Abstract
Background and Objectives
There is growing international concern that food insecurity may negatively impact antiretroviral (ARV) treatment outcomes, but no studies have directly evaluated the effect of food insecurity on viral load suppression and antiretroviral adherence. We hypothesized that food insecurity would be associated with poor virologic response among homeless and marginally housed HIV-positive ARV-treated patients.
Design
This is a cross-sectional study.
Participants and Setting
Participants were ARV-treated homeless and marginally housed persons receiving adherence monitoring with unannounced pill counts in the Research on Access to Care in the Homeless (REACH) Cohort.
Measurements
Food insecurity was measured by the Household Food Insecurity Access Scale (HFIAS). The primary outcome was suppression of HIV viral RNA to <50 copies/ml. We used multivariate logistic regression to assess whether food insecurity was associated with viral suppression.
Results
Among 104 participants, 51% were food secure, 24% were mildly or moderately food insecure and 25% were severely food insecure. Severely food insecure participants were less likely to have adherence >=80%. In adjusted analyses, severe food insecurity was associated with a 77% lower odds of viral suppression (95% CI = 0.06–0.82) when controlling for all covariates. In analyses stratified by adherence level, severe food insecurity was associated with an 85% lower odds of viral suppression (95% CI = 0.02–0.99) among those with <=80% adherence and a 66% lower odds among those with >80% adherence (95% CI = 0.06–1.81).
Conclusions
Food insecurity is present in half of the HIV-positive urban poor in San Francisco, one of the best resourced settings for HIV-positive individuals in the United States, and is associated with incomplete viral suppression. These findings suggest that ensuring access to food should be an integral component of public health HIV programs serving impoverished populations.
KEY WORDS: HIV/AIDS, food insecurity, homeless, HIV viral load suppression, adherence, San Francisco
BACKGROUND AND OBJECTIVES
The urban poor are disproportionately affected by HIV.1 Well-described barriers to antiretroviral treatment access and adherence among HIV-infected urban poor include substance use, mental illness, social stigma, provider trust, medication side effects, lack of social support, low patient self-efficacy, forgetting, and homelessness.2–7 An under-studied potential barrier to HIV treatment access and adherence in the urban poor is food insecurity. Food insecurity is defined as having uncertain or limited availability of nutritionally adequate or safe food or the inability to procure food in socially acceptable ways,8 and is highly prevalent both among the urban poor,9,10 and among people living with HIV/AIDS.8 There is growing recognition internationally that food insecurity may negatively effect HIV disease progression and antiretroviral treatment efficacy, particularly in resource-limited settings, but empirical data on this issue are lacking.11–13
Food insecurity adversely affects health behavior, functional health status, and health outcomes for several diseases other than HIV.14–21 Food insecurity is associated with poor physical and mental health among both children and adults, including worse self-reported health status, and higher rates of obesity, depression, diabetes, and heart disease.14–19 Food insecurity has also been found to be associated with postponing needed medications and care, and increased emergency department use and hospitalizations in the U.S.20,21 Effects of food insecurity on health outcomes and utilization persist even after controlling for other measures of socioeconomic status.14,15,20 Food insecurity can affect health either directly or indirectly through the physiological impact of poor nutritional status,22 and also through other social and behavioral mechanisms that influence or force choices and behaviors.17
The impact of food insecurity on HIV treatment outcomes in North America is unknown. Several small studies from developing countries have found that people living with HIV/AIDS cite lack of food as a barrier to antiretroviral treatment adherence23–25, but no studies have quantitatively assessed whether food insecurity is independently associated with poor adherence. Food insecurity may also impact HIV treatment outcomes through biologic mechanisms. Among 119 HIV-infected drug users in Florida, food insecurity was associated with HIV wasting, which is associated with poor clinical outcomes and poor virologic responses.26–29 Food may also impact antiretroviral pharmacokinetics, leading to sub-optimal drug levels and virologic rebound.11,30–32
To gain a better understanding of possible impacts of food insecurity on HIV RNA suppression in a North American setting, we conducted a cross-sectional study among 104 homeless and marginally housed participants receiving antiretroviral therapy as part of the Research on Access to Care in the Homeless Cohort (REACH). We hypothesized that food insecurity would be associated with poor virologic response among patients on antiretroviral therapy and that this association would be modified by adherence.
DESIGN, PARTICIPANTS AND SETTING
Participants were from the REACH Cohort of HIV-infected homeless and marginally housed adults systematically recruited from San Francisco homeless shelters, free-meal programs, and single room-occupancy hotels charging less than $600/month.1,33 Structured questionnaires were administered to participants at baseline and at three-month intervals. Interviews included information on socio-demographics, alcohol and drug use, sexual behaviors, health services utilization, overall health status, use of antiretrovirals, and use of medications for opportunistic infections. Viral load and CD4 counts were assessed on a quarterly basis for all participants, and unannounced pill counts were conducted monthly for a subset of participants to assess for adherence. Participants signed a written consent form at the onset of the study and were reimbursed $15 per interview.
