Abstract
Foxp3 expressing CD4+CD25+ regulatory T cells (Tregs) have been shown to prevent allograft rejection in clinical and animal models of transplantation. However, the role of Foxp3 in regulating Treg function, and the kinetics and mechanism of action of Tregs in inducing allograft tolerance in transplantation, are still not fully understood. Thus, we investigated the kinetics and function of Tregs in a mouse model of orthotopic corneal transplantation, the most common form of tissue grafting worldwide. Here using in-vitro functional assays and in-vivo Treg adoptive transfer assays, we show that far more relevant than Treg frequency is their level of Foxp3 expression, which is directly associated with the potential of Tregs to prevent allograft rejection by producing regulatory cytokines and suppressing effector T cell activation. In addition, our data clearly demonstrate that Tregs primarily suppress the induction of alloimmunity in regional draining lymph nodes, rather than suppressing the effector phase of the immune response in the periphery. These findings provide new insights on Treg dynamics in transplantation which are crucial for designing therapeutic strategies to modulate Treg function, and to optimize Treg-based cell therapies for clinical translation.
Keywords: Regulatory T cells, Foxp3, Tolerance, Transplantation, Cornea
INTRODUCTION
Immune-mediated rejection remains the single most important cause of graft failure in all forms of tissue transplantation. However, spontaneous development of transplant tolerance in some recipients indicates that just as rejection is mediated by active immune-mediated events, graft acceptance is also sustained by active immunoregulatory mechanisms. One such immune mechanism is mediated by regulatory T cells that have the capacity to suppress host immunity against transplants. Amongst the various forms of regulatory T cells, CD4+CD25+ regulatory T cells (Tregs), which constitute 5-10% of CD4+ T cells, play a central role in inducing and maintaining tolerance to both self- and allo-antigens (1-3).
Tregs are exemplified by their expression of transcription factor Foxp3 (4) and have been reported in a number of clinical and animal models of transplantation (5-8). Despite significant advances in understanding Treg biology, several aspects relevant to transplant settings remain unclear. The majority of previous reports have associated the outcome of the allograft primarily with changes in the frequency of Tregs, either in the lymphoid compartment or at the graft site (9,10). Moreover, levels of Foxp3 expression have been interpreted primarily to reflect Treg frequency rather than defining the regulatory functions of these cells (11-15), although it has been shown that Foxp3 is critically important for both the development of Tregs as well as their suppressor function (16,17). Thus, understanding the significance of Foxp3 expression per se to analyze Treg function, and the dynamics of Treg-mediated tolerance in transplantation may afford new opportunities to harness the potential of these cells to promote tolerance.
We herein investigated the kinetics and function of Tregs in allograft-acceptors and rejectors using a well-characterized mouse model of corneal transplantation (18-20). In this model approximately 50% of allografts are rejected within 3 weeks of transplantation while the remaining half enjoy indefinite survival, indicating involvement of active regulatory mechanisms that promote allograft longevity. Compared to other transplant systems (e.g. skin, heart, kidney, etc.) where a 100% graft rejection rate is observed in unmanipulated recipients, this model provides an exceptional opportunity to study why some of the allografts are spontaneously accepted and to evaluate the role of Tregs in this high frequency of transplant survival.
In the present study, we clearly demonstrate that contrary to previous reports the functional status of Tregs is more reflective of allograft outcome than their numbers. Moreover, the levels of Foxp3 expression in Tregs are directly associated with their potential to suppress T cell activation and prevent allograft rejections.
MATERIALS AND METHODS
Mice
Eight-to 10-wk-old BALB/c (H-2d), C57BL/6 (H-2b), and C3H (H-2k) male mice were purchased from Taconic Farms (Germantown, NY), and used as recipients, donors and third-party controls, respectively. The study was approved by the Institutional Animal Care and Use Committee, and the mice were treated according to the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research.
Corneal transplantation
Standard protocol for murine orthotopic corneal transplantation was used, as described previously (18,20). Briefly, donor center corneas (2 mm diameter) were excised from C57BL/6 mice and sutured on to the recipient graft beds prepared by excising a 1.5-mm site in the central cornea of BALB/c mice. Simultaneously, some BALB/c mice received syngeneic (BALB/c) grafts to control for the non-allospecific effects of surgery. The corneal sutures were removed 7 days after surgery. All grafts were evaluated using slit-lamp biomicroscopy at weekly intervals. Grafts were defined as rejected when they became opaque and the iris details could not be recognized clearly using a standardized opacity grading (ranges, 0-5) scheme. This model renders an easy and confirmatory method to directly evaluate graft endpoints in vivo at different time points without sacrificing the animals, which makes it an outstanding system to study immune responses in the transplant setting.
