Abstract
BACKGROUND
Men with localized prostate carcinoma are faced with important treatment decisions, and quality of life (QoL) information has become a crucial element of decision making. The first objective of this study was to compare the early, health-related QoL (HRQoL) of men with localized prostate carcinoma who were treated with radical prostatectomy, external beam radiotherapy, or brachytherapy. A second objective was to identify demographic and psychosocial variables that predict HRQoL.
METHODS
Two-hundred fifty-six men with localized prostate carcinoma were interviewed within 7 weeks of treatment initiation. The interview included measures of prostate-specific HRQoL (the University of California—Los Angeles Prostate Cancer Index), general HRQoL (the SF-36), and psychosocial variables.
RESULTS
After adjusting for covariates, treatment group differences were found for both prostate specific HRQoL and general HRQoL. Men who underwent prostatectomy reported more urinary and sexual problems and more general physical dysfunction compared with men who were treated with either form of radiation therapy. Men who were treated with brachytherapy reported the fewest problems in sexual function and the least general physical dysfunction. Few treatment group differences were found in mental functioning. Both demographic factors and psychosocial factors predicted HRQoL. Older men and African-American men reported more physical problems than younger men and Caucasian men, respectively. A supportive social environment, high self-efficacy, and high self-esteem were predictive of better HRQoL.
CONCLUSIONS
Shortly after undergoing treatment for localized prostate carcinoma, men who underwent radical prostatectomy, older men, and African-American men are at heightened risk for experiencing prostate-specific and general deficits in HRQoL. Having psychosocial resources from which to draw may enhance HRQoL.
Keywords: quality of life, prostate carcinoma, radical prostatectomy, radiotherapy, social environment, ethnicity, self-efficacy, self-esteem
Prostate carcinoma is the most common solid tumor malignancy in American men. The American Cancer Society estimates that, in 2001, approximately 198,100 men will be diagnosed with prostate carcinoma in the United States.1 Nevertheless, fewer than 20% of these men are expected to die from the disease, and 93% will survive for at least 5 years postdiagnosis, making quality of life (QoL) issues paramount in this population.
The man who is diagnosed with localized prostate carcinoma has several therapeutic options. These include radical prostatectomy (RP), or surgical removal of the prostate gland; external beam radiotherapy (EBR), or focusing radiation on the malignancy from outside of the body; and brachytherapy (BT), or implanting radioactive seeds into the prostate gland. Patients also may elect not to be treated. There is no consensus on which of these therapeutic approaches is best, and results from nonrandomized studies show similar survival rates.2–4 Thus, selection of the appropriate treatment for patients with clinically localized prostate carcinoma frequently is based on factors other than survival advantage.
Both medical and nonmedical factors will determine treatment choice. Stage and grade of disease, age, number and type of comorbid conditions, and access to a given treatment all are important factors in treatment selection. Some men have fewer choices than others. For example, an elderly man with low-grade, early-stage prostate carcinoma and heart disease is not a good candidate for RP. Consequently, he may be encouraged by his physician to select a less risky treatment, such as EBR. However, for many others, the appropriate treatment is less obvious. It is in these situations that information about QoL outcomes becomes critical to decision making.
Several studies have compared health-related QoL (HRQoL) outcomes across treatments.5–11 Most have compared RP with EBR. In general, men who undergo RP report more urinary dysfunction (i.e., greater incontinence and greater use of absorptive pads) and more sexual dysfunction (i.e., reduced erectile capacity and low level of sexual desire) compared with men who are treated with EBR.5,7–11 Bowel dysfunction (i.e., urgency and diarrhea) is reported more often by men who are treated with EBR compared with men who undergo RP.8,10 In one study, men who underwent RP or men who were treated with EBR evidenced short-term reductions in energy level and role limitations due to physical function.7 By 1 year post-treatment, both groups showed significant and clinically meaningful increases in role functioning, whereas only the group of men who underwent RP showed substantial improvements in energy level.
Recently, comparisons have been made between BT and other treatments. Zelefsky et al.12 compared men who were treated with EBR with men who were treated with BT. In the short term, those who received BT showed slightly higher urinary toxicity (e.g., urethral stricture) compared with those who were treated with EBR. Brandeis et al.13 compared men who were treated with BT (both with and without pretreatment EBR) with men who underwent RP.13 Although the RP group reported greater urinary leakage than the BT group, the BT group reported more obstructive and irritative urinary symptoms (i.e., increased frequency and urgency, nocturia, and weak urine stream).
