Abstract
Background
The working alliance has been shown to be a consistent predictor of patient outcome and satisfaction in psychotherapy. This study examines the role of the working alliance and related behavioral indices in predicting medical outcome.
Objective
Cognitive and emotional dimensions of the physician–patient relationship were examined in relation to patients’ ratings of physician empathy, physician multicultural competence, perceived utility of treatment, and patients’ adherence self-efficacy. These factors were then examined as part of a theoretical framework using path analyses to explain patient self-reported adherence to and satisfaction with treatment.
Design
The study was based on an ex-post facto field correlation design.
Participants
One hundred fifty-two adult outpatients from a neurology clinic at Bellevue Hospital, a large municipal hospital in New York City, participated in the study.
Interventions
Surveys given to participants.
Measurements
We used the following measurements: Physician–Patient Working Alliance Scale, Perceived Utility Scale, Treatment Adherence Self-Efficacy Scale, Medical Outcome Study Adherence Scale, Physician Empathy Questionnaire, Physician Multicultural Competence Questionnaire, Medical Patient Satisfaction Questionnaire.
Main Results
The effect sizes for adherence are between 0.07 and 0.21 and for satisfaction between 0.10 to >0.50. Regression and path analyses showed that ratings of physician multicultural competence and patient adherence self-efficacy beliefs predicted patient adherence (SB = 0.34) and (SB = 0.30) and satisfaction (SB = 0.18) and (SB = 0.12), respectively. Working alliance ratings also predicted patient satisfaction (SB = 0.49).
Conclusions
Psychological and interpersonal dimensions of medical care are related to patient adherence and satisfaction. Medical care providers may be able to use these dimensions to target and improve health care outcomes.
KEY WORDS: working alliance, physician–patient relationship, multicultural competence, adherence, satisfaction
INTRODUCTION
The current study is a second report from a program of research that examines the association between patients’ perceptions of their relationship with their physicians and patients’ adherence and satisfaction with treatment. The relationship is defined in terms of the working alliance concept developed and examined for several decades in psychotherapy outcome research. The concept encompasses both cognitive and emotional factors emphasizing physician–patient agreement on the goals and tasks of treatment, and the development of trust and liking between them, particularly for the patient. The current study is a replication and extension of the first investigation, which focused on adapting a measure of the working alliance from psychotherapy for use in behavioral medicine research1. In this study, we examine the role of the working alliance in conjunction with other behavioral indices in explaining patient adherence and satisfaction.
The Working Alliance
Researchers are now investigating the direct role that the physician–patient relationship plays in the treatment and outcome of chronic and serious medical issues, such as diabetes, hypertension, and chronic pain. Despite efforts to examine the relationship via factors such as communication styles, time spent with patients, and friendlier patient-centered approaches in medical care (e.g., encouraging questions from patients), a conceptualization of the medical relationship has not been clearly articulated, particularly a model that accounts for the interplay between patient factors and provider-patient trust and agreement2,3.
Fuertes, Mislowack, Bennett, et al.1 reviewed the relevant literature and concluded that existing measures of the relationship focused on either the emotional or the more cognitive aspects of care, but not both facets simultaneously in one instrument. Additionally, they noted that many of these instruments focused on communication patterns but did not seem to capture agreement on the goals and tasks of treatment, which is at the heart of the working alliance concept.
The working alliance encompasses agreement on explicit goals of treatment, the extent to which there is agreement on explicit tasks outlined for the patient to achieve the goals of treatment, and the extent to which there is an emotional bond, characterized by liking and trust, between patients and their health care providers4. Extensive research on the working alliance has shown that it is a highly consistent and reliable predictor of outcome across modalities of psychological treatment5, and it is widely seen as a foundational and active dimension of any successful psychological treatment for all patients6. While doctors’ competence in medical techniques and skills is undoubtedly central to quality care, relational factors seem to also be important to the overall effectiveness of medical care.
Physician Empathy and Multicultural Competence
It is difficult to overestimate the importance of empathy in effective medical care and physician behavior7,8. Empathy is a fundamental skill in the psychotherapy process, and it has also been implicated as an important dimension of physicians’ communication style9. Empathy has been variously defined by researchers over the years to capture the deep listening and objective understanding of others’ experiences. In the medical literature, empathy has recently been formulated based on Davis’10 theory, which incorporates physician and patient characteristics, including emotional, cognitive, and behavioral indices that are of an intrapersonal and interpersonal nature, each with delineated outcomes for physicians and patients11. Medical researchers have examined the role of empathy in communication and patient care12 and found positive effects for physician empathy on patient care11.