Flow cytometry
Ipsilateral draining submandibular and cervical LNs as well as grafted corneas were harvested and single-cell suspensions were prepared. Single-cell suspensions of corneal samples were prepared by collagenase digestion, as previously described (19). The isolated cells were stained with the following Abs: Anti-CD4/CD3 FITC, anti-CD25 PE and anti-FoxP3 PECy5 (eBioscience) and analyzed on an EPICS XL flow cytometer (Beckman Coulter).
Cell sorting
CD4+ T cells and CD4+CD25+ Tregs from the lymph nodes of naïve and/or different graft recipients were isolated by magnetic separation using CD4+ T cell and regulatory T cell isolation kits (Miltenyi Biotec). Purity of sorted cells was > 97%, and 95% of CD4+CD25+ Tregs were Foxp3+ in all the groups as confirmed by flow cytometry.
Real-time PCR
RNA was isolated with RNeasy Micro Kit (Qiagen) and reverse transcribed using Superscript III Kit (Invitrogen Life Technologies). Real-time PCR was performed using Taqman Universal PCR Mastermix and preformulated primers for FoxP3 (assay ID Mm00475156_ml) and GAPDH (assay ID Mm99999915_gl) (Applied Biosystems). The results were analyzed by the comparative threshold cycle method and normalized by GAPDH as an internal control.
Western blot
Tregs (n=5×105) isolated from the LN of allograft acceptors and rejectors were dissolved in lysis buffer. The protein concentrations in cell lysates were determined using BCA reagent (Thermo Scientific). Equal amounts of protein were boiled in an equal volume of Laemmli sample buffer, and resolved by 10% SDS-PAGE. Proteins were then transferred to PVDF membrane (ImmobilonTM Millipore, Billerica, MA) and probed overnight with primary anti-Foxp3 antibody (Santa Cruz Biotechnology, Inc) or anti-β-actin antibody (abcam). Immunoreactive bands were detected with horseradish peroxidase-conjugated secondary antibodies and visualized by enhanced chemiluminescence. The intensities of immunoreactive bands were analyzed using NIH-ImageJ software.
Suppression assay
For all the suppression assays, including cytokine and transwell assays, CD4+ T effectors (Teff, total CD4+ cells without depleting the CD25+ population) and Tregs were isolated from the draining lymph nodes. Teff cells (1×105) were cocultured with Tregs (5×104), T cell-depleted syngeneic splenocytes (1×105) and 1 μg/ml anti-CD3 antibody for 3 days. Proliferation of CD3 stimulated Teff cell without adding Tregs was considered as control proliferation with 0% suppression. Proliferation was measured using the BrdU incorporation assay (Millipore) and percent suppression was calculated using the following formula: % suppression = [(Teff proliferation without Tregs - Teff proliferation with Tregs) / Teff proliferation without Tregs] x 100. To measure the allo-specificity of Tregs, Teff and Tregs were co-cultured with T cell-depleted allogeneic splenocytes of C57BL/6 or C3H mice without anti-CD3 stimulation. Transwell experiments were performed in 24-well plates using transwell cell culture inserts (1.0 μm, BD Bioscience). Naïve Teff cells were cultured with T cell-depleted syngeneic splenocytes and anti-CD3 antibody, and Tregs were either added directly to the culture or were placed in transwell inserts.
Cytokine assay
Cytokine levels in the supernatants of suppression assays were analyzed using commercially available ELISA kits for murine TGF-β1 and IL-10 (eBiosciences).
Adoptive transfer of Tregs to allograft recipients
First, Tregs were isolated from the draining LN of syngeneically grafted recipients, allograft acceptors and rejectors at week 3 post-transplantation. Subsequently, these Tregs (1×105 cells per mouse) were transferred intravenously to three different groups of allograft recipients at 18h post-surgery. This time-point for Treg transfer was selected on the basis of our previous observation of detecting considerable numbers of graft derived APCs in the draining lymph nodes of recipients at 24h post-transplantation (18). Allograft survival rate in each group (n = 6 per group) was monitored up to 8 week post-transplantation.
Statistical analysis
Student’s t test was used for comparison of mean between the groups. Kaplan-Meier analysis was adopted to construct survival curves, and the log-rank test was used to compare the rates of corneal graft survival. Data are presented as mean ± SEM and considered significant at P<0.05.