Those studies showed that prostate-specific complications, such as urinary, sexual, and bowel dysfunction, will vary by treatment. However, there appear to be few differences across treatment groups in other domains of HRQoL. Apart from some role limitations and decreased energy levels, functioning in most other domains appears to be unaffected by treatment. Nonetheless, concluding that treatments for localized prostate carcinoma have little effect on general HRQoL may be premature. With one notable exception,7 many studies have assessed HRQoL anywhere from several months to several years after treatment. At these later time points, men may have regained most of their general functioning. Undoubtedly, attending to the long-term sequelae of localized prostate carcinoma is important, but men also may have concerns about the effects of different treatments in the short term.14 To address these issues, we investigated prostate specific HRQoL and general HRQoL shortly after men had undergone treatment with RP, EBR, or BT.
A second focus of this analysis was to examine the relation of demographic and psychosocial factors to HRQoL in men who are treated for localized prostate carcinoma. Demographic factors, such as age, ethnicity, and marital status, appear to be important predictors of recovery.6,15,16 Psychosocial factors, such as stress, optimism, and social support, also have been implicated in men's recovery from prostate carcinoma and its treatments.17–19
MATERIALS AND METHODS
Participants and Procedure
For this study, the following medical criteria for patient inclusion were used: primary treatment within the past 3 months, no additional (i.e., salvage) treatment, no evidence of metastasis, and no other diagnosis of other malignant disease (except skin carcinoma). The men in this study all were participating in a clinical trial examining the effects of psychoeducational and support group interventions on their adjustment to prostate carcinoma. The findings reported here are from the first wave of data that were collected prior to random assignment to an experimental condition. Results of the intervention study will be reported elsewhere.
Participants were recruited through the offices of urologists and radiation oncologists in the greater Pittsburgh area. Working with the referring offices, we developed a list of potentially eligible patients. Of 574 recruitment letters sent, we received 89 postcards (16%) declining participation. We telephoned those who had not returned a postcard and described the study in greater detail. At this step, 104 men (18%) declined participation, and 9 men (2%) could not be reached by phone, yielding a final response rate of 65%. Based on their responses to several screening questions, 93 men failed to meet the inclusion criteria and were deemed ineligible. For the current analyses, we included only those men who were treated with RP, EBR, or BT. We excluded men who had received cryosurgery (4%) or had received a combination of EBR and BT (5%) due to the low frequency of these treatments. Thus, the total sample size was 256 men (156 men in the RP group, 51 men in the BT group, and 49 men in the EBR group). Male research assistants interviewed patients in their homes approximately 7 weeks after treatment initiation (mean ± standard error: 46.2 days ± 1.2 days). Time since diagnosis differed across treatment groups (F[2, 253] = 15.54; P < 0.001). Men who underwent RP were treated sooner after diagnosis (mean ± standard error: 131.8 days ± 6.5 days) compared with men who had received either EBR (209.0 days ± 35.1 days) or BT (266.8 days ± 30.8 days). All participants completed informed consent procedures.
Measures
HRQoL outcomes
We used the University of California—Los Angeles (UCLA) Prostate Cancer Index (PCI) to assess prostate-specific HRQoL.5 The PCI yields measures of urinary, sexual, and bowel functioning that often are affected by treatment. Each scale is standardized, with scores ranging from 0 (poor functioning) to 100 (good functioning). We used the SF-3620 as a general measure of HRQoL. The instrument yields scale scores in four physical domains—physical limitations in performing daily activities, role limitations due to physical health, general health perceptions, and bodily pain—and in four mental domains—vitality and/or energy level, role limitations due to emotional health, problems in social functioning, and mental health. Standardized scores range from 0 (poor functioning) to 100 (good functioning). In addition to the eight scales, the SF-36 yields a global physical component summary (PCS) score and mental component summary score (MCS).22 Component scores can range from 0 (poor functioning) to 100 (good functioning).
Psychosocial predictors
We used the Social Provisions Scale (SPS)23 to measure perceived social support from spouse and from family and/or friends. A composite score of three SPS sub-scales (reassurance of worth, guidance, and attachment) was computed for each source of support. Higher scores indicate higher perceived support. We used the Social Constraints Scale24 to assess negative and unsupportive reactions of spouse and family and/or friends (e.g., avoided you or acted uncomfortable when you talked about your disease). Higher scores indicate higher social constraints.
We used a measure of self-efficacy to assess the extent to which men feel capable of controlling various disease-related problems relevant to adjustment (e.g., control urine leakage)21: Higher scores indicate greater self-efficacy. We used the Rosenberg Self-Esteem Scale to assess self-esteem: Higher scores indicate greater self-esteem.
Demographic and Disease-Related Variables
We collected information on demographics and comorbid medical conditions25 at the screening intake and collected information on Gleason grade and TNM stage26 from patient medical records.