In the first quarter of 2006, the Household Food Insecurity Access Scale (HFIAS) was introduced at REACH for a one-time cross-sectional study. Participants were included if they were on three antiretrovirals and receiving adherence monitoring by unannounced pill counts during that quarter. The data presented here refer to the REACH quarterly interview and viral load measurement that occurred within 60 days after the administration of the HFIAS, and the three nearest adherence pill counts after administration of the HFIAS. The UCSF Human Subjects Committee approved all study procedures.
Primary Dependent Variable
The primary outcome was HIV viral suppression <50 copies/mL. Plasma was processed and stored at −40°C within 6 hours of collection. HIV-1 viral load determinations were made using the HIV-1 Amplicor Monitor Version 1.5 ultrasensitive assay (Roche Molecular Systems, Alameda, California, USA), with a lower limit of quantification of 10 copies/mL.
Art adherence
To determine the role of adherence in influencing the relationship between food insecurity and viral load suppression, adherence was controlled for in logistic regression analyses and was also examined as a possible effect modifier. Adherence was measured using unannounced pill counts as described elsewhere.34 We chose this measure because unannounced pill counts do not interfere with the benefits of pill box organizers35 and have been closely correlated with electronically monitored adherence (r = 0.91)36, concurrent viral load (r = 0.67)34, antiretroviral blood levels37, and progression to AIDS38. Pill counts were conducted in duplicate; if results did not match, a third pill count was done. Individuals were reimbursed $10 for each assessment. Pill count adherence was dichotomized as > 80% adherence versus <=80% adherence, reflecting the ability of more potent, currently recommended regimens to suppress HIV below the limit of detection at moderate levels of adherence.39,40
Primary Independent Variable
Food insecurity was measured by the Household Food Insecurity Access Scale (HFIAS), which was previously developed based on validation studies in eight countries including the United States.41–44 Validation studies have demonstrated that the HFIAS is able to distinguish food secure from insecure households across different cultural contexts. Questions represent universal domains of the household food insecurity experience and can be used to assign households and populations along a continuum of severity, from food secure to severely food insecure. The questions cover three domains of the experience of food insecurity: (1) anxiety and uncertainty about food supply, (2) insufficient quality (includes the variety and preferences of the type of food), and (3) insufficient food intake and its physical consequences. Scores range from 9 to 27; higher scores reflect more severe food insecurity.41 Since we postulated that the effects of food insecurity on viral suppression would be most notable for severely food insecure persons, food security was dichotomized as severely food insecure versus all other categories.
Covariates for the study included age (continuous), sex (male/female), race (white versus non-white), income (>= versus < population median), education (>= versus < high school diploma), employment (employed versus unemployed), recent homelessness (sleeping on the street or shelter in past 90 days), drug use over the past 30 days, injection drug use over the past 30 days, nadir CD4 count (continuous + 50 cells), problem drinking (greater than an average of 14 drinks/week for men and 7 drinks/week for women in accordance with the National Institute of Alcohol Abuse and Alcoholism’s definition for risky drinking), and incarceration over the previous 30 days. Depression was assessed by the BDI version II (continuous variable), which has proven to be a reliable and valid measurement of depression in different populations including homeless populations.45–48 We also controlled for current regimen type (fully suppressive regimen including ritonavir-boosted PI regimens and NNRTI regimens versus non-fully suppressive regimen including non-boosted PI regimens and triple NRTI regimens), prior months on any HAART before study entry, and mono/dual NRTI exposure prior to HAART.
Analysis
We used multivariable logistic regression to determine factors associated with viral load suppression. Data were analyzed using SAS software (SAS Institute, Cary, North Carolina, Version 8). We tested the association between food insecurity and viral suppression with and without adherence (>80% adherence versus <=80% adherence) to determine whether adherence influenced the relationship between food insecurity and viral suppression. To assess whether adherence was a possible effect modifier, additional post-hoc models were run stratified by adherence (>80% versus <=80%). To assess other possible mechanisms for the relationship between food insecurity and viral suppression, separate models were run stratified by regimen type, and also by high (>200) versus low (<=200) CD4 to assess the possibility that the relationship between food insecurity and viral suppression was confounded by disease stage. Regression diagnostic procedures yielded no evidence of multi-collinearity or overly influential outliers in any model.
RESULTS
Participant Characteristics
REACH had 294 participants in early 2006; 173 were on ART and of these 104 were receiving adherence monitoring with unannounced pill counts and were included in the study. The mean age was 46.5 (SD 9), 33% of participants were white, 64% were male, and 66% completed high school (Table 1). Fifty-three participants were food secure (51%), 26 were severely food insecure (25%), and the remainder (24%) were either mildly or moderately food insecure. Seventy-three percent had ever received food aid, and of those, 86% had food aid in the previous 30 days. Seventeen participants were on NNRTI-based regimens, and 73 were on ritonavir-boosted PI regimens for a total of 90 participants (87%) on fully suppressive regimens. The remaining participants were either on single-PI ( = 13) or triple NRTI regimen ( = 1). Fifty-six percent had >80% adherence as assessed by pill counts, and 56% had undetectable viral loads.