RESULTS
Tregs in the draining LN express different levels of Foxp3
Regional draining lymph nodes (LN) and grafted corneas were harvested from graft recipients at weekly intervals up to week-4 post-transplantation. At week 3 post-transplantation, allograft recipients were separated into acceptors and rejectors. The flow cytometric analysis of draining LN cell suspensions showed no difference in the frequencies of CD4+CD25+Foxp3+ Tregs, either as a proportion of the total CD4+ T cells (range: 8.5-10.5%) or of the total LN cells (range: 4-5%) among syngeneic recipients, acceptors, and rejectors, at any of the time points (Fig 1a and 1b). Interestingly, in contrast to the Treg frequencies, we observed considerable differences in the levels (mean fluorescence intensity: MFI) of Foxp3 by the Tregs of different groups (Fig 1c). The MFI of Foxp3 in Tregs of allograft acceptors were approximately 50% higher compared to those in the Tregs of allograft rejectors and syngeneic recipients. Additionally, to confirm these differences in the Foxp3 expression levels, we investigated Foxp3 protein levels by western blot in sorted Tregs and mRNA levels by real time PCR in the draining LN as well as in equal number of sorted Tregs of different graft recipient groups. The densities of immunoreactive Foxp3 bands (normalized to densities of β-actin) show that acceptor-Tregs express 2-fold higher Foxp3 protein compared to those by rejector-Tregs (Fig 1c). Similarly, there was a ∼2-fold increase in Foxp3 mRNA expression in the LN of acceptors as compared to those of rejectors at week 3 post-transplantation and thereafter. In addition, the levels of Foxp3 mRNA expression in the LN of rejectors were lower than those of syngeneic recipients, which nearly remained unchanged from baseline levels (Fig. 1d). Similar to the Foxp3 mRNA expression in total LN, the isolated Tregs from the LN of acceptors expressed 2-fold higher levels of Foxp3 mRNA compared to those from the LN of rejectors (Fig. 1e) confirming that Tregs in allograft acceptor express high levels of Foxp3.
FIGURE 1. Kinetics of Treg frequency and Foxp3 expression in syngeneically grafted recipients (Balb/c→Balb/c) and fully disparate allograft (C57Bl/6→Balb/c) acceptors and rejectors.
(a) FACS analysis of draining lymph nodes (LN) cell suspension showing frequencies of CD4+CD25+Foxp3+ Tregs at week-3 post transplantation. (b) Frequencies of Tregs out of CD4+ and total LN cells at weekly intervals from Day 0 to week 4 post-transplantation. (c) Mean fluorescence intensity and western blot analyses showing expression levels of Foxp3 protein in purified Tregs isolated from the LN at wk-3 post-transplantation (*p = 0.036). (d) Real-time PCR analysis of Foxp3 mRNA expression levels in total LN cells at weekly intervals from Day 0 to week 4 post-transplantation (acceptor vs. syngeneic and rejector at wk-3 *p = 0.034 and 0.027; and at wk-4 ‡p = 0.01 and 0.001); and (e) in equivalent numbers of purified Tregs sorted from the LN at week-3 post transplantation (*p = 0.026). (f) Frequencies of corneal graft-infiltrating Foxp3+ Tregs and total CD3+ T cells and (g) MFI of Foxp3 levels in graft-infiltrating Tregs. (h) Real-time PCR analysis of Foxp3 mRNA expression in the grafted corneas of syngeneically graft recipients, allograft acceptors and allograft rejectors at week 3 post-transplantation (*p = 0.037). Each transplant group consists of 4-6 recipient mice and data present the mean ± SEM of three independent experiments. Statistical significance for mRNA and MFI levels is calculated on fold-change values over those of syngeneic or naïve-Tregs. P values are calculated using student’s t-test.
In addition, we wanted to determine whether Tregs migrate to the graft site and, similar to LN-Tregs, express different levels of Foxp3 in accepted versus rejected allografts. The relative frequencies of Foxp3+ Tregs (11-13%) in relation to the total infiltrating T cells (Fig. 1f) as well as expression levels of Foxp3 (MFI: 33-36) in Tregs (Fig. 1g) remained same among the three groups. However, the expression of Foxp3 mRNA was ∼ 2-fold higher in corneas with rejected grafts than those with accepted grafts (Fig. 1h). This higher expression of Foxp3 in rejected grafts was principally due to the nearly ∼2-fold increase in the frequencies of infiltrating T cells (and hence also Tregs) in the corneas with rejected as compared to accepted allografts (Fig. 1f).
