Abstract
The present article provides a conceptual framework of the relation between alcohol involvement (A) and suicide attempts (S). This framework can be broadly construed to reflect two dimensions: directionality (direction of causality; A→S, S→A, or a spurious relation) and temporality (distinguishing between proximal and distal effects of both behaviors). We review and evaluate the evidence on the association between A and S among adolescents using this conceptual framework as a guide. The extant data suggest that this relation is complex and not fully understood. Further, it seems unlikely that a single approach will be found to determine direction of causality, and the specification and validation of hypothesized mechanisms will involve a variety of different types of evidence. Suggestions for additional research using informative designs are discussed.
Suicide is the third leading cause of death among adolescents and accounts for more deaths per year than the next seven leading causes combined (Anderson & Smith, 2003). In 2004, the incidence of suicide was 1.3/100,000 per year among youth aged 10-14 and 8.2/100,000 per year among adolescents aged 15-19 (Center of Disease Control [CDC], 2005). It is estimated that for every death by suicide there are between 8 to 25 nonfatal suicide attempts (Moscicki, 2001). Beyond the tragedy of self-inflicted mortality, the repercussions of adolescent suicide on close friends, extended peer networks, and the family are often severe and account for additional emotional and economic costs to individuals and society (Miller, Covington, & Jenson, 1999). Recognizing the importance of adolescent suicide and suicide attempts to the Nation's health, Healthy People 2010 (Department of Health and Human Services [DHHS], 2000) has listed as high priority goals to reduce, by more than half, completed suicide overall and suicide attempts in youth.
Given the seriousness of suicide, there is historical interest in identifying the factors that predispose adolescents to attempt suicide. Alcohol involvement (AI) is consistently implicated in adolescent suicide attempts (Mehlenbeck, Spirito, Barnett, & Overholser, 2003). This association has been hypothesized since the birth of modern psychiatry. Menninger conceptualized addiction as both a protracted from of chronic suicide and as playing a part in focal deliberate “accidents” (Menninger, 1938). Similar to Menninger, we believe that alcohol can relate to suicide attempts both situationally and chronically, and the aim of this paper is to put forth a conceptual framework of the relation between AI and suicide attempts.
The current manuscript is organized in three parts. The first part provides an overview of a conceptual framework of the link between AI and suicide attempts. The second part reviews and evaluates the evidence on the association between the two behaviors using the conceptual framework as a guide. Specifically, we review the AI-attempt association among adolescents who are, on average, below the age of 18. This age range was selected because 1) suicide-related behaviors among adolescents are a particularly serious public health concern, and 2) as an attempt to review studies using a more homogenous sample in regards to access to alcohol. For instance, adolescents' access to alcohol is typically greater when they are not living at home (e.g., in college dorms), and access to alcohol is related to rates of underage drinking (Wechsler, Kuo, Lee, & Dowdall, 2000). Data from studies conducted in the past twenty years are emphasized to reflect contemporary drinking and suicide attempts. Although it is important to determine whether demographics (e.g., gender, age, and ethnicity) and psychiatric disturbance are key parameters of the AI-suicide attempt relation, discussion of moderation is beyond the scope of this paper. The third part concludes with recommendations for informative designs to determine causality and possible mechanisms of action underlying the alcohol-attempt association.
The present review uses a definition of suicide attempt derived from two expert panels: the first sponsored by the American Association of Suicidology and the second jointly sponsored by the National Institute of Mental Health and the Center for Mental Health Services. These panels defined suicide attempt as a “potentially self-injurious behavior with a nonfatal outcome, for which ether is evidence (either implicit or explicit) that the person intended at some (nonzero) level to kill himself/herself” (O'Carroll, Berman, Maris, & Mosicicki, 1996), p. 247). Studies which examine any suicidality or a continuum of suicidality (e.g., ideation to attempt; Foley, Goldston, Costello, & Angold, 2006) or which use more liberal definitions (e.g., all self-injury regardless of suicide intent; Hawton, Fagg, Simkin, Bale, & Bond, 2000 and “have you tried to kill yourself or done anything that could have killed you,” Lewinsohn, Rohde, & Seeley, 1996) are not included. For the purposes of the present review, AI represents the broad domain of alcohol usage (e.g., frequency of use, frequency of heavy use, quantity consumed), alcohol consequences, and alcohol abuse/dependence symptoms. That is, both proximal alcohol involvement (the amount consumed on an occasion and its acute consequences) and distal alcohol involvement (drinking patterns, alcohol consequences, and alcohol abuse/dependence symptoms) are both subsumed under this broad rubric of AI.
Part 1: Theoretical Framework
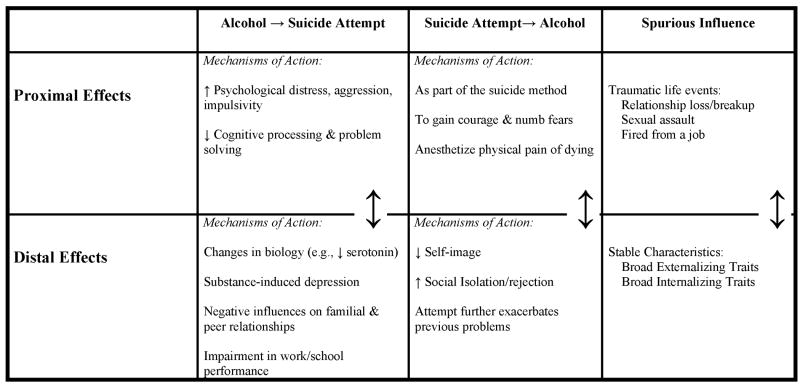
This framework builds upon those proposed by Cooper (2006) in her analyses of the relation between AI and high-risk sexual behavior and from Menninger (1938) and Koob and colleagues (e.g., Koob & Le Moal, 1997), who have highlighted the importance of distinguishing between alcohol's acute and chronic effects on brain and behavior. As shown in Figure 1, this framework can be broadly construed to reflect the alcohol (A) and suicide (S) relation along two domains: (1) directionality, and (2) temporality. By directionality, we mean the extent to which AI leads to a suicide attempt (A→S), a suicide attempt leads to drinking (S→ A), or the extent to which a third variable spuriously causes both A and S. Temporality refers to whether the association is attributable to causal factors that exert influence situationally or over an extended period of time. Specifically, a proximal effect occurs in the hours or minutes after a behavior and exerts its influence over a correspondingly short time interval. A distal effect reflects an accumulated process, or any protracted effect occurring in the days, weeks, or years after a behavior (attempt or drinking). Distal effects are assumed to exert their influence over extended time intervals. With respect to alcohol, we use the terms proximal and distal to correspond to traditional notions of acute and chronic effects.
Figure 1.
Theoretical framework of the alcohol-suicide attempt relation
Some mechanisms might be relevant to multiple subdomains. For example, impulsivity can contribute to both the tendencies to drink heavily and to attempt suicide (distal, third-variable mechanisms). Yet even in this situation, AI can still exert proximal causal influence on suicide attempt (proximal A→S) above and beyond distal effects on both behaviors.
The domains of directionality and temporality are transtheoretical and can be used to describe mechanisms at varying levels of a biopsychosocial model. Moreover, the framework is not limited to adolescence or to suicide attempts as the behavior of interest, but instead may be used to represent putative casual factors for other age groups or problems/disorders. Figure 1 and the discussion below are organized into six cells derived by crossing the directionality and temporality domains. This was done to facilitate exposition of the framework, but it is important to recognize that the temporality domain should be viewed dimensionally because certain phenomena may be intermediate in their temporality (e.g., relationship breakup).
Proximal Effects of A→S
The first model assumes that proximal effects of drinking cause suicide attempts. A review by Hufford (2001) suggests that the mechanisms of action underlying this effect may include alcohol increasing psychological distress, depressed mood and anxiety, aggressiveness, and/or impulsivity. These effects can be conceptualized at the neuropharmacological level such as alcohol increasing activity of GABA, the brain's chief inhibitory neurotransmitter (National Institute of Alcohol Abuse and Alcoholism [NIAAA], 2004), or other central brain mechanisms thought to relate to behavioral activation such as increased serotonin (Julien, 2001).
In addition, cognitive constriction (narrowed attention which reduces perceived potential solutions to a dichotomy – immediate solution or suicide) is frequently observed prior to a suicide attempt (Shneidman, 1985). Alcohol produces a similar effect on cognitive processing via a process termed alcohol myopia (Steele & Josephs, 1990) suggesting that alcohol could play an important role in cognitive constrictions. This hypothesis is consistent with research showing that inhibition conflict (weighing pros and cons and identifying alternative solutions) mediates the relation between intoxication and social behavior (Steele & Southwick, 1985).
Proximal Effects of S→A
Once a decision has been made to attempt suicide, alcohol use may serve several functions. Alcohol expectancies play an inportant role in determining alcohol use and behavior (Goldman, Del Boca, & Darkes, 1999) and, consequently, it is reasonable to hypothesize that suicide-related alcohol expectancies relevant to gaining courage, numbing fears, or anesthetizing the pain of dying may lead to the incorporation of alcohol use into a suicide plan. Drinking may also serve as a “means to an end” as the suicide method itself (e.g., alcohol poisoning; Garfinkel, Froese, & Hood, 1982; Krajnc, Schmidt, Gergoric, & Dogsa, 1998; Withers & Kaplan, 1987).
Distal Effects of A→S
The AI/suicide attempt relation is often viewed as a “proximal” or situational phenomenon, but it is crucial to consider potential mechanisms underlying this relation beyond those associated with proximal intoxication as a cause or a means of suicide attempt. Not surprisingly, the negative interpersonal, academic, and legal problems that can result from problematic drinking (NIAAA, 2004/2005) are often provided by adolescents as reasons for suicide attempts (Windle, 2004). Furthermore, research consistently identifies serotonin hypofunction in completed suicide, serious suicide attempts (see Kamali, Oquendo, & Mann, 2001, for review), and alcohol dependence (Sher, 2006). Serotonin depletion is also associated with increased aggression and impulsivity (Kamali et al., 2001), and these factors predict early-onset alcohol use disorders (Clark, Parker, & Lynch, 1999) and suicide attempts among alcoholics (Bergman & Brismar, 1994; Suominen, Isometsa, Henriksson, Ostamo, & Lonnqist, 1997). Likewise, some theorists (e.g., Koob & LeMoal, 1997) suggest that changes in hedonic tone that accompany distal substance use are central aspects of the addictive process and that the maintenance of substance use in the dependent person is driven by attempts to regulate the affective disturbance that results from distal substance use. Moreover, adolescents appear particularly vulnerable to the neurotoxic effects of alcohol, and adolescent substance use has adverse consequences on brain development and executive functioning (e.g., Crews, Braun, Hoplight, Switzer, & Knapp, 2000). Such above processes can theoretically explain, at a neuropharmacological level, how distal AI (e.g., frequent and heavy alcohol usage, alcohol consequences, and alcohol abuse/dependence) results in vulnerability to suicide. It is also important to note that some mood disorders may be alcohol induced (and remit after a period of abstinence; (Widiger et al., 1994) and alcohol withdrawal is often associated with affective disturbance (Sher & Grekin, 2007). Thus, while the AI/suicide relation is often viewed as a “proximal” or situational phenomenon, the toll of chronic drinking on both the brain and the social environment of the drinker can be severe.