Table 1.
Participant Characteristics †
| Characteristic | All participants = 104 | Food security categories 1,2,3‡ = 78 (75.0%) | Food security category 4 (severely food insecure) = 26 (25.0%) |
|---|---|---|---|
| Age (mean, SD) | 46.5 (7.9) | 46.8 (8.0) | 45.9 (7.6) |
| Non-white (versus white) | 70 (67%) | 53 (68%) | 17 (65%) |
| Male | 66 (64%) | 51 (65%) | 15 (58%) |
| <High school education | 35 (34%) | 25 (32%) | 10 (38%) |
| Employed | 7(7%) | 4 (5%) | 3 (12%) |
| Income (>=median of 878$/month) | 52 (50%) | 37 (47%) | 15 (58%) |
| Recent incarceration | 4 (4%) | 3 (4%) | 1 (4%) |
| Recent homelessness | 3 (3%) | 2 (3%) | 1 (4%) |
| Fully suppressive regimen | 90 (87%) | 67 (86%) | 23 (88%) |
| History of drug use past 30 days | 35 (34%) | 21 (27%)** | 14 (54%)** |
| History of injection drug use past 30 days | 19 (18%) | 12 (15%) | 7 (27%) |
| Problem drinking | 6 (6%) | 4 (5%) | 2 (8%) |
| BDI score (mean, SD) | 11.7 (10.1) | 10.1 (9.2)** | 16.6 (11.3)** |
| Mono or dual NRTI* use prior to HAART** | 92 (89%) | 69 (88%) | 23 (88%) |
| Months on HAART** prior to study (mean, SD) | 41.6 (32) | 40.9 (31.3) | 43.4 (33.1) |
| Nadir CD4 (mean, SD) | 228 (202) | 229 (197) | 223 (220) |
| Pill count adherence >80% | 58 (56%) | 48 (62%)* | 10 (38%)* |
| VL <50 copies/ml | 58 (56%) | 49 (63%)** | 9 (35%)** |
† P values compare severely food insecure versus all other participants for each characteristic. * p <= .05; ** p <= .01;
‡ Food security categories 1, 2 and 3 include food secure, and mildly or moderately food insecure
#Fully suppressive regimen is defined as taking ritonavir boosted PI or NNRTI-based regimen
* Non-nucleoside reverse transcriptase inhibitor
** Highly active antiretroviral therapy
Comparing participant characteristics by food security status, participants who were severely food insecure were more likely to have <=80% adherence, to have detectable HIV RNA, to be depressed, and to report drug use over the past 30 days (Table 1). Examining the distribution of food security status by adherence quintile, participants who were severely food insecure comprised a lower proportion of those with >=80% adherence, and a higher proportion of those with adherence between 20–39%, 40–59%, and 60–79% (Fig. 1).
Figure 1.
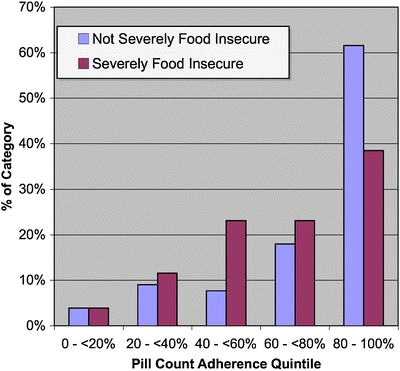
Adherence quintile by food security status.
Correlates of HIV Viral Suppression
In unadjusted analyses (Table 2), the odds of viral suppression was 70% lower among participants who were severely food insecure compared to those who were not severely food insecure (odds ratio (OR) = 0.31, 95% confidence interval [CI] 0.12–0.79). Participants who had >80% adherence and those with higher nadir CD4s also had higher odds of VL suppression. In adjusted analyses without adherence (Table 2 Column 2), severe food insecurity was associated with 79% lower odds of viral suppression (adjusted odds ratio (AOR) = 0.21, 95% CI = 0.06–0.72) when controlling for all other covariates. Nadir CD4 remained associated with viral suppression (AOR = 1.26 per 50 cells, 95% CI = 1.06–1.51). Being on HAART for a longer time prior to study entry was also associated with higher odds of viral suppression (AOR = 1.07 per each three months on HAART, 95% CI = 1.01–1.14), and having received mono or dual NRTI regimens prior to initiating HAART was associated with lower odds of viral suppression (AOR = 0.13, 95% CI = 0.02–0.92).
Table 2.
