Abstract
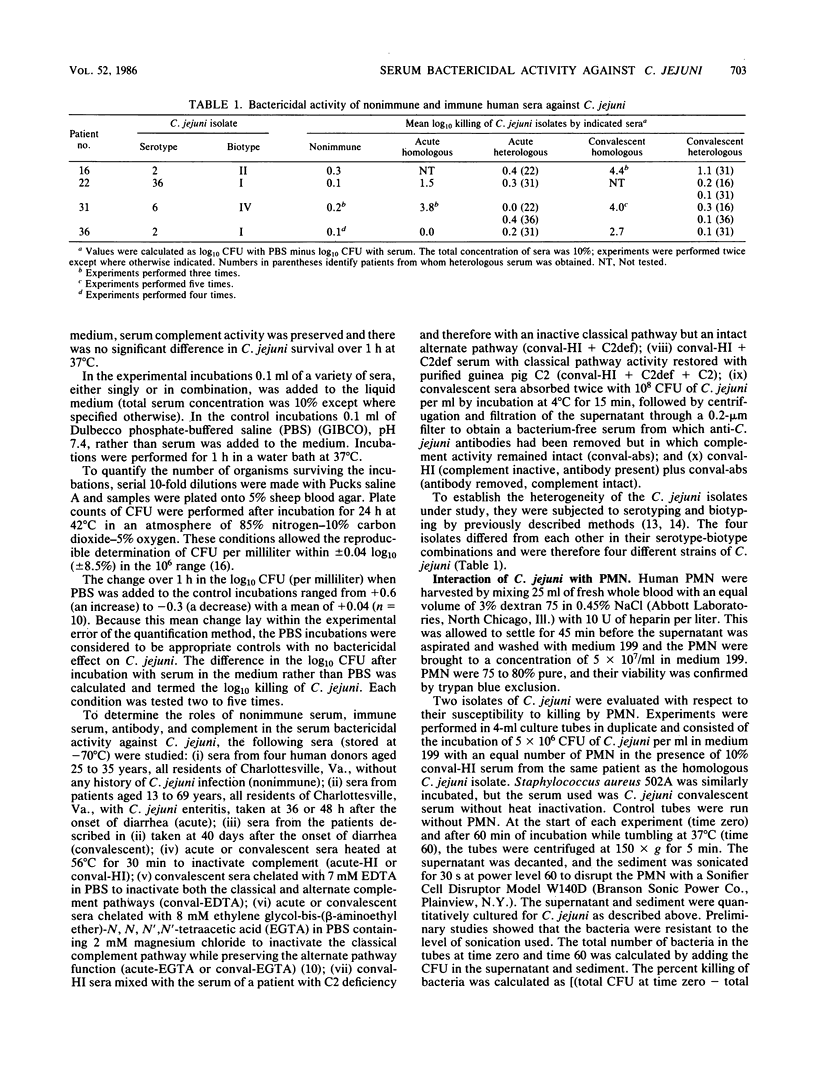
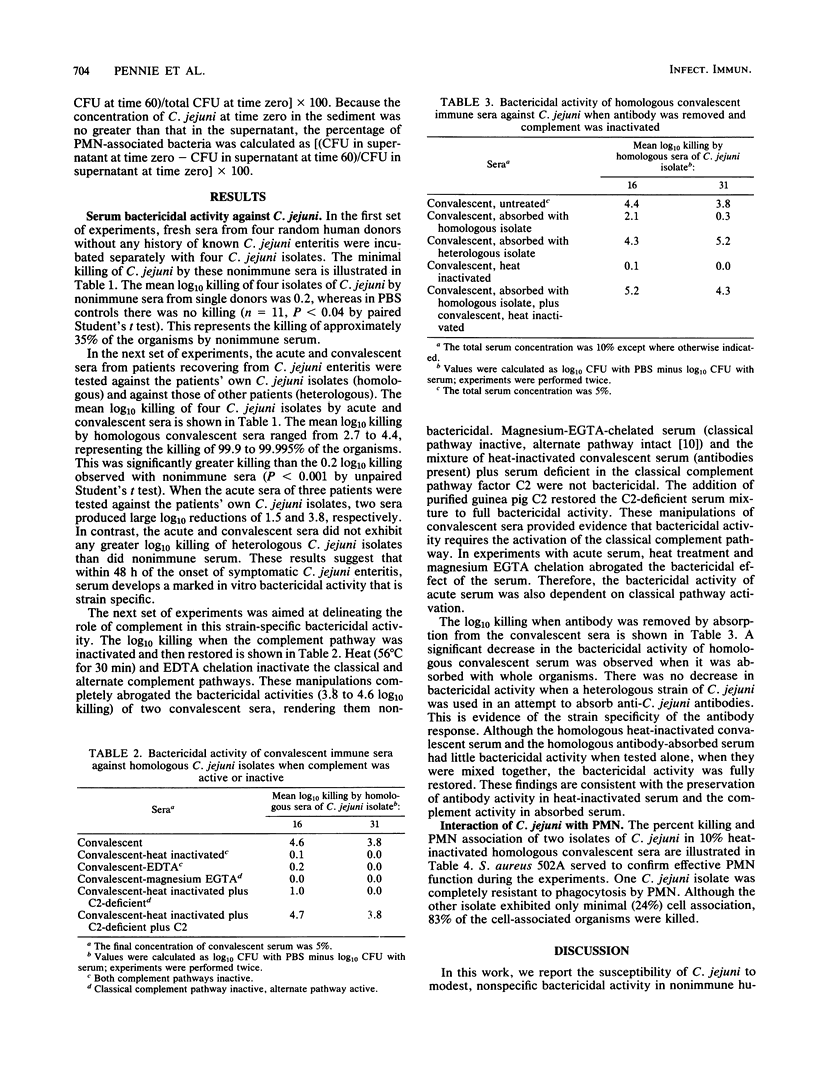
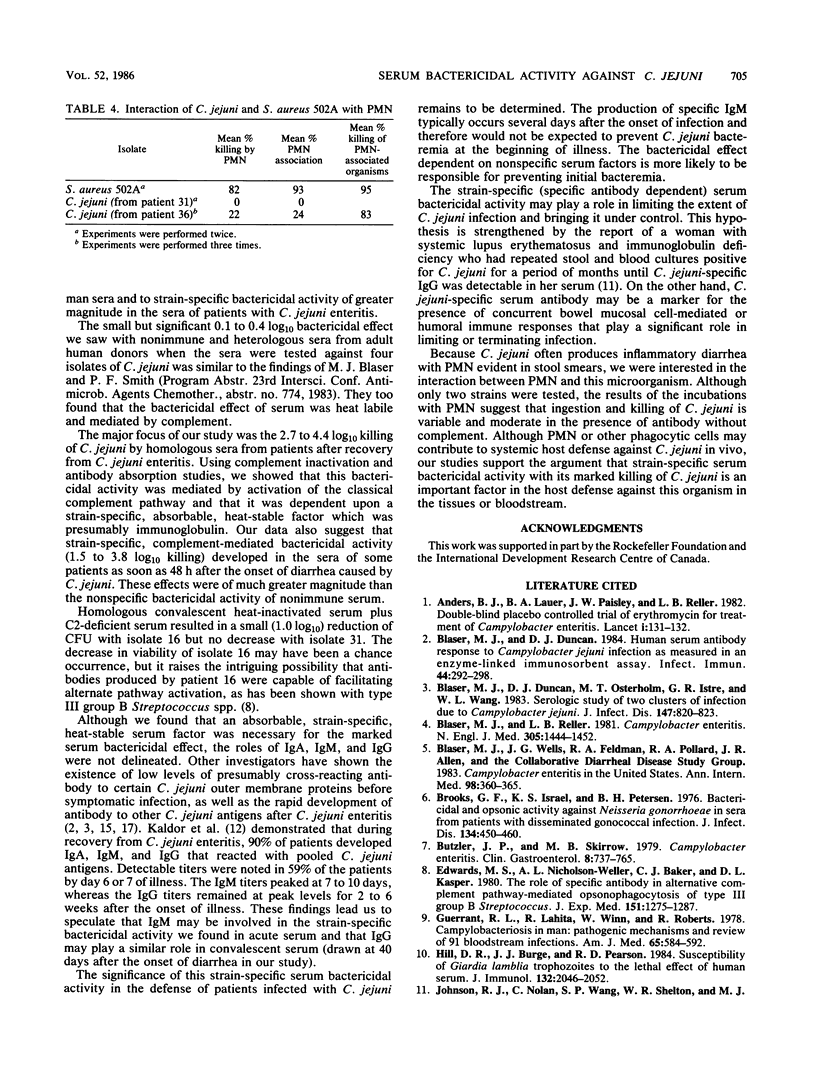
Campylobacter jejuni is a common cause of inflammatory enteritis, which in normal hosts is usually self-limited and resolves without antibiotic therapy. C. jejuni bacteremia is very rare. We examined sera for bactericidal activity that might be important in limiting the extent of C. jejuni infection in man. We studied the ability of nonimmune sera and homologous and heterologous immune sera from infected patients to kill different fresh case isolates of C. jejuni in vitro. The reduction of the log10 concentration of viable C. jejuni (log10 killing) by fresh sera from nonimmune donors was only 0.2. Log10 killing by homologous acute sera varied from 0 to 3.8 (mean, 1.8). Convalescent sera showed remarkable log10 killing of only homologous C. jejuni, with values of 2.7 to 4.4 (mean, 3.7). The bactericidal effects of acute and convalescent sera were abrogated by heat and EDTA chelation, indicating mediation by complement. The role of classical complement pathway activation was supported by chelating sera with magnesium EGTA [ethylene glycol-bis(beta-aminoethyl ether)-N, N, N', N'-tetraacetic acid] and by reconstitution experiments with heat-inactivated sera, C2-deficient serum, and purified C2. The requirement of specific antibody for the serum bactericidal effect was indicated by the loss of bactericidal activity when immune sera were absorbed with homologous but not heterologous whole C. jejuni isolates. The presence of