Abstract
Background
Anxiety and smoking associations have been examined previously, but not in high risk populations of smokers, such as black males, who bear an excess burden of smoking-related illnesses.
Methods
This study assessed the relation between self-reported smoking status and anxiety using data collected by structured telephone interviews with a sample of 430 black, middle-aged males participating in an ongoing cancer prevention trial.
Results
There was a significant association between anxiety caseness and smoking (p = .006), with more probable cases among current smokers. A priori t-tests showed that current smokers had greater anxiety than former and nonsmokers (p's = 0.02). Among current smokers, greater anxiety was associated with heavier smoking (p = .008), an association not present among former smokers.
Discussion
This study could guide future experimental studies examining smoking-anxiety associations and inform intervention strategies addressing anxiety in underserved nicotine dependent populations with high tobacco-related risks.
Keywords: Anxiety symptoms, Smoking, African American, Men, Cancer prevention
Introduction
Anxiety has been implicated in smoking initiation, maintenance, and relapse (for review, see [1]). However, the evidence is not entirely consistent, causal mechanisms are unclear, and boundary conditions have yet to be fully identified. Importantly, little research has examined the relation between anxiety and smoking in high-risk groups and, to our knowledge, none has focused on black smokers. The present study begins to address this gap in the literature by examining the relations between anxiety and smoking prevalence and frequency in a sample of urban and mostly foreign-born black men. There is now ample and sufficient evidence that cigarette smoking is a causal factor in many adult-onset illnesses, including many different cancers, cardiovascular diseases, and respiratory diseases [2]. As a group, black smokers in the United States have elevated risk for tobacco-related diseases [3]. If anxiety plays a role in smoking behavior, the treatment of anxiety symptoms could be an important target for smoking cessation and tobacco-related disease prevention efforts.
Compared with other social groups in the U.S., black men are at particularly high risk for tobacco-related morbidity and mortality cf. [4-7]. For example, smoking is the leading cause of lung cancer and black men have the highest lung cancer incidence and mortality rates: black men are 37% more likely than white men to develop lung cancer [8], despite 2007 estimates showing that U.S. black males have a lower age-adjusted lifetime prevalence of smoking (19% [17.11-20.9%]) than white males (22.3% [21.02-23.60])— with those figures being lower in males between the ages of 45-65 compared to younger age groups [9]. Long-standing evidence consistently suggests that black smokers report smoking fewer cigarettes per day than whites [10]. Bennett and colleagues [11] reported that black immigrants from Africa and the Caribbean have lower smoking rates than native U.S. blacks; however, even in countries with very low smoking prevalence compared to the U.S., there is evidence of enormous tobacco-related burden [12]. Moreover, differences in smoking prevalence between native and immigrant populations disappear in later generation immigrants suggesting increased smoking rates as a result of acculturation [11, 13]. Additional risk of acculturation-related increased smoking rates among black immigrants results from the likelihood of new immigrant populations to live in low socioeconomic status once in the U.S., and low income is a key predictor of smoking and tobacco-related disease in numerous studies in the past few decades.
Despite smoking fewer cigarettes per day, smokers who are black have a stronger preference for high nicotine and mentholated cigarettes, inhale more deeply, and have slower nicotine metabolism than their white counterparts [10, 14-20]. This evidence, together with recent genetics and pharmacology studies (e.g., [21, 22]), suggests that genetic and racial factors partially explain why some subgroups of smokers, such as blacks, may have greater nicotine dependence risk and more difficulty quitting smoking than other groups. Indeed, while blacks are more likely to attempt to quit smoking than whites in any given year [15], their quit smoking success rates are lower than other racial groups [15, 23, 24]. Recent estimates suggest that 70% of black smokers in the U.S. state a desire to quit smoking, yet only 35% ultimately quit smoking compared to 51% of whites [25].
Genetic and pharmacokinetic evidence provide only partial explanations of blacks' increased risk of nicotine dependence and greater difficulty quitting smoking. There may be treatable psychosocial and psychiatric factors, such as anxiety symptoms, that also contribute to cessation difficulties among some black smokers. In broader cross sections of primarily non-minority smokers, researchers have long known that smokers attribute relapse to anxiety symptoms (e.g., [26, 27]) and a recent review of smoking-anxiety associations by Morrisette and colleagues [1] suggests that smokers with comorbid anxiety disorder as well as those with greater pre-quit levels of anxiety may have greater anxiety-related nicotine withdrawal symptoms and have greater difficulty maintaining abstinence after a quit attempt. Thus, examining anxiety-smoking associations in a high-risk population of black men could lead to a better understanding of barriers that affect smoking behavior change and improve treatment strategies to promote cessation and prevent smoking relapse. However, little is known about the anxiety-smoking link in minority populations.