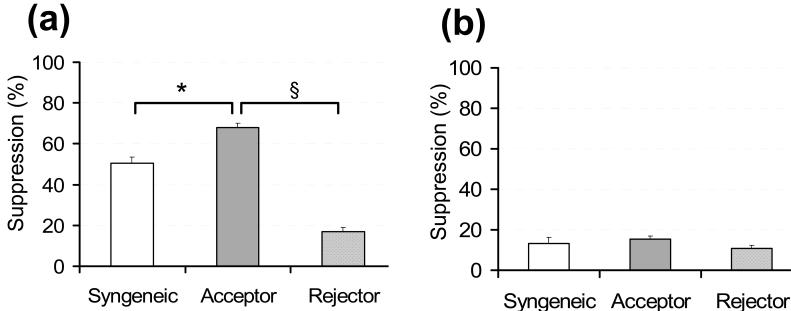
Tregs of allograft acceptors are highly effective in suppressing naïve, but not allo-primed, T cell activation
Using a co-culture suppression assay system, we investigated the regulatory potential of Tregs to suppress the proliferation of CD3 antibody-stimulated naïve T cells (isolated from the LN of naïve BALB/c mice) and allo-primed T cells (isolated from the LN of allograft rejectors). Tregs isolated from the LN of acceptors (acceptor-Tregs) were significantly more effective in suppressing the proliferation of naïve T cells compared to those isolated from the LN of rejectors (rejector-Tregs) and syngeneic recipients (syngeneic-Tregs). Rejector-Tregs were even less effective in suppressing the T cell proliferation than syngeneic-Tregs (Fig. 2a). However in contrast to suppression of naïve T cell activation, Tregs of all the groups failed to efficiently suppress the proliferation of allo-primed effector T cells (Fig. 2b).
FIGURE 2. Suppressor potential of Tregs.
(a) Naïve CD4+T cells isolated from the LN of unprimed BALB/c recipients and (b) allo-primed CD4+T cells isolated from the LN of allograft rejectors were stimulated with CD3-antibody for 3 days in the presence of different Tregs isolated from the LN of syngeneically grafted recipients, allograft acceptors, and allograft rejectors at week 3 post-transplantation. The activity of Tregs is measured at Treg:Teff cell ratio of 1:2. Proliferation was measured using the BrdU incorporation assay and compared with the proliferative responses of respective CD3-stimulated naïve or allo-primed T cell in the absence of Tregs and % suppression was calculated as described in Materials and Methods. Each transplant group consists of 4-6 recipient mice. Data from a representative experiment of three performed is shown. P values are calculated using student’s t-test and error bars represent SEM. *p = 0.018; §p = 0.0002.
Tregs of allograft acceptors produce higher levels of regulatory cytokines and utilize both contact-dependent and independent mechanisms of suppression
To delineate the mechanisms by which Tregs suppress the activation of T cells, we measured the cytokine levels in the supernatant of suppression assays and investigated the mechanisms of suppression using ELISA and transwell assays, respectively. The levels of regulatory cytokines, TGFβ1 and IL10, were significantly higher (∼2-3 folds) in the supernatant of suppression assays with acceptor-Tregs compared to those with rejector-Tregs and syngeneic-Tregs (Fig. 3a). In transwell assays, only acceptor-Tregs were capable of significantly suppressing the T cell proliferation suggesting that these Tregs can utilize both cell-cell contact dependent and contact-independent (cytokine mediated) mechanisms of suppression (Fig. 3b). However, rejector-Tregs and syngeneic-Tregs were unable to suppress T cell proliferation in transwells, corroborating their diminished capacity to produce TGFβ1 and IL10.
FIGURE 3. Mechanism(s) of suppression utilized by Tregs.
(a) ELISA based analysis of cytokines in the supernatant collected at Day 3 from co-cultures of CD3 stimulated naïve T cells isolated from the LN of unprimed BALB/c recipients with the LN-Tregs of different transplant groups (TGF-β1: *p = 0.046, §p = 0.011; IL-10: *p = 0.003, §p = 0.017). (b) In transwell assays, naïve T cells isolated from the LN of unprimed BALB/c recipients were stimulated with anti-CD3 antibody, and the LN-Tregs from different groups were either added directly to the culture or were placed in transwell inserts of 1.0μm pore size (*p = 0.01). Proliferation was measured using the BrdU incorporation assay and compared with the proliferative responses of CD3-stimulated naïve T cell in the absence of Tregs and % suppression was calculated as described in Materials and Methods. Tregs were isolated from the draining lymph nodes of syngeneic recipients, allograft acceptors, and allograft rejectors at week 3 post-transplantation. The activity of Tregs is measured at Treg:Teff cell ratio of 1:2. Each transplant group consists of 4-6 recipient mice. Data from a representative experiment of three performed is shown. P values are calculated using student’s t-test and error bars represent SEM.