Factors Associated with Viral Suppression <50 copies/ml among Homeless and Marginally Housed HIV-Infected Participants in San Francisco ( = 104)
| Characteristic | Odds ratio (OR) (0.95CI) | Adjusted OR without adherence (0.95CI) | Adjusted OR with adherence (0.95CI) |
|---|---|---|---|
| Severely food insecure (HFIAS category 4 vs. categories 1, 2, 3) | 0.31 (0.12–0.79) | 0.21 (0.06–0.72) | 0.23 (0.06–0.82) |
| Age (per year) | 1.03 (0.98–1.08) | 1.02 (0.95–1.09) | 1.03 (0.96–1.10) |
| Non-white (vs. white) | 0.69 (0.30–1.60) | 0.44 (0.15–1.30) | 0.61 (0.19–2.00) |
| Male (vs. Female) | 0.87 (0.39–1.95) | 1.50 (0.46–4.85) | 1.58 (0.44–5.61) |
| >= High school education | 0.77 (0.34–1.74) | 1.11 (0.35–3.52) | 0.90 (0.27–3.01) |
| Employed | 0.57 (0.12–2.70) | 0.69 (0.09–5.38) | 0.58 (0.06–6.10) |
| Income >= mean | 0.73 (0.34–1.59) | 0.82 (0.30–2.27) | 0.82 (0.28–2.38) |
| Recent incarceration | 0.25 (0.03–2.50) | 0.55 (0.04–7.89) | 0.68 (0.04–12.48) |
| Fully suppressive regimen | 0.66 (0.21–2.14) | 1.24 (0.27–5.65) | 1.35 (0.28–6.59) |
| Drug use past 30 days | 0.45 (0.20–1.04) | 0.47 (0.11–2.05) | 0.69 (0.14–3.33) |
| Injection drug use past 30 days | 0.66 (0.24–1.79) | 1.25 (0.21–7.35) | 2.34 (0.34–16.06) |
| Problem Drinking | 0.14 (0.02–1.28) | 0.21 (0.02–2.52) | 0.25 (0.02–3.96) |
| BDI score (per unit) | 1.00 (0.96–1.04) | 1.04 (0.99–1.10) | 1.06 (0.995–1.12) |
| Mono or dual NRTI* use prior to HAART** | 0.38 (0.01–1.49) | 0.13 (0.02–0.92) | 0.21 (0.03–1.67) |
| Months on HAART** prior to study (per 3 months) | 1.04 (0.99–1.08) | 1.07 (1.01–1.14) | 1.08 (1.01–1.15) |
| Nadir CD4 (per 50 cells) | 1.17 (1.04–1.32) | 1.26 (1.06–1.51) | 1.27 (1.05–1.53) |
| Adherence >80% | 5.92 (2.53–13.89) | – | 5.94 (1.81–19.51) |
* Non-nucleoside reverse transcriptase inhibitor
** Highly active antiretroviral therapy
In separate models including the same variables, but also adjusting for adherence >80% (Table 2, column 3), the association between food insecurity and viral load suppression remained unchanged (AOR = 0.23, 95% CI-0.06–0.82). Higher adherence was associated with 5.9 times the odds of viral suppression (95% CI = 1.81–19.5), and previous NRTI use was no longer significantly associated with HIV viral suppression. There were no other appreciable changes in associations with HIV viral suppression. In separate models, controlling for adherence as a continuous variable (not shown), associations between food insecurity and HIV viral suppression were similar (AOR = 0.28, 95% CI 0.09–0.87).
Correlates of HIV Viral Suppression Stratified by Adherence Status
Among individuals with <=80% adherence, severe food insecurity was associated with 85% lower odds of viral suppression (AOR = 0.15, 95% CI = 0.02–0.99, see Table 3). On the other hand, among individuals with >80% adherence, food insecurity was associated with a 66% lower odds of viral suppression and the association was not statistically significant (AOR = 0.34, 95% CI = 0.06–1.81). Among individuals with lower adherence, higher nadir CD4 significantly increased odds of viral suppression, but this association was not seen for those with >80% adherence. Finally, in stratified models, months on HAART was only significantly associated with higher odds of viral suppression for individuals with higher adherence.
Table 3.
Adjusted Factors Associated with Viral Suppression <50 copies/ml Stratified by Adherence Level* ( = 104)
| Characteristic | Adherence > 80% = 58 | Adherence <=80% = 46 |
|---|---|---|
| Adjusted OR (0.95CI) | Adjusted OR (0.95CI) | |
| Severely food insecure (HFIAS category 4 vs. categories 1, 2, 3) | 0.34 (0.06–1.81) | 0.15 (0.02–0.99) |
| Drug use past 30 days | 0.29 (0.05–1.76) | 2.37 (0.48–11.65) |
| Mono or dual NRTI** use prior to HAART*** | 0.22 (0.03–1.52) | 0.10 (0.003–3.92) |
| Months on HAART*** prior to study (per 3 months) | 1.05 (1.01–1.08) | 1.04 (0.96–1.13) |
| Nadir CD4 (per 50 cells) | 1.05 (0.86–1.28) | 1.38 (1.05–1.80) |
*The multivariate regression model was derived including all variables with a value <=0.2
** Non-nucleoside reverse transcriptase inhibitor
*** Highly active antiretroviral therapy
Impact of Regimen Type and CD4 Cell Counts
To explore mechanisms other than adherence for how food insecurity could be associated with viral suppression, we also looked at associations between food insecurity and viral RNA suppression stratified by regimen type. For participants on PI-based regimens ( = 86), the association between severe food insecurity and viral suppression when controlling for adherence was similar as that in the entire sample, with an odds ratio of 0.29 (95% CI = 0.09–0.93). Because nelfinavir drug levels are particularly increased by concurrent food intake, we examined associations to see if they were significant without nelfinavir-treated patients. When we excluded the few patients receiving nelfinavir ( = 6), associations between food insecurity and viral load suppression did not change appreciably. On the other hand, for the minority of participants on NNRTI based regimens ( = 17), we were insufficiently powered to detect such associations. Finally, in separate models stratified by low (<200) versus high (>=200) CD4 cell counts, we found that associations between food insecurity and incomplete HIV RNA suppression were similar in both groups.