Multicultural competence is defined as health care professionals’ ability to assess and monitor how their beliefs, values, and attitudes inform their views of people and their medical problems. Multicultural competence stresses the importance of cultural factors in bio-psycho-social processes, and it seems to be an increasingly emphasized dimension of effective medical care, particularly with ethnic minority and immigrant patients. The bio-psycho-social model of health care13 has evolved in response to the demographic changes that have taken place in the United States over the last 30 years and more recent evidence of outcome disparities for ethnic minority patients who receive medical care7. In the current study, multicultural competence is considered a key dimension for physicians in being able to create an agreeable, trusting, and solution-oriented working alliance with their patients. In the current study, we hypothesized positive associations between perceptions of physician empathy, multicultural competence, and ratings of the working alliance.
Perceived Utility and Adherence Self-Efficacy
In medical care research, perceived utility has not been studied in depth, but as DiMatteo, Hays, Gritz, et al.14 noted, expectations about usefulness of treatment have been shown to be related to health beliefs, and they have also appeared to be associated with various health behaviors, such as whether patients undergo regular breast examinations or wear car seat belts15,16.
Bandura17 defined self-efficacy as the belief in one’s ability to organize and perform behaviors necessary to achieve one’s goals, and several studies in the health psychology literature have found that adherence self-efficacy is associated with adherence to treatment18–20 and utilization of health-related coping strategies21–23. Patients’ beliefs that they can manage and adhere to their treatment regimen seem critical not only to their adherence to treatment, but also to their overall satisfaction with the quality of treatment received. In the current study, we assessed patients’ adherence self-efficacy beliefs regarding their prescribed treatment regimens, and we examined the level of association between such beliefs with their perceptions about the usefulness of treatment and of the working alliance. Given our review of the literature and understanding of these constructs, we hypothesized positive relationships between ratings of the working alliance and patients’ perceptions of the utility of treatment and adherence self-efficacy beliefs.
Adherence and Satisfaction
It is estimated that between 20–50% of patients do not adhere to their medical regimens24,25, and that economic costs due to this phenomenon range from 25 to 100 billion dollars a year in additional treatment and hospital admission costs14,26. Despite a considerable amount of research aimed at understanding the underlying factors associated with adherence failure, no appreciable or predictable effect sizes have been uncovered as a consequence of patient characteristics, personality traits, or demographic factors3. Osterberg and Blaschke26 argue that the term “adherence” is more appropriate than “compliance,” because it implies agreement and decision-making on the part of patients, and adherence is most likely to occur in a “therapeutic alliance” (p. 487) between doctor and patient. In their review of the medical literature, Osterberg and Blaschke26 also note “poor therapeutic relationships” as a factor in patient non-adherence (p. 490). With respect to patient satisfaction, it has been studied extensively for years, but in the current study we include it to account for its level of overlap with adherence and its role in our structured model. Given the prominent role of the working alliance in our program of research, we hypothesized that ratings of the working alliance would be significantly associated with patient adherence and satisfaction, above and beyond variance explained by perceived utility, adherence self-efficacy, multicultural competence, and empathy.
METHODS
Approximately 190 patients were approached for participation in the study and 152 agreed; most cited other appointments or a need to get home as reasons for not participating. Participants were outpatients from a general neurology clinic at Bellevue Hospital, a large municipal hospital in New York City. A power analysis prior to the study indicated that with a medium effect size expected, power set at 0.80, and significance levels set at 0.01, 134 patients would be needed to adequately test our hypotheses27. Patients were 81 men and 71 women, 33 were Euro-American, 66 African-American, 44 Hispanic, 6 Asian-American, and 3 did not specify their race. The average age was 45.1 (SD = 12.75). Approximately 68% of the participants were immigrants. Inclusion criteria included the following: patients (1) over the age of 18; (2) able to speak and read English; and (3) saw the same physician at least two times in the last 6 months, including the day of data collection, for one or more chronic medical conditions. Participants completed the survey in person at the clinic after their medical visit and were compensated $20. This study was approved by the Institutional Review Boards of Fordham University and New York University School of Medicine, and the Research Department at Bellevue Hospital.