Data Analysis
Frequency distributions and correlations were used to describe the sample, identify possible covariates, and uncover correlations among the variables. We used analyses of variance (ANOVA) and analyses of covariance (ANCOVA) to compare the effects of the various treatments on HRQoL. We also used ANOVA and ANCOVA techniques to analyze the correlations of ethnicity, education, and marital status to HRQoL. It was necessary to introduce covariates into some of the analyses to reduce the chances of uncovering spurious correlations between predictors and HRQoL. A variable was deemed a covariate if it was correlated significantly with both the predictor and the HRQoL parameter. The covariates controlled in each analysis are described below (see Results). We used correlation analyses to identify relations between patient age, psychosocial variables, and HRQoL.
RESULTS
Participant Characteristics
Table 1 shows that the majority of the men were married, Caucasian, college-educated, not currently working, and underwent RP. Clinical and pathologic stages ranged from T1N0M026 (clinically inapparent tumor not palpable or visible by imaging [T1], no regional lymph node metastasis [N0], ands no distant metastasis [M0]) to T3N0M0 (tumor extends through the prostate capsule [T3], no regional lymph node metastasis [N0], and no distant metastasis [M0]). Across all men, tumors were moderately differentiated (mean Gleason sum, 6.1). However, both disease stage and tumor grade varied by treatment. Among men classified with T3 tumors, all underwent RP, whereas men classified with T1 tumors were more likely to have received EBR than either of the other treatments (chi-square test [degrees of freedom (df) 4], 59.0; P < 0.001). The RP group had higher Gleason scores (mean ± standard error: 6.4 ± 0.1) compared with either the EBR group (5.7 ± 0.2) or the BT group (5.6 ± 0.1; F[2, 253] = 16.0; P < 0.001).
TABLE 1.
Patient Characteristics (N = 256)
| Characteristic | No. | % |
|---|---|---|
| Mean age ± SE in yrs (range) | 65.0 ± 0.5 (45−80) | — |
| Marital status | ||
| Married or in marital relationship | 221 | 86 |
| Separated, divorced | 17 | 7 |
| Widowed | 12 | 5 |
| Never married | 6 | 2 |
| Ethnicity | ||
| Caucasian | 229 | 89 |
| African-American | 27 | 11 |
| Education (highest level achieved) | ||
| Graduated from high school | 68 | 27 |
| Graduated from college | 62 | 24 |
| Postgraduate training | 54 | 21 |
| Some college | 43 | 17 |
| Less than high school | 29 | 11 |
| Employment status | ||
| Not working | 134 | 52 |
| Working | 122 | 48 |
| Religion | ||
| Catholic | 116 | 45 |
| Protestant | 104 | 41 |
| Other | 18 | 7 |
| Judaism | 12 | 5 |
| Agnostic/atheist | 6 | 2 |
| Type of treatment | ||
| RP | 156 | 61 |
| BT | 51 | 20 |
| EBRa | 49 | 19 |
| Adjuvant hormone therapy | ||
| No | 216 | 84 |
| Yes | 40 | 16 |
| Mean days ± SE since diagnosis (range) | 173.5 ± 10.4 (33−1311) | — |
| Mean days ± SE since surgery (RP only) (range) | 48.0 ± 1.6 (15−98) | — |
| Mean days ± SE since seed implants (BT only) (range) | 43.2 ± 2.7 (7−87) | — |
| Mean days ± SE since start of radiation (EBR only) (range) | Mean = 43.5 days, SE = 3.1 | |
| TNM stage | Range 7−99 days | |
| T2N0M0 | 176 | 69 |
| T1N0M0 | 48 | 19 |
| T3N0M0 | 31 | 12 |
| Missing | 1 | < 1 |
| Gleason sum at diagnosis (mean ± SE) | 6.1 ± 0.1 | — |
| Other malignant disease | ||
| No | 228 | 89 |
| Yes (melanoma only) | 28 | 11 |
| Prostate problem before treatment | ||
| None | 185 | 72 |
| Benign prostatic hyperplasia | 40 | 16 |
| Prostatitis | 15 | 6 |
| Urination difficulties | 15 | 6 |
| Elevated PSA | 1 | < 1 |
SE: standard error; RP: radical prostatectomy; BT: brachytherapy; EBR: external beam radiotherapy; PSA: prostate specific antigen.
Thirty patients (61%) received concurrent radiation treatment at the time of data collection.
