Abstract
While obesity has been increasing in the United States, little is known about the variation in recent BMI and waist circumference (WC) distribution shifts across socio-demographic groups. We assessed shifts in BMI and WC distributions and compared between-group differences over the past decade, and projected future BMI and WC distributions and prevalence of obesity and central obesity using National Health and Nutrition Examination Survey (NHANES) 1988–1994 and 1999–2004 data. BMI/WC distributional shifts overall and in percentiles were compared across groups. Average yearly shift was calculated and used for projecting future distributions and prevalence. Both BMI and WC increased more in their uppermost percentile distribution, though BMI shift declined toward the uppermost percentiles among women. Heavier Americans gained more adiposity over the past decade. Ethnic (non-Hispanic (NH) white vs. black) disparities in mean BMI and WC became wider. Over the survey period, mean BMI increased by 1.3 units vs. 1.8 units among men and women, whereas WC, by 4.2 cm vs. 4.8 cm. Young adults had the largest increase. Shift in women’s WC was stable between the 25th and 75th percentiles, but gained pace at higher WC, while women’s BMI and men’s BMI and WC shifts increased linearly. NH black women had the largest shifts and would have central obesity and obesity prevalence of 90.8 and 70.7% by 2020. Shifts in BMI and WC distribution varied across age-, gender-, and ethnic groups. Future rise in the obesity and central obesity prevalence rates are expected, but would vary by demographic groups.
INTRODUCTION
Over the past few decades, the United States has witnessed a marked increase in its obesity prevalence, which has doubled since the 1980s. There are large disparities across population groups in terms of age, gender, race/ethnicity, and socio-economic status (1). The World Health Organization currently defines overweight and obesity with BMI (weight (kg)/height(m)2) cut points of 25 and 30, respectively (2, 3). These were recommended by a National Heart, Lung, and Blood Institute’s and North American Association for the Study of Obesity expert committee (4). The National Heart, Lung, and Blood Institute’s/North American Association for the Study of Obesity committee also recommends using waist circumference (WC) cut points of 40 inches (102 cm) in men and 35 inches (88 cm) in women to define “central obesity.” Increasingly, research shows that WC or central obesity is a better predictor of chronic diseases, mainly type 2 diabetes, hypertension and dyslipidemias, than overall adiposity assessed using BMI (5,6). WC may be equally or more useful than BMI due to its higher predictive value for future health risks, ease of measurement, and understanding by the general public (4–6).
The question remains unanswered as to whether shifts in BMI and WC over the past two decades in the United States have been occurring at equal rate across distributions of both measures and whether they varied by gender and ethnicity. It has been suggested that the increase in BMI has been concentrated in higher weight groups based on a recent study (7), a finding with great public health implications in terms of rising health-care and quality-of-life costs (8,9). While trends in mean BMI and obesity prevalence (1,10–17) and mean WC and prevalence of central obesity (18–23) have been recently studied in the United States and other countries, none have looked at simultaneous distributional shifts (in terms of percentiles) across time in BMI and WC or have attempted to use those findings to make future projections. In addition, to date, no study has examined those shifts closely across race/ethnicity groups. Previously, one study assessed distributional shifts in terms of percentiles of BMI up to 1994 in the United States (7), while another compared BMI and WC shifts using a similar methodology in the United Kingdom (24).
This study uses the most recent US nationally representative cross-sectional data and earlier data to assess the shifts in BMI and WC distributions and compare the ethnic- and gender differences in the shifts. In addition, based on these shifts and several assumptions, we projected the future BMI and WC distribution as well as the obesity and central obesity prevalence for each gender–ethnic group.
METHODS AND PROCEDURES
Databases
The National Health and Nutrition Survey (NHANES) database include a series of cross-sectional surveys initiated in the 1960s that provided nationally representative information on the nutrition and health status of the US civilian population. We used two series of NHANES data collected during periods of 1988–1994 (III) and 1999–2004. In this analysis, we opted not to include earlier waves of NHANES as our goal was to examine the shifts over the recent two decades, and these more recent data may be better to help predict future trends. Our analyses were limited to participants aged ≥20 years old.
NHANES III (1988–1994)
NHANES III is a survey that was carried out between 1988 and 1994 using a multistage, stratified sampling design. The survey oversampled older adults (60 years or more) and minority groups (nonHispanic (NH) black and Mexican Americans (MA)). Sampled individuals were first interviewed at home and then invited to a mobile examination center to undergo body measurements, clinical evaluations, and laboratory testing. Anthropometric measurements were performed on all study participants using standardized methods and equipment. BMI was computed based on measured weight and height. Weight was measured on a Toledo self-zoning weight scale while participants wore light clothing provided by mobile examination center. Height was measured with a stadiometer to the nearest millimeter. As for WC, it was measured in a standard manner using a steel measuring tape to the nearest 0.1 cm. positioning it at the high point of the ilium where it crosses the midaxillary line (25–28).
NHANES (1999–2004)
Since 1999, NHANES has been a continuous annual survey. The data were recently made available for the first 6 years of the period 1999–2004. Three bi-annual waves of NHANES (1999–2000, 2001–2002, and 2003–2004) were combined to enhance statistical power and obtain a more accurate picture of the current situation. Similar to NHANES III, sampling design was stratified multistage with oversampling of older adults and minorities. In addition, the low income population was also oversampled. Home interviews were followed by a mobile examination center examination, where follow-up questionnaires, various clinical and body measurements were conducted and blood samples were drawn. Using standardized methods and equipments, anthropometric measurements including weight, height, and WC were performed similarly to those in NHANES III (29,30).
Classification of obesity and central obesity
Obesity was defined as BMI ≥30 kg/m2 and central obesity with WC ≥102 cm or 40 inches for men, and ≥88 cm or 36 inches for women (1).
Covariates
The socio-demographic variables included in our analysis were age, gender, and race/ethnicity. The latter was categorized as NH whites, NH blacks and MA, and “other ethnicity.”