MEASURES
The Physician–Patient Working Alliance Scale
(PPWA) was developed based on a measure used in psychotherapy research originally adapted by Tracey and Kokotovic28. Fuertes, Mislowack, Bennett, et al.1 described how the measure was adapted and reported the internal consistency to be 0.93, and 0.82, 0.72, and 0.89 for the tasks, goals, and bond subscales, respectively. An analysis of the correlations among the three subscales showed significant overlap, ranging from 0.75 to 0.80. A principal components yielded a one factor solution with structure coefficient values ranging from 0.62 to 0.86 (Eigen value of 7.11 explaining 59% of the variance. 1). Given these results, the overall scale is treated as a general measure of the alliance.
Perceived Utility Scale
We used four items from the Perceived Utility Scale of DiMatteo, Hays, Gritz, et al.’s14 Adherence Determination Questionnaire to assess participants’ attitudes about the usefulness of the current treatment plans prescribed by their physicians.
Treatment Adherence Self-Efficacy Scale
Adherence self-efficacy was assessed via a previously used treatment adherence self-efficacy measure18. Participants were asked to indicate their level of agreement on how likely they felt able to engage in behaviors amenable to their doctor’s treatment plan.
Medical Outcome Study (MOS)
We utilized four items from the General Adherence measure of the MOS29. These items provide investigators with a global indication of patient compliance by asking subjects to indicate how often during the past four weeks certain behaviors were true.
Physician Empathy Questionnaire (PEQ)
Empathy was measured using a revised (see Fuertes, Mislowack, Bennett, et al.1 for a description) version of the Jefferson Scale of Physician Empathy12.
Physician Multicultural Competence Questionnaire
Physician multicultural competence was assessed using a revised version of the Cross-Cultural Counseling Inventory-Revised (CCCI-R;30). The items were revised by changing the words “counseling” and “counselor” to “medical care” and “physician,” respectively.
Medical Patient Satisfaction Questionnaire
Fuertes, Mislowack, Bennett, et al.1 described how they developed an 11-item measure to assess patients’ global satisfaction with various realms of treatment.
Data Analyses
Data were analyzed via means and standard deviations, correlations, regression, and path analyses. Analyses were conducted using the AMOS 6.0/SPSS 14.0 statistical package. In terms of the path analyses, two path models were specified, corresponding to the two dependent variables of interest, namely patient satisfaction and adherence. In both models, correlations were only estimated between exogenous variables (e.g., multicultural competence, empathy). We also allowed free estimation of the co-variation of the residuals of endogenous variables. All error terms were assumed to be uncorrelated. Three types of fit indices were used to assess the overall fit of the model: the chi-square statistic, the comparative fit index (CFI), and the root mean square error of approximation (RMSEA). The chi-square statistic provides an asymptotically valid significance test of model fit. The CFI estimates the relative fit of the target model in comparison to a baseline model where all of the variables in the model are uncorrelated. The values of the CFI range from 0 to 1, with values greater than 0.95 indicating an acceptable model fit. Finally, the RMSEA is an index that takes the model complexity into account. An RMSEA of 0.05 or less is considered to be reasonable fit.
RESULTS
The following internal consistency coefficient alphas were found for each measure: 1) 0.90 for the physician–patient Working Alliance Scale, 2) 0.64 for the Perceived Utility Scale, 3) 0.89 for the Treatment Adherence Self-Efficacy Scale, 4) 0.68 for the four items from the General Adherence measure of the MOS, 5) 0.83 for the Physician Empathy Questionnaire, 6) 0.87 for the Physician Multicultural Competence Questionnaire, and 7) 0.90 for the Medical Patient Satisfaction Questionnaire. Table 1 presents the means, standard deviations, and zero-order correlations for all the variables. An inspection of the correlations reveals many positive and highly significant relationships among these variables. The correlations with adherence ratings can be classified as small to medium in effect size range (i.e., when these correlations are squared, they are between 0.07 and 0.21)27 and with satisfaction as small to large in effect size range (0.10 to >0.50). Small to medium effect sizes are also evident between empathy and satisfaction and between empathy and multicultural competence.
Table 1.