Intercorrelations of HRQoL Outcomes
Partial correlations were computed to assess relations of prostate-specific HRQoL and general HRQoL. Age was a covariate in these analyses. Better urinary function (correlation coefficient (r) = 0.43; P < 0.001), sexual function (r = 0.38; P < 0.001), and bowel function (r = 0.39; P < 0.001) were associated with better general physical functioning. Better urinary function (r = 0.21; P < 0.01), sexual function (r = 0.21; P < 0.01), and bowel function (r = 0.35; P < 0.001) also were associated with better general mental functioning.
Relation of Treatment to HRQoL Outcomes
We conducted ANOVAs and ANCOVAs on the urinary, sexual, and bowel scales of the UCLA PCI to determine whether type of treatment was associated with prostate specific HRQoL. In analyses of urinary and sexual function, age was used as a covariate. One-way tests revealed significant treatment-related differences on two scales of the PCI: urinary function (F[2, 251] = 78.7; P < 0.001) and sexual function (F[2, 249] = 39.4; P < 0.001). Neuman–Keuls post-hoc tests (P < 0.05) were used to identify differences. Men in the EBR group had better urinary function (mean ± standard error: 87.6 ± 3.4) compared with men in the BT group (79.5 ± 3.2). Both radiation groups had better urinary function compared with men in the RP group (44.0 ± 1.9). All men experienced considerable sexual dysfunction, but men in the BT group (38.2 ± 3.1) and men in the EBR group (34.5 ± 3.3) reported better function compared with men in the RP group (9.6 ± 1.8). There were no significant treatment-related differences for bowel function.
We also conducted one-way ANOVAs and ANCOVAs on the PCS and MCS component scores and the eight domain scores of the SF-36 to determine whether type of treatment was associated with general HRQoL. Neuman–Keuls tests were used again to identify differences. Age was a covariate in the analyses involving the MCS, role-physical, role-emotional, and mental health scores. Comorbid conditions were covaried from the analysis of the PCS score.
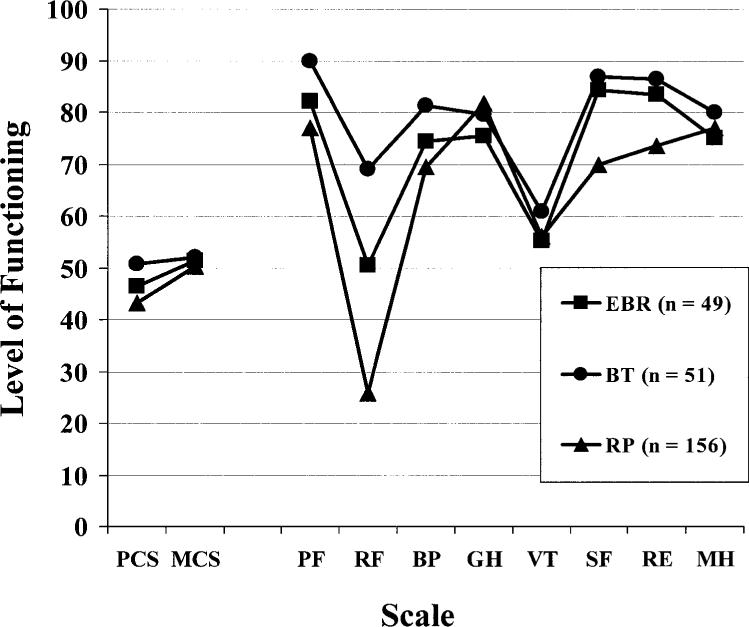
Figure 1 shows a profile of the SF-36 component and domain scores for the three treatment groups. Significant treatment group differences were found across the PCS score (F[2, 252] = 17.3; P < 0.001) but not the MCS score. Men in the BT group reported higher general physical functioning compared with men in the EBR or RP groups. Furthermore, men in the EBR group reported higher general physical functioning compared with men in the RP group. Differences also were apparent across four of the domain scores: physical function (F[2, 253] = 9.6; P < 0.001), role-physical function (F[2, 252] = 28.7; P < 0.001), bodily pain (F[2, 253] = 4.1; P < 0.05), and social function (F[2, 253] = 10.4; P < 0.001). Men in the BT group reported higher physical and role-physical function than men in the EBR or RP groups. Men in the EBR group reported higher role-physical function compared with men in the RP group. Bodily pain was lower in the BT group compared with the RP group. Finally, men in the BT group and men in the EBR group reported higher social function compared with men in the RP group. There were no treatment group differences in the domains of general health, vitality/ energy, role-emotional function, or mental health.
FIGURE 1.
Profiles of general health-related quality of life (HRQoL) by treatment. Note that the treatment group means were adjusted for age or comorbid conditions when appropriate. EBR: external beam radiotherapy; BT: brachytherapy; RP: radical prostatectomy; PCS: physical component summary score; MCS: mental component summary score; PF: physical function; RF: role-physical function; BP: bodily pain; GH: general health; VT: vitality/energy level; SF: social function; RE: role-emotional function; MH: mental health. Higher scores mean better HRQoL.