Study population
After excluding pregnant women and subjects below 20 years of age, the final sample sizes for our analyses were 16,581 for NHANES III (population estimates: 50.0% men; 76.6% NH whites, 10.7% NH blacks, 4.9% MA, and 7.8% other ethnicity) and 15,332 for NHANES 1999–2004 (48.8% men; 11.0% NH black, 7.2% MA, and 9.6% other ethnicity). Out of those, 14,544 in NHANES III had both BMI and WC data, while 12,614 in NHANES 1999–2004 had these complete data (i.e., 12–14% of eligible sample had missing data).
Data analysis
Means with s.e. of BMI and WC as well as prevalence of obesity and central obesity were computed after taking into account sampling design complexity for variance estimation and using appropriate weights to adjust for oversampling and to obtain nationally representative estimates. Differences in BMI and WC means between gender and race/ethnicity groups were tested using ANOVA and t -tests. Trends in mean BMI and WC were examined between NHANES III and 1999–2004 waves and significance of change was assessed based on overlap between 95% CI.
Shift in BMI and WC distributions
Overlayed distributions of BMI and WC for NHANES III and 1999–1904 were represented using kernel densities, which are nonparametric smoothed graphs that are independent of bin width when compared to histograms (31). Next, changes in percentile values of the distribution of BMI and WC at the two points in time (1988–1994 and 1999–2004) were analyzed graphically using a variation of the mean-difference plot (m-d) curves. While those curves traditionally are plots of the change in the percentile value between waves on the y-axis against the mean of the values from the two time periods (7,24), we chose to represent this graph as follows: On the x -axis, the actual percentile (e.g., 25th) was plotted against the yearly average absolute shift in the BMI or WC value on the y-axis. The average yearly shift was estimated using regression models, e.g., BMI = yearly shift × 10.5 years; 10.5 was the difference between the midpoints of year period). (See Equation 1).
Projections of future BMI/WC distribution and obesity/central obesity prevalence
Point estimates of the % yearly shifts in BMI and WC were used to conduct a simulation whereby data from NHANES 1999–2004 was used to project future changes in distributions based on past shift patterns (using Equation 2). To this end, average absolute yearly shifts were applied to all subjects in NHANES 1999–2004 based on their corresponding percentiles and new values of BMI/WC were estimated as projections for the years of 2010 and 2020. Assuming no changes in age, sex, and race/ethnicity distributions in the US population, means of BMI and WC and prevalence of obesity and central obesity were then projected. BMI and WC kernel density smoothed graphs were also created (not presented). Because of the small sample size, we chose not report the results for the “other ethnicity” group. j = percentile, t = wave midpoint time, Yj,t: mean value of period-specific
percentile for BMI/WC. βj = absolute shift in BMI/WC for percentile j. Yi, j,t: projected value of BMI/WC for each subject i. Yi, j,0: baseline value of BMI/WC for each subject i. Δt = projection year - 2001.5.
All of our analyses, e.g., percentile estimates and kernel density graphs, took into account oversampling of population groups by including appropriate sampling weights. Primary sampling units and strata were also considered when computing means of BMI and WC. All analyses were conducted using STATA version 9.0 (Stata, College Station, TX).
RESULTS
Ten-year trends in mean BMI and WC: by gender and race/ethnicity
Mean values of BMI and WC by gender, age, and race/ethnicity as well as shifts in means over the 10-year period are presented in Table 1. Over this period, mean BMI increased by 1.3 units among men and 1.8 units among women. Average WC increased substantially; by 4.2 cm. among men and 4.8 cm. among women. Both mean shifts were statistically significant. While BMI in NHANES III was significantly higher among men, the reverse pattern was observed in 1999–2004. Mean WC was significantly higher among men and the gender gap has become wider with time (6.7 cm vs. 8.1 cm. difference). In both waves, mean BMI increased linearly with age particularly between the age groups 20–29 and 50–59 for NHANES III, and 20–29 to 60–69 for NHANES 1999–2004, but dropped among the very old (70+). A similar pattern was observed for WC.
Table 1.
Shifts in the distribution of body mass index and waist circumference between NHANES III (1988–1994) and 1999–2004, by gender age and race/ethnicity
| BMI (kg/m2) (mean ± s.e.)
|
WC (cm) (mean ± s.e.)