DISCUSSION
We found that half of urban poor HIV-infected individuals in a particularly well-resourced North American setting were food insecure, and that food insecurity independently increases the risk of incomplete viral suppression. The prevalence of food insecurity in this study is consistent with Normén’s estimate that 48% of individuals on antiretrovirals in a drug-treatment program in Vancouver are food insecure.8 The consistency in two well-resourced settings with well-established public health delivery systems suggests that food insecurity may be a significant problem in other North American settings as well. We also found that severe food insecurity was associated with nearly 80% lower odds of viral suppression when controlling for other covariates. This suggests that ensuring consistent access to food may be an important and neglected intervention to improve antiretroviral treatment effectiveness. These findings support recommendations by the World Health Organization, UNAIDS, the World Food Program, and other international organizations that interventions addressing food insecurity should be integrated with HIV/AIDS programming activities where possible.11–13 While there is a growing international concern that food insecurity may compromise treatment effectiveness in emerging antiretroviral treatment programs in developing countries, our findings suggest that food insecurity may compromise treatment efficacy even in well-resourced settings. The finding that food insecurity is independently associated with viral suppression adds to the body of literature suggesting that non-medical services, such as access to food, adequate housing49 and case management,50 impact upon HIV clinical outcomes and should be considered as part of comprehensive HIV care packages.
Adherence modified the association between food insecurity and HIV RNA suppression; for individuals who were less adherent, severe food insecurity was associated with an 85% reduction in the odds of viral suppression. For individuals with >80% adherence, there was still a 66% reduction in the odds of viral suppression for individuals who were severely food insecure, but this association was no longer significant. Given the small sample, we can not exclude an association for more adherent individuals. These findings, however, suggest that food security interventions may exert the largest impacts in terms of treatment efficacy on food insecure individuals with low levels of adherence.
Food insecurity was associated with non-adherence in a non-linear fashion. People with severe food insecurity were more likely to have 20–80% adherence than those who were not severely food insecure. The finding that food insecurity is associated with lower levels of adherence is especially important given that these lower ranges of adherence (<80%) are more likely to be associated with incomplete viral suppression with currently used regimens.39,40
Our data suggest that the association between food insecurity and viral suppression is not explained by difference in average monthly adherence. Unannounced pill count adherence is one of the best available adherence measurement strategies, yet it does not pick up patterns of adherence including treatment interruptions, which are associated with viral rebound within defined strata of average adherence.51 Food insecurity may also impact viral suppression through biologic mechanisms. While not explicitly examined in this study, once such mechanism is that food may impact the pharmacokinetics of antiretroviral medications. The association between food insecurity and viral suppression was strong for individuals using PI-based regimens. Several protease inhibitors such as nelfinavir and ritonavir require food for maximal absorption, and the absence of food may negatively affect the pharmacokinetics of these drugs.31,32,52 Given that only a minority of participants in this study were receiving NNRTIs, larger studies with more patients on NNRTIs will help determine whether regimen type modifies the association between food insecurity and HIV RNA suppression. Nutritional status is another putative mechanism for how food insecurity may be associated with incomplete viral suppression and poor clinical outcomes. Malnutrition is a potential consequence of food insecurity,53 and studies have shown that low body mass index (BMI) and weight loss are associated with both higher HIV RNA levels and mortality for individuals on HAART.26,54,55 As we did not assess BMI or other nutritional parameters in this population, we cannot infer the extent to which poor nutritional status or HIV wasting may have contributed to the association between food insecurity and viral suppression.
There were several important limitations to this study. The cross-sectional design does not demonstrate causality. One possible interpretation of our findings is that individuals who were sicker as a result of poor virologic response subsequently had difficulties procuring food. Yet, we found that the impact of food insecurity on VL suppression was similar among people with higher CD4 counts making this possibility less likely. We could not determine the role of malnutrition on mediating relationships between food insecurity and VL suppression. In addition, socioeconomic status is a complex and multidimensional construct and may not be completely represented by income, education, employment and housing status. Finally, because of the small sample, cross-sectional design and the fact that we measured average adherence rather than patterns of adherence, including treatment interruptions, we were unable to determine whether adherence was on the causal pathway between food insecurity and viral load suppression. Longitudinal or intervention studies using larger sample sizes with detailed measures of patterns of adherence are, therefore, needed to better understand the relationships between food insecurity, antiretroviral adherence and HIV RNA suppression.