Distal Effects of S→ A
Although not typically considered, the aftermath of a suicide attempt may result in altered interpersonal environments that increase the risk for AI (e.g., frequent and heavy alcohol usage, alcohol consequences, and alcohol abuse/dependence). Suicide attempt is a markedly deviant behavior, and deviant behaviors often lead to peer rejection, which in turn could lead to association with deviant peers (e.g., Patterson, DeBaryshe, & Ramsey, 1989) and future substance use in the context of peer rejection (Prinstein & La Greca, 2004). In addition, several studies have documented that the attempter's environment was altered when they were assessed one to two years post-attempt. For instance, one study showed that 58% of adolescent suicide attempters were no longer living at home with a parent (Barter, Swaback, & Todd, 1968), and another documented that 74% experienced school changes (Cohen-Sandler, Berman, & King, 1982) post-attempt. School changes may be voluntary, due to moving or embarrassment/harassment because of the attempt, or involuntary (e.g., expelled or denied enrollment). One study documented that 23% of adolescent suicide attempters were subsequently involved in physical fighting three months post-hospitalization (Spirito et al., 1992). In addition, young adults who attempt suicide often are not allowed to continue college enrollment due to fears of litigation (Bender, 2006; Moran, 2006) which disrupts a student's social world. Finally, psychiatric hospitalization is perceived as stigmatizing (Townsend & Rakfeldt, 1985) and perceived devaluation-discrimination can lead to decreased self-esteem among those with mental illness (Link, Struening, Neese-Todd, Asmussen, & Phelan, 2001). Thus, in such cases unsuccessful suicide attempt may lead to problematic drinking in order to self-medicate (Khantzian, 1997) negative feelings or social consequences that may follow a failed attempt.
Spurious Effects, Z→ A & S
Finally, it is possible that drinking and suicide attempts are not causally related, but rather spuriously correlated due to a common third-variable influence which is antecedent to both. Like directional associations, these spurious associations can be conceptualized at both proximal and distal mechanistic levels. In statistical parlance, distal third-variable influences can be viewed as arising from fixed covariates while proximal third-variable influences can arise from situational or time-varying covariates. Thus, the situational or distal relation between drinking and suicide attempt may be spurious. For instance, individuals may engage in both behaviors because of stable characteristics such as poor impulse control and/or as a dysfunctional coping strategy (e.g., avoidance coping, see Cooper, Wood, Orcutt, & Albino, 2003). In addition, these behaviors may be a manifestation of broader psychopathology such as internalizing psychopathology (Krueger, 1999; Derogatis & Fitzpatrick, 2004; Derogatis & Melisaratos, 1983) and/or externalizing psychopathology (Achenbach, 1978; Hinshaw, 1987; Jessor & Jessor, 1975; Krueger, 1999). Alternatively, acute intoxication and suicide attempts may be spuriously related through a proximal traumatic life event that causally influences both behaviors (e.g., relationship break up, sexual assault or bereavement (Overholser & Spirito, 2003; Volpicelli, Balaraman, Hahn, Wallace, & Bux 1999).
Complex Causal Chains
Although not specifically outlined in our framework, highly complex mediational chains are possible. First, AI may reciprocally influence suicide attempts, setting up a vicious and potentially deadly downward spiral. Second, the proximal effects of drinking may synergize with the distal effects of alcohol consumption. Distal effects of alcohol misuse create a mood diathesis and decreased self-regulation (Koob & Le Moal, 2001) which feed the proximal effects of drinking (e.g., increased impulsivity and depressed mood). This complex chain is plausible for those adolescents who heavily alcohol involved (i.e., dependent). In sum, despite the broad, general assumption that alcohol consumption is causally associated with suicide attempts, theory and indirect empirical data suggest a more complex relation varying in the domains of directionality and temporality. In the next section, studies investigating the link between AI and suicide attempts among adolescents are reviewed and evaluated in the context of the conceptual framework.
Part 2: Evaluating the Evidence
In this section, evidence for a causal relation between AI and suicide attempt is evaluated in terms of directionality and temporality. The synthesis of research findings are presented in order of least-informative to most-informative within 4 cells (i.e., Proximal Effects of A→S and S→A; Distal Effects of A→S and S→A). To synthesize existing research findings, we first describe proximal alcohol-attempt relations. Due to the descriptive nature of the research on adolescent alcohol intake proximal to a suicide attempt bivariate or unique associations cannot be reviewed. Instead, descriptive data pertaining to alcohol use which surrounds a suicide attempt will be presented. Next, we describe distal AI-suicide attempt relations. This section is divided into two subsections. The first subsection reviews simple bivariate associations (meaning that there are just two variables being considered: AI and attempt) and the next subsection reviews unique relations controlling for theoretically relevant covariates. For ease of presentation, research relating to spurious associations between AI and suicide attempt and general methodological considerations will be embedded within each section.
Proximal Alcohol-Suicide Attempt Relations
Ambiguous Directionality of Proximal Relations
In this section, we review clinical studies of suicide attempters. These studies report the proportion of suicide attempters who drank or used substances surrounding the time of the suicide attempt. Such research is descriptive in nature and is ambiguous with respect to establishing directionality. For instance, between 7% and 37% of suicide attempters presenting to a hospital following a suicide attempt tested positive for alcohol using blood or urine samples (Mannenbach, Hargarten, & Phelan, 1997; Spirito, Mehlenbeck, Barnett, Lewander, & Voss, 2003), and 14% to 40% self-reported consuming or being under the influence of alcohol at the time of the attempt (Groholt, Ekeberg, & Haldorsen, 2000; Kotila & Lonnqvist, 1988; Vajda & Steinbeck, 2000). Results from surveys of high school students (Wichstrom, 2000), homeless youth (Sibthorpe, Drinkwater, Gardner, & Bammer, 1995), juvenile delinquents (Howard, Lennings, & Copeland, 2003), and adolescent outpatients (Rotheram-Borus, Walker, & Ferns, 1996) indicate that approximately one quarter (ranging from 24% to 28%) use alcohol or drugs at the time of the attempt. Perhaps not surprisingly then, substance abusers in treatment (Berman & Schwartz, 1990; Cavaiola & Lavender, 1999) also indicate a high prevalence of drinking or drug use accompanying suicide attempts (40% to 74%).
Although it is difficult to determine if these “occasion specific” rates of alcohol consumption are higher than would be expected in either non-attempters on comparable measurement occasions (case controls) or higher than the same attempters on appropriately matched non-attempt occasions (case-crossover comparison), there is strong reason to suspect that the prevalence of drinking surrounding suicide attempts occasions is elevated. Not only are rates of co-occurrence seemingly high, but a case-crossover study of an adult sample (Borges et al., 2004) indicated that there is a strong within-subjects relation between drinking and suicide attempts. Unfortunately, there are no case-crossover studies in adolescence and the majority of studies on the relation between proximal alcohol consumption and adolescent suicide attempts are descriptive in nature, and cannot resolve the directional of the event-based alcohol-suicide attempt relation.
Proximal Effects of A→S
Unlike the studies mentioned above, which provide rates of alcohol use surrounding a suicide attempt, in this section we review studies which inquire about directionality (i.e., whether alcohol's proximal effect leads to a suicide attempt) but provide far from conclusive evidence. Specifically, Kotila & Lonnqvist, 1988 describe adolescents' perceptions of alcohol's impact on suicide attempts and conclude that a considerable minority (25%) of hospitalized suicide attempters report a provoking influence of alcohol on an attempt (Kotila & Lonnqvist, 1988). Eight percent of these adolescents claimed to have suicidal thoughts or make attempts only when drinking (Kotila & Lonnqvist, 1988). However, it is well known that individuals are ill suited for determining the causes of their behavior (Nisbett & Ross, 1980) and self-reported attributions of alcohol playing a causal role must be interpreted with considerable caution.
Proximal Effects of S→A
In this section, we review studies which specifically inquire about an adolescent's method of suicide attempt. Among hospitalized suicide attempters, very few adolescents (range 1.6%-2.9%) specifically list alcohol as the primary (or part of the) suicide attempt method (Garfinkel et al., 1982; Krajnc et al., 1998; Withers & Kaplan, 1987). Unfortunately, the majority of published research in this area was not suitable for inclusion in the present review due to the ambiguous description of the attempt method (e.g., ingestion of substances, poisoning, overdose, drugs). Moreover, it is typical for adolescents who attempt suicide by overdose to use more than one substance (e.g., (Garfinkel et al., 1982). Asking about the primary method obscures possible measurement of alcohol consumption as a suicide method employed during the attempt. Still, although alcohol may not play a prominent role as part of a suicide plan for most adolescents, it apparently does for a small minority and, therefore, needs to be considered.
Summary
Research on the proximal relation between alcohol and suicide attempts is in its nascent stage. A substantial minority of suicide attempters consume alcohol prior to or during a suicide attempt. Some adolescents perceive alcohol as a causal influence on their attempt, while very few report use of alcohol as the method of attempt.
General Methodological Considerations
There is a number of general methodological considerations pertaining to sample selection, measurement of alcohol consumption, assessment of adolescents' purpose for consumption, and descriptive nature of reports. First, the overwhelming majority of studies sampled adolescents who presented to the hospital following a suicide attempt. However, the majority of adolescent suicide attempters (68%) do not seek medical attention (CDC, 2004). Attempters who present to the emergency department may differ from attempters who do not on a range of characteristics other than medical severity (e.g., greater help-seeking behavior, more severe pathology). Thus, clinical ascertainment may result in limited generalizability of results (Kazdin, 1998).
Second, measurement and reporting of alcohol consumption as a precursor to a suicide attempt or as a suicide method is not optimal. Researchers routinely report on consumption of drugs or substances without distinguishing among alcohol, illicit drugs, or prescription medications. Overdose is the most common method for adolescent suicide attempt (Overholser & Spirito, 2003), but it is unclear from the literature whether alcohol is typically a component of overdose.
Researchers who do report specifically on alcohol use tend to use self-report measures. Objective measures have less bias than subjective self-report measures, and only two reports used objective measures of alcohol consumption (e.g., blood and urine samples). However, among reports using objective measures of alcohol, the time-frame from first sip to hospital arrival is varied or is not reported (e.g., Spirito et al., 2003 [7%; no time frame provided], and Mannenbach et al., 1997 [36%; within 6 hours]). Long intervals between the last drink and the actual time of measurement can contribute to unreliable estimates of the level of intoxication during the attempt. Third, different amounts of alcohol could be used depending on the purpose of consumption. For instance, attempters who incorporate drinking as part of the suicide plan (S→A) may not want to be overly intoxicated to the point where the likelihood of a successful attempt is compromised but rather he or she may consume low-levels of alcohol to obtain an anxiolytic or “liquid courage” effect without severe impairment (especially if there is high ambivalence surrounding the plan). Conversely, attempters using alcohol as the method of attempt (S→A) would presumably consume large quantities. Among individuals without an immediate plan (i.e., he or she has no prior plan of suicide before drinking), higher amounts of alcohol consumed could presumably increase the likelihood of attempt (A→S), at least up to a certain point. We hypothesize that an individual who drinks to extreme excess but does not suffer a lethal effect will be incapacitated and unable to follow through with an attempt planned after drinking was initiated. Thus, there may be different relations between alcohol and suicide attempt depending on the purpose and amount consumed. Researchers need to inquire about the purpose of alcohol consumption, while employing objective measurement of adolescents' alcohol levels in close proximity to the time of hospital arrival.