|
|||||
|---|---|---|---|---|---|---|
| NHANES III (1988–1994) | NHANES 1999–2004 | Change | NHANES III (1988–1994) | NHANES 1999–2004 | Change | |
| Gender | ||||||
| Men | 26.6 ± 0.1* | 27.9 ± 0.1* | 1.3** | 95.3 ± 0.3* | 99.5 ± 0.2* | 4.2** |
| Women | 26.4 ± 0.2 | 28.2 ± 0.1 | 1.8** | 88.6 ± 0.4 | 93.4 ± 0.4 | 4.8** |
| Both genders | ||||||
| Age (years) | ||||||
| 20–29 | 24.7 ± 0.2* | 26.7 ± 0.2* | 2.0** | 84.2 ± 0.3* | 90.9 ± 0.4 | 6.7** |
| 30–39 | 26.3 ± 0.2 | 27.8 ± 0.2 | 1.5** | 90.0 ± 0.5 | 93.9 ± 0.5 | 3.9** |
| 40–49 | 27.1 ± 0.2 | 28.6 ± 0.2 | 1.5** | 93.7 ± 0.5 | 97.2 ± 0.4 | 3.5** |
| 50–59 | 28.0 ± 0.2 | 29.0 ± 0.2 | 1.0 | 97.3 ± 0.5 | 99.5 ± 0.5 | 2.2** |
| 60–69 | 27.4 ± 0.2 | 29.2 ± 0.1 | 1.8** | 97.8 ± 0.4 | 101.7 ± 0.4 | 3.9** |
| 70+ | 26.4 ± 0.1 | 27.3 ± 0.1 | 0.9** | 95.8 ± 0.3 | 98.6 ± 0.2 | 2.8** |
| Race/ethnicity | ||||||
| NH white | 26.3 ± 0.1* | 27.9 ± 0.1* | 1.6** | 92.1 ± 0.3* | 96.7 ± 0.3* | 4.6** |
| NH black | 27.6 ± 0.2 | 29.7 ± 0.2 | 2.0** | 92.3 ± 0.3 | 97.2 ± 0.4 | 4.9** |
| Mex Am | 27.4 ± 0.1 | 28.4 ± 0.2 | 1.1** | 92.5 ± 0.3 | 95.5 ± 0.7 | 3.2** |
| Other | 25.8 ± 0.3 | 27.1 ± 0.3 | 1.4** | 89.0 ± 1.0 | 92.5 ± 0.8 | 3.8** |
| Men | ||||||
| Age (years) | ||||||
| 20–29 | 25.2 ± 0.2* | 26.7 ± 0.2* | 1.5** | 87.8 ± 0.4* | 93.1 ± 0.5* | 5.3** |
| 30–39 | 26.5 ± 0.2 | 27.6 ± 0.2 | 1.1** | 93.6 ± 0.6 | 96.7 ± 0.6 | 3.1** |
| 40–49 | 27.3 ± 0.2 | 28.4 ± 0.2 | 1.1** | 97.7 ± 0.5 | 100.9 ± 0.5 | 3.2** |
| 50–59 | 27.8 ± 0.2 | 28.7 ± 0.2 | 0.9** | 100.5 ± 0.5 | 103.0 ± 0.6 | 2.5** |
| 60–69 | 27.4 ± 0.2 | 29.0 ± 0.2 | 1.6** | 101.7 ± 0.5 | 105.9 ± 0.5 | 4.2** |
| 70+ | 26.3 ± 0.2 | 27.2 ± 0.1 | 0.9** | 99.3 ± 0.5 | 102.7 ± 0.4 | 3.4** |
| Race/ethnicity | ||||||
| NH white | 26.7 ± 0.1* | 28.1 ± 0.1* | 1.4** | 96.3 ± 0.3* | 100.9 ± 0.3* | 4.6** |
| NH black | 26.5 ± 0.1 | 27.8 ± 0.2 | 1.3** | 91.9 ± 0.3 | 95.7 ± 0.5 | 3.8** |
| Mex Am | 26.8 ± 0.1 | 27.9 ± 0.2 | 1.1** | 93.5 ± 0.5 | 96.9 ± 0.6 | 3.4** |
| Other | 25.5 ± 0.3 | 26.9 ± 0.3 | 1.4** | 90.7 ± 1.3 | 94.8 ± 0.9 | 4.1** |
| Women | ||||||
| Age (years) | ||||||
| 20–29 | 24.2 ± 0.2* | 26.6 ± 0.2 | 2.4** | 80.2 ± 0.6* | 87.5 ± 0.7* | 7.3** |
| 30–39 | 26.2 ± 0.3 | 27.9 ± 0.3 | 1.8** | 86.4 ± 0.8 | 90.7 ± 0.7 | 4.3** |
| 40–49 | 27.0 ± 0.3 | 28.8 ± 0.3 | 1.8** | 89.6 ± 0.8 | 93.6 ± 0.7 | 4.0** |
| 50–59 | 28.3 ± 0.3 | 29.2 ± 0.3 | 0.9** | 94.2 ± 0.8 | 96.1 ± 0.8 | 1.9** |
| 60–69 | 27.4 ± 0.2 | 29.3 ± 0.2 | 1.9** | 94.5 ± 0.5 | 98.0 ± 0.5 | 3.5** |
| 70+ | 26.4 ± 0.2 | 27.4 ± 0.2 | 1.0** | 93.3 ± 0.5 | 95.7 ± 0.4 | 2.4** |
| Race/ethnicity | ||||||
| NH white | 26.0 ± 0.2* | 27.7 ± 0.2* | 1.7** | 88.0 ± 0.5* | 92.7 ± 0.5* | 4.7** |
| NH black | 28.6 ± 0.2 | 31.3 ± 0.2 | 2.7** | 92.6 ± 0.5 | 98.4 ± 0.5 | 5.8** |
| Mex Am | 28.1 ± 0.1 | 29.1 ± 0.3 | 1.0** | 91.1 ± 0.3 | 93.9 ± 0.8 | 2.8** |
| Other | 26.1 ± 0.5 | 27.3 ± 0.4 | 1.2** | 87.2 ± 1.2 | 90.5 ± 1.0 | 3.3** |
Mex Am, Mexican American; NH, non-Hispanic; NHANES, National Health and Nutrition Examination Survey; WC, waist circumference.
P < 0.05 for the null hypothesis that means of BMI/WC are equal between socio-demographic variable categories.
P < 0.05 for the null hypothesis that there is no significant change in BMI/WC means between NHANES III and 1999–2004.
In addition, the largest absolute increase in means of BMI and WC was consistently among the youngest adult group aged 20–29 (2.0 kg/m2 and 6.7 cm, respectively). Racial/ethnic disparities in mean BMI and WC have become wider over time particularly when comparing NH blacks to NH whites (e.g., 1.8 kg/m2 vs. 1.3 kg/m2 for BMI). When looking at men and women separately, absolute shifts in BMI and WC among men were consistently the largest among NH whites and “other” ethnic groups and among young adults (20–29 years) and those aged 60–69. They were the smallest among those aged 50–59 and MA. Among women, shifts in BMI and WC were by far the largest in young adults (20–29 years) and among NH blacks, and the smallest among MA and those aged 50–59 years.
