ABSTRACT
BACKGROUND
Education about substance use (SU) disorders remains inadequate in medical training.
OBJECTIVE
To describe the Chief Resident Immersion Training (CRIT) program in addiction medicine and to evaluate its impact on chief resident (CR) physicians’ substance use knowledge, skills, clinical practice, and teaching.
DESIGN
A controlled educational study of CRIT programs (2003, 2004, and 2005) for incoming CRs in generalist disciplines. Intervention CRs were trained to diagnose, manage, and teach about SU. The control CRs sought but did not receive the intervention.
PARTICIPANTS
Eighty-six CR applicants to the CRIT program.
MEASUREMENTS
Baseline and 6-month questionnaires assessing substance use knowledge, skills, clinical practice, and teaching. Outcomes were compared within groups from baseline to follow-up and between groups at follow-up.
RESULTS
The intervention (n = 64) and control (n = 22) CRs were similar demographically. At 6-month follow-up, the intervention CRs reported a significant increase in SU knowledge, confidence, and preparedness to diagnose, manage, and teach and an increase in SU clinical and teaching practices compared to their baseline and control CRs.
CONCLUSIONS
This intensive training for chief residents (CRs) improved knowledge, confidence, and preparedness to diagnose, manage, and teach about substance use (SU), affecting both the CRs’ SU clinical and teaching practices. The CRIT program was an effective model for dissemination of SU knowledge and skills to educators in a key position to share this training with a broader audience of medical trainees. This model holds potential to address other high priority medical, yet under-addressed, content areas as well.
KEY WORDS: medical education, addiction, chief resident training, substance-related disorders
INTRODUCTION
Education about substance use (SU) disorders remains inadequate in medical training.1 This deficiency persists despite the contribution of SU to disability and premature death,2 and its prevalence and societal costs.3–5 Screening and management of SU merit a position in medical curricula that reflects the importance as a mainstream medical problem.6–10 Many physicians fail to address SU disorders because of discomfort with SU-related patient discussions,11 deficient knowledge and clinical skills,12,13 and negative attitudes,14,15 all resulting in barriers to providing optimal medical care for this population.16
Medical educators are starting to address this need for physician training in SU screening, assessment, and management.17–22 Formal curricula on these subjects have been developed23,24 and evaluated,25,26 and recommendations for the medical care of addicted patients have been published.6,27,28 Nevertheless, dissemination of up-to-date addiction research into generalist practice and into residency curricula remains a significant challenge.16,29,30
Substance use education aimed at improving physician trainees’ attitudes and clinical practice has been effective.31,32 Confidence in ability to screen and refer patients is positively associated with perceived responsibility and clinical practice.33 Wider dissemination of these practices requires creative strategies to develop a workforce that is knowledgeable about state-of-the-art approaches to patient management and motivated to implement such practices in a range of settings.1,26,34,35 As noted in the Institute of Medicine Report Improving the Quality of Health Care for Mental and Substance-Use Conditions,16 medical educators have not adequately addressed past recommendations to update training of medical professionals, leaving trainees ill equipped in their ability to care for patients with SU disorders.
Chief residents (CRs) play a key role in training future physicians.36 Not only is their teaching central to medical education,37,38 but CRs often become change agents in future leadership roles.39 Despite these pivotal roles, published efforts to advance medical training by capitalizing on the CRs role are rare. A training effort in SU that has influential medical educators and leaders, such as CRs, as its target audience has enormous potential to integrate SU clinical training into medical curricula and practice.36,40
The Chief Resident Immersion Training (CRIT) program sought to provide incoming generalist CRs with the scientific foundation of addiction medicine and state-of-the-art substance use (SU) diagnosis and management skills, in order to facilitate integration of SU content into residency program curricula and CR teaching.
METHODS
Study Design and Subjects
This study is a controlled educational evaluation of applicants to the 4-day annual CRIT program in Addiction Medicine from 2003–2005. The programs were advertised at http://www.bumc.bu.edu/CARE and by mailings to generalist residency training program directors and professional organizations. All applicants had accepted CR positions for the following academic year in internal medicine, family medicine, or emergency medicine, with priority given to outstanding candidates who (1) demonstrated the presence of a supportive faculty member to assist in promoting the teaching of substance use (SU) and (2) would have dedicated time for teaching during their CR year. Due to resource limitations, enrollment was limited to no more than 22 attendees per year based on their application, which included a curriculum vitae, personal statement, and letter of recommendation. The intervention group consisted of CRIT program attendees, while the control group consisted of applicants who were either not accepted or accepted but unable to attend. This study was approved by the Boston Medical Center Institutional Review Board.
CRIT Program Description
The CRIT program curriculum was developed by national experts in physician SU education. After the first year in 2002, the curriculum was modified based on attendees’ evaluations and an independent evaluator-led attendee focus group. Subsequent program evaluations gave feedback to faculty, resulting in minor teaching and programmatic modifications. The CRIT program was held at a conference center in Cape Cod, Massachusetts.