Relation of Demographic and Psychosocial Variables with HRQoL Outcomes
Demographic
Several demographic variables were associated with HRQoL. Older men tended to have poorer urinary function (r −0.14; P < 0.05) and sexual function (r −0.33; P < 0.001) but better general mental functioning (r = 0.14; P < 0.05) after controlling for treatment type and comorbidity. For analyses of ethnicity (Caucasian vs. African-American), comorbid conditions, treatment type, and age were covariates. Caucasian men reported better urinary function (mean ± standard error: 60.9 ± 1.5) than African-American men (47.4 ± 4.4; F[1, 250] = 8.4; P < 0.01) and reported better bowel function (82.7 ± 1.2) than African-American men (70.5 ± 3.4; F[1, 252] = 11.3; P < 0.01). Caucasian men also reported higher general physical functioning (45.8 ± 0.5) than African-American men (41.6 ± 1.6; F[1, 251] = 6.5; P < 0.05). Educational status (high school educated vs. college educated) was associated with general mental functioning (F[1, 253] = 6.4; P < 0.05) controlling for age and comorbidity. College-educated men reported higher general mental functioning (51.9 ± 0.7) than men who had not advanced beyond high school (49.1 ± 0.9). Finally, marital status was associated with general physical functioning at a trend level (F[1, 254] = 3.8; P < 0.06). Married men (45.8 ± 0.6) reported higher general physical functioning than unmarried men (42.7 ± 1.7).
Psychosocial
Positive and negative social-environmental factors were associated with HRQoL after controlling for age. More social support from the spouse was associated with better urinary function (r = 0.15; P < 0.05) and better general mental functioning (r = 0.16; P < 0.05). More social support from family and/or friends was associated with better general physical functioning (r = 0.16; P < 0.05) and better general mental functioning (r = 0.21; P < 0.01). Greater social constraints from the spouse were associated with lower general mental functioning (r −0.26; P < 0.001). Greater social constraints from family and/or friends were associated with lower general physical functioning (r −0.13; P < 0.05) and lower general mental functioning (r −0.26; P < 0.001).
Self-concept also was related to HRQoL. Number of comorbid conditions was the only covariate in these analyses. A higher level of self-efficacy for disease-related problems was associated with better urinary function (r = 0.25; P < 0.001), sexual function (r = 0.48; P < 0.001), and bowel function (r = 0.27; P < 0.001) and with better general physical functioning (r = 0.28; P < 0.001) and better general mental functioning (r = 0.43; P < 0.001). Although it was unrelated to prostate-specific HRQoL, a higher level of self-esteem was related to better general physical (r = 0.29; P < 0.001) and better general mental functioning (r = 0.32; P < 0.001).
DISCUSSION
The primary objective of this study was to examine the short-term effects of different treatments on the HRQoL of men with localized prostate carcinoma. It is the first study to compare disease-specific and general HRQoL outcomes across three common treatment groups: RP, EBR, and BT. In general, men who underwent RP evidenced the poorest disease-specific HRQoL. Similar to other studies,5,7–10,13 men who underwent RP reported poorer urinary and sexual function than men who were treated with radiation. Similar to findings in a recent study by Zelefsky et al.,12 the men in the current study who were treated with BT had worse urinary function than men who were treated with EBR. However, unlike the results of prior studies that have shown more bowel dysfunction in men who were treated with EBR,8,10 we found no treatment group differences in bowel function. Notably, those earlier studies assessed men years after treatment. Thus, bowel problems may be a latent side effect of EBR.
We used the SF-36 to compare general HRQoL across treatment groups. Overall, men in the BT group reported the best general physical functioning, and men in the RP group reported the worst general physical functioning. We found significant treatment group differences in PCS scores and in four of the eight domain scores: physical limitations in performing daily activities, role limitations due to physical health, body pain, and social function limitations. Men in the BT group scored the highest in these domains, and men in the RP group scored the lowest; men in the EBR group scored in between those in the BT group and the RP group. Other studies have shown few differences across treatment groups in general HRQoL,5,10,13 although they did not assess functioning in the early recovery period, as was done in the current study.
There were no treatment group differences in the domains of general health perception or vitality/energy level. It is interesting to note that general health reportedly was quite good in all treatment groups. Perhaps, after overcoming prostate carcinoma, the impact of other relatively minor ailments is perceived as insignificant. All treatment groups reported similar levels of energy. This finding mirrors that reported by others5,7 and suggests that, shortly after the initiation of treatment, energy levels are not substantially different across these treatment groups.