Purpose
The present study examines the relation between smoking status and anxiety symptoms, using a standardized measure of anxiety symptoms, in a sample of middle-aged, black men participating in an ongoing cancer prevention trial in the New York City metropolitan area. Based on prior research in samples of white smokers, we hypothesized that smoking would be significantly associated with anxiety symptoms. The findings will address a gap in the literature, but we consider this study to be preliminary and hypothesis generating for future research because the analyses were exploratory and secondary to the aims of the parent study.
Methods
Design
This study examined responses to survey data collected as part of an ongoing randomized controlled trial entitled, the Cancer Awareness and Prevention trial. In the trial, participants were randomized to one of two telephone-delivered health education intervention conditions promoting either informed decision-making about prostate cancer testing or awareness of and adoption of national dietary recommendations for fruit and vegetable consumption. Surveys were administered prior to the intervention and again approximately eight months later. Participants received $10 cash or a $10 gift card upon completion of each survey. Social-demographic variables were assessed at baseline, whereas anxiety and smoking variables were assessed at follow-up. There was no relation between intervention condition and either anxiety or smoking status at follow-up. The study was approved by the relevant university Institutional Review Boards and informed consent was obtained from all participants.
Participants
Participants in the parent study were recruited by telephone screening of beneficiaries of a health benefit fund comprising approximately 355,000 individuals in the New York City metropolitan area. Inclusion criteria included being a self-identified black male between the ages of 45 to 70 years old. A unique strength of this study is that this population had many black men from the Caribbean. There has been a rapid increase in Caribbean immigrants to the U.S. in the past few decades—and they represent almost one-third of New York City's black population [28]—but, little is known about their smoking habits and risk factors. Exclusion criteria included a prior prostate cancer diagnosis, a prostate cancer test within the past 12 months, and a stated intention to travel or to be unreachable by telephone for follow-ups. Between June 2005 and July 2007, 1,777 individuals were telephoned and screened for eligibility. Among those screened, 490 (27.6%) were eligible and completed the baseline survey, 1153 (64.9%) were ineligible, 134 (7.5%) refused after eligibility was confirmed. A final sample of 430 participants with complete smoking and anxiety data was used for this study.
Data Collection and Measures
Trained interviewers used a structured, telephone interview to collect data. Interviews were audio-recorded and monitored for quality control. Supervisors performed quality ratings on two-thirds of all interviews using a 10-point rating form that assessed a range of interviewer behaviors, including accuracy of questioning and data recording, interview pace, and responsiveness to respondents' questions. Eighty-four percent of the checked interviews scored 9 (90%) or better. During the formative evaluation phase of this research, survey materials were subject to a variety of techniques to reduce response error, including cognitive interviewing [29] and readability tests. Thirty-five men from the target population were enrolled to assist with the formative evaluation. Cognitive interviewing techniques included probes that assessed comprehension, ease of item recall, difficulty level, and how men were processing questions. Responses were reviewed and used to inform revisions of the survey. A Simple Measure of Gobbledygook (SMOG) [30, 31] was used to assess readability of the preliminary survey questions. The SMOG analysis helped us to determine readability and identify ways to modify the survey so that it resulted in a 7th grade readability score.
Descriptive Social and Demographic Variables
The following social and demographic variables were assessed: age, immigrant status, marital status, and education.
Generalized Anxiety Symptoms
Anxiety symptoms were measured using the 7-item anxiety subscale of the Hospital Anxiety and Depression Scale (HADS) [32]. The HADS is frequently used as a screening tool to measure generalized anxiety symptoms in hospital, outpatient, and community samples, often in cancer and cancer prevention studies [33]. Participants rated their symptoms (e.g., tense, worrying thoughts, feelings of panic) over the previous week using a four-point Likert scale (0-3, varying response categories). A summary anxiety symptom score was calculated by summing the items. Internal consistency of the measure was good (Cronbach's alpha = .73). Sellick and Edwardson [34] suggest the following cut-points for determining caseness: <8 = non-case, 8-10 = borderline case, >10 = probable case of diagnosable anxiety disorder.