Distribution shift patterns in BMI and WC: by gender and race/ethnicity
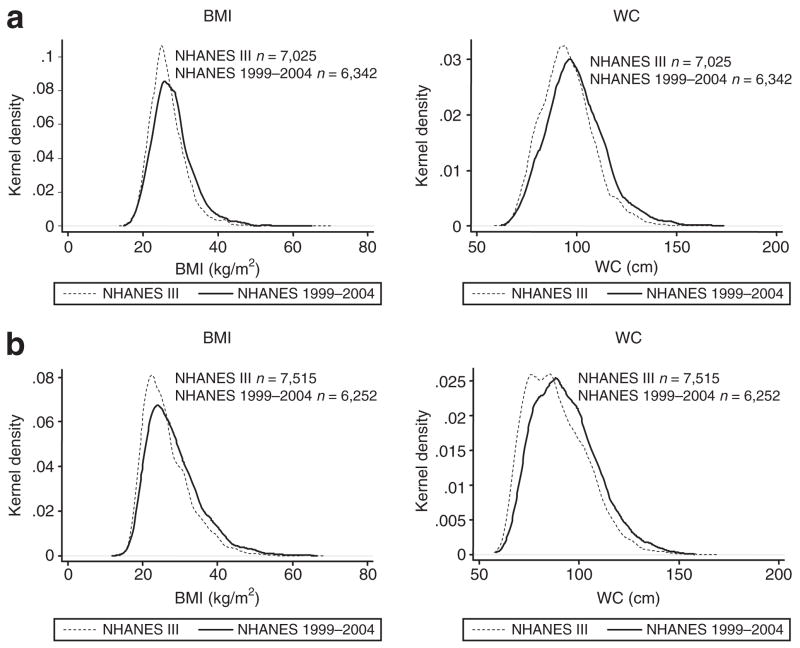
Figure 1 shows BMI and WC distribution curves and their shift patterns over time by gender. Among both genders, WC distribution appeared to shift at a relatively equal pace across all percentiles. However, unlike women, men experienced a lowering of the peaks in the bell-shaped distribution. In contrast, shifts in BMI were relatively faster at percentiles above the median compared to those below it, which may explain change in shape to a flatter distribution and the downward shift observed.
Figure 1.
BMI and waist circumference (WC) distribution shifts among US men and women between National Health and Nutrition Examination Survey (NHANES) III (1988–1994) and NHANES 1999–2004. (a) Men and (b) women.
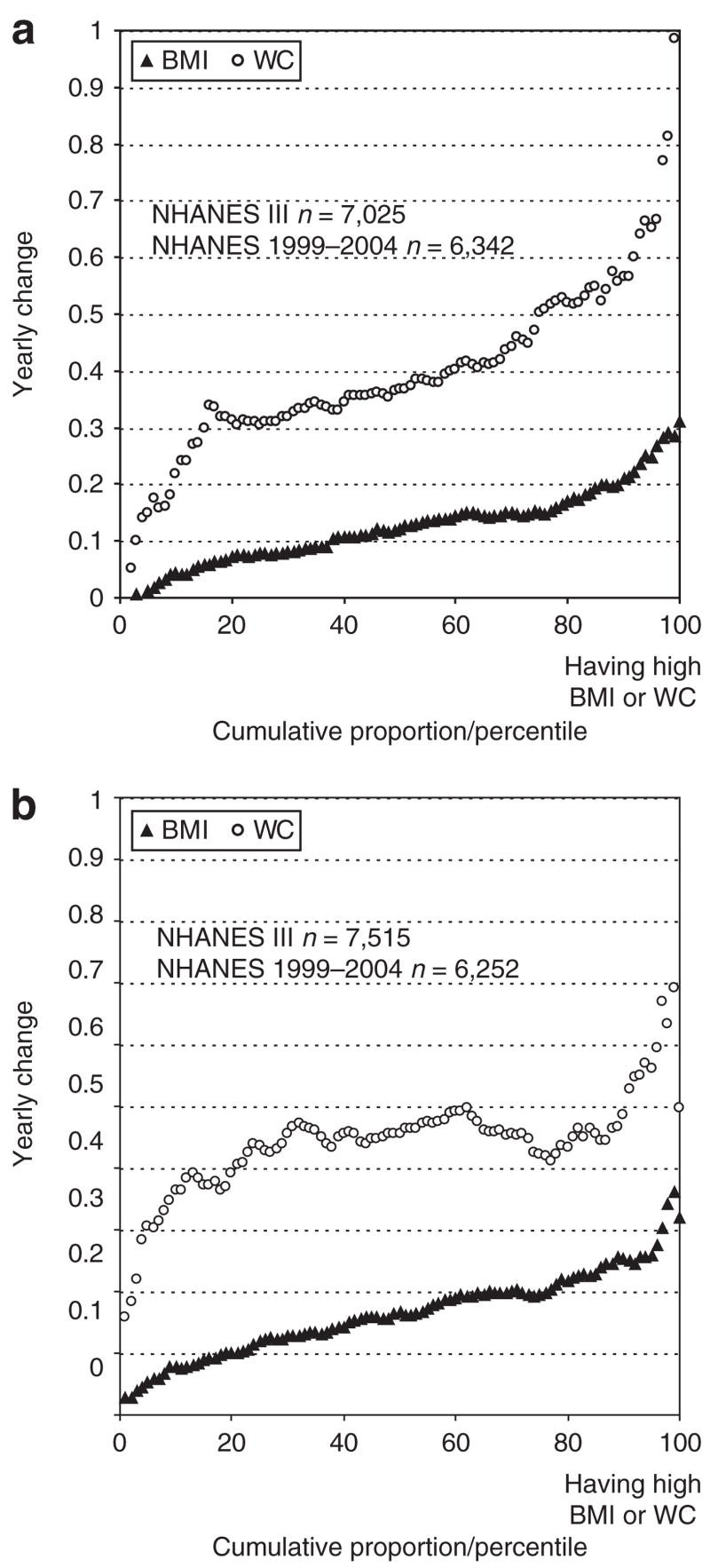
To study time shifts in BMI and WC distributions more closely, yearly changes in mean BMI and WC in each percentile group were plotted in an overlayed manner in Figure 2 through Figure 4. In the total population, while yearly shift in BMI varied from <0.1 kg/m2 at lower percentiles to around 0.4 kg/m2 at upper percentiles, WC yearly shifts in percentiles had a nonlinear pattern whereby they were stable between the 25th and 75th percentile at a value of 0.4 cm (data not shown). Gender differences in shift patterns were noted. In fact, the stable shift pattern of WC between the 25th and 75th percentile was only noted among women at an annual value of between 0.4 and 0.5 cm (Figure 2).