Curriculum and Faculty The CRIT curriculum (see Appendix A) utilized principles of adult and experiential learning and provided an in-depth evidence-based synthesis of major advances in the field of addiction medicine. The curriculum included a keynote address on the science of addiction, by a National Institute on Drug Abuse senior scientist. CRIT faculty, all with addiction and medical education expertise, role modeled teaching methods, including didactic case-based presentations, small group discussions, journal clubs, role plays, visits to Alcoholics Anonymous (AA) meetings, and small group conversations with individuals in recovery. Both the AA meeting visits and session with individuals in recovery were preceded by an orientation describing the learning objectives and followed by a debriefing session emphasizing the use of these curricular elements in teaching physician trainees. The use of experiential learning and specifically AA meeting visits41,42 are curricular elements that have been used successfully in physician training. Attendees received SU resources and teaching tools, including slide presentations, case studies for small group work, instructions and role descriptions for skill practice exercises, up-to-date medical literature, and important SU websites. The program also included instruction on teaching skills, including small group instruction, giving feedback, teaching reluctant learners, and ways to integrate SU issues into teaching.
Substance Use Teaching Project The CRIT curriculum included the development of a SU teaching project to enhance transfer of learning from the CRIT setting to the CRs’ work setting. Prior to arrival, CR attendees were asked to discuss possible SU teaching projects with their residency program director and a faculty mentor, giving consideration to residency program needs and CRs’ interests. The CRs explicitly stated project goals, objectives, implementation methods, potential resources and barriers, a timeline, and outcomes using a worksheet (see Appendix B). CRs met with CRIT faculty to further develop an achievable project. To encourage institutional support, a copy of the teaching project was sent to the CR’s mentor and residency program director.
Assessments
The outcome evaluation comparing the intervention and control CRs consisted of self-assessment questionnaires completed at the time of the CRIT application (baseline) and 6-months after the CRIT program (follow-up). The majority of questions used five-point Likert-type scales based on work by D’Onofrio et al.43 CRs were asked to rate their knowledge, skills, and confidence (“not at all” to “very”) and specific clinical and teaching practices (“never” to “always”). In addition, the intervention CRs completed a pre- and post-CRIT multiple-choice knowledge exam at the training based on didactic session content and an 11-month questionnaire about SU teaching project implementation and impact. The baseline, 6-, and 11-month follow-up questionnaires were administered via e-mail, and the pre- and post-CRIT knowledge exams were completed at the CRIT course. All were returned to the CRIT independent evaluator. Intervention CRs received a gift worth approximately $10, and control CRs received a $50 honorarium after completing the follow-up questionnaires. CRs used unique IDs for assessments to assure confidentiality.
Outcomes
Substance Use Clinical Knowledge, Skills, and Practice Multiple outcomes measured CRs knowledge, confidence, and self-reported SU clinical practices. The baseline and 6-month questionnaires assessed self-reported clinical knowledge and skills (SU neurobiology, screening, readiness to change assessment, referral options, pharmacotherapy, and relapse) and self-reported clinical confidence and practice (confidence in diagnosing SU problems and frequency of using screening tools with new patients, counseling drug and alcohol using patients, and referring drug- and alcohol-dependent patients for specialty treatment). A multiple-choice knowledge exam was administered to attendees immediately before and after the program.
Substance Use Teaching Skills and Practice Teaching outcomes included self-reported responsibility for, confidence in, and frequency of teaching about SU. Additionally, CRs were asked how prepared they felt to teach about SU compared to other chronic medical conditions (i.e., congestive heart failure and dementia). For the intervention CRs’ SU teaching project, outcomes included type of teaching activity, impact on residency program curriculum, and implementation facilitators and barriers.
Statistical Analysis
Baseline comparison of the intervention and control groups was performed using chi-square and t-tests, as appropriate, for analysis of the demographic variables (Table 1). The differences in self-reported knowledge, skills, and practice from baseline to 6-month follow-up were compared within each group using the paired t-test procedure (Table 2). Differences between group medians for outcomes at 6 months were examined using the Wilcoxon signed rank test. A two-sided p-value of 0.05 was considered statistically significant. Mean scores of the intervention group multiple-choice knowledge exams for attendees were compared.
Table 1.