Smoking History and Current Status
All smoking data were collected by self-report. Self-report is considered a reliable and valid measure of smoking status and history [35], particularly when respondents are not enrolled in a smoking cessation trial. Smoking status was recorded as a three-level variable (never smoked, former smoker, current smoker). Current and former smokers reported years of smoking and average number of cigarettes smoked per day. Former smokers reported number of years since they had quit smoking.
Analytic Approach
A Chi-square test was used to assess the association between smoking status (never, former, current) and anxiety (non-case, borderline case, probable case). A one-way ANOVA with follow-up contrasts (Least Square Difference) was used to examine mean differences in total anxiety scores between never, former, and current smokers. Finally, among current smokers, the bivariate relation between daily smoking rate (cigarettes smoked per day) and total anxiety score was tested. Analyses were performed using SPSS version 16.
Results
Participant Characteristics
The sample consisted of 430 black men who were mostly middle-aged (M = 54.96, SD = 6.23 years), married (83%) and foreign born (82%). Immigrants were mostly from the Caribbean (62%). Nearly one-third had less than a high school education. A slight majority of the men were never smokers (n = 233; 54%). Forty-four percent (n = 197) of the sample had a history of smoking. Among those with a history of smoking, 60 (30%) were current smokers and 137 (70%) were former smokers. On average, the current smokers had smoked for more than two decades (M = 25.60, SD = 11.18 years) and would be considered light-to-moderate smokers (M = 9.87, SD = 7.49 cigarettes per day). On average, the former smokers quit more than a decade ago (M = 14.98, SD = 10.78 years quit), had smoked for less than two decades (M = 18.55 SD = 11.39), and would be considered light-to-moderate smokers (M = 12.33, SD = 9.97 cigarettes per day). Based on their HADS scores, the majority of men (n = 411, 95.6%) were non-cases (normal anxiety symptom presentation), 10 (2.3%) were borderline cases, and 9 (2.1%) were probable cases.
Anxiety-Smoking Association
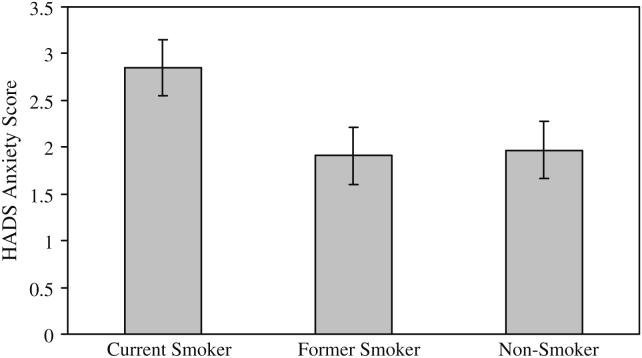
These analyses did not include any covariates, because anxiety was unrelated to the measured social and demographic variables. There was a statistically significant association between HADS anxiety category and smoking status, χ2 (4, N = 430) = 14.27, p = .006. Phi estimates of effect size show that this association explains 18.22% of the variance. More than half (56%) of all men in the probable anxiety case category currently smoke, in contrast to only 20% of borderline cases and 13% of non-cases. Mean anxiety scores also varied as a function of smoking status, F (2,427) = 2.97, p = 0.05. Contrast analyses and the means shown in Fig. 1 revealed that current smokers reported a higher level of anxiety than former smokers (p = .02) and never smokers (p = .02). There was no difference in anxiety between former and never smokers. Among the current smokers (n = 60), heavier smokers had higher anxiety scores (r = 0.34, p = .008). Among the former smokers (n = 134), there was no relation between previous daily smoking rate and current reported anxiety (r = 0.07, p = 0.45). In secondary analysis, we assessed the effect of nativity on the smoking-anxiety association using univariate ANOVA analyses (immigrant [yes/no] vs. smoking status [never/former/current] predicting mean anxiety score.) There was not a significant interaction, suggesting that the association between anxiety symptoms and smoking status were similar between immigrant and native U.S. groups.
Fig. 1.