Figure 2.
Yearly average change in BMI (kg/m2) and waist circumference (WC, cm) across their distributions by gender: ordinary least square estimate of average yearly shift within percentile groups. (a) Men and (b) women. NHANES, National Health and Nutrition Examination Survey.
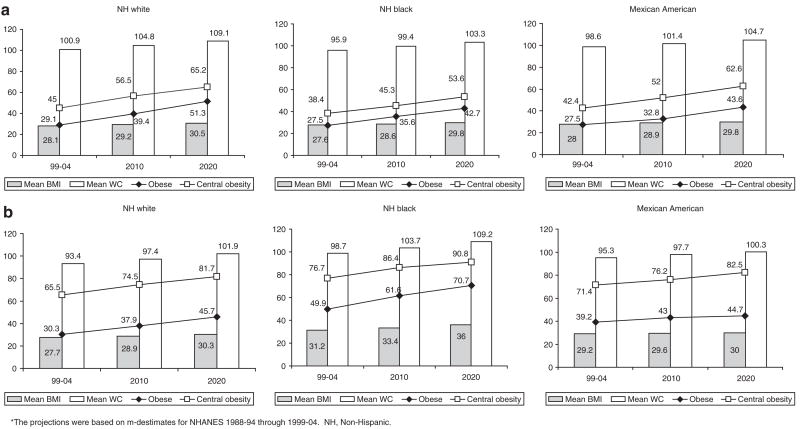
Figure 4.
Projected future mean BMI and waist circumference and the prevalence (%) of obesity and central obesity for 2010 and 2020 among US adults, by gender and race/ethnicity. (a) US men: NH white, NH black, MA and (b) US women: NH white, NH black, MA. The projections were based on mean-difference estimates for National Health and Nutrition Examination Survey (NHANES) 1988–1994 through 1999–2004. NH, Non-Hispanic; MA, Mexican American.
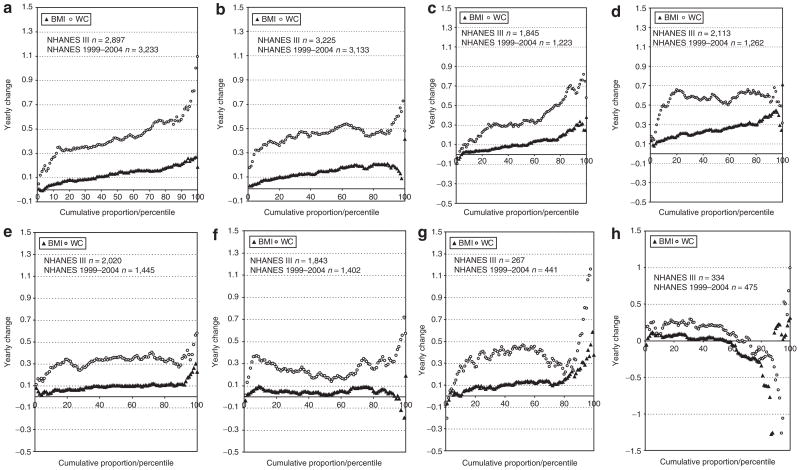
Examining shift patterns by race/ethnicity and gender (Figure 3), we found that shift acceleration in BMI at upper percentiles was noted among all ethnic groups and for both genders, except for MA and women of “other ethnicity.” However, yearly shifts in BMI among NH black women were significantly faster than those for WC. In addition, NH black women have shifted in WC at an elevated rate of 0.5 cm/year whenever their percentile ranking was above the 10th. Similarly they experienced a yearly shift in BMI of over 0.2 kg/m2 for the greatest part of their distribution (>30th percentile), compared to NH whites who only shifted to that value >70th percentile. This can be contrasted with shift patterns among MA men in whom WC and BMI seem to change over time with equal amounts across all percentiles and at a faster pace in percentiles over the. Among MA women, the opposite pattern was observed whereby BMI percentiles >60th percentile appeared to decline in absolute value at least up till the 90th percentile. WC shifts among MA women had an irregular pattern of acceleration. Moreover, Figure 3 shows (in nearly all panels) that the percentile increases in BMI and WC are highest in the uppermost percentiles among men. However, among women, a declining shifts in BMI at the uppermost percentiles was noted for certain ethnic groups including the “other ethnicity” category.
Figure 3.
Yearly average change in BMI (kg/m2) and waist circumference (WC, cm) across their distributions by gender and race/ethnicity: ordinary least square estimate of average yearly shift within percentile groups. (a) Non-Hispanic (NH) white men, (b) NH white women, (c) NH black men, (d) NH black women, (e) Mexican-American (MA) men, (f) MA women, (g) Other ethnicity, men, and (h) Other ethnicity, women. Distribution shifts may be influenced by the smaller sample size available among “other” ethnic groups. NHANES, National Health and Nutrition Examination Survey.
Future projections: distributions and prevalence estimates
Figure 4 shows our future projections for 2010 and 2020. In men, by 2020 mean BMI will be the highest among NH white men, followed closely by NH blacks. However, prevalence of obesity and central obesity would be highest among NH white and MA men. Among women, mean BMI and WC, obesity and central obesity prevalence will be the highest among NH black women by 2020. The rates of increase in both obesity and central obesity would be the slowest among MA women. One salient pattern is that among women, only NH blacks would close the gap in prevalence of obesity and central obesity by 2020.