Baseline characteristics of applicants (n = 86) to the Chief Resident Immersion Training (CRIT) program in addiction medicine 2003–2005, stratified by group
| Characteristic | Intervention n = 64 (%) | Control n = 22 (%) | p-value |
|---|---|---|---|
| Gender | |||
| Female | 30 (47) | 11 (50) | 0.81 |
| Race | 0.58 | ||
| White | 40 (63) | 15 (68) | |
| Black | 6 (9) | 2 (9) | |
| Asian | 14 (22) | 2 (9) | |
| Hispanic | 2 (3) | 1 (5) | |
| Other | 2 (3) | 2 (9) | |
| Age in years, mean [SD] | 30.3 [2.4] | 30.8 [4.4] | 0.61 |
| Specialty | 0.60 | ||
| Emergency medicine | 4 (6) | 1 (5) | |
| Family medicine | 4 (6) | 2 (9) | |
| Internal medicine | 56 (88) | 19 (86) | |
| Fellowship plans | 38 (59) | 12 (55) | 0.69 |
| Foreign medical graduate | 16 (25) | 6 (27) | 0.83 |
| Alpha Omega Alpha member | 5 (8) | 2 (9) | 0.85 |
| Mentor support named in application | 48 (75) | 12 (55) | 0.19 |
| Substance use (SU) usually/always a topic in residency program | 32 (50) | 10 (45) | 0.71 |
| Training in SU treatment is encouraged in residency program | 50 (78) | 15 (68) | 0.35 |
| Has informed, competent faculty member source of SU information | 54 (86)* | 21 (100)† | 0.07 |
*(n = 63)
†(n = 21)
Table 2.
Chief residents’ clinical knowledge, skills and practice and teaching skills and practice related to substance use (SU), at baseline and 6-month follow-up
| Intervention mean (SD) | Control mean (SD) | Difference between group follow-up mediansb (range) | |||
|---|---|---|---|---|---|
| Characteristic (on a scale of 1–5) | Baseline n = 64 | Follow-upa n = 64 | Baseline n = 22 | Follow-upa n = 19 | |
| Clinical knowledge, skills, and practice | |||||
| How knowledgeable are you about: | |||||
| Neurobiology of addiction? | 2.2 (0.8) | 3.3 (0.7)*** | 2.0 (0.6) | 2.4 (0.7)* | 1 (−2,4)* |
| Screening for substance use? | 3.1 (0.8) † | 4.2 (0.7)*** | 2.9 (0.8) | 3.2 (0.9) | 1 (−2,3)** |
| Readiness to change assessment? | 2.9 (1.0) † | 4.2 (0.9)*** | 2.5 (0.7) | 3.4 (0.9)** | 1 (−2,4) |
| Available referral options? | 2.7 (0.9) | 3.8 (0.8)*** | 2.6 (0.7) | 3.1 (0.8) | 1 (−2,4)* |
| Pharmacotherapy for addiction? | 2.9 (1.0) | 4.0 (0.8)*** | 2.7 (0.7) | 3.0 (0.7) | 1 (−2,3)** |
| Relapse? | 2.1 (0.8) | 3.4 (0.9)*** | 2.0 (0.7) | 2.5 (0.9)* | 1 (−1,4)* |
| How confident are you in diagnosing SU problems? | 3.1 (0.8) | 4.0 (0.8)*** | 3.3 (1.0) | 3.4 (0.8) | 1 (−2,3)** |
| How often do you: | |||||
| Use a SU screening tool with new patients? | 3.3 (0.9) | 4.0 (0.9)*** | 3.0 (1.1) | 3.1 (0.9) | 1 (−1,3)** |
| Counsel drug abusing patients about drug problems? | 3.9 (0.8) | 4.2 (0.7)** | 3.7 (0.8) | 4.0 (0.7) | 0 (−2,3) |
| Counsel drinkers about alcohol problems? | 3.9 (0.7) | 4.2 (0.7)** | 3.9 (0.7) | 4.0 (0.7) | 0 (−2,2) |
| Refer drug-dependent patients to treatment? | 3.8 (0.9) | 4.0 (0.9)* | 3.6 (0.8) | 3.8 (0.9) | 0 (−2,2) |
| Refer alcohol-dependent patients to treatment? | 3.8 (0.8) | 4.1 (0.8) | 3.7 (0.9) | 3.9 (0.8) | 0 (−2,2) |
| Teaching skills and practice | |||||
| How responsible do you feel for teaching about SU? | 4.2 (0.9) | 4.4 (0.7) | 4.3 (0.9) | 3.6 (1.0)* | 0 (−4,4)* |
| How confident are you in: | |||||
| Incorporating SU into your teaching? | 2.9 (1.0) | 4.0 (0.8)*** | 3.1 (1.2) | 3.1 (0.9) | 1 (−2,4)** |
| Making presentations on SU issues? | 2.7 (1.0) | 4.0 (0.8)*** | 2.7 (1.3) | 2.6 (0.8) | 1 (−3,4)** |
| Incorporating SU information into resident’s curriculum? | 3.1 (1.1) | 4.1 (0.8)*** | 3.1 (1.2) | 3.0 (1.0) | 1 (−2,4)** |
| How often do you: | |||||
| Cover alcohol abuse? | 2.5 (0.8) | 3.2 (0.7)*** | 2.1 (0.6) | 2.3 (0.9) | 0 (−3,3)* |
| Cover drug abuse? | 2.4 (0.8) | 3.0 (0.7)*** | 2.0 (0.6) | 2.3 (1.0) | 0 (−3,1) |
*p < 0.05, **p < 0.01, ***p < 0.001 †n = 60
aThe test of significance compared the baseline mean to the follow-up mean within each group
bThe test of significance compared the intervention group follow-up median to the control group follow-up median
RESULTS
Eighty-six chief resident (CR) applicants to the CRIT program (2003–2005) were assessed; 64 attended CRIT (intervention group), and 22 did not (control group). Of the control group, six had been accepted to the program. The baseline characteristics of the intervention and control groups were similar (Table 1). Applicants represented 56 different residency programs (87% internal medicine, 7% family medicine, and 6% emergency medicine) from 23 states. All intervention and control CRs completed the baseline assessment; 6-month follow-up was 100% (64/64) and 86% (19/22) for the intervention and control groups, respectively. All of the intervention CRs completed the pre- and post-CRIT multiple-choice knowledge exams. All intervention CRs developed a SU teaching project, and 98% (63/64) completed the 11-month follow-up questionnaire.