Tregs of allograft acceptors show allospecificity
Increased production of TGFβ1 and IL10 by acceptor-Tregs point toward a subset of induced Tregs which may be alloantigen-specific. To characterize this specificity further, we analyzed the suppression potential of Tregs of the different groups against proliferation of recipient naïve T cells (BALB/c) to donor (C57BL6)-specific antigen presenting cells (APC) and third party (C3H) APC, allodisparate to both recipients and donors (Fig. 4). Similar to suppression of CD3 antibody-stimulated T cells, acceptor-Tregs were more effective in suppressing donor-specific antigen (C57BL6-APC) stimulated T cells compared to syngeneic-Tregs. In contrast, no difference was observed in the potential of acceptor-Tregs and syngeneic-Tregs in suppressing the activation of non-specific third party antigen (C3H-APC) stimulated T cells; indeed, this suppression was equal to the suppression of donor-specific antigen stimulated T cells by syngeneic-Tregs. However, rejector-Tregs showed little to no suppression of any of the antigen stimulated T cells. These results clearly suggest induction of alloantigen-specific Tregs only in acceptors.
FIGURE 4. Alloantigen-specificity of Tregs.
The suppression potential of regulatory T cells was evaluated against proliferation of recipient’s naïve T cells to donor-specific and third-party (allodisparate to both recipient and donor) antigens. Naïve T cells from the LN of unprimed BALB/c mice (graft recipients) were co-cultured with antigen presenting cells (APC) of C57BL6 mice (graft donors) or C3H mice (third-party) in the presence of Tregs isolated form the draining lymph nodes of syngeneic recipients, allograft acceptors, and allograft rejectors at week 3 post-transplantation (*p = 0.012, Acceptor-Tregs: C57BL6-APC vs. C3H-APC). Proliferation was measured using the BrdU incorporation assay and compared with the proliferative responses of respective APC stimulated naïve T cell in the absence of Tregs and % suppression was calculated as described in Materials and Methods. Each transplant group consists of 4-6 recipient mice. Data from a representative experiment of three performed is shown. P values are calculated using student’s t-test and error bars represent SEM.
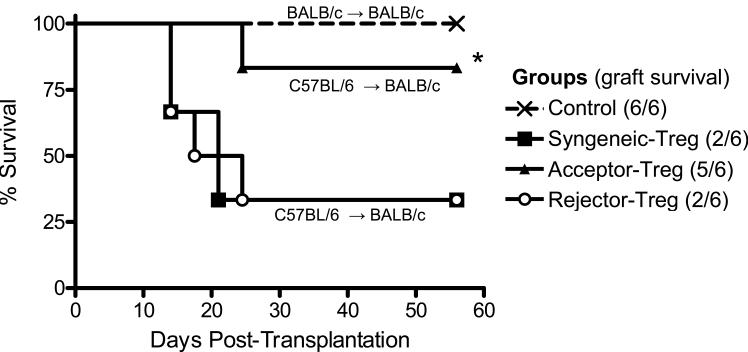
Tregs of allograft acceptors on adoptive transfer prevent allograft survival
Our in-vitro Treg functional data on T cell suppression and cytokine expression clearly demonstrated that Foxp3hi expressing Tregs from the LN of allograft acceptors are highly functionally effective compared to those of rejectors. Finally, we wanted to confirm this functional efficacy of Foxp3hi expressing Tregs in-vivo by demonstrating there ability to prevent graft rejection. Thus, we performed a Treg adoptive transfer experiment in which Tregs isolated from the LN of syngeneically grafted recipients, allograft acceptors, and rejectors at week 3 post-transplantation were transferred intravenously to three different groups of allograft recipients (Fig. 5). Only the group that was adoptively transferred with acceptor-Tregs showed significant increase in the allograft survival rate (83%, p = 0.03, Kaplan-Meier analysis), no improvement in graft survival was observed in the other groups of recipients which received syngeneic-Tregs or rejector-Tregs.
FIGURE 5. Effect of Treg adoptive transfer on allograft survival.