DISCUSSION
Our findings indicate that the rise in adiposity in the United States was unequally distributed across the population and that shifts across the spectrum of BMI and WC varied between race/ethnicity and gender groups. There are several patterns noted for the population-level changes in BMI and WC between the later 1980s and 2004. First, overall, both BMI and WC distribution appeared to shift (increase) faster in the upper end of the population distribution (i.e., those with high BMI and WC). In other words, heavier Americans had become heavier over time—“the fat becoming fatter,” though this varied by gender and ethnicity. Although yearly shifts in BMI and WC among men had a similar pattern of linear increase across percentiles, acceleration in WC shifts at upper percentiles was a more obvious pattern among women after leveling off between the 20th and 90th percentile (Figure 2). BMI appeared to change with greater amounts across all percentiles among NH black women compared to women of NH white ethnicity, though in both cases, the absolute yearly shift tended to decline in uppermost percentiles (>90th percentile). The same pattern of decline was observed among MA women and women of other “ethnic” groups. However, NH black women’s shifts in BMI before the 90th percentile were accelerating in a linear fashion with increased percentile ranking unlike WC which was stable across percentiles, leading to an apparent closure of the gap in upper percentiles between these two measures among this gender/ethnic group compared to NH white women (Figure 3d vs. Figure 3b).
Second, ethnic disparities in mean BMI and WC have become wider since 1988–1994 particularly when comparing NH blacks to NH whites. In addition, absolute shifts in means of BMI and WC were consistently the largest among NH black women and young women aged 20–29 years and the smallest among MA and older adults aged 50–59 years. In fact, among older subjects (50+), there was a clear discontinuity in the mean BMI shifts whereby those aged 60–69 experience the largest increase. This finding was also observed in a recent longitudinal study and may be related to the survival of heavier subjects over time who had higher access to Medicare services rather than a biological phenomenon (32).
Third, based on the trends observed in the past decade, WC is projected to become increasingly displaced to the right with no significant downward curve shift. In contrast, the BMI distribution is expected to become increasingly flat over time. Assuming little change in demographic composition for the United States in the next 15 years, we projected the future BMI and WC distribution and the prevalence of obesity and central obesity for each gender/ethnic group. We projected these prevalence rates would remain the highest among NH black women by the year 2020 (70.7 and 90.8%, respectively).
Two previous studies conducted among adults in the United States. (earlier NHANES 1976–1980 to 1988–1994) and the United Kingdom came to similar conclusions, a dissymmetric shift occurring in the overall distribution. Between 1976–1980 and 1988–1994, US adults’ BMI distribution has gained skewness with a greater shift in its upper part, but the authors did not examine WC (7). They argued that the patterns suggested a combination of both profound environmental determinants and a population with a high degree of susceptibility. A recent UK study shows marked shifts in both BMI and WC and a combination of overall upward increase and a rise in skewness, which was more pronounced among younger British adults. In particular, WC increased by >8 cm in 10 years in young women, ~0.8 cm/year (24). In our US study population, for all adults ages combined, the 90th percentile of WC increased at 0.5–0.7 cm/year, which is comparable to the UK study. Young US adults also experienced more sizeable shifts in mean WC compared to their older counterparts.
In addition to the overall BMI and WC shift patterns, the variation in the shifts across gender and race/ethnicity groups may provide hints about the causes of the obesity epidemic in the United States. Whereas genetic drifts are unlikely to occur within a decade, environmental and behavioral changes are more probable roots to this problem. It is possible, however, that differences in weight gain across race/ethnicity and gender groups are behavioral and environmental responses that are also dependent on genetic susceptibility. Gene–environment interaction model fits well to help explain human adiposity (33–35). Our findings suggest that, subjects who are genetically susceptible and belong to the upper percentiles of the distribution (BMI or WC) may be differentially affected by (or respond to) environmental changes that promote weight and adiposity and gain.
Our findings point to a gender–ethnicity interaction whereby environmental changes had similar effects in some cases and divergent effects in others on overall adiposity (BMI) and body fat distribution as WC indicates visceral fat. Among men, in general, shift patterns in BMI and WC were similar particularly among MA. In contrast, yearly BMI shifts among women had an upward trend with increasing percentiles, while WC patterns of shifts were constant at least between the 25th and 75th percentiles. NH black women had the highest yearly increase for both WC and BMI. However, their prevalence of obesity (BMI ≥ 30) appeared to increase at a faster pace than central obesity, indicating that environmental changes may affect weight gain to a larger extent than abdominal fat deposition. In all other groups, except for women of “other ethnicity,” comparable increases were noted for prevalence of obesity and central obesity.
The finding that the increase in overall and central adiposity has been mostly noted among young adults, particularly women, suggests that environmental changes have impacted more strongly on this demographic group in recent years, although this may also be due to their relatively lower initial prevalence. Lifestyles that are more likely to be adopted by young people include intake of high energy density foods and snacking habits, eating away-from-home and sedentary behaviors (e.g., computer games, internet, TV watching habits) are all possible mechanisms explaining age disparities.
This study has a number of strengths. First, it is based on a representative data of adults in the United States and our analysis corrected for design complexity and yielded national estimates. Second, it is the first study to examine shifts in both WC and BMI simultaneously in the United States and compare those shifts across gender, age, and race/ethnicity groups. Third, it is also the first to use past trends in distributional shifts in both anthropometric parameters to project future prevalence estimates for obesity and central obesity.