Substance Use Clinical Knowledge, Skills, and Practice (Table 2)
The intervention CRs showed significant improvement (p < 0.001) at 6-month follow-up compared to baseline assessment in self-reported knowledge on SU neurobiology, screening, readiness to change assessment, referral options, pharmacotherapy, and relapse. Similarly, they had increased confidence (p < 0.05) in diagnosing SU problems and more frequently used a SU screening tool with new patients, counseled drug and alcohol using patients, and referred drug-dependent patients to treatment. The control CRs improved in some outcomes from baseline to follow-up. When comparing the intervention group and the control group medians at 6-month follow-up, the intervention group displayed statistically significant (p < 0.05) improvement in self-reported knowledge of SU neurobiology, screening, referral options, pharmacotherapy, and relapse, as well as confidence in diagnosing SU problems and frequency of using a SU screening tool with new patients. The mean pre- and post-CRIT multiple-choice knowledge exam scores for the intervention CRs were 67% and 78% answers correct, respectively (p < 0.001).
Substance Use Teaching Skills and Practice (Table 2)
The intervention CRs showed significant improvement (p < 0.001) at 6-month follow-up compared to baseline in confidence in incorporating SU into teaching, making presentations on SU issues, and incorporating SU information into residents’ curriculum. The frequency of covering alcohol and drug abuse in teaching similarly improved. Differences between the intervention group and the control group medians at 6-month follow-up were also significant (p < 0.05) for those outcomes, with the exception of frequency of covering drug abuse. At baseline, both groups reported high levels of feeling responsible for teaching about SU. While the intervention CRs had no change in their reported levels of feeling responsible to teach about SU at follow-up, the control CRs had a significant decrease (p < 0.05). Almost all (97%) of intervention CRs reported being “more” or “much more” likely to incorporate SU content into their teaching as a result of their CRIT training. When reporting their preparedness to teach about SU and other chronic conditions (i.e., congestive heart failure, dementia), the intervention group showed significant improvement (p < 0.05) at follow-up in their preparedness to teach about alcohol abuse as compared to the control group (Fig. 1).
Figure 1.
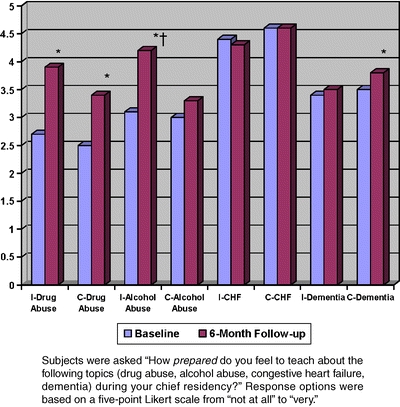
Changes in chief resident’s preparedness to teach substance use compared to other chronic conditions at baseline and 6-month follow-up by group {n = 86 [64 intervention (I), 22 control (C)] at baseline, and n = 83 [64 intervention (I), 19 control (C)] at 6-month follow-up}. *p < 0.05, comparing baseline to follow-up within group; †p < 0.05, comparing intervention to control group at 6-month follow-up. I = Intervention, C = Control.
Substance Use Teaching Project
All intervention CRs developed a SU teaching project. At 11-month follow-up, 86% (56/64) reported that their teaching project had an impact on their residency program curriculum. Examples of the SU teaching projects included new or expanded SU curriculum (n = 21), new SU lecture or teaching activity (n = 33), and SU screening protocols (n = 16). Two CRs published an assessment of the impact of their SU teaching project, one included taking residents and medical students to an Alcoholics Anonymous meeting 42 and the other the successful implementation of an “Educational Half Day” focusing on SU.44 CRs identified cooperative residency program staff and support from a mentor as the top two facilitators in helping to achieve their SU teaching project, while the top two barriers were time constraints and competing priorities.