Finally, due to the descriptive nature of the research, it is impossible to evaluate the directionality of the event-based alcohol-suicide attempt relation or whether drinking and suicide attempts are spuriously correlated due to a common third-variable influence. It is imperative for investigators to not only improve on the methodological limitations (e.g., sample selection, measurement of alcohol consumption, and assessment of the adolescent's purpose for consumption) listed above, but also to move away from simple description to evaluating the likelihood of a causal or spurious association.
Distal Alcohol-Suicide Attempt Relations
Bivariate Relations: Two variables (AI and attempt) are considered
Ambiguous Directionality of Distal Relations
In this section, we review research which is ambiguous with respect to establishing directionality of the alcohol-suicide attempt distal relation. Specifically, we summarize results from cross-sectional survey studies on the bivariate distal association between adolescent AI and suicide attempts. For instance, a relation between suicide attempt and frequency of drinking and of heavy drinking, alcohol consequences, and alcohol abuse and dependence diagnoses has been reported in numerous cross-sectional surveys of adolescents ascertained from schools (Grossman, Milligan, & Deyo, 1991; Howard-Pitney, LaFromboise, Basil, September, & Johnson, 1992; Kebede & Ketsela, 1993; Kinkel, Bailey, & Josef, 1989; Manson, Beals, Dick, & Duclos, 1989; Shaughnessy, Doshi, & Jones, 2004; Windle & Windle, 1997), the community (Felix-Ortiz, Munoz, & Newcomb, 1994; Glowinski et al., 2001; Madianos, Gefou-Madianou, & Stefanis, 1994), mental health outpatient clinics (Bryant, Garrison, Valois, & Rivard, 1995; Rotheram-Borus et al., 1996), and juvenile detention centers (Putnins, 1995), but not invariably so (Cosgrave et al., 2004; DeSimone, Murray, & Lester, 1994; Yoder, 1999). Unfortunately, studies operationalized alcohol frequency and alcohol consequences differently and there was no standardization of measurement.
The bivariate association between AI and suicide attempts may vary as a function of the attempt phenotype. For example, in one school-based cross-sectional survey, alcohol use frequency was higher among those individuals making a medically attended attempt than those making a not medically attended attempt (Burge, Felts, Chenier, & Parrillo, 1995). The increased prevalence of AI among those adolescents making more lethal or serious attempts highlights the potential clinical significance of AI.
Distal Effects of A→S
The above cross-sectional surveys correlating AI and suicide attempt are ambiguous with respect to establishing temporal precedence of alcohol consumption and suicide attempt. In this section, we review case-control studies based on suicide attempts, clinical studies based on suicide attempt characteristics (e.g., medical seriousness of attempt), as well as prospective studies where suicide attempters are followed and drinking prior to the index attempt is used to predict reattempts. In each of the studies reviewed below, the assessment of AI referenced the period prior to the adolescents' presentation to the hospital (or control event). Thus, unlike the cross-sectional surveys mentioned above, these studies provide stronger, but far from conclusive evidence for the direction of the AI and suicide attempt relation (e.g., even if temporality is established, spurious effects are not). However, it is important to note that AI is assessed retrospectively and the experience of the outcome (i.e., suicide attempt) may distort an adolescent's reporting of his or her AI.
Case-control studies
Evidence for a distal relation between AI and suicide attempt varies as a function of the selected comparison group. Research demonstrates that frequency of consumption differentiates suicide attempters who present to the emergency room (ER) from ER controls (McKenry, Tishler, & Kelley, 1983). Moreover, past substance abuse differentiates adolescent ER suicide attempters from non-suicidal ER or medical controls (Garfinkel et al., 1982; Paluszny, Davenport, & Kim, 1991). Although differences in past substance abuse have been documented, some evidence suggests that these groups do not differ in terms of past substance dependence (Gmitrowicz & Kolodziej-Maciejewska, 2002), but alcohol and other substances are important contributors to both unintended injuries (Vinson, Maclure, Reidinger, & Smith, 2003) and a wide range of medical conditions (Weathermon & Crabb, 1999). However, when comparing ER suicide attempters with psychiatric controls, researchers report that substance abuse does not differentiate these groups (Brent et al., 1993; Spirito, Stark, Fristad, Hart, & Owens-Stively, 1987). Thus, it is possible that substance abuse is less likely to differentiate hospitalized suicide attempters from a control group as the psychiatric severity of the control group increases. However, it is important to consider that the level of psychiatric disturbance among the controls is unknown before this discrepancy in findings is attributed to level of psychiatric severity. Additionally, the degree to which these findings are related to alcohol abuse/dependence, rather than substance abuse in general, is unknown.
Clinical studies of attempt characteristics
From a clinical perspective, it is important to determine whether AI relates to the medical seriousness of an attempt. There is some evidence that the relation between substance abuse and medical seriousness may vary as a function of the chosen method of the suicide attempt, but the current research is inconclusive. For instance, among hospitalized suicide attempters (regardless of their suicide method), prior alcohol or drug abuse does not differentiate levels of lethality of attempt (i.e., possibility of death if left untreated (Nasser & Overholser, 1999; Paluszny et al., 1991). However, among attempters who overdosed on over-the-counter or prescription pills, severe attempters (indicated by extreme toxicity levels) had higher rates of prior substance abuse than mild or moderate attempters (Spirito et al., 1987). A possible conjecture is that attempters by overdose with a history of substance use have a greater familiarity with the amount of drugs needed to achieve a particular state and avoid (or achieve) a particular consequence (e.g., death). This knowledge could increase the lethality of attempt. However, the specific drugs (i.e., alcohol, prescription drugs, or illicit drugs) that adolescent attempters abuse prior to an attempt or used during the attempt are generally unknown.
Prospective studies of suicide attempters
The strongest predictor of a subsequent suicide attempt is a previous attempt (Harris & Barraclough, 1997; Hawton, 1987; Roy, 1982). When youth actually make a suicide attempt, they cross a behavioral threshold that is more severe than suicidal thoughts or plans. Such occurrence may increase likelihood of a subsequent attempt because attempts are now a part of the behavioral repertoire (Goldston, 2003). Furthermore, youth may learn from failed attempts, thus increasing the potential for lethality. Given that previous suicide attempters are at increased risk for reattempt, it is important to determine whether AI prior to the index hospitalization predicts reattempt. Among participants in two studies examining this question, a pattern of general substance use or alcohol abuse prior to hospitalization following an attempt predicted a future attempt within six months in one study (Stewart, Manion, Davidson, & Cloutier, 2001) and within one year in the second study (Vajda & Steinbeck, 2000). Thus, there is some evidence that AI predicts reattempt within the following year among high-risk samples of adolescent suicide attempters.
Distal Effects of S→A
In this section, we review prospective studies of suicide attempters which determine participants' pattern of alcohol use following their suicide attempt and cross-sectional cohort studies which attempt to shed light on whether a first suicide attempt usually precedes regular alcohol use using retrospective reports.
Prospective studies of suicide attempters
Few studies have examined the possibility that drinking can occur as a consequence of a suicide attempt. Spirito et al. (1992) found that 16.7% of adolescents presenting to a general hospital after a suicide attempt used alcohol at least once a week at a three-month follow-up Additionally, hospitalized adolescent suicide attempters have been shown to be more likely to drink at least weekly or meet criteria for alcohol abuse than non-suicidal pediatric controls between 5 and 15 years later (Laurent, Foussard, David, Boucharlat, & Bost, 1998; Otto, 1972). None of these studies reported assessing drinking patterns prior to the attempt, limiting our ability to determine whether post-attempt drinking was a consequence of the suicide attempt.
Cross-sectional cohort studies
Interestingly, a cohort study using a representative sample of Missouri female adolescent twins found adolescents retrospectively report that their first suicide attempt precedes the onset of regular alcohol use by an average of 1.4 years (SD = 2.3) among alcohol dependent subjects and 1.8 years (SD = 2.5) among non-alcohol dependent subjects (Glowinski et al., 2001). These findings highlight the potential error of assuming that AI invariably precedes suicide attempt without considering the possibility of reverse causation (or third-variable causation).
Summary
Cross-sectional self-report survey data show that a significant bivariate relation (meaning that two variables are being considered in a statistical analysis) is generally found between AI (i.e., frequency of drinking and of heavy drinking, alcohol consequences, and alcohol abuse and dependence diagnoses) and suicide attempts across diverse samples, and that AI can relate to attempts with potentially higher lethality (i.e., those which receive medical attention). Hospitalized suicide attempters (cases) have higher rates of substance abuse than controls, with the exception of non-suicidal controls with clear psychiatric disturbance. While it is unclear whether substance abuse relates to the medical severity of an attempt in clinically ascertained samples of ER patients, AI (i.e., general substance use or alcohol abuse) prior to hospitalization due to a failed suicide attempt predicts reattempt within one year post-hospitalization.
In addition, there is very little research examining the possibility that AI is a consequence, and not a potential cause, of a failed suicide attempt. Adolescents tend to drink regularly and have alcohol problems after an attempt, both in the short- and long-term and one population-based study found that adolescent's first suicide attempt often preceded regular drinking. However, it is unclear whether adolescents' previously established drinking patterns change as a result of an attempt and whether various confounders may explain such a relation.
General Methodological Considerations
There are four main methodological considerations in examining this literature: the assessment of AI vs. general substance use, assessment of substance use, restricted sampling of suicide attempters, and the bivariate nature (meaning that two variables are being considered) of current research. First, it is unknown whether AI, rather than substance use, more generally relates to the attempt characteristics (e.g., severity) or differentiates attempters from various controls. It is important for researchers to address whether the relation between adolescent substance use and suicide attempt is distinctive to alcohol, or attributable to other varieties of drug use (see Specificity and Unique Relations below). Second, in clinically ascertained samples, most reports did not adequately describe the assessment of substance abuse and simply indicated that clinician's determined whether substance abuse was present or absent during their evaluation. Third, researchers investigating how substance abuse impacts the potential lethality of an attempt only sampled individuals who presented to a hospital following a suicide attempt. To estimate effects of lethality with less bias, it is important for researchers to also include attempters who did not seek medical attention. Those who do not seek medical attention are, arguably less likely to have made a serious attempt (potentially creating a range restriction problem). On the other hand, those who do not seek medical attention may still make suicide attempts with great potential for harm. Including attempters who did not seek medical attention in future studies will increase our ability to accurately estimate effects of covariates (including alcohol) on lethality. Finally, due to the bivariate nature of the preponderance of current research (meaning that two variables are being included in a statistical analysis), it is impossible to evaluate whether drinking and suicide attempts are spuriously correlated due to a common third-variable influence and to establish specificity of the ostensible cause.