It appears that treatment group differences in general HRQoL occurred mainly in physical domains. There were no treatment-related differences in general mental functioning (MCS score) or in the domains of role limitations due to emotional functioning. Like the results of other studies,5,10 our results suggest that emotional health is not influenced differentially by surgical treatment versus radiation treatment for patients with localized prostate carcinoma.
The current results show that treatments for patients with localized prostate carcinoma may be associated with early declines in disease-specific and general HRQoL. Others have shown that, although urinary, sexual, bowel, and general HRQoL declines are common in the first months after treatment, functioning in these domains improves substantially by 1 year post-treatment.7,13,15,16 Together, these findings carry clinical import. Information on early HRQoL outcome can help to prepare men mentally for the complications that they will experience with their chosen treatment, thus alleviating any negative psychological consequences that may arise. Data on long-term outcome can help to reassure patients that functioning in most HRQoL domains will improve with time. Furthermore, our findings suggest that interventions aimed at facilitating early recovery from treatments for patients with localized prostate carcinoma should target four areas: physical functioning, role functioning, sexual dysfunction, and urinary dysfunction—particularly in men who undergo RP.
We found that worse urinary, sexual, and bowel function tended to be associated with worse general physical and mental functioning. These relations held even after age was controlled. The results from prior studies have been mixed. Some have shown that greater prostate-specific dysfunction is not associated with general HRQoL,10,11 whereas others have found that greater prostate-specific dysfunction is associated with lower general HRQoL and greater distress and “bother.”6 Differences in the timing of assessment may explain these inconsistencies. Studies showing no relations assessed men years after treatment, when prostate-specific complications were reduced. However, our study, like others that have shown relations, assessed men within months of treatment. Early in recovery, men tend to have greater treatment-related complications and may have greater difficulty coping with these complications.
A secondary objective of this study was to identify demographic and psychosocial factors that predict HRQoL. Age and ethnicity were found to be robust predictors of HRQoL, whereas education level and marital status were less strongly related to it. Like findings in previous reports,6,16 older men reported worse urinary and sexual function but better general mental functioning compared with younger men. It is possible that the older men in our study already had accommodated to preexisting urinary and sexual problems or that they were more inclined to expect that physical health problems would occur with treatment. Thus, they may have been more prepared mentally than the younger men for problems in physical function. African-American men in our study appeared to be at higher risk for physical problems. African-American men reported worse urinary and bowel function and worse general physical functioning than Caucasian men. This is especially intriguing given that a greater percentage of African-American men (56%) than Caucasian men (37%) received some form of radiation treatment, which, as our results and others have shown, tends to result in fewer physical complications than RP. Although we are cautious in drawing conclusions from such a small sample of men and with no pretreatment data, these findings suggest that African-American men may experience more difficulty recovering physically from treatment than Caucasian men.
Married men reported better general physical functioning than unmarried men. Men who had attended college reported better general mental function than men who were not formally educated beyond high school. Perhaps unmarried and less educated men lack the personal and interpersonal resources needed to adjust mentally to the post-treatment experience. If so, then they may be good candidates for educational interventions that may shore up any coping deficits.
The availability of social support and the absence of social constraints were related to better general physical and mental functioning. These results suggest that the quality of the social environment may affect post-treatment adjustment. There are many ways in which a supportive environment may be beneficial. It may help in coping with the loss of basic bodily functions by providing informational or instrumental assistance that can make such problems more manageable. It also may prevent feelings of isolation and thereby reduce the sense that one is progressing through recovery alone. Emotional support may provide reassurance that one is loved and cared for in times of stress. Finally, a warm and supportive atmosphere may make a man feel more comfortable with discussing his illness with others. Open disclosure has been associated with better mental adjustment to prostate carcinoma.18 Social factors, however, were associated less with prostate-specific HRQoL. Perhaps any modification of disease specific physical problems lies within the person alone.
Intrapersonal factors were the strongest psychosocial predictors of HRQoL. Higher self-efficacy for disease-related problems was associated with better prostate-specific HRQoL and better general HRQoL. Higher self-esteem was predictive of better general HRQoL. These results suggest that possessing certain personal resources may lead to better adjustment. Although we are cautious in making this suggestion from cross-sectional data, a recent longitudinal intervention study supports this interpretation. Increasing self-esteem has been associated with better adjustment in women with newly diagnosed breast carcinoma attending an educational support group intervention.27 A sense of personal control and self-worth may lead patients to persist in their efforts at recovery, perhaps by seeking the help of others or by adhering to medical regimens.