DISCUSSION
The Chief Resident Immersion Training (CRIT) program in addiction medicine effectively transferred evidence-based SU knowledge and practice to 64 CRs in generalist disciplines and more importantly, enhanced the SU curriculum in 47 residency programs. Training CRs, who have a primary responsibility for educating medical trainees, appears to be one important pragmatic strategy to address the compelling need for better physician training in the identification and management of patients with SU-related problems.
Educating trainees about SU poses extraordinary challenges. Until a few decades ago, there was little research to guide the practice of addiction medicine by generalists. Yet in 1990, the Institute of Medicine stated that most patients with SU issues should receive care in a primary care setting.45 A decade later, Fiellin and colleagues described the basic core competencies in SU education for physicians and recommended increased efforts to provide physicians with a level of SU training commensurate with the economic and clinical impact of SU disorders.1 In 2008, medical education has yet to provide adequate training in SU, resulting in a dearth of generalist faculty with an interest and expertise in SU to serve as teachers, role models, or mentors. Recently, the National Institute on Drug Abuse has joined forces with the American Medical Association to improve SU training in medical education.21
Renner described three critical elements to successfully train physicians in addiction medicine: (1) an adequate knowledge base, (2) a positive attitude toward the patient and the benefits of treatment, and (3) a sense of responsibility for the clinical problem.46 The CRIT program exposed CRs to up-to-date SU knowledge and evidence-based practices. The immersion experience allowed CRs to focus on the CRIT curriculum without the inevitable distractions of their jobs at home. The faculty modeled different teaching methodologies with an emphasis on interactive learning. Meeting with individuals in recovery demonstrated the reality of treatment, its successes, and challenges. In addition, the physician faculty, all generalists with special expertise in addiction and medical education, served as role models of physicians who had successfully integrated academic, clinical, and research careers in addictions and medical education. The SU teaching project helped foster the transfer of SU knowledge and skills to the CRs’ home institutions. CRs were asked to identify a mentor at their institution as this support system was viewed as key to successful local implementation of teaching projects. The finding that intervention CRs had greater increases in self-perceived preparedness to teach about alcohol abuse compared to no changes in teaching about another chronic medical condition, such as dementia, which remained persistently low, highlights the fact that such improvements do not occur spontaneously.
Targeting CRs was a tactical decision in order to magnify the impact of the immersion program. Other successful interventions have increased the knowledge and skills of generalist residents,26,32 but have not demonstrated the potential to shift the values and culture of a residency program to include more SU training. In addition to being pivotal educators in the clinical training of students and residents, CRs have additional strengths. They are chosen for the high quality of their medical knowledge, clinical skills, and organizational abilities. As role models, CRs have the opportunity to impact the knowledge, skills, and attitudes of trainees. Surprisingly, there have been relatively few efforts to advance medical training by capitalizing on the role of CRs as influential instructors, leaders, and role-models. One example is a CRIT program for the care of older adults to teach geriatric medicine skills to a single institution’s chief residents.47 Engaging these key young medical leaders early in their careers when they are open to new ideas is a strategy with enormous educational potential.
The CRIT program evaluation has several limitations worth considering. The control group was smaller than the intervention group, and neither group was randomly assigned. If the control group had been larger, it is possible that some of the outcomes that were significant in the intervention group would have also been significant in the control group; however, the absolute change between baseline and follow-up was almost always smaller in the control group. The non-randomized nature of the study could have led to confounding. For example, because enrollment in the intervention group was based on selection by the CRIT program directors and 73% of the control group was not accepted, intervention CRs might have been more qualified than the controls. However, both groups were similar in the baseline variables measured. Another limitation is the overall small sample size, which makes it difficult to identify differences between groups. Nevertheless, many results did reach statistical significance. Next, it is possible that due to the self-reported nature of the data, some of the findings may be attributed to social desirability bias. Social desirability may have been more of an issue for the intervention group. To mitigate this bias, CRs returned their questionnaires to an independent evaluator, and were told that faculty and staff would only see de-identified aggregate data. While we found improvements in clinical knowledge, skills, and practice among the CR attendees, we were unable, by study design, to detect if these improvements continued downstream to their trainees. However, in two cases we are aware of CRs conducting their own assessment of impact of their teaching project.42,44 Future research on the CRIT model should consider a more in-depth investigation of impact on the CRs’ trainees. Finally, the conclusions of this study may not be generalizable to all generalist CRs, as the CRIT program enrolled CRs who self-selected for interest in this training and had a disproportionately high representation from internal medicine.
In summary, immersion programs directed at CRs incorporating a variety of teaching modalities and the explicit development of a teaching project can help transmit substance use knowledge and teaching expertise to medical trainees. Chief Resident Immersion Training (CRIT) impacted physicians who play a critical role in medical trainee education but are not often trained in substance use themselves. CRs are an untapped resource for changing medical education and practice about substance use disorders, and this CRIT model holds potential to address other high-priority medical content areas as well.