specific antibodies was further documented by agglutination of only homologous C. jejuni suspensions by heat-inactivated immune sera. Studies with polymorphonuclear leukocytes suggested that ingestion and killing of two C. jejuni strains were modest and variable in the presence of heat-inactivated homologous serum. In summary, the data document a potent serum bactericidal effect that develops rapidly and specifically during C. jejuni enteritis and may be an important factor in host defense against C. jejuni.
Full text
PDF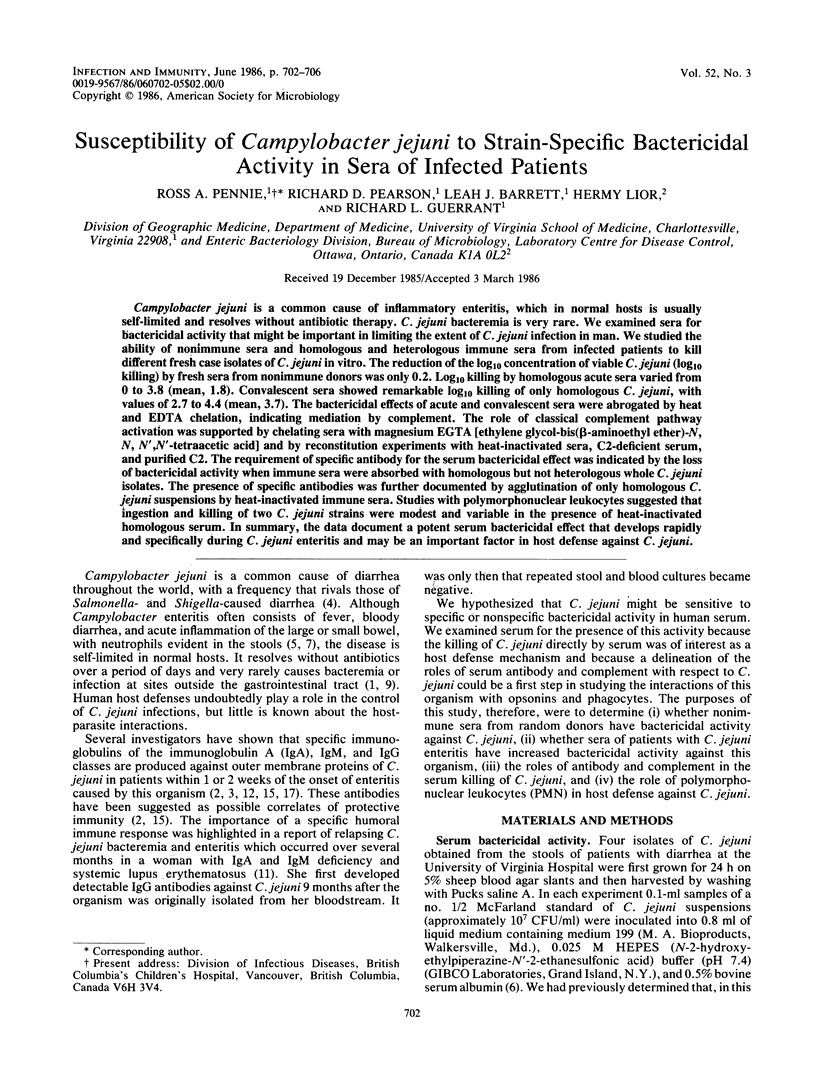

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anders B. J., Lauer B. A., Paisley J. W., Reller L. B. Double-blind placebo controlled trial of erythromycin for treatment of Campylobacter enteritis. Lancet. 1982 Jan 16;1(8264):131–132. doi: 10.1016/s0140-6736(82)90380-4. [DOI] [PubMed] [Google Scholar]
- Blaser M. J., Duncan D. J. Human serum antibody response to Campylobacter jejuni infection as measured in an enzyme-linked immunosorbent assay. Infect Immun. 1984 May;44(2):292–298. doi: 10.1128/iai.44.2.292-298.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaser M. J., Duncan D. J., Osterholm M. T., Istre G. R., Wang W. L. Serologic study of two clusters of infection due to Campylobacter jejuni. J Infect Dis. 1983 May;147(5):820–823. doi: 10.1093/infdis/147.5.820. [DOI] [PubMed] [Google Scholar]
- Blaser M. J., Reller L. B. Campylobacter enteritis. N Engl J Med. 1981 Dec 10;305(24):1444–1452. doi: 10.1056/NEJM198112103052404. [DOI] [PubMed] [Google Scholar]