Tregs were isolated from the LN of syngeneically grafted recipients (syngeneic Treg), allograft acceptors (acceptor Treg) and allograft rejectors (rejector Treg) at week 3 post-transplantation; 1×105 Tregs per recipients were intravenously transferred to three different groups of allograft (C57BL6→ BALB/c) recipients at 18h post-surgery. Graft survival was monitored up to 8-wk post-transplantation. Controls recipients were syngeneically grafted (BALB/c→BALB/c) and received no Tregs. (n = 6 per group; *p = 0.035, Kaplan-Meier survival analysis).
DISCUSSION
Here we show that the frequencies of Tregs remain unchanged in allograft-acceptors versus allograft-rejectors in both the LN and grafts. However, Tregs isolated from the LN of allograft acceptors express significantly higher levels of Foxp3 compared to those of allograft rejectors. In addition, these Foxp3hi expressing Tregs are functionally highly effective in preventing graft rejection as demonstrated by adoptive transfer experiments.
Despite strong evidence about the association of Foxp3 primarily with Treg development and function, care must be taken with any simple interpretation of Foxp3 analysis. Recent human studies have shown that most T cells transiently turn on Foxp3 during early activation stages (21,22). Thus, it is imperative to characterize Tregs at both the phenotypic and functional levels, as most transplant studies are now using Foxp3 as a marker to define Tregs. Moreover, these reports are associating allograft outcome with Foxp3 PCR analysis or Treg frequencies (9-15). Our data clearly suggest that Foxp3 PCR analysis dose not simply reflect Treg frequencies. Increased Foxp3 expression in the LN of allograft acceptors was mainly due to the high level of Foxp3 expression in Tregs themselves, and not simply due to their increased numbers. In contrast to the LN, we did not observe differences either in Foxp3 levels in graft-infiltrating Tregs, or their frequencies in relation to total infiltrating T cells in accepted versus rejected grafts. However, the absolute numbers of Tregs in rejected grafts were higher than those in accepted grafts which is the main reason for the increased Foxp3 mRNA expression in rejected grafts. In addition to Tregs homing into grafts, these findings suggest that evaluation of only a single T cell subset (Tregs or T effectors) either at the graft site or in the lymphoid compartment may potentially lead to incomplete conclusions. Treg migration to the graft site appears to be either a response to downregulate the ongoing inflammation or non-specific homing due to a greater propensity of T cells to be recruited to sites of inflammation in the periphery. These findings are in accord with several previous studies demonstrating increased Foxp3 expression in the biopsies of rejected kidney grafts, and suggest the presence of intragraft Tregs as a consequence of the normal immune response during rejection (10,23).
The essential role of Foxp3 in regulating the suppressor function of Tregs has been well documented (16,17). Our observations of increased Foxp3 levels in the LN-Tregs of allograft acceptors prompted us to hypothesize that higher Foxp3 levels in Tregs are associated with their enhanced regulatory functions. Thus to validate our hypothesis, we analyzed the function of Tregs isolated from the LN of different transplant groups. Our data demonstrate that Foxp3hi Tregs isolated from the LN of allograft acceptors were more effective in suppressing naïve-T cell proliferation and in producing higher levels of TGF-β1 and IL-10 compared to those isolated from allograft rejectors and syngeneic recipients. However, Tregs of all the transplant groups failed to efficiently suppress the proliferation of allo-primed effector T cells. These findings suggest that Tregs may be more effective in regulating alloimmune response at the induction phase than at the effector phase. Our previous findings of more numbers of Tregs in rejected corneas with their inability to prevent rejection also lend support to this notion. The inefficiency of Tregs to suppress the allo-primed effector T cells may be due to the intrinsic resistance of effector T cells to suppression, potentially due to effector T cells’ increased capacity to produce cytokines (e.g., IL-6, TNFα, and IFNγ) which can inhibit and antagonize Treg function (24). Although, peripherally-induced CD4+CD25+ Tregs are phenotypically indistinguishable from thymus-derived CD4+CD25+ natural-Tregs, higher levels of TGF-β1 and IL-10 secretion by the acceptor-Tregs point toward the development of induced-Tregs in allograft acceptors. In addition, our data demonstrate the induction of alloantigen-specific Tregs only in the LN of allograft acceptors which corroborate with previous reports suggesting that peripheral development of alloantigen-specific Tregs occurs in the lymph nodes (25) and constitutively high expression of Foxp3 is required for Treg differentiation and function (16,17). Finally, our findings of Treg adoptive transfer experiment clearly show that only Tregs isolated from the LN of allograft acceptors are capable of preventing allograft rejection.
