non-users of changes in CPF use, including having copy and pasted text be readily identifiable (highlighted or italics), alerts that notify writers when their note does not differ significantly from prior notes, and restrictions on parts of notes from being copied (i.e., physical exam). CPF users seemed particularly resistant to limitations on copying from other authors or from certain types of notes (i.e., admission notes).
DISCUSSION
The use of the copy and paste function appears to have become an integral part of electronic note writing among physicians using a hospital computerized documentation system and the copying of physical exams and notes from other authors and from past visits, deemed “high risk” in previous studies4,5, is common. While articles in the medical literature suggest CPF use in electronic note writing may threaten the usefulness of physician documentation5 and the safety of patient care4–6,14, physicians in our study did not largely report the same beliefs. Although it is currently unknown whether CPF use or the introduction of electronic note writing has enhanced or jeopardized physician documentation and patient care, most physician respondents did acknowledge that CPF-created notes contained content flaws previously described in the literature3,13. It is unclear why these flaws have not translated into negative perceptions of CPF on the part of more physicians.
Physician reluctance to report negative outcomes is well known15, and in our study, CPF users may be especially unwilling or unable to recognize pitfalls in a function that allows them to cope with increasing demands on their time. Resident and faculty physicians currently carry a heavier patient workload daily due to the reduction in residency work hours16,17, the shift of inpatient care from primary physicians to hospitalists18, and reductions in the average patient length of stay19,20. Health IT implementations, themselves, may have introduced additional time burdens as note writing and ordering have moved away from patients’ bedsides3.
Resident physicians, who represent the preponderance of electronic note writers and CPF users, may be more susceptible to these time constraints. Alternatively, the differences in the attitudes of CPF users and non-users may reflect a different understanding of the purpose of patient notes among resident and faculty physicians. In our study, residents report maintaining other methods including handwritten or typed sheets to keep track of patient information for daily clinical decision-making and communication. This parallel record implies that electronic notes are not meeting all their documentation needs, whether due to content, structure or an inherent property of computerized documentation systems, such as their reduced portability. Maintaining two records, however, would seem to add work, reduce efficiency and introduce potential for error21.
If not to document daily changes, physicians may value electronic notes for other reasons. Physicians in our study reported CPF most improved documentation of patients’ entire hospital course. Running summaries have likely become valuable tools, as the inpatient population co-morbidity has increased over time22, and patients are cared for by more physicians during a hospital stay23. Approximately half of all respondents also believed that the use of CPF improved documentation for billing irrespective of their note-writing preferences, and half of all CPF users believed it improved documentation for legal purposes. Our key informants from the offices of billing compliance and legal affairs, however, disagreed, stating that the ability to assess daily changes in patient condition and care is most important in billing and legal documentation. This disparity between what physicians and billing and legal advisers value in patient notes may increase the risk of billing fraud and legal liability.
Although CPF users report that CPF has improved physician documentation overall, they likely recognize the existence of irresponsible CPF use as evidenced by their identification of flaws in the content of CPF notes and their unified support of physician education in the responsible use of CPF. In addition, their resistance to making copy and pasted text identifiable may reflect an inadvertent acknowledgement of irresponsible use. The best way to improve the content of electronic physician notes, however, is not clear. Limitations or restrictions to CPF use were rejected by physicians in our survey, and the danger of not incorporating their opinions in designing health IT systems is widespread refusal to use the systems24,25. Physician educational interventions, although supported by our respondents, have had mixed results in other areas26,27. Changing the computerized documentation system to better meet both resident and faculty physicians’ needs might prove more effective in modifying physician behavior. A system that is portable and can integrate daily and long-term patient information concurrently might provide adequate incentive for physicians to keep entered information accurate and up to date.
As this study was designed to ascertain physician perceptions of CPF use and not objective data, it was limited by the recall and social desirability biases of the respondents. In addition, although we included a definition of CPF in our survey, copy and pasted material is not readily identifiable within the EMR. We relied on the respondents’ ability to differentiate between CPF and non-CPF notes to answer questions about the structure and content of these notes. This survey involved physicians from two affiliated academic institutions with similar documentation systems and may not be generalizable to other health-care staff and physicians at different hospitals with other documentation systems. However, the CPFs at the two hospitals were significantly different, as were the patterns of CPF use, making the results more robust than a single site survey would provide.
CONCLUSION
Both CPF use and the changes in the practice of hospital medicine have contributed to shifts in the structure, content and use of inpatient notes. CPF use has become an integral part of patient note writing and simple restrictions or changes to its use will likely decrease acceptance by physicians. Defining and streamlining purposes of patient notes could add much valued efficiency and accuracy to physician documentation.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOC 108 KB)
Acknowledgements
The authors would like to thank Drs. Erika Abramson, Susan Bostwick, Joseph Cooke, and Charles Schleien. Dr. O’Donnell was funded through the Department of Public Health at Weill Cornell Medical College as a Fellow in Outcomes and Effectiveness Research. The authors of this study have no financial conflicts of interest to disclose.