Acknowledgements
Preliminary study results were presented at the 27th annual meeting of the Society of General Internal Medicine in Chicago, IL, in May 2004, the 28th annual meeting of the Association for Medical Education and Research in Substance Abuse in Washington, DC, in November 2004 and the 67th annual meeting of the College on Problems of Drug Dependence in Orlando, FL, in June 2005. The authors thank the following for their contributions to the manuscript: Jacqueline Ashba, MA, MPH, and Don Allensworth-Davies, MSc, at the Data Coordinating Center, Boston University School of Public Health, Boston, MA (data management); Thomas W. Clark, formerly at Health and Addictions Research, Inc. (evaluation); Wendy Budwey, MSW (program management); the CARE Program Advisory Committee (program oversight); Nella P. Mupier, MPH (manuscript preparation); and Belle Brett, EdD, for thoughtful comments on this manuscript. Program support was provided by the National Institute on Drug Abuse R25 DA13582. Dr. Samet receives support from NIAAA: K24-AA015674.
Conflict of Interest None disclosed.
Appendix A: Example Schedule
Clinical teaching in addiction medicine. A Chief Resident Immersion Training (CRIT) program
| Day 1 | ||
| 12:00–3:30 | Arrival and hotel check-in | |
| 3:30–5:00 | Pre-CRIT multiple-choice knowledge exam | |
| 5:00–6:30 | Reception and dinner | |
| Welcome, opening remarks | ||
| 6:15–7:00 | Ice breaker | |
| “What was your most memorable adult learning experience? Why?” | ||
| Review of adult learning principles | ||
| 7:00–7:15 | Introduction to substance use teaching project | |
| 7:15–8:15 | Teaching project discussion: What is a doable chief resident project? | |
| Day 2 | ||
| 7:40–8:45 | Breakfast | |
| 8:45–9:00 | Introductions | |
| 9:00–10:00 | NIDA keynote address: The science of addiction | Dr. Condon/Miner (NIDA) |
| 10:15–10:35 | Principles of addiction | Dr. Samet |
| 10:35–11:05 | Screening | Dr. Barnes |
| 11:05–12:30 | Assessment and brief intervention | Dr. Samet |
| 12:30–3:00 | Lunch and break | |
| 3:00–3:30 | Alcohol: Inpatient management | Dr. Saitz |
| 3:30–4:00 | Opioids: Inpatient management | Dr. Alford |
| 4:00–4:30 | Running small groups | Dr. Jackson |
| 5:00–6:30 | Skills practice session I (three groups) | All faculty |
| 7:00–8:30 | Dinner/social | |
| Day 3 | ||
| 7:40–9:00 | Breakfast (one on one: teaching project discussion) | All faculty |
| 9:00–9:30 | Alcohol: Outpatient management | Dr. Saitz |
| 9:30–10:00 | Opioids: Outpatient management | Dr. Alford |
| 10:00–10:30 | Prescription drug abuse | Dr. Alford |
| 11:00–12:30 | Skills practice session II (three groups) | All faculty |
| 12:30–3:00 | Lunch and break | |
| 3:00–4:00 | Giving feedback/reluctant learner | Dr. Jackson |
| 4:10–5:10 | Five concurrent workshops | |
| HIV and substance use | Dr. Samet | |
| Clinical epidemiology rounds | Dr. Saitz | |
| Marijuana: Myths and realities | Dr. Barnes | |
| Tool kit for teachers | Dr. Jackson | |
| SU psychosocial services | Dr Amodeo | |
| 5:30–6:30 | Dinner | |
| 6:00–6:30 | Orientation: 12-Step meetings | Dr. Amodeo |
| 6:40–8:30 | 12-Step meetings | |
| 6:30–7:30 | One on one: Teaching project discussion | All faculty |
| Day 4 | ||
| 6:15–8:30 | 12-Step meetings | |
| 8:30–9:30 | Breakfast (one on one: Teaching project discussion) | All faculty |
| 9:40–10:00 | Debrief: 12-Step meetings | Dr. Amodeo |
| 10:00–10:30 | Stimulants and sedatives | Dr. Alford |
| 10:50–11:50 | Skills practice session III (three groups) | All faculty |
| 11:50–12:15 | Orientation: Luncheon with guests in recovery | Dr. Amodeo |
| 12:15–1:15 | Luncheon with guests in recovery | |
| 1:30–2:00 | Debrief: Luncheon with guests in recovery | Dr. Amodeo |
| 2:00–2:35 | Medical complications of substance use | Dr. Samet |
| 2:55–3:55 | Four selected teaching project presentations | Four participants |
| 3:55–4:20 | Questions and answers | Faculty |
| 4:20–5:00 | Incorporating substance use into curriculum | Dr. Barnes |
| 5:00–5:30 | Post-CRIT multiple-choice knowledge exam | |
| 5:45–7:00 | Dinner: Certificates of completion | |
| 7:00 | Adjourn |
Appendix B: SU teaching project worksheet
References
- 1.Fiellin D, Butler R, D’Onofrio G, Brown R, O’Connor P. The physician’s role in caring for patients with substance use disorders: Implications for medical education and training. Subst Abus. 2002;23:207–12. [DOI] [PubMed]
- 2.Michaud CM, Murray CJ, Bloom BR. Burden of disease—implications for future research. JAMA. 2001;285:535–9. [DOI] [PubMed]
- 3.NIAAA. Estimated economic costs of alcohol abuse in the United States, 1992 and 1998. Available at: http://www.niaaa.nih.gov/Resources/DatabaseResources/QuickFacts/EconomicData/cost8.htm. Accessed August 25, 2008.