Our study also suffers from a few limitations. First, the trend analyses are based on two nationally representative cross- sectional surveys that were conducted independently 10.5 years apart. It is possible that minor differences in sampling design and shifts in population composition might have affected the estimated changes in BMI and WC. A recent descriptive report of longitudinal changes from US studies that included BMI and other measures of adiposity indicated that annual changes in BMI were greater within cohort studies initiated during the 1989–1996 period compared to another earlier national cohort study conducted between 1971–1975 and 1981–1984 (the NHANES-I follow-up study) (32). In other word, people of the same age gained more weight/BMI with age during more recent years than the past. On average, the later cohorts’ annual BMI gain was higher by 0.1 unit in white, and by 0.07–0.26 in African-American men and women for mid ages 32–77 years than the NHANES-I follow-up study cohort. On average, the annual changes in BMI within each cohort examined ranged between -0.04 units (for white men aged 79 years at baseline) and 0.43 units (for black women aged 29 years at baseline), depending on baseline age within the cohort, gender, race/ethnicity, and the cohorts. In general, these values seemed to be comparable to our findings of BMI annual percentile shifts, which varied from <0.1 kg/m2 at lower percentiles to around 0.4 kg/m2 at upper percentiles. Second, our future projections of BMI and WC distribution and related obesity prevalence are based on the trends observed in the past and on an assumption of few future population composition changes. This is an oversimplified scenario because our analysis did not attempt to accurately predict the future situation and there are many uncertainties regarding the future population distribution and environmental and policy changes in the United States. On the other hand, our projected estimates are gender- and race/ethnicity specific, and thus have controlled partly for some possible population composition changes. Third, some of the shift patterns observed may be affected by smaller samples sizes for minority groups (e.g., women of “other ethnicity”) selected by NHANES, which were subject to large estimate errors or uncertainties.
Our findings have some important policy implications. One is that the national goals specified in Healthy People 2010 related to obesity cannot be met. These goals need be reassessed and reframed to be more realistic and may need to target the whole population rather than only the overweight groups. In addition, when setting the Healthy People 2020 goals, the differential shifts in adiposity measures across the population distribution need be considered; and more dramatic and effective national programs and policies are needed to help achieve the goals due to the multilevel nature of the obesity etiology (36–38). One of our recent studies shows that if the obesity increase trend in the United States is not controlled, it can have many serious public health and social consequences. For example, by 2048, the overall prevalence of overweight and obesity among American adults would approach 100% and the total health-care costs attributable to obesity and overweight would double every decade to 860.7–956.9 billion US dollars by 2030, accounting for 16–18% of total US health-care costs (39).
In conclusion, while overall, means of BMI and WC have increased significantly over time and are expected to do so for most socio-demographic groups in the United States, patterns of shifts in distribution differed between these two measures and across gender and ethnic groups. In most of these groups, it is clear that the heavy is becoming heavier though central adiposity (measured by WC) is increasing more rapidly at the uppermost percentiles, with a nonlinear shift pattern observed among women, and an absolute increase in WC leveling off at a high value for most of the distribution among NH black women. Broader and more comprehensive and vigorous prevention, screening, and treatment programs should be implemented to reverse the shifts in adiposity measures, we observed. Creative initiatives to impact environmental changes are needed. In addition, ethnic and gender disparities should be studied further to disentangle the biological from the environment components explaining those differences in distributional shifts.
Acknowledgments
The study was supported in part by research grants from the US Department of Agriculture (2044-05322), the National Institutes of Health (NIDDK R01 DK63383 and NICHD 1R03HD056073), and the Johns Hopkins Center for A Livable Center.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
References
- 1.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 2.WHO Expert Committee. Technical Report Series 54. WHO; Geneva: 1995. Physical status, the use and interpretation of anthropometry. [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) Technical report series 894. WHO: Geneva; 2000. Obesity: preventing and managing the global epidemic: Report of a WHO consultation. [PubMed] [Google Scholar]
- 4.National Institute of Health (NIH) NH, Lung, and Blood Institute’s (NHLBI), North American Association for the Study of Obesity (NAASO) The practical guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. NIH; Bethesda, MD: 2000. [Google Scholar]
- 5.Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am J Clin Nutr. 2005;81:555–563. doi: 10.1093/ajcn/81.3.555. [DOI] [PubMed] [Google Scholar]
- 6.Zhu S, Heymsfield SB, Toyoshima H, et al. Race-ethnicity-specific waist circumference cutoffs for identifying cardiovascular disease risk factors. Am J Clin Nutr. 2005;81:409–415. doi: 10.1093/ajcn.81.2.409. [DOI] [PubMed] [Google Scholar]
- 7.Flegal KM, Troiano RP. Changes in the distribution of body mass index of adults and children in the US population. Int J Obes Relat Metab Disord. 2000;24:807–818. doi: 10.1038/sj.ijo.0801232. [DOI] [PubMed] [Google Scholar]
- 8.Daviglus ML, Liu K, Yan LL, et al. Body mass index in middle age and health-related quality of life in older age: the Chicago heart association detection project in industry study. Arch Intern Med. 2003;163:2448–2455. doi: 10.1001/archinte.163.20.2448. [DOI] [PubMed] [Google Scholar]