This study was funded by Weill Cornell Medical College through support for Dr. O’Donnell as part of her fellowship in the Department of Public Health. There was no external funding for this study.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-008-0843-2) contains supplementary material, which is available to authorized users.
Portions of the study data were presented at the Gerontological Society of America Annual Scientific Meeting in San Francisco, CA, in November, 2007 and the Pediatric Academic Society Annual Conference in Honolulu, HI, in May, 2008.
References
- 1.Walton RT, Harvey E, Dovey S, Freemantle N. Computerised advice on drug dosage to improve prescribing practice. Cochrane Database Syst Rev. 2001;CD002894. [DOI] [PubMed]
- 2.Kohn LCJ, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Committee on Quality in America. Washington, DC: Institute of Medicine, National Academy Pr: 1999.
- 3.Embi PJ, Yackel TR, Logan JR, Bowen JL, Cooney TG, Gorman PN. Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians. J Am Med Inform Assoc. 2004;11:300–9. [DOI] [PMC free article] [PubMed]
- 4.Hammond KW, Helbig ST, Benson CC, Brathwaite-Sketoe BM. Are electronic medical records trustworthy? Observations on copying, pasting and duplication. AMIA Annu Symp Proc. 2003;269–73. [PMC free article] [PubMed]
- 5.Thielke S, Hammond K, Helbig S. Copying and pasting of examinations within the electronic medical record. Int J Med Inform. 2007;76(Suppl 1):122–8. [DOI] [PubMed]
- 6.Weir CR, Hurdle JF, Felgar MA, Hoffman JM, Roth B, Nebeker JR. Direct text entry in electronic progress notes. An evaluation of input errors. Methods Inf Med. 2003;42:61–7. [PubMed]
- 7.Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc. 2004;11:104–12. [DOI] [PMC free article] [PubMed]
- 8.Berger RG, Kichak JP. Computerized physician order entry: helpful or harmful? J Am Med Inform Assoc. 2004;11:100–3. [DOI] [PMC free article] [PubMed]
- 9.Han YY, Carcillo JA, Venkataraman ST. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2005;116:1506–12. [DOI] [PubMed]
- 10.Zhan C, Hicks RW, Blanchette CM, Keyes MA, Cousins DD. Potential benefits and problems with computerized prescriber order entry: analysis of a voluntary medication error-reporting database. Am J Health Syst Pharm. 2006;63:353–8. [DOI] [PubMed]
- 11.Koppel R, Metlay JP, Cohen A. Role of computerized physician order entry systems in facilitating medication errors. Jama. 2005;293:1197–203. [DOI] [PubMed]
- 12.Hartzband P, Groopman J. Off the record-avoiding the pitfalls of going electronic. N Engl J Med. 2008;358:1656–8. [DOI] [PubMed]
- 13.Hirschtick RE. A piece of my mind. Copy-and-paste. JAMA. 2006;295:2335–6. [DOI] [PubMed]
- 14.Yackel TR, Embi PJ. Copy-and-paste-and-paste. JAMA. 2006;296:2315. author reply -6. [DOI] [PubMed]
- 15.Leape LL. Reporting of adverse events. N Engl J Med. 2002;347:1633–8. [DOI] [PubMed]
- 16.Reed DA, Levine RB, Miller RG. Effect of residency duty-hour limits: views of key clinical faculty. Arch Intern Med. 2007;167:1487–92. [DOI] [PubMed]
- 17.Okie S. An elusive balance-residents’ work hours and the continuity of care. N Engl J Med. 2007;356:2665–7. [DOI] [PubMed]
- 18.Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514–7. [DOI] [PubMed]
- 19.Kozak LJ, DeFrances CJ, Hall MJ. National Hospital Discharge Survey: 2004 annual summary with detailed diagnosis and procedure data: National Center for Health Statistics: 2006. [PubMed]
- 20.Levit K, Ryan K, Elixhauser A, Stranges E, Kassed C, Coffey R. HCUP Facts and Figures: Statistics on Hospital-Based Care in the United States, 2005. Rockville, MD: Agency for Healthcare Research and Quality; 2007. [PubMed]
- 21.Arora V, Kao J, Lovinger D, Seiden SC, Meltzer D. Medication discrepancies in resident sign-outs and their potential to harm. J Gen Intern Med. 2007;22:1751–5. [DOI] [PMC free article] [PubMed]
- 22.Merill CT, Elixhauser A. Hospitalization in the United States, 2002. Rockville, MD: Agency for Heathcare Research and Quality; 2005.
- 23.Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006;166:1173–7. [DOI] [PubMed]
- 24.Connolly C. Cedars-Sinai doctors cling to pen and paper. Washington Post. March 21, 2005: A01.
- 25.Scott JT, Rundall TG, Vogt TM, Hsu J. Kaiser Permanente’s experience of implementing an electronic medical record: a qualitative study. Bmj. 2005;331:1313–6. [DOI] [PMC free article] [PubMed]
- 26.Davis D, O’Brien MA, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? Jama. 1999;282:867–74. [DOI] [PubMed]
- 27.Reeves S, Zwarenstein M, Goldman J, et al. Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2008:CD002213. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.
(DOC 108 KB)