Specificity and Unique Relations
There are several constructs which are associated with both AI and suicide attempts among adolescents. Consequently, it is critical to establish specificity of cause at the level of the risk factor. Arguably the first step in establishing specificity of cause is to “rule out” closely related constructs as accounting for the observed relation between AI and suicide attempts. Below we highlight important confounds that make it difficult to identify specific relations between AI and suicide attempts. Confounds, by definition, are associated with both the predictor and criterion. Thus, in the case of AI having a specific effect on suicide attempt or suicide attempt having a specific effect on AI, specificity of cause needs to be established with respect to confounding factors reflecting vulnerability to suicide attempts and drinking.
Although typically considered a part of the externalizing spectrum (Achenbach, 1978; Hinshaw, 1987; Jessor & Jessor, 1975; Krueger, 1999), alcohol use disorders are associated with a wide-range of psychological disorders including those from both the internalizing and externalizing spectrum. That is, although problematic alcohol use is associated with a range of externalizing psychopathological symptoms and syndromes including conduct disturbance/antisocial personality traits, risky and/or precocious sexual behavior, school problems, other substance abuse, and sensation-seeking, impulsivity, and poor self-regulatory traits (Best, Manning, Gossop, Gross, Strang, 2005; Donovan, Jessor, and Costa, 1999; Fergusson, & Lynskey, 1996). It is also associated with internalizing psychopathology such as mood and anxiety disorders (e.g., Rohde, Lewinsohn, & Seeley, 1996). Conversely, although suicide attempts are most commonly associated with mood disorders such as depression (APA, 1994), it is also associated with the externalizing spectrum of problem behaviors (Galaif, Sussman, Newcomb, & Locke, 2007). Moreover, both problematic alcohol use and suicide attempts are strongly associated with some disorders (e.g., borderline personality disorder; bipolar I disorder) that show strong characteristics of both externalizing (e.g., impulsivity) and internalizing (e.g., affective instability) domains. Consequently, the range of potential confounding traits and psychopathology is vast because neither alcohol use disorder or suicide attempt comorbidities are limited to a single class of disorder. Thus, if trait-like, third variables are to be modeled statistically, they must cover the most critical domains of potential confounding and a broad, possibly redundant approach is warranted. Despite difficulty classifying some types (and subtypes) of many forms of psychopathology, we summarize relevant literature on potential confounds within the framework of internalizing and externalizing traits, problems, and behavior.
Distal Effects of A→S
For the reasons described above, it is important to determine whether AI remains significantly associated with suicide attempt in the presence of two domains of confounding risk variables focusing on broad internalizing and externalizing traits/behaviors.
Cross-sectional studies
As a preliminary step we review whether AI has a unique association with adolescent suicide attempts, while acknowledging that cross-sectional survey studies do not address temporal priority, let alone etiology. Clinical and community surveys collectively report a unique association between adolescent suicide attempt and frequency of drinking and intoxications, alcohol consequences, and alcohol abuse and dependence diagnoses in the presence of one (Bryant et al., 1995; Garrison, McKeown, Valois, Vincent, & Murray, 1993; Grossman et al., 1991; Lyon et al., 2000; Rossow & Wichstrom, 1994; Wagner, Cole, & Schwartzman, 1996) and two (Glowinski et al., 2001; Wichstrom, 2000; Windle, 2004) domains of confounding risk variables. For instance, a sample of 2,586 high school students completed an in-school survey assessing risk factors for suicide attempts (Yip et al., 2004). Moderate alcohol use (i.e., 1-3 times a week) was significantly associated with past-year suicide attempt controlling for depressive symptoms, having sexual intercourse prior to age 14, and other drug use, as well as other theoretically important covariates (e.g., quality of familial and peer relationships, loss). However, this study was conducted in Hong Kong and similar results may not be found in the United States or other Western countries. We could not identify any published studies which include multiple domains of confounding risk variables in the prediction of medically attended attempt among adolescents. Regardless, prospective data are needed to determine specificity of cause at the level of the risk factor.
Prospective survey studies
Longitudinal research demonstrates that AI uniquely predicts subsequent suicide attempt (at least when the time-interval between assessments is relatively short). Specifically, investigators report a unique AI (i.e., alcohol quantity-frequency and frequency of intoxication) effect when the assessments are within two years of one another (e.g., 6 months, Reifman & Windle, 1995; 2 years, Wichstrom, 2000). For example, among a nationally representative study of Norwegian students in grades 7-12, Time 1 (T1) past year number of alcohol intoxications predicted a future suicide attempt two years later (T2) controlling for T1 suicide attempt, internalizing traits (e.g., depressed mood), externalizing traits (e.g., other drug use), as well as a range of potential covariates (e.g., peer acceptance and parental environment (Wichstrom, 2000). However, T2 number of alcohol intoxications did not predict a suicide attempt five years later (T3) multivariately (Wichstrom & Hegna, 2003).
In a controlled study of a New Zealand birth cohort (Fergusson & Woodward, 2002; Woodward & Fergusson, 2001), a diagnosis of alcohol abuse between the ages of 14 and 15 did not predict suicide attempt from the previous assessment to age 21 controlling for previously diagnosed depression, conduct disorder, and other covariates (e.g., deviant affiliations, parental loss, and childhood sexual abuse). At first glance, these results suggest a relatively more proximal relation between alcohol and suicide attempt. However, the majority of prospective studies reviewed above controlled for only a few confounding risk variables from the internalizing and externalizing domains.
Distal Unique Effects of S→A
Although little research has been conducted on whether AI uniquely predicts suicide attempts among adolescents, even less is known about the unique effects of suicide attempt in the prediction of adolescent AI after controlling for confounding risk variables from internalizing and externalizing domains.
Cross-sectional survey studies
Cross-sectional research on whether suicide attempt accounts for unique variance in AI, controlling for confounding risk domains, is extremely limited. This methodology does not address specificity of cause at the level of the risk factor. However, as a first pass we review this research to determine whether suicide attempts and AI share variance which does not overlap with potential confounding risk variables. First, among a sample of 1,325 nationally representative adolescents living in Greece (Madianos et al., 1994), suicide attempt in the previous year discriminated between problem and non-problem drinkers, controlling for internalizing traits (i.e., depressive symptoms), externalizing traits (i.e., other drug use and dropping out of school), and other covariates (e.g., family alcohol problems). Second, among a sample of 6,760 boys recruited from the greater Miami area (Vega, Zimmerman, Warheit, Apospori, & Gil, 1993), neither lifetime suicide attempt nor depressive symptoms was associated with an alcohol use composite (i.e., lifetime use, frequency of use, and age of alcohol initiation) controlling for externalizing traits (e.g., delinquency) and other covariates (e.g., peer approval of substance use, low family pride, and problematic family substance use), which were all uniquely associated with alcohol use. The extant data is inconclusive as to whether suicide attempt accounts for unique variance in AI.
Prospective survey studies
Only one study has investigated whether adolescent suicide attempt prospectively predicts AI controlling for at least one variable within a confounding risk domain. In this study, investigators analyzed data from a New Zealand birth cohort regarding the subsequent mental health outcomes of a suicide attempt made during adolescence (Fergusson, Horwood, Ridder, & Beautrais, 2005). Suicide attempt prior to age 18 did not predict alcohol dependence from ages 18 to 25 controlling for previously diagnosed depression, personality characteristics such as neuroticism and novelty seeking, and additional covariates assessed prior to 18 (e.g., deviant peer affiliations, prior SUD, family history of alcohol problems, childhood physical, sexual abuse and living situation). The investigators did not report the significance of depression or the covariates, limiting the ability to hypothesize which variable may have accounted for the AI-attempt relation. However, the main effects model was extended to include interactions between prior suicide attempt and gender in the prediction of later alcohol dependence and found that suicide attempt was unrelated to alcohol dependence for males but was associated with increased risk of subsequent alcohol dependence among females.
Summary
A→S
Cross-sectional studies collectively show that AI (i.e., frequency of drinking and intoxications, alcohol consequences, and alcohol abuse and dependence diagnoses) accounts for unique variance in adolescent suicide attempts controlling for variables within confounding risk domains (i.e., internalizing and externalizing domains). When the time interval between assessments is two years or shorter, longitudinal research suggests that AI (i.e., alcohol quantity-frequency and frequency of intoxication) uniquely predicts subsequent suicide attempt. Similar prospective studies on medically attended attempt do not exist.
S→A
Only three studies report findings concerning whether adolescent suicide attempt accounts for unique variance in AI (i.e., alcohol consequence, alcohol dependence diagnosis, and alcohol composite [lifetime use, frequency of use, and age of alcohol initiation]) controlling for at least one confounding risk domain and provide mixed findings regarding a unique effect. A single prospective study found no overall association between suicide attempt and subsequent alcohol dependence, but suicide attempt was predictive of later alcohol dependence among girls (but not among boys). Research examining the effect of adolescent medically attended attempt on AI, controlling for variables within the confounding risk domains, do not exist.
General Methodological Considerations
There are several methodological considerations relevant to modeling of (and inclusion of) confounding risk variables, to conducting formal tests of mediation, and to determining the generalizability of findings. First, authors of the studies reviewed above did not adequately model relevant variables that would facilitate testing whether third variables (e.g., broader externalizing) account for the AI-attempt relation. Although we did not compile an exhaustive list of confounding risk variables, studies typically controlled for few variables contained within the two domains, which limits the possibility of determining specificity of cause of the risk factor of interest (i.e., AI or suicide attempt). There were no relevant studies in which inherently mixed externalizing/internalizing conditions (e.g., BPD and bipolar I) were included as covariates. Indeed, it is possible that the combination of both externalizing and internalizing traits/behaviors (as evidenced by both BPD and mixed states in bipolar I disorder) represents a particularly potent type of disturbance leading to both suicide attempts and AI.
Given the range of psychopathology that is associated with both problematic alcohol use and suicide attempts, it is clear that demonstrating unique statistical associations after accounting for relevant confounds is not a trivial task. Clearly it would be desirable to systematically assess symptoms associated with all major Axis I disorders and Axis II disorders and include these as control variables (as either individual manifest disorder or broad-latent variables measuring the internalizing and externalizing domains) in statistical analyses. However, this approach is probably not practicable in most large survey studies where participant burden is great and budgets are pressed. Additionally, some efficient but broad symptom measures (e.g., symptom checklists) traditionally do a far better job of measuring internalizing rather than externalizing pathology (e.g., Gotlib, 1984). At a minimum, however, it would seem important to include problematic traits and those conditions are both prevalent and are comorbid with both conditions. For example, including assessments of emotional distress (e.g., symptom inventories) and current and past impulsive and antisocial behavior (e.g., drug use and delinquency inventories) represent useful markers covering a broad range of conditions and should control for the most egregious confounding.