- 9.Daviglus ML, Liu K, Yan LL, et al. Relation of body mass index in young adulthood and middle age to Medicare expenditures in older age. JAMA. 2004;292:2743–2749. doi: 10.1001/jama.292.22.2743. [DOI] [PubMed] [Google Scholar]
- 10.Berg C, Rosengren A, Aires N, et al. Trends in overweight and obesity from 1985 to 2002 in Goteborg, West Sweden. Int J Obes (Lond) 2005;29:916–924. doi: 10.1038/sj.ijo.0802964. [DOI] [PubMed] [Google Scholar]
- 11.Galuska DA, Serdula M, Pamuk E, Siegel PZ, Byers T. Trends in overweight among US adults from 1987 to 1993: a multistate telephone survey. Am J Public Health. 1996;86:1729–1735. doi: 10.2105/ajph.86.12.1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lahti-Koski M, Vartiainen E, Mannisto S, Pietinen P. Age, education and occupation as determinants of trends in body mass index in Finland from 1982 to 1997. Int J Obes Relat Metab Disord. 2000;24:1669–1676. doi: 10.1038/sj.ijo.0801437. [DOI] [PubMed] [Google Scholar]
- 13.Lindstrom M, Isacsson SO, Merlo J. Increasing prevalence of overweight, obesity and physical inactivity: two population-based studies 1986 and 1994. Eur J Public Health. 2003;13:306–312. doi: 10.1093/eurpub/13.4.306. [DOI] [PubMed] [Google Scholar]
- 14.Mokdad AH, Serdula MK, Dietz WH, et al. The spread of the obesity epidemic in the United States, 1991–1998. JAMA. 1999;282:1519–1522. doi: 10.1001/jama.282.16.1519. [DOI] [PubMed] [Google Scholar]
- 15.Monteiro CA, MH DAB, Conde WL, Popkin BM. Shifting obesity trends in Brazil. Eur J Clin Nutr. 2000;54:342–346. doi: 10.1038/sj.ejcn.1600960. [DOI] [PubMed] [Google Scholar]
- 16.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 17.Rasmussen F, Johansson M, Hansen HO. Trends in overweight and obesity among 18-year-old males in Sweden between 1971 and 1995. Acta Paediatr. 1999;88:431–437. doi: 10.1080/08035259950169837. [DOI] [PubMed] [Google Scholar]
- 18.Elobeid MA, Desmond RA, Thomas O, Keith SW, Allison DB. Waist circumference values are increasing beyond those expected from BMI increases. Obesity (Silver Spring) 2007;15:2380–2383. doi: 10.1038/oby.2007.282. [DOI] [PubMed] [Google Scholar]
- 19.Ford ES, Mokdad AH, Giles WH. Trends in waist circumference among U.S. adults. Obes Res. 2003;11:1223–1231. doi: 10.1038/oby.2003.168. [DOI] [PubMed] [Google Scholar]
- 20.Li C, Ford ES, McGuire LC, Mokdad AH. Increasing trends in waist circumference and abdominal obesity among US adults. Obesity (Silver Spring) 2007;15:216–224. doi: 10.1038/oby.2007.505. [DOI] [PubMed] [Google Scholar]
- 21.Okosun IS, Chandra KM, Boev A, et al. Abdominal adiposity in U.S. adults: prevalence and trends, 1960–2000. Prev Med. 2004;39:197–206. doi: 10.1016/j.ypmed.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 22.Okosun IS, Choi ST, Boltri JM, et al. Trends of abdominal adiposity in white, black, and Mexican-American adults, 1988 to 2000. Obes Res. 2003;11:1010–1017. doi: 10.1038/oby.2003.139. [DOI] [PubMed] [Google Scholar]
- 23.Visscher TL, Seidell JC. Time trends (1993–1997) and seasonal variation in body mass index and waist circumference in the Netherlands. Int J Obes Relat Metab Disord. 2004;28:1309–1316. doi: 10.1038/sj.ijo.0802761. [DOI] [PubMed] [Google Scholar]
- 24.Wardle J, Boniface D. Changes in the distributions of body mass index and waist circumference in English adults, 1993/1994 to 2002/2003. Int J Obes (Lond) 2008;32:527–532. doi: 10.1038/sj.ijo.0803740. [DOI] [PubMed] [Google Scholar]
- 25.Center for Disease Control and Prevention (CDC) The Third National Health and Nutrition Examination Survey (NHANES III 1988–94) Reference Manuals and Reports (CD-ROM) Centers for Disease Control and Prevention; Bethesda, MD: 1996. [Google Scholar]
- 26.Center for Disease Control and Prevention (CDC) National Health and Nutrition Examination Survey: Anthropometric measures. [Accessed 25 September 2006];2006 http://www.cdc.gov/nchs/data/nhanes/nhanes3/cdrom/nchs/manuals/anthro.pdf.
- 27.Centers for Disease Control (CDC) NHANES III anthropometric procedures video. [Accessed 25 September 2007]; http://www.cdc.gov/nchs/about/major/nhanes/avideo.htm.
- 28.Chumlea NC, Kuczmarski RJ. Using a bony landmark to measure waist circumference. J Am Diet Assoc. 1995;95:12. doi: 10.1016/s0002-8223(95)00003-8. [DOI] [PubMed] [Google Scholar]
- 29.Center for Disease Control and Prevention (CDC) National Health and Nutrition Examination Survey. [Accessed25 September 2006];2006 http://www.cdc.gov/nchs/nhanes.htm.
- 30.Center for Disease Control and Prevention (CDC) National Health and Nutrition Examination Survey: Anthropometric measures for 2003–04. [Accessed 25 September 2006];2006 http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/BM.pdf.
- 31.Scott DW, editor. Theory, Practice and Visualization. Wiley; New York: 1992. Multivariate Density Estimation. [Google Scholar]
- 32.Kahn HS, Cheng YJ. Longitudinal changes in BMI and in an index estimating excess lipids among white and black adults in the United States. Int J Obes (Lond) 2008;32:136–143. doi: 10.1038/sj.ijo.0803697. [DOI] [PubMed] [Google Scholar]
- 33.Barsh GS, Farooqi IS, O’Rahilly S. Genetics of body-weight regulation. Nature. 2000;404:644–651. doi: 10.1038/35007519. [DOI] [PubMed] [Google Scholar]
- 34.Challis BG, Yeo GS. Past, present and future strategies to study the genetics of body weight regulation. Brief Funct Genomic Proteomic. 2002;1:290–304. doi: 10.1093/bfgp/1.3.290. [DOI] [PubMed] [Google Scholar]
- 35.Horwitz BA. Introduction: physiology, pathophysiology, and genetics of body weight/adiposity regulation. Exp Biol Med (Maywood) 2001;226:961–962. doi: 10.1177/153537020122601101. [DOI] [PubMed] [Google Scholar]
- 36.Bray G, Bouchard C, James WPT. Handbook of Obesity: Clinical Applications. 2. Marcel Dekker; New York: 1998. [Google Scholar]
- 37.Kumanyika SK, Obarzanek E. Pathways to obesity prevention: report of a National Institutes of Health workshop. Obes Res. 2003;11:1263–1274. doi: 10.1038/oby.2003.172. [DOI] [PubMed] [Google Scholar]
- 38.US Department of Health and Human Services PHS. The Surgeon General’s Call To Action To Prevent and Decrease Overweight and Obesity. Office of the Surgeon General; Rockville, MD: 2001. [PubMed] [Google Scholar]
- 39.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. [e-pub ahead of print 24 July 2008];Obesity. 2008 doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]