In summary, these findings provide new insights into the role of Tregs in transplantation immunity. For the first time, the present study reports that the functional status of Tregs is more reflective of the allograft outcome than their absolute frequencies, and that the levels of Foxp3 expression are directly associated with the Treg potential in preventing graft rejection. In addition, this is the first description of Treg localization and function in corneal transplantation, the most common form of tissue grafting. Our data also demonstrate the induction of allospecific Tregs in graft recipients, which clearly are able to suppress the induction of alloimmunity in regional draining lymph nodes but are not equally effective in suppressing the effector phase of the immune response. These observations have at least two important implications in regulating the immune responses to tissue transplants beyond the obvious applications to corneal alloimmunity. First, predicting and/or correlating allograft survival, or studying the effect of therapeutic agents on Treg biology in transplantation, exclusively on the basis of Treg frequencies (either in lymphoid tissues or graft site) may potentially lead to inaccurate conclusions. Second, potentiating Treg function to suppress alloimmunity, particularly at the induction phase, may be more helpful in promoting transplant longevity than at the effector phase.
Footnotes
This work was supported by NIH (NEI RO1-12963) and the Eye Bank Association of America.
REFERENCES
- 1.Wood KJ, Sakaguchi S. Regulatory T cells in transplantation tolerance. Nat. Rev. Immunol. 2003;3:199–210. doi: 10.1038/nri1027. [DOI] [PubMed] [Google Scholar]
- 2.Kang SM, Tang Q, Bluestone JA. CD4+CD25+ regulatory T cells in transplantation: progress, challenges and prospects. Am. J. Transplant. 2007;7:1457–1463. doi: 10.1111/j.1600-6143.2007.01829.x. [DOI] [PubMed] [Google Scholar]
- 3.Sakaguchi S. Naturally arising Foxp3-expressing CD25+CD4+ regulatory T cells in immunological tolerance to self and non-self. Nat. Immunol. 2005;6:345–352. doi: 10.1038/ni1178. [DOI] [PubMed] [Google Scholar]
- 4.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science. 2003;299:1057–1061. [PubMed] [Google Scholar]
- 5.Joffre O, Santolaria T, Calise D, Al Saati T, Hudrisier D, Romagnoli P, van Meerwijk JP. Prevention of acute and chronic allograft rejection with CD4+CD25+Foxp3+ regulatory T lymphocytes. Nat. Med. 2008;14:88–92. doi: 10.1038/nm1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graca L, Cobbold SP, Waldmann H. Identification of regulatory T cells in tolerated allografts. J. Exp. Med. 2002;195:1641–1646. doi: 10.1084/jem.20012097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.San Segundo D, Fábrega E, López-Hoyos M, Pons F. Reduced numbers of blood natural regulatory T cells in stable liver transplant recipients with high levels of calcineurin inhibitors. Transplant. Proc. 2007;39:2290–2292. doi: 10.1016/j.transproceed.2007.07.076. [DOI] [PubMed] [Google Scholar]
- 8.Korczak-Kowalska G, Wierzbicki P, Bocian K, Klosowska D, Niemczyk M, Wyzgal J, Korecka A, Durlik M, Chmura A, Paczek L, Górski A. The influence of immuosuppressive therapy on the development of CD4+CD25+ T cells after renal transplantation. Transplant. Proc. 2007;39:2721–2723. doi: 10.1016/j.transproceed.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 9.Bestard O, Cruzado JM, Rama I, Torras J, Gomà M, Serón D, Moreso F, Gil-Vernet S, Grinyó JM. Presence of FoxP3+ Regulatory T Cells Predicts Outcome of Subclinical Rejection of Renal Allografts. J. Am. Soc. Nephrol. 2008 May 21; doi: 10.1681/ASN.2007111174. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bunnag S, Allanach K, Jhangri GS, Sis B, Einecke G, Mengel M, Mueller TF, Halloran PF. Foxp3 expression in human kidney transplant biopsies is associated with rejection and time post transplant but not with favorable outcomes. Am. J. Transplant. 2008 May 28; doi: 10.1111/j.1600-6143.2008.02268.x. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 11.Naka EL, Ponciano VC, Rangel EB, Cenedeze MA, Pacheco-Silva A, Camara NO. FOXP3-positive regulatory cells inside the allograft and the correlation with rejection. Transplant. Proc. 2006;38:3202–3204. doi: 10.1016/j.transproceed.2006.10.123. [DOI] [PubMed] [Google Scholar]