Second, results from prior research point to robustness of the relation between AI and suicide attempt, but they do not provide information about the nature of this association. Specifically, studies lacked formal testing of mediation. A mediator is a third variable that accounts for the relationship between a predictor and a criterion (Barron & Kenny, 1986). Testing of mediated effects (Holmbeck, 1997) is useful for elucidating underlying processes and for identifying targets for intervention that could disrupt a causal chain. Such tests are needed to estimate both direct and indirect paths from S→ A and A→ S.
Finally, this research synthesis revealed that majority of studies, controlling for variables within multiple confounding risk domains, were conducted within the United States and were of a cross-sectional design, while the majority of somewhat controlled prospective studies were conducted in other countries (i.e., Hong Kong, New Zealand, Greece, and Norway). It is unknown whether the results from prospective studies conducted outside of the United States would be generalizable to American adolescents and, given large variability across countries in adolescent suicide (World Health Organization, 2008) and drinking patterns (Heath, 1995), U.S. based studies are needed.
Part 3: Recommendations and Implications
Informative Design
The extant data suggest that no single causal mechanism can account for the relation between AI and suicide attempts. Thus, researchers must evaluate a range of plausible models to gauge their relevance. Consideration of the multiple possible causal and non-causal mechanisms underlying the suicide/alcohol relation highlights the difficulty in deriving strong tests of mechanisms. It seems unlikely that a single “magic bullet” approach will be found and that the specification and validation of hypothesized mechanisms will involve a variety of different types of evidence.
Proximal effects
Short-term, event-based, longitudinal designs, such as case-crossover designs (Maclure & Mittleman, 2000) and daily diary studies (including ecological momentary assessment; EMA; Stone & Shiffman, 1994), may be useful for studying directionality and proximal mechanisms underlying the proximal alcohol use-attempt relation. Case-crossover studies assess individuals at the time of a target event (e.g., presenting to the ER after a suicide attempt; e.g., Borges et al., 2004) and also at a within-subject control event (e.g., a week or month earlier). This methodology is ideal for studying presumably more severe attempts (i.e., medically attended attempts) and could disentangle the causal link between suicide attempt and AI by assessing alcohol use immediately after a suicide attempt and also on a control day. The general logic of the case cross-over design can be extended to daily diary studies (including real-time electronic diaries such as in EMA) where data is collected prospectively and, in principle, could provide multiple case-crossovers within individuals. Participants in EMA studies provide data in-real time, typically multiple times per day, using a device such as a palmtop computer or personal digital assistant. EMA is a naturalistic approach that permits the identification of immediate antecedents (including both environmental and psychological variables) and the larger environmental context relevant to target events such as suicide attempt or even suicide ideation.
EMA studies in a population-based sample would require the use of very large samples for extended periods of time to observe sufficient suicide attempts to conduct meaningful statistical analyses. Thus, researchers must be thoughtful in the selection of participants who would be at risk for both alcohol use and suicide attempt during a relatively short observation period. Obviously, protective measures need to be taken when assessing participants at high-risk for suicide. An EMA study may be feasible using individuals enrolled in an intensive outpatient psychotherapy, such as Dialectical Behavior Therapy (Linehan, 1993), whereby protective measures such as daily check-ins or coaching calls are not foreign to the therapy. In fact, a recent EMA study has been conducted with borderline outpatients (Trull et al., in press). It might seem that individuals who are highly dysregulated, under extreme stress, or consuming alcohol are ill-suited to participate in EMA studies requiring high compliance rates “in the field.” However, experience to date clearly demonstrates that patients with major mental illness including schizophrenia (Myin-Germeys, Delespaul, & deVries, 2000), unspecified psychotic disorders (Myin-Germeys, Delespaul, & Van Os, 2005; Thewissen, Bentall, Lecomte, van Os, & Myin-Germeys, 2008), and bipolar disorder (Scharer et al., 2002) can employ this methodology to study dynamic aspects of pathology-relevant constructs and individuals can reliably use electronic diaries to record even high levels of drinking in the field (Hufford, Shields, Shiffman, Paty, & Balabanis, 2002). In fact, a recent EMA study (Trull et al., in press) measuring affective instability among those with BPD or current major depressive disorder (MDD), found high compliance rates across the two groups (BPD: 87% and MDD: 88%). Individuals with current suicidal ideation or behavior were not excluded from the study. We anticipate in the not-too-distant future, alcohol intoxication can be measured objectively, unobtrusively, and in real time (Swift, 1992; Webster & Gablor, 2007). Being able to integrate these objective measures of intoxication with suicide-related thoughts and behaviors will permit probing analyses of the potential role of alcohol in suicide-related behavior.
Both types of event-based designs permit “within-subject” analyses which hold constant fixed covariates and thus effectively rule out distal third-variable causation as a sole explanation for an alcohol use/suicide attempt relation. Within-subject effects cannot easily be attributed to directional distal processes except to the extent that they increase the likelihood of generating causative situational variables. For example, a distal heavy drinking pattern could increase risk for suicide not because of “allostatic” changes to the brain and hedonic tone (a hypothesized distal mechanism). Rather a distal heavy drinking pattern may increase the risk for a suicide attempt by increasing the number of occasions that an individual will experience a proximal event of alcohol intoxication.
If researchers are able to rule out temporally specific third variables in case-crossover designs, researchers can be confident that proximal processes underlying the alcohol-suicide relation exist. However, the traditional case-crossover design does not easily lend itself to the identification of mechanisms of action and resolution of the direction of effect. EMA provides a more flexible method for examining these mechanisms. For instance, participants could report on their suicide-related alcohol expectancies (S→A), and researchers could examine the extent to which appraisal of immediate stressors and possible solutions are altered by alcohol use prior to an attempt (A→S).
More complex mechanisms could also be examined. For example, alcohol may be particularly relevant during particular types of suicide attempts, (e.g., ambivalent attempts). Alcohol myopia theory (Steele & Josephs, 1990) suggests that, among individuals ambivalent about committing suicide, alcohol use would increase the salience of reasons to die while simultaneously decreasing the salience of inhibitory factors that produce the ambivalence. Clearly, this would increase the likelihood of a suicide attempt. In this regard, EMA studies would be an important adjunct to laboratory studies in establishing basic relations between drinking, cognitive restraint, and suicide attempt.
Obviously, it would be unethical to induce suicidal intent or ideation in a laboratory setting. However, laboratory studies may be a viable approach for studying hypothesized proximal mechanisms between acute intoxication and suicide attempts. For example, alcohol myopia theory suggests that alcohol intoxication would lead the drinker to focus on the most immediate, salient features of his environment with more distal features being less accessible. Thus, a depressed individual (in the absence of pleasant distracters) would be more likely to experience a “crying in one's beer effect” (Steele & Josephs, 1990). It could be hypothesized that, in the context of depression and a depressing environment, the most salient, depressogenic cues would be most influential and more distal concepts (e.g., adaptive problem solving, reasons for living) would be least accessible. Some have used mood induction to study hypothesized proximal processes in suicide attempt such as impaired problem solving and reasons for living (Turzo & Range, 1991; Williams, Barnhofer, Crane, & Beck, 2005), and this general strategy could be extended to examine the effect of acute alcohol intoxication on these proposed precursors of suicide attempt. Using these types of laboratory models we can experimentally manipulate the amount of alcohol consumed to see if there is a dose-response relation with alcohol, as both a main effect and as part of an interaction effect with both fixed covariates (e.g., history of prior attempt) and other independent variables (e.g., mood induction). In this way we can examine the effect of alcohol intoxication on mood-induced impaired problem-solving, hopelessness, accessibility of reasons for living, or any of a host of proposed mediators.
Although there is an extensive literature examining alcohol effects on basic aspects of cognition that could inform theory and research on suicide, no published study has examined the effect of acute intoxication on cognitive processes that are explicitly associated with suicidal behavior (see Hufford, 2001) and presumed to influence the probability of a suicide attempt. The viability of such an approach to assessing presumed mediating mechanisms is well demonstrated by a recent study by Nock & Banaji (2007) who used implicit measures of suicidal cognitions to assess automatic, implicit cognition (with respect to self-relevance and attitude) regarding suicide. Such measures could be used to characterize the effects of alcohol on the perceived valence of suicidal acts and inform theories that suggest that the conflict-reducing effects of alcohol (Steele & Southwick, 1985) might be especially relevant to understanding how alcohol might trigger suicidal actions in those who are highly ambivalent about suicide.
To reiterate, we are NOT proposing to induce or create suicidal ideation in a laboratory setting or to administer alcohol to individuals who are acutely suicidal. Also, we are not proposing to conduct alcohol challenges studies among adolescents or individuals who are severely alcohol dependent. As such, these studies would represent only partial tests of presumed mechanisms underlying the relation between adolescent acute intoxication and suicide attempt. However, such partial tests of hypothesized mechanisms can help to rule out plausible but unlikely mechanisms. For example, if alcohol doesn't affect impaired problem solving it is unlikely that this is a mechanism of action underlying the proximal alcohol-suicide attempt relation.
Distal effects
Although event-based and laboratory assessments have great potential for illustrating proximal mechanisms, long-term designs are needed to resolve slowly evolving distal processes (e.g., alcohol-induced neurological changes [A→S] or altered self-image [S→A]). Prospective panel designs allow researchers to temporally track suicide attempt and problematic drinking over time as well assess indices of distal neurological, social and cognitive changes. There are many longitudinal cohort studies examining mental health outcomes, but few focus on suicide attempts. It is important to consider enriching ongoing prospective studies by assessing suicide attempts using questions regarding intent (and by not solely assessing attempts in the context of major depression) as well as by tracking indices of distal changes that may mediate the AI/suicide attempt relation. Since there is some evidence that the distal effect of problematic drinking on suicide attempt may be observed for up to two years, it is imperative for mechanistic studies to have multiple waves of measurements within this two-year time frame. However, due to a dearth of prospective research, the ideal follow-up period to investigate the distal effect of suicide attempt on AI is unknown. In sum, researchers will need to create a network of proof, with different tiers of evidence, to establish the AI-attempt relation in terms of directionality, temporality, and mechanisms of action. Likely there is no “magic bullet” approach, and a multifaceted research program is required.