Mean (SE) anxiety as a function of smoking status (n = 430)
Discussion
This study addresses a gap in the smoking and health disparities literatures by providing initial support of our hypothesis: in a high-risk sample of middle-aged, urban African American and immigrant black men, smoking is significantly associated with anxiety symptoms—results consistent in studies with non-minority smokers. In this sample, significantly more individuals identified by the HADS as probable cases with anxiety disorder were smokers; and smokers reported greater mean anxiety symptoms than either former or never smokers. Moreover, current smokers with heavier daily smoking had significantly greater mean anxiety symptom scores than the current smokers who smoked fewer cigarettes per day. This association between daily smoking rates and anxiety was not observed in former smokers, and there was no moderating effect of nativity, suggesting consistent anxiety-smoking associations among U.S. and immigrant black subgroups in our sample.
To our knowledge, this study is the first to demonstrate relations between anxiety symptoms and smoking in a sample of black male smokers. Based on probable and borderline caseness, our sample had relatively high rates of potential generalized anxiety (4.4%) compared to current and lifetime prevalence of anxiety in black (1.9%; 3.0%), middle aged (2.1%; 5.2%), and urban dwellers (2.0%; 4.0%) [36]. This sample's anxiety rates together with its higher lifetime and current smoking prevalence estimates compared to current U.S. estimates of blacks may represent an inflated risk of anxiety-smoking associations in the general population—evidence that future population-based studies must bear out. On the other hand, the results highlight an important association that could prompt future examination of mechanisms underlying this relation in minority smokers. Such future research is important in addressing tobacco-related disparities in this group, such as difficulties in quitting. Moreover, the clear anxiety-smoking association highlights that the target population (combined native and immigrant, urban, non-patient, black male smokers) could be an excellent one for future prospective studies that could capitalize on nativity comparisons in better understanding the development of anxiety-smoking associations. For example, Bennett and colleagues [11] suggest fairly rapid changes in smoking status within the first couple of years after migration due to acculturation adaptations to U.S. society that could influence both anxiety and health behaviors such as smoking status, particularly in low income, urban settings. Future studies that prospectively examine short-term changes in smoking status during the process of acculturation could provide greater information on smoking-anxiety associations. Expanded discussion of potential mechanisms underlying anxiety-smoking relations, and theoretical conceptualizations of this relation is beyond the scope of this brief report. Extant theories explain the occurrence and maintenance of each disorder (anxiety and nicotine dependence) separately, but there continues to be a need for more comprehensive theories that conceptualize anxiety-smoking co-occurrence.
This study supports the premise that even subsyndromal anxiety symptoms may relate to the maintenance of nicotine dependence—a relation that could potentially undermine smoking cessation intentions and actions. This is a particular concern in black smokers, who appear to have greater difficulty quitting smoking than other groups of smokers. Therefore, to address the public health priority to improve smoking treatments for underserved high-risk smokers, future studies could explore the efficacy of theoretically based strategies that address anxiety symptom management within the context of smoking cessation and relapse prevention. In recent decades, treatment approaches based on conditioning theory applications for anxiety disorders have been explored in addictions treatment [37-41]. Further efforts in this arena could promote strategies that incorporate cue exposure or anxiety management components to simultaneously address anxiety symptoms and nicotine dependence.
In addition to replication studies to determine the reliability of these results, further study is warranted to inform the directionality of the smoking-anxiety association. Anecdotal and empirical evidence have previously demonstrated associations between anxiety, stress, and smoking in other subgroups of smokers, but the associations are not well understood [1]. Nicotine can have anxiolytic effects that vary depending on dose, route and timing of administration, and degree of anxiety evoked; and epidemiological evidence suggests higher incidence of smoking in populations with anxiety disorders compared to nonclinical populations [1]. Additional evidence suggests that smoking deprivation and nicotine withdrawal can produce anxiogenic effects [42], however, little is known about the conditions under which smoking could increase anxiety symptoms in smokers, or affect the maintenance of smoking among those with anxiety disorders or persistent anxiety symptoms. Hence, there remains a great opportunity for research to improve our understanding of smoking-anxiety associations, mechanisms that underlie the associations and pathways that lead to the co-occurrence of anxiety, anxiety disorders, tobacco use, and tobacco dependence—particularly among high risk populations of smokers who bear the larger proportion of tobacco-related disease risk.