- Blaser M. J., Wells J. G., Feldman R. A., Pollard R. A., Allen J. R. Campylobacter enteritis in the United States. A multicenter study. Ann Intern Med. 1983 Mar;98(3):360–365. doi: 10.7326/0003-4819-98-3-360. [DOI] [PubMed] [Google Scholar]
- Brooks G. F., Israel K. S., Petersen B. H. Bactericidal and opsonic activity against Neisseria gonorrhoeae in sera from patients with disseminated gonococcal infection. J Infect Dis. 1976 Nov;134(5):450–462. doi: 10.1093/infdis/134.5.450. [DOI] [PubMed] [Google Scholar]
- Butzler J. P., Skirrow M. B. Campylobacter enteritis. Clin Gastroenterol. 1979 Sep;8(3):737–765. [PubMed] [Google Scholar]
- Edwards M. S., Nicholson-Weller A., Baker C. J., Kasper D. L. The role of specific antibody in alternative complement pathway-mediated opsonophagocytosis of type III, group B Streptococcus. J Exp Med. 1980 May 1;151(5):1275–1287. doi: 10.1084/jem.151.5.1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrant R. L., Lahita R. G., Winn W. C., Jr, Roberts R. B. Campylobacteriosis in man: pathogenic mechanisms and review of 91 bloodstream infections. Am J Med. 1978 Oct;65(4):584–592. doi: 10.1016/0002-9343(78)90845-8. [DOI] [PubMed] [Google Scholar]
- Hill D. R., Burge J. J., Pearson R. D. Susceptibility of Giardia lamblia trophozoites to the lethal effect of human serum. J Immunol. 1984 Apr;132(4):2046–2052. [PubMed] [Google Scholar]
- Johnson R. J., Nolan C., Wang S. P., Shelton W. R., Blaser M. J. Persistent Campylobacter jejuni infection in an immunocompromised patient. Ann Intern Med. 1984 Jun;100(6):832–834. doi: 10.7326/0003-4819-100-6-832. [DOI] [PubMed] [Google Scholar]