Conclusion
The association between AI and suicide attempts is complex and not fully understood. This is not surprising in that there is evidence that both trait and situational factors influence both behaviors and these two behaviors can influence each other. Indeed, different research strategies are probably needed for elucidating different aspects of the suicide attempt/alcohol relation. EMA studies could be especially useful for testing the plausibility of proximal directional influences of one behavior on the other and proximal mechanisms that may explain this association. These studies could be complemented by experimental, laboratory studies. As a whole, these types of studies, while useful for studying short-term processes, are not ideal for studying processes that play out over extended periods of time. In this case, panel or cohort studies might be especially useful for demonstrating the plausibility of more distal processes. Because of the limitations involved in each approach to studying suicidal attempts (i.e., case-control studies, case-crossover studies, cohort studies, EMA studies, and laboratory studies), a comprehensive menu of research strategies seem called for in order to feel confident in piecing together different parts of the puzzle. Although each research approach has limitations, when a collection of approaches can be employed (especially when the individual approaches share differing profiles of strengths and weaknesses) we are in a much stronger position to understand this complex problem.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. The child behavior profile: I. Boys aged 6-11. Journal of Consulting and Clinical Psychology. 1978;46(3):478–488. doi: 10.1037//0022-006x.46.3.478. [DOI] [PubMed] [Google Scholar]
- Anderson RN, Smith BL. Deaths: Leading causes for 2001. National Vital Statistics Report. 2003;52:1–86. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- Aseltine RH, DeMartino R. An outcome evaluation of the SOS suicide prevention program. American Journal of Public Health. 2004;94(3):446–451. doi: 10.2105/ajph.94.3.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barter JT, Swaback DO, Todd D. Adolescent suicide attempts: A follow-up study of hospitalized patients. Archives of General Psychiatry. 1968;19:523–527. doi: 10.1001/archpsyc.1968.01740110011002. [DOI] [PubMed] [Google Scholar]
- Bender E. Liability issues shape colleges' response to suicide attempts. Psychiatric News. 2006 June 2;:1. [Google Scholar]
- Bergman B, Brismar B. Characteristics of violent alcoholics. Alcohol and Alcoholism. 1994;29:451–457. [PubMed] [Google Scholar]
- Berman AL, Schwartz RH. Suicide attempts among adolescent drug users. American Journal of Diseases of Children. 1990;144:310–314. doi: 10.1001/archpedi.1990.02150270060026. [DOI] [PubMed] [Google Scholar]
- Best D, Manning V, Gossop M, Gross S, Strang J. Excessive drinking and other problem behaviours among 14-16 year old schoolchildren. Addictive Behaviors. 2006;31:1424–1435. doi: 10.1016/j.addbeh.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Borges G, Cherpitel C, MacDonald S, Giesbrecht N, Stockwell T, Wilcox H. A case-crossover study of acute alcohol use and suicide attempt. Journal of Studies on Alcohol. 2004;65:708–714. doi: 10.15288/jsa.2004.65.708. [DOI] [PubMed] [Google Scholar]
- Brent DA, Kolko DJ, Wartella ME, Boylan MB, Moritz G, Baugher M, et al. Adolescent psychiatric inpatients' risk of suicide attempt at 6-month follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:95–105. doi: 10.1097/00004583-199301000-00015. [DOI] [PubMed] [Google Scholar]
- Bryant ES, Garrison CZ, Valois RF, Rivard JC. Suicidal behavior among youth with severe emotional disturbance. Journal of Child and Family Studies. 1995;4:429–443. [Google Scholar]
- Bukstein OG, Glancy LJ, Kaminer Y. Patterns of affective comorbidity in a clinical population of dually diagnosed adolescent substance abusers. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:1041–1045. doi: 10.1097/00004583-199211000-00007. [DOI] [PubMed] [Google Scholar]
- Burge V, Felts M, Chenier T, Parrillo AV. Drug use, sexual activity, and suicidal behavior in U.S. High school students. Journal of School Health. 1995;65:222–227. doi: 10.1111/j.1746-1561.1995.tb03366.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Morbidity and Mortality Weekly Report. 2004;53:1–29. [Google Scholar]
- Centers for Disease Control and Prevention & National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) 2005 Retrieved January 15, 2007, from http://www.cdc.gov/ncipc/wisqars.
- Cavaiola AA, Lavender N. Suicidal behavior in chemically dependent adolescents. Adolescence. 1999;34:735–744. [PubMed] [Google Scholar]
- Clark DB, Parker AM, Lynch KG. Psychopathology and substance-related problems during early adolescence: A survival analysis. Journal of Clinical Child Psychology. 1999;28:333–341. doi: 10.1207/S15374424jccp280305. [DOI] [PubMed] [Google Scholar]
- Cohen-Sandler R, Berman AL, King RA. A follow-up study of hospitalized suicidal children. Journal of the American Academy of Child Psychiatry. 1982;21:398–403. doi: 10.1016/s0002-7138(09)60945-6. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Does drinking promote risky sexual behavior? A complex answer to a simple question. Current Directions in Psychological Science. 2006;15:19–23. [Google Scholar]
- Cooper M, Wood PK, Orcutt HK, Albino A. Personality and the predisposition to engage in risky or problem behaviors during adolescence. Journal of Personality and Social Psychology. 2003;84:390–410. doi: 10.1037//0022-3514.84.2.390. [DOI] [PubMed] [Google Scholar]
- Cosgrave E, Killackey E, Yung A, Buckby J, Godfrey K, Stanford C, et al. Depression, substance use and suicidality in help-seeking adolescents: A survey of prevalence. Australian Journal of Guidance and Counselling. 2004;14:162–175. [Google Scholar]
- Crews FT, Braun CJ, Hoplight B, Switzer RC, III, Knapp DJ. Binge ethanol consumption causes differential brain damage in young adolescent rats compared with adult rats. Alcoholism: Clinical & Experimental Research. 2000;24:1712–1723. [PubMed] [Google Scholar]
- Department of Health and Human Services. Healthy People 2010. With understanding and improving health and objectives for improving health. 2nd. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- Derogatis LR, Fitzpatrick M. The SCL-90-R, the Brief Symptom Inventory (BSI), and the BSI-18. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment: Volume 3: Instruments for adults. 3rd 2004. [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- DeSimone A, Murray P, Lester D. Alcohol use, self-esteem, depression, and suicidality in high school students. Adolescence. 1994;29:939–942. [PubMed] [Google Scholar]
- Donovan JE, Jessor R, Costa FM. Adolescent problem drinking: Stability of psychosocial and behavioral correlates across a generation. Journal of Studies on Alcohol. 1999;60:352–361. doi: 10.15288/jsa.1999.60.352. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, McCaffrey DF, Ghosh-Dastidar B, Longshore DL. New inroads in preventing adolescent drug use: Results from a large-scale trial of project ALERT in middle schools. American Journal of Public Health. 2003;93:1830–1836. doi: 10.2105/ajph.93.11.1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felix-Ortiz M, Munoz R, Newcomb MD. The role of emotional distress in drug use among Latino adolescents. Journal of Child amd Adolescent Substance Abuse. 1994;3:1–22. [Google Scholar]
- Fergusson DM, Horwood L, Ridder EM, Beautrais AL. Suicidal behaviour in adolescence and subsequent mental health outcomes in young adulthood. Psychological Medicine. 2005;35:983–993. doi: 10.1017/s0033291704004167. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Lynskey MT. Alcohol misuse and adolescent sexual behaviors and risk taking. Pediatrics. 1996;98:91–96. [PubMed] [Google Scholar]
- Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Archives of General Psychiatry. 2002;59:225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- Foley DL, Goldston DB, Costello J, Angold A. Proximal psychiatric risk factors for suicidality in youth: The great smoky mountains study. Archives of General Psychiatry. 2006;63:1017–1024. doi: 10.1001/archpsyc.63.9.1017. [DOI] [PubMed] [Google Scholar]
- Galaif ER, Sussman S, Newcomb MD, Locke TF. Suicidality, depression, and alcohol use among adolescents: A review of empirical findings. International Journal of Adolescent Medicine and Health. 2007;19:27–35. doi: 10.1515/ijamh.2007.19.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrison CZ, McKeown RE, Valois RF, Vincent ML, Murray L. Aggression, substance sue, and suicidal behaviors in high school students. American Journal of Public Health. 1993;83:179–184. doi: 10.2105/ajph.83.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfinkel BD, Froese A, Hood J. Suicide attempts in children and adolescents. American Journal of Psychiatry. 1982;139:1257–1261. doi: 10.1176/ajp.139.10.1257. [DOI] [PubMed] [Google Scholar]
- Glowinski AL, Bucholz KK, Nelson EC, Fu Q, Madden PA, Reich W, et al. Suicide attempts in an adolescent female twin sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1300–1307. doi: 10.1097/00004583-200111000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gmitrowicz A, Kolodziej-Maciejewska H. Dysfunction of the hypothalamo-pituitary-adrenal axis in adolescents after a suicide attempt. Archives of Psychiatry and Psychotherapy. 2002;4:37–51. [Google Scholar]
- Goldman MS, Del Boca FK, Darkes J. Alcohol expectancy theory: The application of cognitive neuroscience. In: Leonard KE, editor. Psychological theories of drinking and alcoholism. 2nd. New York: Guilford Press; 1999. pp. 203–246. [Google Scholar]
- Goldston DB. Measuring suicidal behavior and risk in children and adolescents. Washington, DC: American Psychological Association; 2003. [Google Scholar]
- Gotlib IH. Depression and general psychopathology in university students. Journal of Abnormal Psychology. 1984;93:19–30. doi: 10.1037//0021-843x.93.1.19. [DOI] [PubMed] [Google Scholar]
- Groholt B, Ekeberg O, Haldorsen T. Adolescents hospitalised with deliberate self-harm: The significance of an intention to die. European Child and Adolescent Psychiatry. 2000;9:244–254. doi: 10.1007/s007870070027. [DOI] [PubMed] [Google Scholar]
- Grossman DC, Milligan B, Deyo RA. Risk factors for suicide attempts among Navajo adolescents. American Journal of Public Health. 1991;81:870–874. doi: 10.2105/ajph.81.7.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris E, Barraclough B. Suicide as an outcome for mental disorders: A meta-analysis. British Journal of Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Hawton K. Assessment of suicide risk. British Journal of Psychiatry. 1987;150:145–153. doi: 10.1192/bjp.150.2.145. [DOI] [PubMed] [Google Scholar]