There are a few limitations to this study. First, because the data are cross sectional and correlational, it is difficult to eliminate competing explanations of the observed associations. In future work, we will assess the trajectory of HRQoL over time. Second, no information was obtained on pretreatment levels of function. Hence, we do not know how much prostate-specific HRQoL and general HRQoL changed from pretreatment levels.
In this study, we found that early HRQoL outcomes differed across treatment groups for patients with localized prostate carcinoma. Overall, men who underwent RP experienced more urinary and sexual problems and had more general physical deficits compared with men who were treated with radiation. Among the radiation types, men who were treated with BT fared better than men who were treated with EBR across most of the HRQoL outcomes. We also identified demographic and psychosocial factors that predicted HRQoL. Age and ethnicity were strong demographic predictors. Older men and African-American men suffered more physical deficits compared with younger men and Caucasian men, respectively. Physicians may find it helpful to share this risk information with patients prior to selection of therapy. It may assist the patient in selecting an option that is best suited to his individual needs and better prepare him for what is to come. Self-efficacy and self-esteem were the strongest psychosocial predictors. Men low in self-efficacy or self-esteem experienced declines in physical and mental HRQoL. For men with few interpersonal or intrapersonal resources from which to draw, clinical or support group interventions may be desirable.
Acknowledgments
Supported by grant T32 MH19953 from the National Institute of Mental Health (D.T.E.) and grant RO1 CA68354 from the National Cancer Institute (principal investigator, S.J.L.).
The authors thank the important contributions of our coinvestigators, Drs. Richard Schulz, Ronald Hrebinko, Jeffrey Cohen, Thomas Hakala, and Raoul Salup. They also thank their research staff, Renee Rhodes, Timothy Roberts, Michael Mattis, Rocco Mercurio, Karen Pealer, and Todd Crouch, as well as their consultants, Lynn Robertson, R.N.; Leslie Bonci, R.D.; and Drs. Donald Trump, Jay Lutins, Adam Brufsky, John Franz, Stephen Campanella, Scott Long, Robert Schwartz, Ralph Miller, and Ronald Benoit.
Footnotes
Presented in part at the Pan American Congress of Psychosocial and Behavioral Oncology, New York, New York, October 21−23, 1999.
REFERENCES
- 1.American Cancer Society . Cancer facts and figures 2001. American Cancer Society; Atlanta: 2001. [Google Scholar]
- 2.Hanks GE. Radiotherapy or surgery for prostate cancer? Ten and fifteen-year results of external beam therapy. Acta Oncol. 1991;30:231–7. doi: 10.3109/02841869109092359. [DOI] [PubMed] [Google Scholar]
- 3.Chodak GW, Thisted RA, Gerber GS, Johansson JE, Adolfsson J, Jones GW, et al. Results of conservative management of clinically localized prostate cancer. N Engl J Med. 1994;330:242–8. doi: 10.1056/NEJM199401273300403. [DOI] [PubMed] [Google Scholar]
- 4.Lu-Yao GL, Yao S-L. Population-based study of long-term survival in patients with clinically localised prostate cancer. Lancet. 1997;349:906–10. doi: 10.1016/S0140-6736(96)09380-4. [DOI] [PubMed] [Google Scholar]
- 5.Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, Leach GE, et al. Quality-of-life outcomes in men treated for localized prostate cancer. JAMA. 1995;273:129–35. doi: 10.1001/jama.273.2.129. [DOI] [PubMed] [Google Scholar]
- 6.Litwin MS, Flanders SC, Pasta DJ, Stoddard ML, Lubeck DP, Henning JM. Sexual function and bother after radical prostatectomy or radiation for prostate cancer: multivariate quality-of-life analysis from CaPSURE. Cancer of the Prostate Strategic Urologic Research Endeavor. Urology. 1999;54:503–8. doi: 10.1016/s0090-4295(99)00172-7. [DOI] [PubMed] [Google Scholar]
- 7.Lubeck DP, Litwin MS, Henning JM, Stoddard ML, Flanders SC, Carroll PR. Changes in health-related quality of life in the first year after treatment for prostate cancer: results from CaPSURE. Urology. 1999;53:180–6. doi: 10.1016/s0090-4295(98)00408-7. [DOI] [PubMed] [Google Scholar]