Means, Standard Deviations, and Correlations for All Variables ( = 152)
| Variable | M(SD) | Working alliance | Perceived utility of treatment | Medical treatment adherence self-efficacy | Patient adherence with treatment | Patient satisfaction with treatment | Physician empathy | Physician multicultural competence |
|---|---|---|---|---|---|---|---|---|
| Working alliance | 48.4(7.56) | 1.0 | - | - | - | - | - | - |
| Perceived utility of treatment | 15.6(2.58) | 0.58* | 1.0 | - | - | - | - | - |
| Medical treatment adherence self-efficacy | 33.9(6.55) | 0.44* | 0.45* | 1.0 | - | - | - | - |
| Patient adherence with treatment | 19.2(3.78) | 0.35* | 0.33* | 0.46* | 1.0 | - | - | - |
| Patient satisfaction with treatment | 43.0(7.63) | 0.77* | 0.53* | 0.45* | 0.33* | 1.0 | - | - |
| Physician empathy | 48.0(7.62) | 0.72* | 0.46* | 0.40* | 0.28* | 0.67* | 1.0 | - |
| Physician multicultural competence | 32.6(7.04) | 0.66* | 0.44* | 0.44* | 0.45* | 0.63* | 0.66* | 1.0 |
*P < 0.001
Table 2 presents the results of simultaneous regression analyses. With respect to patient satisfaction, the predictors explained 66 percent of the adjusted variance (F = 56.30, df1 = 5, df2 = 143, = 0.001, R2 = 0.67, AdjR2 = 0.66), with ratings of the working alliance being highly statistically significant and ratings of physician multicultural competence and patient adherence self-efficacy being statistically significant. With respect to adherence, the predictors explained 27 percent of the adjusted variance (F = 12.17, df1 = 5, df2 = 142, = 0.001, R2 = 0.30, AdjR2 = 0.27), with ratings of physician multicultural competence and patient adherence self-efficacy being highly statistically significant. Variance inflation for all these analyses was under 3, well below the highest recommended level of 10.
Table 2.
Simultaneous Regression Analyses on Patient Satisfaction and Adherence
| Variable | SB | T | P |
|---|---|---|---|
| Dependent variable: patient satisfaction with treatment | |||
| Working alliance | 0.49 | 5.86 | 0.001 |
| Physician empathy | 0.14 | 1.77 | 0.08 |
| Perceived utility of treatment | 0.03 | 0.45 | 0.65 |
| Physician multicultural competence | 0.18 | 2.46 | 0.02 |
| Medical treatment adherence self-efficacy | 0.12 | 2.14 | 0.04 |
| Dependent variable: patient adherence with treatment | |||
| Working alliance | 0.02 | 0.47 | 0.90 |
| Physician empathy | −0.17 | −1.46 | 0.27 |
| Perceived utility of treatment | 0.09 | 0.96 | 0.29 |
| Physician multicultural competence | 0.34 | 3.48 | 0.001 |
| Medical treatment adherence self-efficacy | 0.30 | 3.73 | 0.001 |
In terms of the path analyses, Figure 1 shows that the model of patient satisfaction fit the data well (χ2 (2, N = 145) =0.781, < 0.05, CFI = 1.00 and RMSEA = 0.00). Most paths in our model were significant, particularly the path from physician empathy to working alliance to satisfaction. The only path that was not significant was the perceived utility to satisfaction. The direct path from multicultural competence to satisfaction was only marginally significant. Figure 2 shows that the model of patient adherence provided an adequate but less than perfect fit to the data, (χ2 (4, N = 145) = 14.13, < 0.01, CFI = 0.97 and RMSEA = 0.13). The only significant paths to patient adherence were evident from physician multicultural competence and adherence self-efficacy.
Figure 1.
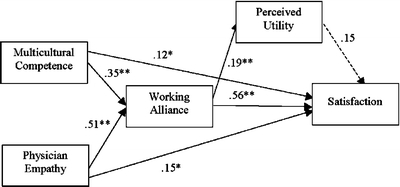
Model of patient satisfaction with standardized coefficients. Continuous lines note significant paths. Dashed lines note non-significant paths. Note ** < 0.001, * < 0.05
Figure 2.