- 4.Office of National Drug Control Policy. The economic cost of drug abuse in the United States, 1992–2000. Available at: http://www.whitehousedrugpolicy.gov/publications/economic_costs/. Accessed August 25, 2008.
- 5.SAMHSA. Results from the 2006 national survey of drug use and health: national findings. Available at: http://www.drugabusestatistics.samhsa.gov/NSDUH/2k6NSDUH/2k6results.cfm. Accessed August 25, 2008.
- 6.Friedmann PD, Saitz R, Samet JH. Management of adults recovering from alcohol or other drug problems: relapse prevention in primary care. JAMA. 1998;279:1227–31. [DOI] [PubMed]
- 7.Lewis DC. The role of internal medicine in addiction medicine. J Addict Dis. 1996;15:1–17. [DOI] [PubMed]
- 8.McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–95. [DOI] [PubMed]
- 9.Saitz R, Horton NJ, Larson MJ, Winter M, Samet JH. Primary medical care and reductions in addiction severity: a prospective cohort study. Addiction. 2005;100:70–8. [DOI] [PubMed]
- 10.Samet JH, Friedmann P, Saitz R. Benefits of linking primary medical care and substance abuse services: patient, provider, and societal perspectives. Arch Intern Med. 2001;161:85–91. [DOI] [PubMed]
- 11.McCormick KA, Cochran NE, Back AL, Merrill JO, Williams EC, Bradley KA. How primary care providers talk to patients about alcohol: a qualitative study. J Gen Intern Med. 2006;21:966–72. [DOI] [PMC free article] [PubMed]
- 12.Kuehn BM. Despite benefit, physicians slow to offer brief advice on harmful alcohol use. JAMA. 2008;299:751–3. [DOI] [PubMed]
- 13.Vastag B. Addiction poorly understood by clinicians: experts say attitudes, lack of knowledge hinder treatment. JAMA. 2003;290:1299–303. [DOI] [PubMed]
- 14.Saitz R, Friedmann PD, Sullivan LM, et al. Professional satisfaction experienced when caring for substance-abusing patients: faculty and resident physician perspectives. J Gen Intern Med. 2002;17:373–6. [DOI] [PMC free article] [PubMed]
- 15.Stimmel B, Cohen D, Colliver J, Swartz M. An Assessment of house staff’s knowledge of alcohol and substance abuse utilizing standardized patients. Subst Abus. 2000;21:1–7. [DOI] [PubMed]
- 16.Institute of Medicine. Improving the quality of health care for mental and substance-use conditions. Washington, DC: The National Academies Press; 2006. [PubMed]
- 17.Fleming MF, Barry KL, Davis A, Kropp S, Kahn R, Rivo M. Medical education about substance abuse: changes in curriculum and faculty between 1976 and 1992. Acad Med. 1994;69:362–9. [DOI] [PubMed]
- 18.Miller NS, Sheppard LM, Colenda CC, Magen J. Why physicians are unprepared to treat patients who have alcohol— and drug-related disorders. Acad Med. 2001;76:410–8. [DOI] [PubMed]
- 19.Foley ME, Garland E, Stimmel B, Merino R. Innovative clinical addiction research training track in preventive medicine. Subst Abus. 2000;21:111–9. [DOI] [PubMed]
- 20.Fleming MF, Manwell LB, Kraus M, Isaacson JH, Kahn R, Stauffacher EA. Who teaches residents about the prevention and treatment of substance use disorders? A national survey. J Fam Pract. 1999;48:725–9. [PubMed]
- 21.Kuehn BM. Centers to weave addiction treatment into medical education. JAMA. 2007;297:1763. [DOI] [PubMed]
- 22.Wyatt SA, Vilensky W, Manlandro JJ Jr., Dekker MA. Medical education in substance abuse: from student to practicing osteopathic physician. J Am Osteopath Assoc. 2005;105:S18–S25. [PubMed]
- 23.Project Mainstream: improving substance abuse education for health professionals. Available at: http://www.projectmainstream.net. Accessed March 11, 2008.