A recent study offers one explanation for the anxiety differences observed between current smokers and non-smokers in the present study sample. Okuyemi and colleagues [43] demonstrated that relative to nonsmokers, smokers showed greater activity in brain regions associated with emotion and reward, suggesting that smokers may have greater sensitivity to anxiety-eliciting stimuli than nonsmokers. They also found differential attention and arousal responses to the presentations of smoking cues between Caucasian and African American smokers, suggesting greater anxiety-related sensitivity among the African American smokers. Alongside Okuyemi and colleagues [43] results, the present findings provide evidence that smoking maintenance in black men may be influenced in part by emotional factors, an argument that has thus far received little attention.
Several limitations should be considered in the interpretation of the present results. Foremost, the study relied on a secondary analysis of data from an ongoing study with objectives unrelated to smoking, thus, preventing us to test broader sets of hypotheses about smoking-anxiety relations with more expanded, standardized measures. Additional limitations include the self-report nature of the data, lack of biomarker data to verify smokers' reported smoking status, and the retrospective reports of daily smoking rates among the former smokers. Therefore, advancing understanding of the potential relation between smoking rates and anxiety requires replication of these results in future studies with biomarkers and a prospective design. We also did not assess year of immigration to assess the potential influence of acculturation on smoking and anxiety. Previous research has shown that a greater acculturation may increase the homogeneity among U.S. blacks of both native and immigrant backgrounds with respect to smoking rates and factors that might influence smoking [11]. Other sample limitations included a relatively small sample size, and the exclusion of younger men and men with history of prostate cancer. Thus, we emphasize the limits to the generaliz-ability of the results even though the results supported our hypothesis and can guide future population-based studies as well as prospective research designs to better delineate smoking-anxiety associations in minority male smokers.
This study adds to evidence of an association between anxiety and current smoking and, to our knowledge, it is the first study to demonstrate this relation in black male smokers—a population at high risk for tobacco-related disease that demonstrates greater difficulty quitting smoking than other populations. It is clear that associations between anxiety, anxiety disorders, nicotine dependence, and smoking cessation are complex, and substantial efforts are needed to better understand their co-occurrence. Future research that examines potential mechanisms could lead to improved intervention development and disease prevention efforts in this population. For example, exploring mechanisms through cue exposure paradigms could inform smoking interventions that simultaneously address anxiety symptoms and nicotine dependence. Moreover, greater attention to the inclusion of underserved and minority groups in such research would address a large gap in the literature and move the field toward reducing disparities in tobacco-related disease and treatment outcomes.
Acknowledgments
This work was supported by grant from the National Institutes of Health (CA104223) to Stephen J. Lepore, Ph.D. The authors thank Uma Nair, MA for her assistance in preparing references for this paper.
References
- Morissette SB, Tull MT, Gulliver SB, Kamholz BW, Zimering RT. Anxiety, anxiety disorders, tobacco use, and nicotine: a critical review of interrelationships. Psychol Bull. 2007;133(2):245–72. doi: 10.1037/0033-2909.133.2.245. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services . The health consequences of smoking: a report of the Surgeon General. U.S. Department of Health and Human Services, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. http://www.surgeongeneral.gov/library/smokingconsequences/. Accessed May 20, 2008. [Google Scholar]
- Ahluwalia JS, Dang KS, Choi WS, Harris KJ. Smoking behaviors and regular source of health care among African Americans. Prev Med. 2002;34(3):393–6. doi: 10.1006/pmed.2001.1004. [DOI] [PubMed] [Google Scholar]
- Cooper R, Rotimi C. Hypertension in blacks. Am J Hypertens. 1997;10(7 Pt 1):804–12. doi: 10.1016/s0895-7061(97)00211-2. [DOI] [PubMed] [Google Scholar]
- Carter JS, Pugh JA, Monterrosa A. Non-insulin-dependent diabetes mellitus in minorities in the United States. Ann Intern Med. 1996;125(3):221–32. doi: 10.7326/0003-4819-125-3-199608010-00011. [DOI] [PubMed] [Google Scholar]
- Hodgson DC, Zhang W, Zaslavsky AM, Fuchs CS, Wright WE, Ayanian JZ. Relation of hospital volume to colostomy rates and survival for patients with rectal cancer. J Natl Cancer Inst. 2003;95(10):708–16. doi: 10.1093/jnci/95.10.708. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention The burden of chronic diseases and their risk factors: National and State perspectives. 2004 http://www.cdc.gov/nccdphp/burdenbook2004. Accessed December 10, 2007.