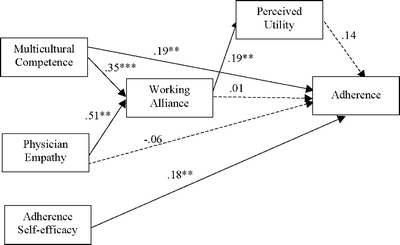
Model of patient adherence with standardized coefficients. Continuous lines note significant paths. Dashed lines note non-significant paths. Note ** < 0.001, * < 0.05
DISCUSSION
These results provide support for our hypotheses and specified path models, while also revealing unexpected findings. Our first hypothesis was supported in that we found strong effect sizes between perceptions of physician empathy, multicultural competence, and ratings of the working alliance. We also found support for the second hypothesis, in that we found moderate effect sizes between ratings of the working alliance and patients’ perceptions of the utility of treatment and adherence self-efficacy beliefs. Finally, we found partial support for our third hypothesis: we found that working alliance ratings were significantly associated with patient satisfaction but not adherence, above and beyond empathy, perceived utility, physician multicultural competence, and patient adherence self-efficacy. Unexpectedly, results from simultaneous regression analyses and path analyses showed that physician multicultural competence and adherence self-efficacy were highly associated with patient satisfaction and adherence.
The current study provides preliminary evidence about behavioral indices in medical care that are associated with patient satisfaction and adherence. These data speak to the value of physicians’ interpersonal behavior in affecting their patients’ experiences of treatment. Physician empathy was important to the patients in this study, and it may be helpful to note some of the items included in this scale: “It is important to me that my doctor understands my emotional status,” “My doctor’s understanding of my feelings gives me a sense of validation that is helpful,” and “I feel better when my doctor understands my feelings.” The prevalent theme in these items is that understanding of feelings is important and helpful to patients feeling better. Also important to patients was physician multicultural competence. Again, it seems helpful to note some of the items included in this scale: “My doctor seems to value and respect cultural differences,” “My doctor has a clear understanding of what is going on with me,” “My doctor communicates with me in an appropriate manner.” These items indicate that respect and proper communication yield strong results in terms of patient satisfaction and self-reported adherence. Physician multicultural competence may have earned for doctors the respect of the patients, and therefore they reportedly complied with the treatment; multicultural competence may have been important in the current study because the majority of patients surveyed were ethnic minorities (i.e., 72% African-American and Hispanic) and immigrants, while the majority of physicians, as reported by the patients, were Euro-American (i.e., 63%). Also important to self-reported treatment adherence is the role of patients’ adherence self-efficacy. Patients who feel capable of enacting behaviors expected of them by the doctor and the nature of the treatment (e.g., altering diet, increasing exercise, taking medication as prescribed) tend to exhibit those behaviors. This result has tremendous implications for treatment, for example, by highlighting the importance of assessing patient self-efficacy in the medical interview, and the value of health care providers intervening to enhance patients’ efficacious beliefs.
There are several limitations to the current study. The sample was comprised solely of neurology patients, and so this may limit the generalizability of these findings to other patient populations. Additionally, the sample was non-randomly obtained, and the results represent survey self-reports that may only partially reflect the true attitudes and perceptions of the participants. Although evidence exists that self-report measures tend to overestimate adherence behaviors, self-report data via questionnaires have been found to be more concordant with electronic adherence measures than other means of data gathering (e.g., interview data) 31. Despite this limitation, it is important to note that patients were guaranteed confidentiality and anonymity, and they were encouraged to express their true beliefs in responding to the survey items. A related limitation is that physicians’ assessments of both the working alliance and patient adherence were not included in the current design, which future research studies can address by including simultaneous ratings of both the patient and health care provider.
In summary, this second study in our program of research presents new findings about the important role of physician empathy and multicultural competence, along with patients’ adherence self-efficacy beliefs, in predicting patient satisfaction and adherence.
Acknowledgements
This study was funded by a grant from the Office of Research and Sponsored Programs at Fordham University.
Conflict of Interest None disclosed.
References
- 1.Fuertes JN, Mislowack A, Bennett J, et al. The physician patient working alliance. Patient Educ Couns. 2007;66:29–36. [DOI] [PubMed]
- 2.Laine C, Davidoff F. Patient-centered medicine. A professional evolution. JAMA. 1996;275:152–6. [DOI] [PubMed]
- 3.Christensen AJ, Johnson JA. Patient adherence with medical treatment regimens: an interactive approach. Curr Dir Psychol Sci. 2002;11:94–7. [DOI]
- 4.Bordin E. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research, and Practice. 1979;16:252–60. [DOI]
- 5.Wampold BE. Outcomes of individual counseling and psychotherapy: empirical evidence addressing two fundamental questions. In: Brown SD, Lent RW, eds. Handbook of Counseling Psychology. 3rd ed. New York: Wiley; 2000. pp. 3711–39.