- 24.Klamen DL, Miller NS. Integration in education for addiction medicine. J Psychoactive Drugs. 1997;29:263–8. [DOI] [PubMed]
- 25.Alford DP, Richardson JM, Chapman SE, Dube CE, Schadt RW, Saitz R. A web-based Alcohol Clinical Training (ACT) curriculum: is in-person faculty development necessary to affect teaching? BMC Med Educ. 2008;8:11. [DOI] [PMC free article] [PubMed]
- 26.Parish SJ, Ramaswamy M, Stein MR, Kachur EK, Arnsten JH. Teaching about substance abuse with objective structured clinical exams. J Gen Intern Med. 2006;21:453–9. [DOI] [PMC free article] [PubMed]
- 27.Samet JH, Rollnick S, Barnes H. Beyond CAGE. A brief clinical approach after detection of substance abuse. Arch Intern Med. 1996;156:2287–93. [DOI] [PubMed]
- 28.Alford DP, Compton P, Samet JH. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann Intern Med. 2006;144:127–34. [DOI] [PMC free article] [PubMed]
- 29.Isaacson JH, Fleming M, Kraus M, Kahn R, Mundt M. A national survey of training in substance use disorders in residency programs. J Stud Alcohol. 2000;61:912–5. [DOI] [PubMed]
- 30.Abrams-Weintraub T, Saitz R, Samet JH. Education of preventive medicine residents: alcohol, tobacco, and other drug abuse. Am J Prev Med. 2003;24:101–5. [DOI] [PubMed]
- 31.Karam-Hage M, Nerenberg L, Brower KJ. Modifying residents’ professional attitudes about substance abuse treatment and training. Am J Addict. 2001;10:40–7. [DOI] [PubMed]
- 32.Chossis I, Lane C, Gache P, et al. Effect of training on primary care residents’ performance in brief alcohol intervention: a randomized controlled trial. J Gen Intern Med. 2007;22:1144–9. [DOI] [PMC free article] [PubMed]
- 33.Geller G, Levine DM, Mamon JA, Moore RD, Bone LR, Stokes EJ. Knowledge, attitudes, and reported practices of medical students and house staff regarding the diagnosis and treatment of alcoholism. JAMA. 1989;261:3115–20. [DOI] [PubMed]
- 34.Marcus MT, Brown RL, Straussner SL, et al. Creating change agents: a national substance abuse education project. Subst Abus. 2005;26:5–15. [DOI] [PubMed]
- 35.Madden TE, Graham AV, Straussner SL, et al. Interdisciplinary benefits in Project MAINSTREAM: a promising health professions educational model to address global substance abuse. J Interprof Care. 2006;20:655–64. [DOI] [PubMed]
- 36.Doughty RA, Williams PD, Seashore CN. Chief resident training. Developing leadership skills for future medical leaders. Am J Dis Child. 1991;145:639–42. [DOI] [PubMed]
- 37.Levine SA, Caruso LB, Vanderschmidt H, Silliman RA, Barry PP. Faculty development in geriatrics for clinician educators: a unique model for skills acquisition and academic achievement. J Am Geriatr Soc. 2005;53:516–21. [DOI] [PubMed]
- 38.Steel K. The medical chief residency in university hospitals. Ann Intern Med. 1972;76:541–4. [DOI] [PubMed]
- 39.Alpert JJ, Levenson SM, Osman CJ, James S. Does being a chief resident predict leadership in pediatric careers? Pediatrics. 2000;105:984–8. [PubMed]
- 40.Mygdal WK, Monteiro M, Hitchcock M, Featherston W, Conard S. Outcomes of the first family practice chief resident leadership conference. Fam Med. 1991;23:308–10. [PubMed]
- 41.Bigby J, Barnes HN. Evaluation of a faculty development program in substance abuse education. J Gen Intern Med. 1993;8:301–5. [DOI] [PubMed]
- 42.Rose AJ, Stein MR, Arnsten JH, Saitz R. Teaching internal medicine resident physicians about alcoholics anonymous: a pilot study of an educational intervention. Subst Abus. 2006;27:5–11. [DOI] [PMC free article] [PubMed]
- 43.D’Onofrio G, Nadel ES, Degutis LC, et al. Improving emergency medicine residents’ approach to patients with alcohol problems: a controlled educational trial. Ann Emerg Med. 2002;40:50–62. [DOI] [PubMed]
- 44.Nigwekar SU, Morse DS. Educational half day: an innovative way to incorporate substance abuse curriculum into residency training. Subst Abus. 2006;27:1–3. [DOI] [PubMed]
- 45.Institute of Medicine. Broadening the base of treatment for alcohol problems. Washington DC: The National Academies Press; 1990. [PubMed]
- 46.Renner JA Jr. How to train residents to identify and treat dual diagnosis patients. Biol Psychiatry. 2004;56:810–6. [DOI] [PubMed]
- 47.Levine S, Chao S, Brett B, et al. Chief resident immersion training in the care of older adults: an innovative inter-specialty education and leadership intervention. J Am Geriatr Soc. 2008;56:1140–5. [DOI] [PubMed]