In summary, food insecurity was associated with incomplete viral suppression in the urban poor of San Francisco, one of the best-resourced settings for HIV-positive individuals in the world. The impact of food insecurity on viral suppression may be due to the combined effect of behavioral (adherence) and biologic (pharmacokinetics) mechanisms that lead to suboptimal drug levels required for viral suppression. These findings suggest that addressing fundamental human needs, such as access to food, should be an integral component of HIV programs serving impoverished populations in the United States.
Acknowledgements
This study was funded by NIMH 54907 and was also supported by NIH/NCRR UCSF-CTSI grant number UL1 RR024131. Dr Weiser received additional funding from NIMH 79713-01. Dr. Bangsberg received additional funding from NIAAA 015287. HIV RNA kits were donated by Roche. The authors wish to thank Richard Clark, Steven Deeks, and REACH study participants who shared their experiences. Results of this study were presented at the 15th Conference of Retrovirus and Opportunistic Infections in February, 2008.
Conflict of Interest Statement None disclosed.
Funding sources This study was funded by NIMH 54907 and was conducted at the UCSF Clinical and Translational Science Initiative Tenderloin Clinical Research Center, NIH U54 RR023566-01. Dr. Weiser received additional funding from NIMH 79713-01. Dr. Bangsberg received additional funding from NIAAA 015287. HIV RNA kits were donated by Roche.
Footnotes
The Positive Health Program and Center for AIDS Prevention Studies are programs of the UCSF AIDS Research Institute.
Sheri Weiser, Edward Frongillo, Elise Riley and David Bangsberg contributed substantially to conception and design of the research study. Sheri Weiser participated in acquisition of data. Sheri Weiser, Edward Frongillo, Kathleen Ragland, Elise Riley, Robert Hogg and David Bangsberg participated in data analysis and interpretation. Sheri Weiser, Edward Frongillo, Kathleen Ragland, Elise Riley, Robert Hogg and David Bangsberg participated in drafting and editing of the manuscript. All authors approved the final version of the manuscript.
REFERENCES
- 1.Robertson MJ, Clark RA, Charlebois ED, et al. HIV seroprevalence among homeless and marginally housed adults in San Francisco. Am J Public Health. 2004;94(7):1207–17. Jul. [DOI] [PMC free article] [PubMed]
- 2.Moss AR, Hahn JA, Perry S, et al. Adherence to highly active antiretroviral therapy in the homeless population in San Francisco: a prospective study. Clin Infect Dis. 2004;39(8):1190–8. Oct 15. [DOI] [PubMed]
- 3.Mills EJ, Nachega JB, Buchan I, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. Jama. 2006;296(6):679–90. Aug 9. [DOI] [PubMed]
- 4.Ammassari A, Trotta MP, Murri R, et al. Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S123–7. Dec 15. [DOI] [PubMed]
- 5.Altice FL, Mostashari F, Friedland GH. Trust and the acceptance of and adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;28(1):47–58. Sep 1. [DOI] [PubMed]
- 6.Lucas GM, Cheever LW, Chaisson RE, Moore RD. Detrimental effects of continued illicit drug use on the treatment of HIV-1 infection. J Acquir Immune Defic Syndr. 2001;27(3):251–9. Jul 1. [DOI] [PubMed]
- 7.Mills EJ, Nachega JB, Bangsberg DR, et al. Adherence to HAART: a systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Med. 2006;311e438. Nov. [DOI] [PMC free article] [PubMed]
- 8.Normen L, Chan K, Braitstein P, et al. Food insecurity and hunger are prevalent among HIV-positive individuals in British Columbia, Canada. J Nutr. 2005;135(4):820–5. Apr. [DOI] [PubMed]
- 9.Dachner N, Tarasuk V. Homeless “squeegee kids”: food insecurity and daily survival. Soc Sci Med. 2002;54(7):1039–49. Apr. [DOI] [PubMed]
- 10.Furness BW, Simon PA, Wold CM, Asarian-Anderson J. Prevalence and predictors of food insecurity among low-income households in Los Angeles County. Public Health Nutr. 2004;7(6):791–4. Sep. [DOI] [PubMed]
- 11.Seume-Fosso E, Rajabiun S, Cogill B, Elder L, Castleman T, Sheckler A. Food and Nutrition Technical Assistance. HIV/AIDS: A Guide For Nutritional Care and Support. Washington, DC October 2004. http://www.fantaproject.org/publications/HIVguide.shtml. Accessed September 23, 2008.
- 12.World Health Organization. Nutrient Requirements for People Living with HIV/AIDS: Report of a Technical Consultation. Geneva, Switzerland 13–15 May 2003. http://www.who.int/nutrition/publications/Content_nutrient_requirements.pdf. Accessed September 23, 2008.
- 13.Programming in the Era of AIDS: WPF’s Response to HIV/AIDS. Rome, Italy: World Food Programme; February 5–7 2003. http://reliefweb.int/rw/lib.nsf/db900sid/PANA-7DSFKW/$file/wfp_jan2003.pdf?openelement. Accessed September 23, 2008.