- 12.Veronese F, Rotman S, Smith RN, Pelle TD, Farrell ML, Kawai T, Benedict Cosimi A, Colvin RB. Pathological and clinical correlates of FOXP3+ cells in renal allografts during acute rejection. Am. J. Transplant. 2007;7:914–922. doi: 10.1111/j.1600-6143.2006.01704.x. [DOI] [PubMed] [Google Scholar]
- 13.Dijke IE, Velthuis JH, Caliskan K, Korevaar SS, Maat AP, Zondervan PE, Balk AH, Weimar W, Baan CC. Intragraft FOXP3 mRNA expression reflects antidonor immune reactivity in cardiac allograft patients. Transplantation. 2007;83:1477–1484. doi: 10.1097/01.tp.0000264997.53153.8b. [DOI] [PubMed] [Google Scholar]
- 14.Yang H, Ding R, Sharma VK, Hilaire FS, Lagman M, Li B, Thomas DA, Luo X, Song P, Stauffer C, August P, Suthanthiran M. Hyperexpression of Foxp3 and IDO during acute rejection of islet allografts. Transplantation. 2007;83:1643–1647. doi: 10.1097/01.tp.0000263991.74052.46. [DOI] [PubMed] [Google Scholar]
- 15.Dijke IE, Caliskan K, Korevaar SS, Maat AP, Zondervan PE, Balk AH, Weimar W, Baan CC. FOXP3 mRNA expression analysis in the peripheral blood and allograft of heart transplant patients. Transpl. Immunol. 2008;18:250–254. doi: 10.1016/j.trim.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat. Immunol. 2003;4:330–336. doi: 10.1038/ni904. [DOI] [PubMed] [Google Scholar]
- 17.Wan YY, Flavell RA. Regulatory T-cell functions are subverted and converted owing to attenuated Foxp3 expression. Nature. 2007;445:766–770. doi: 10.1038/nature05479. [DOI] [PubMed] [Google Scholar]
- 18.Liu Y, Hamrah P, Zhang Q, Taylor AW, Dana MR. Draining lymph nodes of corneal transplant hosts exhibit evidence for donor major histocompatibility complex (MHC) class II-positive dendritic cells derived from MHC class II-negative grafts. J. Exp. Med. 2002;195:259–268. doi: 10.1084/jem.20010838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shen L, Jin Y, Freeman GJ, Sharpe AH, Dana MR. The function of donor versus recipient programmed death-ligand 1 in corneal allograft survival. J. Immunol. 2007;179:3672–3679. doi: 10.4049/jimmunol.179.6.3672. [DOI] [PubMed] [Google Scholar]
- 20.Huq S, Liu Y, Benichou G, Dana MR. Relevance of the direct pathway of sensitization in corneal transplantation is dictated by the graft bed microenvironment. J. Immunol. 2004;173:4464–4469. doi: 10.4049/jimmunol.173.7.4464. [DOI] [PubMed] [Google Scholar]
- 21.Pillai V, Ortega SB, Wang CK, Karandikar NJ. Transient regulatory T-cells: a state attained by all activated human T-cells. Clin. Immunol. 2007;123:18–29. doi: 10.1016/j.clim.2006.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang J, Ioan-Facsinay A, van der Voort EI, Huizinga TW, Toes RE. Transient expression of FOXP3 in human activated nonregulatory CD4+ T cells. Eur. J. Immunol. 2007;37:129–38. doi: 10.1002/eji.200636435. [DOI] [PubMed] [Google Scholar]
- 23.Haanstra KG, Wubben JA, Korevaar SS, Kondova I, Baan CC, Jonker M. Expression patterns of regulatory T-cell markers in accepted and rejected nonhuman primate kidney allografts. Am. J. Transplant. 2007;7:2236–2246. doi: 10.1111/j.1600-6143.2007.01917.x. [DOI] [PubMed] [Google Scholar]
- 24.Korn T, Reddy J, Gao W, Bettelli E, Awasthi A, Petersen TR, Bäckström BT, Sobel RA, Wucherpfennig KW, Strom TB, Oukka M, Kuchroo VK. Myelin-specific regulatory T cells accumulate in the CNS but fail to control autoimmune inflammation. Nat. Med. 2007;13:423–431. doi: 10.1038/nm1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ochando JC, Yopp AC, Yang Y, Garin A, Li Y, Boros P, Llodra J, Ding Y, Lira SA, Krieger NR, Bromberg JS. Lymph node occupancy is required for the peripheral development of alloantigen-specific Foxp3+ regulatory T cells. J. Immunol. 2005;174:6993–7005. doi: 10.4049/jimmunol.174.11.6993. [DOI] [PubMed] [Google Scholar]