- Hawton K, Fagg J, Simkin S, Bale E, Bond A. Deliberate self-harm in adolescents in Oxford, 1985-1995. Journal of Adolescence. 2000;23:47–55. doi: 10.1006/jado.1999.0290. [DOI] [PubMed] [Google Scholar]
- Heath DB, editor. International handbook on alcohol and culture. Westport: Greenwood Press; 1995. [Google Scholar]
- Hinshaw SP. On the distinction between attentional deficits/hyperactivity and conduct problems/aggression in child psychopathology. Psychological Bulletin. 1987;101:443–463. [PubMed] [Google Scholar]
- Holmbeck GN. Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. Journal of Consulting and Clinical Psychology. 1997;65:599–610. doi: 10.1037//0022-006x.65.4.599. [DOI] [PubMed] [Google Scholar]
- Howard-Pitney B, LaFromboise TD, Basil M, September B, Johnson M. Psychological and social indicators of suicide ideation and suicide attempts in Zuni adolescents. Journal of Consulting and Clinical Psychology. 1992;60:473–476. doi: 10.1037//0022-006x.60.3.473. [DOI] [PubMed] [Google Scholar]
- Howard J, Lennings CJ, Copeland J. Suicidal behavior in a young offender population. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 2003;24:98–104. doi: 10.1027//0227-5910.24.3.98. [DOI] [PubMed] [Google Scholar]
- Hufford MR. Alcohol and suicidal behavior. Clinical Psychology Review. 2001;21:797–811. doi: 10.1016/s0272-7358(00)00070-2. [DOI] [PubMed] [Google Scholar]
- Hufford MR, Shields AL, Shiffman S, Paty J, Balabanis M. Reactivity to ecological momentary assessment: An example using undergraduate problem drinkers. Psychology of Addictive Behaviors. 2002;16:205–211. [PubMed] [Google Scholar]
- Jessor R, Jessor SL. Adolescent development and the onset of drinking. A longitudinal study. Journal of Studies on Alcohol. 1975;36:27–51. doi: 10.15288/jsa.1975.36.27. [DOI] [PubMed] [Google Scholar]
- Julien RM. A primer of drug action. 9th. New York: Worth Publishers; 2001. [Google Scholar]
- Kalafat J, Elias M. An evaluation of a school-based suicide awareness intervention. Suicide and Life-Threatening Behavior. 1994;24:224–233. [PubMed] [Google Scholar]
- Kamali M, Oquendo MA, Mann J. Understanding the neurobiology of suicidal behavior. Depression and Anxiety. 2001;14:164–176. doi: 10.1002/da.1062. [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Burleson JA, Goldberger R. Cognitive-behavioral coping skills and psychoeducation therapies for adolescent substance abuse. Journal of Nervous and Mental Disease. 2002;190:737–745. doi: 10.1097/00005053-200211000-00003. [DOI] [PubMed] [Google Scholar]
- Kandel DB. Stages and pathways of drug involvement: Examining the gateway hypothesis. New York: Cambridge University Press; 2002. [Google Scholar]
- Kazdin AE. Research design in clinical psychology. 3rd. Needham Heights, MA: Allyn & Bacon; 1998. [Google Scholar]
- Kebede D, Ketsela T. Suicide attempts in Ethiopian adolescents in Addis Abeba high schools. Ethiopian Medical Journal. 1993;31:83–90. [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kinkel R, Bailey CW, Josef NC. Correlates of adolescent suicide attempts: Alienation, drugs and social background. Journal of Alcohol and Drug Education. 1989;34:85–96. [Google Scholar]
- Koob GF, Le Moal M. Drug abuse: Hedonic homeostatic dysregulation. Science. 1997;278:52–58. doi: 10.1126/science.278.5335.52. [DOI] [PubMed] [Google Scholar]
- Koob GF, Le Moal M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology. 2001;24:97–129. doi: 10.1016/S0893-133X(00)00195-0. [DOI] [PubMed] [Google Scholar]
- Kotila L, Lonnqvist J. Adolescent suicide attempts: Sex differences predicting suicide. Acta Psychiatrica Scandinavica. 1988;77:264–270. doi: 10.1111/j.1600-0447.1988.tb05119.x. [DOI] [PubMed] [Google Scholar]
- Krajnc MS, Schmidt I, Gergoric A, Dogsa I. Suicide attempts in Slovenian juveniles, 1978-1994. Nordic Journal of Psychiatry. 1998;52:487–492. [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Kruesi MJP, Grossman J, Pennington JM, Woodward PJ, Duda D, Hirsch JG. Suicide and violence prevention: Parent education in the emergency department. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:250–255. doi: 10.1097/00004583-199903000-00010. [DOI] [PubMed] [Google Scholar]
- Laurent A, Foussard N, David M, Boucharlat J, Bost M. A 5-year follow-up study of suicide attempts among French adolescents. Journal of Adolescent Health. 1998;22:424–430. doi: 10.1016/s1054-139x(97)00262-0. [DOI] [PubMed] [Google Scholar]
- Lee YG, Abdel-Ghany M. American youth consumption of licit and illicit substances. International Journal of Consumer Studies. 2004;28:454–465. [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Adolescent suicide ideation and attempts: Prevalence, risk factors, and clinical implications. Clinical Psychology: Science and Practice. 1996;3:25–46. [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. Stigma as a barrier to recovery: The consequences of stigma for the self-esteem of people with mental illnesses. Psychiatric Services. 2001;52:1621–1626. doi: 10.1176/appi.ps.52.12.1621. [DOI] [PubMed] [Google Scholar]
- Lyon ME, Benoit M, O'Donnell RM, Getson PR, Silber T, Walsh T. Assessing African American adolescents' risk for suicide attempts: Attachment theory. Adolescence. 2000;35:121–134. [PubMed] [Google Scholar]
- Maclure M, Mittleman MA. Should we use a case-crossover design? Annual Review of Public Health. 2000;21:193–221. doi: 10.1146/annurev.publhealth.21.1.193. [DOI] [PubMed] [Google Scholar]
- Madianos MG, Gefou-Madianou D, Stefanis C. Adolescent drinking and alcohol-related problems in a nationwide general population. International Journal of the Addictions. 1994;29:1581–1599. doi: 10.3109/10826089409047952. [DOI] [PubMed] [Google Scholar]
- Mannenbach MS, Hargarten SW, Phelan MB. Alcohol use among injured patients aged 12 to 18 years. Academic Emergency Medicine. 1997;4:40–44. doi: 10.1111/j.1553-2712.1997.tb03641.x. [DOI] [PubMed] [Google Scholar]
- Manson SM, Beals J, Dick RW, Duclos C. Risk factors for suicide among Indian adolescents at a boarding school. Public Health Reports. 1989;104:609–614. [PMC free article] [PubMed] [Google Scholar]
- McKenry PC, Tishler CL, Kelley C. The role of drugs in adolescent suicide attempts. Suicide and Life-Threatening Behavior. 1983;13:166–175. doi: 10.1111/j.1943-278x.1983.tb00014.x. [DOI] [PubMed] [Google Scholar]
- Mehlenbeck R, Spirito A, Barnett N, Overholser J. Behavioral factors: Substance use. In: Spirito A, Overholser JC, editors. Evaluating and treating adolescent suicide attempters: From research to practice. San Diego, CA: Academic Press; 2003. pp. 113–146. [Google Scholar]
- Myin-Germeys I, Delespaul P, deVries MW. Schizophrenia Patients are more emotionally active than is assumed based on their behavior. Schizophrenia Bulletin. 2000;26:847–854. doi: 10.1093/oxfordjournals.schbul.a033499. [DOI] [PubMed] [Google Scholar]
- Myin-Germeys I, Delespaul P, Van Os J. Behavioral sensitization to daily life stress in psychosis. Psychological Medicine. 2005;35:733–741. doi: 10.1017/s0033291704004179. [DOI] [PubMed] [Google Scholar]
- Menninger KA. Man against himself. Oxford, England: Harcourt, Brace; 1938. [Google Scholar]
- Miller TR, Covington K, Jensen A. Costs of injury by major cause, United States, 1995: Cobbling together estimates. In: Mulder S, van Beeck EF, editors. Measuring the burden of injury. Amsterdam: ECOSA; 1999. pp. 23–40. [Google Scholar]
- Miller AL, Rathus JH, Linehan MM. Dialectical Behavior Therapy with Suicidal Adolescents. New York: Guilford Press; 2007. [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting & Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- Moran M. Lawsuit prompts college to end policy on suicide attempts. Psychiatric News. 2006 October 6;:27. [Google Scholar]
- Moscicki EK. Epidemiology of completed and attempted suicide: Toward a framework for prevention. Clinical Neuroscience Research. 2001;1:310–323. [Google Scholar]
- Nasser E, Overholser J. Assessing varying degrees of lethality in depressed adolescent suicide attempters. Acta Psychiatrica Scandinavica. 1999;99:423–431. doi: 10.1111/j.1600-0447.1999.tb00988.x. [DOI] [PubMed] [Google Scholar]
- National Institute of Alcohol Abuse and Alcoholism. Alcohol and development in youth—A multidisciplinary overview. Alcohol Research & Health. 20042005;28:112–120. [PMC free article] [PubMed] [Google Scholar]
- National Institute of Alcohol Abuse and Alcoholism. Neuroscience research and therapeutic targets. Alcohol Alert. 2004;61:1–6. [Google Scholar]
- Nisbett R, Ross L. Century Psychology Series. Upper Saddle River NJ: Prentice Hall; 1980. Human inference: Strategies and shortcomings of social judgment. [Google Scholar]
- Nock MK, Banaji MR. Prediction of suicidal ideation and attempts among adolescents using a brief performance-based test. Journal of Consulting and Clinical Psychology. 2007;75:707–715. doi: 10.1037/0022-006X.75.5.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Carroll PW, Berman A, Maris RW, Moscicki EK. Beyond the tower of Babel: A nomenclature for suicidology. Suicide and Life-Threatening Behavior. 1996;26:237–252. [PubMed] [Google Scholar]
- Otto U. Suicidal acts by children and adolescents. A follow-up study. Acta Psychiatrica Scandinavica. 1972;233:7–123. [PubMed] [Google Scholar]
- Overholser J, Spirito A. Precursors to adolescent suicide attempts. In: Spirito A, Overholser JC, editors. Evaluating and treating adolescent suicide attempters: From research to practice. San Diego, CA: Academic Press; 2003. pp. 19–41. [Google Scholar]
- Paluszny M, Davenport C, Kim WJ. Suicide attempts and ideation: Adolescents evaluated on a pediatric ward. Adolescence. 1991;26:209–215. [PubMed] [Google Scholar]
- Patterson G, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. American Psychologist. 1989;44:329–335. doi: 10.1037//0003-066x.44.2.329. [DOI] [PubMed] [Google Scholar]
- Pelkonen M, Marttunen M. Child and adolescent suicide: Epidemiology, risk factors, and approaches to prevention. Pediatric Drugs. 2003;5:243–265. doi: 10.2165/00128072-200305040-00004. [DOI] [PubMed] [Google Scholar]
- Perry CL, Williams CL, Veblen-Mortenson S, Toomey T, Komro K, Anstine PS, et al. Outcomes of a community-wide alcohol use prevention program during early adolescence: Project Northland. American Journal of Public Health. 1996;86:956–965. doi: 10.2105/ajph.86.7.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinstein MJ, La Greca AM. Childhood peer rejection and aggression as predictors of adolescent girls' externalizing and health risk behaviors: A 6-year longitudinal study. Journal of Consulting and Clinical Psychology. 2004;72:103–112. doi: 10.1037/0022-006X.72.1.103. [DOI] [PubMed] [Google Scholar]