- 14.Siefert K, Heflin CM, Corcoran ME, Williams DR. Food insufficiency and physical and mental health in a longitudinal survey of welfare recipients. J Health Soc Behav. 2004;45(2):171–86. Jun. [DOI] [PubMed]
- 15.Heflin CM, Siefert K, Williams DR. Food insufficiency and women’s mental health: findings from a 3-year panel of welfare recipients. Soc Sci Med. 2005;61(9):1971–82. Nov. [DOI] [PubMed]
- 16.Che J, Chen J. Food insecurity in Canadian households. Health Rep. 2001;12(4):11–22. Aug. [PubMed]
- 17.Alaimo K, Olson CM, Frongillo EA. Family food insufficiency, but not low family income, is positively associated with dysthymia and suicide symptoms in adolescents. J Nutr. 2002;132(4):719–25. Apr. [DOI] [PubMed]
- 18.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007;22(7):1018–23. Jul. [DOI] [PMC free article] [PubMed]
- 19.Vozoris NT, Tarasuk VS. Household food insufficiency is associated with poorer health. J Nutr. 2003;133(1):120–6. Jan. [DOI] [PubMed]
- 20.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–7. Jan. [DOI] [PMC free article] [PubMed]
- 21.Kersey MA, Beran MS, McGovern PG, Biros MH, Lurie N. The prevalence and effects of hunger in an emergency department patient population. Acad Emerg Med. 1999;6(11):1109–14. Nov. [DOI] [PubMed]
- 22.Campbell CC. Food insecurity: a nutritional outcome or a predictor variable? J Nutr. 1991;121(3):408–15. Mar. [DOI] [PubMed]
- 23.Weiser S, Wolfe W, Bangsberg D, et al. Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. J Acquir Immune Defic Syndr. 2003;34(3):281–8. Nov 1. [DOI] [PubMed]
- 24.Au JT, Kayitenkore K, Shutes E, et al. Access to adequate nutrition is a major potential obstacle to antiretroviral adherence among HIV-infected individuals in Rwanda. Aids. 2006;20(16):2116–8. Oct 24. [DOI] [PubMed]
- 25.Hardon AP, Akurut D, Comoro C, et al. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care. 2007;19(5):658–65. May. [DOI] [PubMed]
- 26.Campa A, Yang Z, Lai S, et al. HIV-related wasting in HIV-infected drug users in the era of highly active antiretroviral therapy. Clin Infect Dis. 2005;41(8):1179–85. Oct 15. [DOI] [PubMed]
- 27.Kotler DP, Tierney AR, Wang J, Pierson RN Jr. Magnitude of body-cell-mass depletion and the timing of death from wasting in AIDS. Am J Clin Nutr. 1989;50(3):444–7. Sep. [DOI] [PubMed]
- 28.Melchior JC, Niyongabo T, Henzel D, Durack-Bown I, Henri SC, Boulier A. Malnutrition and wasting, immunodepression, and chronic inflammation as independent predictors of survival in HIV-infected patients. Nutrition. 1999;15(11–12):865–9. Nov–Dec. [DOI] [PubMed]
- 29.van der Sande MA, van der Loeff MF, Aveika AA, et al. Body mass index at time of HIV diagnosis: a strong and independent predictor of survival. J Acquir Immune Defic Syndr. 2004;37(2):1288–94. Oct 1. [DOI] [PubMed]
- 30.Castleman T, Seumo-Fosso E, Cogill B. Food and Nutrition Implications of Antiretroviral Therapy in Resource Limited Settings. Washington, DC: Food and Nutrition Technical Assistance Project. Academy for Educational Development; May 2004. http://www.fantaproject.org/downloads/pdfs/tn7_ARVs.pdf. Accessed September 23, 2008.
- 31.Gustavson L, Lam W, Bertz R, et al. Assessment of the bioequivalence and food effects for liquid and soft gelatin capsule co-formulations of ABT-378/ritonavir (ABT-378/r) in healthy subjects. Paper presented at: 40th Interscience Conference on Antimicrobial Agents and Chemotherapy, 2000; Toronto, Canada.