- 6.Gelso CJ, Carter JA. The relationship in counseling and psychotherapy: components, consequences, and theoretical antecedents. J Couns Psychol. 1985;13:155–244. [DOI]
- 7.Zinn W. The empathic physician. Arch Intern Med. 1993;153:306–12. [DOI] [PubMed]
- 8.Rogers AI. The cornerstone of medicine: the physician–patient relationship. Am J Gastroenterol. 2007;102:1594–5. [DOI] [PubMed]
- 9.Silvester J, Patterson F, Koczwara A, Ferguson E. “Trust me...” Psychological and behavioral predictors of perceived physician empathy. J Appl Psychol. 2007;92:519–27. [DOI] [PubMed]
- 10.Davis MH. Empathy: A Social Psychological Approach. Boulder, CO: Westview Press; 1996.
- 11.Larson EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship. JAMA. 2005;293:1100–6. [DOI] [PubMed]
- 12.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Veloksi JJ, Magee M. The Jefferson Scale of Physician Empathy: further psychometric data and differences by gender and specialty at item level. Acad Med. 2002;77(10 Suppl):S58–60. [DOI] [PubMed]
- 13.Engle GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–36. [DOI] [PubMed]
- 14.DiMatteo MR, Hays RD, Gritz ER, et al. Patient adherence to cancer control regimens: scale development and initial validation. Psychol Assess. 1993;5:102–12. [DOI]
- 15.Ronis DL, Harel Y. Health beliefs and breast examination behaviors: analyses of linear structural relations. Psychol Health. 1989;3:259–85. [DOI]
- 16.Sutton SR, Eiser JR. The decision to wear a seat belt: the role of cognitive factors, fear, and prior behaviour. Psychol Health. 1990;4:111–23. [DOI]
- 17.Bandura A. Self-efficacy: The Exercise of Control. New York: W.H. Freeman; 1997.
- 18.Catz SL, Kelly JA, Bogart LM, Benotsch EG, McAuliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol. 2000;19:124–33. [DOI] [PubMed]
- 19.Eldred LJ, Wu AW, Chaisson RE, Moore RD. Adherence to antiretroviral and pneumocystis prophylaxis in HIV disease. J Acquir Immune Defic Syndr. 1998;18:117–25. [DOI] [PubMed]
- 20.Zebracki K, Drotar D. Outcome expectancy and self-efficacy in adolescent asthma self-management. Child Health Care. 2004;33:133–49. [DOI]
- 21.Bandura A, Cioffi D, Taylor CB, Brouillard ME. Perceived self-efficacy in coping with cognitive stressors and opioid activation. J Pers Soc Psychol. 1988;55:479–88. [DOI] [PubMed]
- 22.Jensen MP, Turner JA, Romano JM. Self-efficacy and outcome expectancies: relationship to chronic pain coping strategies and adjustment. Pain. 1991;44:263–9. [DOI] [PubMed]
- 23.Rokke PD, Fleming-Ficek S, Siemens NM, Hegstad HJ. Self-efficacy and choice of coping strategies for tolerating acute pain. J Behav Med. 2004;27:343–60. [DOI] [PubMed]
- 24.Berg JS, Dischler J, Wagner DJ, Raia JJ, Palmer-Shevlin N. Medication compliance: a healthcare problem. Ann Pharmacother. 1993;27(9 Suppl):S1–24. [PubMed]
- 25.Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med. 2007;167:540–50. [DOI] [PubMed]
- 26.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. [DOI] [PubMed]
- 27.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988.
- 28.Tracey TJ, Kokotovic AM. Factor structure of the Working Alliance Inventory. Psychol Assess. 1989;1:207–10. [DOI]
- 29.Hays RD. The Medical Outcomes Study (MOS) Measures of Patient Adherence. 1994. Available at: http://www.rand.org/health/surveys/MOS.adherence.measures.pdf. Accessed February 11, 2005.
- 30.LaFromboise TD, Coleman HLK, Hernandez A. Development and factor structure of the Cross-Cultural Counseling Inventory-Revised. Prof Psychol Res Pr. 1991;22:380–88. [DOI]
- 31.Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: a summary of the literature. Med Care. 2004;42:649–52. [DOI] [PubMed]