- American Cancer Society Cancer facts and figures for African Americans. 20072008 http://www.cancer.org/downloads/STT/CAFF2005AACorrPWSecured.pdf. Accessed March 1, 2007.
- Centers for Disease Control and Prevention Early release of selected estimates based on data from the January-September 2007. National Health Interview Survey. 2008:49–54. http://www.cdc.gov/nchs/data/nhis/earlyrelease/200803_08.pdf. Accessed May 20, 2008.
- Kabat GC, Morabia A, Wynder EL. Comparison of smoking habits of blacks and whites in a case-control study. Am J Public Health. 1991;81(11):1483–6. doi: 10.2105/ajph.81.11.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett GG, Wolin KY, Okechukwu CA, et al. Nativity and cigarette smoking among lower income blacks: results from the healthy directions study. J Immigr Minor Health. 2008;10(4):305–11. doi: 10.1007/s10903-007-9088-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lwegaba A. Excess healthcare cost associated with a low smoking prevalence, Barbados. West Indian Med J. 2004;53(1):12–6. [PubMed] [Google Scholar]
- Klonoff EA, Landrine H. Acculturation and cigarette smoking among African Americans: replication and implications for prevention and cessation programs. J Behav Med. 1999;22(2):195–204. doi: 10.1023/a:1018739616989. [DOI] [PubMed] [Google Scholar]
- Clark PI, Gautam S, Gerson LW. Effect of menthol cigarettes on biochemical markers of smoke exposure among black and white smokers. Chest. 1996;110(5):1194–8. doi: 10.1378/chest.110.5.1194. [DOI] [PubMed] [Google Scholar]
- Giovino GA, Schooley MW, Zhu BP, et al. Surveillance for selected tobacco-use behaviors - United States, 1900-1994. MMWR Surveill Summ. 1994;43(3):1–43. [PubMed] [Google Scholar]
- Kabat GC, Hebert JR. Use of mentholated cigarettes and lung cancer risk. Cancer Res. 1991;51(24):6510–3. [PubMed] [Google Scholar]
- Okuyemi KS, Ebersole-Robinson M, Nazir N, Ahluwalia JS. African-American menthol and nonmenthol smokers: differences in smoking and cessation experiences. J Natl Med Assoc. 2004;96(9):1208–11. [PMC free article] [PubMed] [Google Scholar]
- Okuyemi KS, Richter KP, Ahluwalia JS, Mosier MC, Nazir N, Resnicow K. Smoking reduction practices among African American smokers. Nicotine Tob Res. 2002;4(Suppl 2):S167–73. doi: 10.1080/1462220021000032744. [DOI] [PubMed] [Google Scholar]
- Perez-Stable EJ, Herrera B, Jacob P, 3rd, Benowitz NL. Nicotine metabolism and intake in black and white smokers. JAMA. 1998;280(2):152–6. doi: 10.1001/jama.280.2.152. [DOI] [PubMed] [Google Scholar]
- Wagenknecht LE, Cutter GR, Haley NJ, et al. Racial differences in serum cotinine levels among smokers in the Coronary Artery Risk Development in (Young) Adults study. Am J Public Health. 1990;80(9):1053–6. doi: 10.2105/ajph.80.9.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz NL. Clinical pharmacology of nicotine: implications for understanding, preventing, and treating tobacco addiction. Clin Pharmacol Ther. 2008;83(4):531–41. doi: 10.1038/clpt.2008.3. [DOI] [PubMed] [Google Scholar]
- Mwenifumbo JC, Sellers EM, Tyndale RF. Nicotine metabolism and CYP2A6 activity in a population of black African descent: impact of gender and light smoking. Drug Alcohol Depend. 2007;89(1):24–33. doi: 10.1016/j.drugalcdep.2006.11.012. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Novotny TE, Pierce JP, Hatziandreu EJ, Patel KM, Davis RM. Trends in cigarette smoking in the United States. The changing influence of gender and race. JAMA. 1989;261(1):49–55. [PubMed] [Google Scholar]
- Trinidad DR, Gilpin EA, White MM, Pierce JP. Why does adult African-American smoking prevalence in California remain higher than for non-Hispanic whites. Ethn Dis. 2005;15(3):505–11. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Smoking cessation during previous year among adults - United States, 1990 and 1991. MMWR. 1998;42(26):504–7. [PubMed] [Google Scholar]
- Brandon TH, Tiffany ST, Obremski KM, Baker TB. Postcessation cigarette use: the process of relapse. Addict Behav. 1990;15(2):105–14. doi: 10.1016/0306-4603(90)90013-n. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Relapse following smoking cessation: a situational analysis. J Consult Clin Psychol. 1982;50(1):71–86. doi: 10.1037//0022-006x.50.1.71. [DOI] [PubMed] [Google Scholar]
- New York City Department of City Planning The Newest New Yorkers 2000: Immigrant New York in the New Millennium Briefing Booklet. 2004 http://www.nyc.gov/html/dcp/pdf/census/nny_briefing_booklet.pdf. Accessed May 20, 2008.