- 8.Fowler FJ, Jr., Barry MJ, Lu-Yao G, Wasson JH, Bin L. Outcomes of external-beam radiation therapy for prostate cancer: a study of Medicare beneficiaries in three Surveillance, Epidemiology, and End Results areas. J Clin Oncol. 1996;14:2258–65. doi: 10.1200/JCO.1996.14.8.2258. [DOI] [PubMed] [Google Scholar]
- 9.Lim AJ, Brandon AH, Fiedler J, Brickman AL, Boyer CI, Raub WA, Jr., et al. Quality of life: radical prostatectomy versus radiation therapy for prostate cancer. J Urol. 1995;154:1420–25. doi: 10.1016/s0022-5347(01)66881-2. [DOI] [PubMed] [Google Scholar]
- 10.Shrader-Bogen CL, Kjellberg JL, McPherson CP, Murray CL. Quality of life and treatment outcomes: prostate carcinoma patients’ perspectives after prostatectomy or radiation therapy. Cancer. 1997;79:1977–86. doi: 10.1002/(sici)1097-0142(19970515)79:10<1977::aid-cncr20>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 11.Lilleby W, Fossa SD, Waehre HR, Olsen DR. Long-term morbidity and quality of life in patients with localized prostate cancer undergoing definitive radiotherapy or radical prostatectomy. Int J Radiat Oncol Biol Phys. 1999;43:735–43. doi: 10.1016/s0360-3016(98)00475-1. [DOI] [PubMed] [Google Scholar]
- 12.Zelefsky MJ, Wallner KE, Ling CC, Raben A, Hollister T, Wolfe T, et al. Comparison of the 5-year outcome and morbidity of three-dimensional conformal radiotherapy versus transperineal permanent iodine-125 implantation for early-stage prostatic cancer. J Clin Oncol. 1999;17:517–522. doi: 10.1200/JCO.1999.17.2.517. [DOI] [PubMed] [Google Scholar]
- 13.Brandeis JM, Litwin MS, Burnison CM, Reiter RE. Quality of life outcomes after brachytherapy for early stage prostate cancer. J Urol. 2000;163:851–7. [PubMed] [Google Scholar]
- 14.Robinson L, Hughes LC, Adler DC, Strumpf N, Grobe SJ, McCorkle R. Describing the work of nursing: the case of postsurgical nursing interventions for men with prostate cancer. Res Nurs Health. 1999;22:321–8. doi: 10.1002/(sici)1098-240x(199908)22:4<321::aid-nur6>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 15.Litwin MS, McGuigan KA, Shpall AI, Dhanani N. Recovery of health related quality of life in the year after radical prostatectomy: early experience. J Urol. 1999;161:515–9. [PubMed] [Google Scholar]
- 16.Stanford JL, Feng Z, Hamilton AS, Gilliand FD, Stephenson RA, Eley JW, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the Prostate Cancer Outcomes Study. JAMA. 2000;283:354–60. doi: 10.1001/jama.283.3.354. [DOI] [PubMed] [Google Scholar]
- 17.Bjorck JP, Hopp DP, Jones LW. Prostate cancer and emotional functioning: effects of mental adjustment, optimism, and appraisal. J Psychosoc Oncol. 1999;17:71–85. [Google Scholar]
- 18.Lepore SJ, Helgeson VS. Social constraints, intrusive thoughts, and mental health after prostate cancer. J Soc Clin Psychol. 1998;17:89–106. [Google Scholar]
- 19.Ptacek JT, Pierce GR, Ptacek JJ, Nogel C. Stress and coping processes in men with prostate cancer: the divergent views of husbands and wives. J Soc Clin Psychol. 1999;18:299–324. [Google Scholar]
- 20.Stewart AL, Hays RD, Ware JE. The MOS Short-Form General Health Survey. Med Care. 1988;26:724–35. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Lepore SJ, Helgeson VS. Psychoeducational support group enhances quality of life after prostate cancer. Cancer Res Ther Control. 1999;8:81–91. [Google Scholar]
- 22.Ware JE, Kosinski M, Keller SD. Physical and mental health summary scales: a user's manual. The Health Institute, New England Medical Center; Boston: 1994. [Google Scholar]
- 23.Cutrona CE, Russell DW. The provisions of social relationships and adaptation to stress. In: Jones WH, Perlman D, editors. Advances in personal relationships. JAI Press; Greenwich: 1987. pp. 37–68. [Google Scholar]
- 24.Lepore SJ, Ituarte PHG. Optimism about cancer enhances mood by reducing negative social relations. Cancer Res Ther Control. 1999;8:165–74. [Google Scholar]
- 25.Katz JN, Change LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Fleming ID, Cooper JS, Henson DE, Hutter RVP, Kennedy BJ, Murphy GP, et al. American Joint Committee on Cancer staging manual. 5th ed. Lippincott; Philadelphia: 1997. [Google Scholar]
- 27.Helgeson VS, Cohen S, Schulz R, Yasko J. Education and peer discussion group interventions and adjustment to breast cancer. Arch Gen Psychiatr. 1999;56:340–7. doi: 10.1001/archpsyc.56.4.340. [DOI] [PubMed] [Google Scholar]