- Kaldor J., Pritchard H., Serpell A., Metcalf W. Serum antibodies in Campylobacter enteritis. J Clin Microbiol. 1983 Jul;18(1):1–4. doi: 10.1128/jcm.18.1.1-4.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lior H. New, extended biotyping scheme for Campylobacter jejuni, Campylobacter coli, and "Campylobacter laridis". J Clin Microbiol. 1984 Oct;20(4):636–640. doi: 10.1128/jcm.20.4.636-640.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lior H., Woodward D. L., Edgar J. A., Laroche L. J., Gill P. Serotyping of Campylobacter jejuni by slide agglutination based on heat-labile antigenic factors. J Clin Microbiol. 1982 May;15(5):761–768. doi: 10.1128/jcm.15.5.761-768.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills S. D., Bradbury W. C. Human antibody response to outer membrane proteins of Campylobacter jejuni during infection. Infect Immun. 1984 Feb;43(2):739–743. doi: 10.1128/iai.43.2.739-743.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennie R. A., Zunino J. N., Rose C. E., Jr, Guerrant R. L. Economical, simple method for production of the gaseous environment required for cultivation of Campylobacter jejuni. J Clin Microbiol. 1984 Sep;20(3):320–322. doi: 10.1128/jcm.20.3.320-322.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svedhem A., Gunnarsson H., Kaijser B. Diffusion-in-gel enzyme-linked immunosorbent assay for routine detection of IgG and IgM antibodies to Campylobacter jejuni. J Infect Dis. 1983 Jul;148(1):82–92. doi: 10.1093/infdis/148.1.82. [DOI] [PubMed] [Google Scholar]