- Putnins AL. Recent drug use and suicidal behaviour among young offenders. Drug and Alcohol Review. 1995;14:151–158. [Google Scholar]
- Reifman A, Windle M. Adolescent suicidal behaviors as a function of depression, hopelessness, alcohol use, and social support: A longitudinal investigation. American Journal of Community Psychology. 1995;23:329–354. doi: 10.1007/BF02506948. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Psychiatric comorbidity with problematic alcohol use in high school students. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:101–109. doi: 10.1097/00004583-199601000-00018. [DOI] [PubMed] [Google Scholar]
- Rossow I, Wichstrom L. Parasuicide and use of intoxicants among Norwegian adolescents. Suicide and Life-Threatening Behavior. 1994;24:174–183. [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Walker JU, Ferns W. Suicidal behavior among middle-class adolescents who seek crisis services. Journal of Clinical Psychology. 1996;52:137–143. doi: 10.1002/(SICI)1097-4679(199603)52:2<137::AID-JCLP3>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- Roy A. Risk factors for suicide in psychiatric patients. Archives of General Psychiatry. 1982;39:1089–1095. doi: 10.1001/archpsyc.1982.04290090071014. [DOI] [PubMed] [Google Scholar]
- Rudd M, Rajab M, Orman DT, Stulman DA, Joiner T, Dixon W. Effectiveness of an outpatient intervention targeting suicidal young adults: Preliminary results. Journal of Consulting and Clinical Psychology. 1996;64:179–190. doi: 10.1037//0022-006x.64.1.179. [DOI] [PubMed] [Google Scholar]
- Scharer LO, Hartweg V, Varlerius G, Graf M, Hoern M, Biedermann C, et al. Life charts on a palmtop computer: first results of a feasibility study with an electronic diary for bipolar patients. Bipolar Disorders. 2002;4:107–108. doi: 10.1034/j.1399-5618.4.s1.51.x. [DOI] [PubMed] [Google Scholar]
- Shaughnessy L, Doshi SR, Jones SE. Attempted suicide and associated health risk behaviors among Native American high school students. Journal of School Health. 2004;74:177–182. doi: 10.1111/j.1746-1561.2004.tb08217.x. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Grekin ER. Alcohol and affect regulation. In: Gross J, editor. Handbook of Emotion Regulation. New York: Guilford; 2007. pp. 560–580. [Google Scholar]
- Sher L. Alcoholism and suicidal behavior: A clinical overview. Acta Psychiatrica Scandinavica. 2006;113:13–22. doi: 10.1111/j.1600-0447.2005.00643.x. [DOI] [PubMed] [Google Scholar]
- Shneidman E. Definition of suicide. New York: Wiley; 1985. [Google Scholar]
- Sibthorpe B, Drinkwater J, Gardner K, Bammer G. Drug use, binge drinking and attempted suicide among homeless and potentially homeless youth. Australian and New Zealand Journal of Psychiatry. 1995;29:248–256. doi: 10.1080/00048679509075917. [DOI] [PubMed] [Google Scholar]
- Spirito A, Esposito-Smythers C. Cognitive behavioral therapy for adolescent suicidal behavior. In: Kendall, editor. Child and Adolescent Therapy: Cognitive-Behavioral Procedures. 3rd. New York: Guilford Press; 2005. [Google Scholar]
- Spirito A, Mehlenbeck R, Barnett N, Lewander W, Voss A. The relation of mood and behavior to alcohol use in adolescent suicide attempters. Journal of Child and Adolescent Substance Abuse. 2003;12:35–53. [Google Scholar]
- Spirito A, Plummer B, Gispert M, Levy S, Kurkjian J, Lewander W, et al. Adolescent suicide attempts: Outcomes at follow-up. American Journal of Orthopsychiatry. 1992;62:464–468. doi: 10.1037/h0079362. [DOI] [PubMed] [Google Scholar]
- Spirito A, Stark L, Fristad M, Hart K, Owens-Stively J. Adolescent suicide attempters hospitalized on a pediatric unit. Journal of Pediatric Psychology. 1987;12:171–189. doi: 10.1093/jpepsy/12.2.171. [DOI] [PubMed] [Google Scholar]
- Steele CM, Josephs RA. Alcohol myopia: Its prized and dangerous effects. American Psychologist. 1990;45:921–933. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- Steele CM, Southwick L. Alcohol and social behavior: I. The psychology of drunken excess. Journal of Personality and Social Psychology. 1985;48:18–34. doi: 10.1037//0022-3514.48.1.18. [DOI] [PubMed] [Google Scholar]
- Stewart S, Manion IG, Davidson S, Cloutier P. Suicidal children and adolescents with first emergency room presentations: Predictors of six-month outcome. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:580–587. doi: 10.1097/00004583-200105000-00018. [DOI] [PubMed] [Google Scholar]
- Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavorial medicine. Annals of Behavioral Medicine. 1994;16:199–202. [Google Scholar]
- Suominen K, Isometsa E, Henriksson M, Ostamo A, Lonnqvist J. Hopelessness, impulsiveness and intent among suicide attempters with major depression, alcohol dependence, or both. Acta Psychiatrica Scandinavica. 1997;96:142–149. doi: 10.1111/j.1600-0447.1997.tb09919.x. [DOI] [PubMed] [Google Scholar]
- Swift RM, Swette L. Assessment of ethanol consumption with a wearable, electronic ethanol sensor/recorder. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical models. Totowa, NJ: Humana Press; 1992. pp. 189–202. [Google Scholar]
- Thewissen V, Bentall RP, Lecomte T, van Os J, Myin-Germeys I. Fluctuations in self-esteem and paranoia in the context of daily life. Journal of Abnormal Psychology. 2008;117:143–153. doi: 10.1037/0021-843X.117.1.143. [DOI] [PubMed] [Google Scholar]
- Thompson EA, Eggert LL, Randell BP, Pike KC. Evaluation of indicated suicide risk prevention approaches for potential high school dropouts. American Journal of Public Health. 2001;91:742–752. doi: 10.2105/ajph.91.5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend JM, Rakfeldt J. Hospitalization and first-contact mental patients: Stigma and changes in self-concept. Research in Community and Mental Health. 1985;5:269–301. [Google Scholar]
- Trull TJ, Sher KJ, Minks-Brown C, Durbin J, Burr R. Borderline personality disorder and substance use disorders: A review and integration. Clinical Psychology Review. 2000;20:235–253. doi: 10.1016/s0272-7358(99)00028-8. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Solhan MB, Tragesser SL, Jahng S, Wood PK, Piasecki TM, Watson D. Affective instability: Measuring a core feature of borderline personality disorder using ecological momentary assessment. Journal of Abnormal Psychology. doi: 10.1037/a0012532. in press. [DOI] [PubMed] [Google Scholar]
- Turzo AP, Range LM. Reasons for living: Mood effects revisited. Journal of Applied Social Psychology. 1991;21:1161–1168. [Google Scholar]
- Vajda J, Steinbeck K. Factors associated with repeat suicide attempts among adolescents. Australian and New Zealand Journal of Psychiatry. 2000;34:437–445. doi: 10.1080/j.1440-1614.2000.00712.x. [DOI] [PubMed] [Google Scholar]
- Vega WA, Zimmerman RS, Warheit GJ, Apospori E, Gil AG. Risk factors for early adolescent drug use in four ethnic and racial groups. American Journal of Public Health. 1993;83:185–189. doi: 10.2105/ajph.83.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinson DC, Maclure M, Reidinger C, Smith GS. A population-based case-crossover and case-control study of alcohol and the risk of injury. Journal of Studies on Alcohol. 2003;64:358–366. doi: 10.15288/jsa.2003.64.358. [DOI] [PubMed] [Google Scholar]
- Volpicelli J, Balaraman G, Hahn J, Wallace H, Bux D. The role of uncontrollable trauma in the development of PTSD and alcohol addiction. Alcohol Research & Health. 1999;23:256–262. [PMC free article] [PubMed] [Google Scholar]
- Wagner BM, Cole RE, Schwartzman P. Comorbidity of symptoms among junior and senior high school suicide attempters. Suicide and Life-Threatening Behavior. 1996;26:300–307. [PubMed] [Google Scholar]
- Waldron HB, Slesnick N, Brody JL, Charles W, Thomas R. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. Journal of Consulting and Clinical Psychology. 2001;69:802–813. [PubMed] [Google Scholar]
- Weathermon R, Crabb DW. Alcohol and medication interactions. Alcohol Research & Health. 1999;23:40–51. [PMC free article] [PubMed] [Google Scholar]
- Webster G, Gabler HC. Assessment of dermal ethanol emission sensors: Experimental design. Biomedical Sciences Instrumentation. 2007;43:348–353. [PubMed] [Google Scholar]
- Wechsler H, Kuo M, Lee H, Dowdall GW. Environmental correlates of underage alcohol use and related problems of college students. American Journal of Preventive Medicine. 2000;19:24–29. doi: 10.1016/s0749-3797(00)00163-x. [DOI] [PubMed] [Google Scholar]
- Wichstrom L. Predictors of adolescent suicide attempts: A nationally representative longitudinal study of Norwegian adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:603–610. doi: 10.1097/00004583-200005000-00014. [DOI] [PubMed] [Google Scholar]
- Wichstrom L, Hegna K. Sexual orientation and suicide attempt: A longitudinal study of the general Norwegian adolescent population. Journal of Abnormal Psychology. 2003;112:144–151. [PubMed] [Google Scholar]
- Widiger TA, Frances AJ, Pincus HA, First MB, Ross R, Davis W. DSM-IV sourcebook. Vol. 1. Washington, DC: American Psychiatric Publishing; 1994. [Google Scholar]
- Williams J, Barnhofer T, Crane C, Beck A. Problem solving deteriorates following mood challenge in formerly depressed patients with a history of suicidal ideation. Journal of Abnormal Psychology. 2005;114:421–431. doi: 10.1037/0021-843X.114.3.421. [DOI] [PubMed] [Google Scholar]
- Windle M. Suicidal behaviors and alcohol use among adolescents: A developmental psychopathology perspective. Alcoholism: Clinical and Experimental Research. 2004;28:29S–37S. doi: 10.1097/01.alc.0000127412.69258.ee. [DOI] [PubMed] [Google Scholar]
- Windle RC, Windle M. An investigation of adolescents' substance use behaviors, depressed affect, and suicidal behaviors. Journal of Child Psychology and Psychiatry. 1997;38:921–929. doi: 10.1111/j.1469-7610.1997.tb01611.x. [DOI] [PubMed] [Google Scholar]
- Withers LE, Kaplan DW. Adolescents who attempt suicide: A retrospective clinical chart review of hospitalized patients. Professional Psychology: Research and Practice. 1987;18:391–393. [Google Scholar]
- Woodward LJ, Fergusson DM. Life course outcomes of young people with anxiety disorders in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1086–1093. doi: 10.1097/00004583-200109000-00018. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Country Reports and Charts. 2008 Retrieved February, 2008, http://www.who.int/mental_health/prevention/suicide/country_reports/en/print.html.
- Yip PS, Liu K, Lam T, Stewart SM, Chen E, Fan S. Suicidality among high school students in Hong Kong. Suicide and Life-Threatening Behavior. 2004;34:284–297. doi: 10.1521/suli.34.3.284.42772. [DOI] [PubMed] [Google Scholar]
- Yoder KA. Comparing suicide attempters, suicide ideators and nonsuicidal homeless and runaway adolescents. Suicide and Life-Threatening Behavior. 1999;29:25–36. [PubMed] [Google Scholar]