- Willis G. Cognitive interviewing and questionnaire design: a training manual. Office of Research and Methodology, U.S. Department of Health and Human Services. 1994 http://www.nida.nih.gov/pdf/monographs/monograph167/416-438_Willis.pdf. Accessed June 30, 2008.
- McLaughlin GH. SMOG grading - a new readability formula. J Read. 1969;22:639–46. [Google Scholar]
- Weinrich SP, Boyd M, Herman J. Tool adaptation to reduce health disparities. In: Stromborg M, Olsen S, editors. Instruments for clinical health-care research. Boston, MA; Jones and Bartlett Publishers: 2003. pp. 20–32. [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Bultz BD. Cancer distress screening. Needs, models, and methods. J Psychosom Res. 2003;55(5):403–9. doi: 10.1016/s0022-3999(03)00514-2. [DOI] [PubMed] [Google Scholar]
- Sellick SM, Edwardson AD. Screening new cancer patients for psychological distress using the hospital anxiety and depression scale. Psychooncology. 2007;16(6):534–42. doi: 10.1002/pon.1085. [DOI] [PubMed] [Google Scholar]
- Hatziandreu EJ, Pierce JP, Fiore MC, Grise V, Novotny TE, Davis RM. The reliability of self-reported cigarette consumption in the United States. Am J Public Health. 1989;79(8):1020–3. doi: 10.2105/ajph.79.8.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF. About 26% of people in the U.S. have an anxiety, mood, impulse control, or substance disorder. Evid Based Ment Health. 2006;9(1):27. doi: 10.1136/ebmh.9.1.27. [DOI] [PubMed] [Google Scholar]
- Collins BN, Brandon TH. Effects of extinction context and retrieval cues on alcohol cue reactivity among nonalcoholic drinkers. J Consult Clin Psychol. 2002;70(2):390–7. [PubMed] [Google Scholar]
- Conklin CA. Environments as cues to smoke: implications for human extinction-based research and treatment. Exp Clin Psychopharmacol. 2006;14(1):12–9. doi: 10.1037/1064-1297.14.1.12. [DOI] [PubMed] [Google Scholar]
- Lee JH, Kwon H, Choi J, Yang BH. Cue-exposure therapy to decrease alcohol craving in virtual environment. Cyberpsychol Behav. 2007;10(5):617–23. doi: 10.1089/cpb.2007.9978. [DOI] [PubMed] [Google Scholar]
- Marissen MA, Franken IH, Blanken P, van den Brink W, Hendriks VM. Cue exposure therapy for the treatment of opiate addiction: results of a randomized controlled clinical trial. Psychother Psychosom. 2007;76(2):97–105. doi: 10.1159/000097968. [DOI] [PubMed] [Google Scholar]
- Thewissen R, Snijders SJ, Havermans RC, van den Hout M, Jansen A. Renewal of cue-elicited urge to smoke: implications for cue exposure treatment. Behav Res Ther. 2006;44(10):1441–9. doi: 10.1016/j.brat.2005.10.010. [DOI] [PubMed] [Google Scholar]
- West R, Hajek P. What happens to anxiety levels on giving up smoking? Am J Psychiatry. 1997;154(11):1589–92. doi: 10.1176/ajp.154.11.1589. [DOI] [PubMed] [Google Scholar]
- Okuyemi KS, Powell JN, Savage CR, et al. Enhanced cue-elicited brain activation in African American compared with Caucasian smokers: an fMRI study. Addict Biol. 2006;11(1):97–106. doi: 10.1111/j.1369-1600.2006.00007.x. [DOI] [PubMed] [Google Scholar]