- 32.Bardsley-Elliot A, Plosker GL. Nelfinavir: an update on its use in HIV infection. Drugs. 2000;59(3):581–620. Mar. [DOI] [PubMed]
- 33.Zolopa AR, Hahn JA, Gorter R, et al. HIV and tuberculosis infection in San Francisco’s homeless adults. Prevalence and risk factors in a representative sample. Jama. 1994;272(6):455–61. Aug 10. [DOI] [PubMed]
- 34.Bangsberg DR, Hecht FM, Charlebois ED, et al. Adherence to protease inhibitors, HIV-1 viral load, and development of drug resistance in an indigent population. Aids. 2000;14(4):357–66. Mar 10. [DOI] [PubMed]
- 35.Petersen ML, Wang Y, van der Laan MJ, Guzman D, Riley E, Bangsberg DR. Pillbox organizers are associated with improved adherence to HIV antiretroviral therapy and viral suppression: a marginal structural model analysis. Clin Infect Dis. 2007;45(7):908–15. Oct 1. [DOI] [PMC free article] [PubMed]
- 36.Bangsberg DR, Bronstone A, Hofmann R. A computer-based assessment detects regimen misunderstandings and nonadherence for patients on HIV antiretroviral therapy. AIDS Care. 2002;14(1):3–15. Feb. [DOI] [PubMed]
- 37.Descamps D, Flandre P, Calvez V, et al. Mechanisms of virologic failure in previously untreated HIV-infected patients from a trial of induction-maintenance therapy. Trilege (Agence Nationale de Recherches sur le SIDA 072) Study Team). Jama. 2000;283(2):205–11. Jan 12. [DOI] [PubMed]
- 38.Bangsberg DR, Perry S, Charlebois ED, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. Aids. 2001;15(9):1181–3. Jun 15. [DOI] [PubMed]
- 39.Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clin Infect Dis. 2006;43(7):939–41. Oct 1. [DOI] [PubMed]
- 40.Shuter J, Sarlo JA, Kanmaz TJ, Rode RA, Zingman BS. HIV-infected patients receiving lopinavir/ritonavir-based antiretroviral therapy achieve high rates of virologic suppression despite adherence rates less than 95%. J Acquir Immune Defic Syndr. 2007;45(1):4–8. May 1. [DOI] [PubMed]
- 41.Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide. Version 3. Washington, D.C.: Food and Nutrition Technical Assistance. Academy for Educational Development; August 2007. http://www.foodsec.org/tr/nut/hfias.pdf. Accessed September 23, 2008.
- 42.Swindale A, Bilinsky P. Development of a universally applicable household food insecurity measurement tool: process, current status, and outstanding issues. J Nutr. 2006;136(5):1449S–52S2. May. [DOI] [PubMed]
- 43.Frongillo EA, Nanama S. Development and validation of an experience-based measure of household food insecurity within and across seasons in Northern Burkina Faso. J Nutr. 2006;136(5):1409S–19S. May. [DOI] [PubMed]
- 44.Coates J, Frongillo EA, Rogers BL, Webb P, Wilde PE, Houser R. Commonalities in the experience of household food insecurity across cultures: what are measures missing? J Nutr. 2006;136(5):1438S–48S. May. [DOI] [PubMed]
- 45.Beck A, Steer R, Garbin M. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [DOI]
- 46.Riley ED, Bangsberg DR, Perry S, Clark RA, Moss AR, Wu AW. Reliability and validity of the SF-36 in HIV-infected homeless and marginally housed individuals. Qual Life Res. 2003;12(8):1051–8. Dec. [DOI] [PubMed]
- 47.Storch EA, Roberti JW, Roth DA. Factor structure, concurrent validity, and internal consistency of the Beck Depression Inventory-Second Edition in a sample of college students. Depress Anxiety. 2004;19(3):187–9. [DOI] [PubMed]
- 48.Weiser SD, Riley ED, Ragland K, Hammer G, Clark R, Bangsberg DR. Brief report: factors associated with depression among homeless and marginally housed HIV-infected men in San Francisco. J Gen Intern Med. 2006;21(1):61–4. Jan. [DOI] [PMC free article] [PubMed]
- 49.Kidder DP, Wolitski RJ, Campsmith ML, Nakamura GV. Health status, health care use, medication use, and medication adherence among homeless and housed people living with HIV/AIDS. Am J Public Health. 2007;97(12):2238–45. Dec. [DOI] [PMC free article] [PubMed]
- 50.Kushel MB, Colfax G, Ragland K, Heineman A, Palacio H, Bangsberg DR. Case management is associated with improved antiretroviral adherence and CD4 + cell counts in homeless and marginally housed individuals with HIV infection. Clin Infect Dis. 2006;43(2):234–42. Jul 15. [DOI] [PubMed]
- 51.Parienti JJ, Das-Douglas M, Massari V, et al. Not all missed doses are the same: sustained NNRTI treatment interruptions predict HIV rebound at low-to-moderate adherence levels. PLoS ONE. 2008;37e2783. [DOI] [PMC free article] [PubMed]
- 52.Abbot Laboratories. Kaletra, US package insert. Available at: http://www.fda.gov/cder/foi/label/2005/021226s016lbl.pdf Accessed November 14, 2007.
- 53.Gillespie S, Kadiyala S. HIV/AIDS and Food and Nutrition Security: From Evidence to Action. Washington, DC: International Food Policy Reseach Institute; 2005.
- 54.Batterham MJ, Garsia R, Greenop P. Prevalence and predictors of HIV-associated weight loss in the era of highly active antiretroviral therapy. Int J STD AIDS. 2002;13(11):744–7. Nov. [DOI] [PubMed]
- 55.Tang AM, Forrester J, Spiegelman D, Knox TA, Tchetgen E, Gorbach SL. Weight loss and survival in HIV-positive patients in the era of highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;31(2):230–6. Oct 1. [DOI] [PubMed]


