Abstract
Objective
To use a common ethnographic study protocol across five countries to provide data to confirm social and risk settings and risk behaviors, develop the assessment instruments, tailor the intervention, design a process evaluation of the intervention, and design an understandable informed consent process.
Design
Methods determined best for capturing the core data elements were selected. Standards for data collection methods were established to enable comparable implementation of the ethnographic study across the five countries.
Methods
The methods selected were participant observation, focus groups, open-ended interviews, and social mapping. Standards included adhering to core data elements, number of participants, mode of data collection, type of data collection instrument, number of data collectors at each type of activity, duration of each type of activity, and type of informed consent administered. Sites had discretion in selecting which methods to use to obtain specific data.
Results
The ethnographic studies provided input to the Trial’s methods for data collection, described social groups in the target communities, depicted sexual practices, and determined core opinion leader characteristics; thus providing information that drove the adaptation of the intervention and facilitated the selection of venues, behavioral outcomes, and community popular opinion leaders (C-POLs).
Conclusion
The described rapid ethnographic approach worked well across the five countries, where findings allowed local adaptation of the intervention. When introducing the C-POL intervention in new areas, local non-governmental and governmental community and health workers can use this rapid ethnographic approach to identify the communities, social groups, messages, and C-POLs best suited for local implementation.
Keywords: behavioral interventions, culture, developing nations, ethnography, qualitative data
Introduction
In November 1999, the US National Institute for Mental Health (NIMH) launched the NIMH Collaborative HIV/STD Prevention Trial (hereafter, the Trial), using an evidence-based community-level sexual behavior change HIV/sexually transmitted disease (STD) prevention intervention model adapted by Kelly and colleagues [1,2]. This model is based on the work of Rogers and colleagues [3,4], who examined and described how technological and behavioral innovations diffuse throughout a community, and how they are adopted, accepted, and become normative within populations. Rogers found that innovations are often first originated by a subset of community members who are its opinion leaders. These are the trusted trendsetters whose actions, attitudes, and views influence those of other community members. Expanding on the work of Rogers and colleagues [3,4], Kelly et al. [5], St Lawrence et al. [6] and Sikkema et al. [7] demonstrated the efficacy of such interventions with gay men, women, and adolescents in the United States.
Kelly [8] specified nine core elements that must be incorporated into a successful HIV/STD prevention programme on the basis of this diffusion of innovations model (for additional details, see ‘The community popular opinion leader HIV prevention programme: conceptual basis and intervention procedures’ [9] in this issue). Ensuring fidelity to these core elements is critical when this evidence-based intervention is adapted and adopted in new settings. In addition, ongoing monitoring of implementation of the intervention is important to ensure that the integrity of these core elements is maintained.
Ethnography is the study of the social and cultural norms, mores, values, and beliefs of a group of people, using primarily qualitative research methods [10–13]. Ethnography traditionally has required immersion in cultures and an extended period of field-based research. In the 1980s, models for rapid or focused ethnographic assessment were developed and applied in various research areas [14–21]. In these settings, participant observational data were combined with open-ended qualitative interview data, which permitted an in-depth exploration of such sensitive topics as substance abuse and sexual behavior. These more focused ethnographic assessments have permitted formative research to be conducted more rapidly, which is useful when tailoring and implementing interventions in a short timeframe. Formative research allows community involvement in the design of prevention and clinical trial protocols [22], probably leading to greater community acceptance. In addition, advances in analytical software have allowed for more systematic analysis of the data collected [23–27].
The Trial used an integrated methods approach, starting with a formative research phase using qualitative methods, to provide input into the design of the quantitative assessment and intervention. Rapid ethnography was part of the process used to achieve culturally sensitive adaptation and implementation of the intervention. This paper describes how simultaneous, rapid ethnography in five countries enabled researchers to adapt and tailor the community popular opinion leader (C-POL) intervention [9] to each unique study site. Even though the site researchers had extensive experience with different populations in their countries, the implementation of this particular behavior change model had not been attempted. It was thus ill-advised to make assumptions about target populations without conducting formative research to help in the adaptation of the intervention. Site-specific ethnographic and epidemiological data were needed to identify the populations at risk of HIV and STD that should be targeted with the intervention [28], the specific venues where the Trial should be conducted [29], and how the intervention should be tailored given the characteristics and sexual practices of the target populations in the venues.
Ethnographic study
The goals of the ethnographic study were to describe individuals’ sexual and HIV/STD knowledge as well as the sexual practices that put them at risk of HIV and STDs, healthcare practices and beliefs, health-seeking behavior, the social groups and interactions of individuals and settings where these interactions occur, characteristics of individuals who might make good popular opinion leaders, and suggestions for prevention messages. In addition, the ethnographic study provided a formative research opportunity to explore or assess specific issues as they arose during the conduct of the initial phases of the study. For example, one of the nine core elements defined by Kelly [8] is the identification of a venue that is a cohesive social setting in which opportunities to have social interactions are abundant, providing numerous occasions for risk-reduction conversations among an identified high-risk group of people. One contribution of the ethnographic study was input to the selection of these settings in each of the five country sites. The ethnography study thus identified community settings that were social gathering places, in each study country, using participant observation and focus groups or individual interviews. Study social settings selected and confirmed as study venues were: food markets with individually owned stalls in China; clusters of wine shops in slums in India; gathering points of young, high-risk people in barrios in Peru; vocational and trade school dormitories in Russia; and retail establishments in business centers of growth points in Zimbabwe (see ‘Selection of populations represented in the NIMH Collaborative HIV/STD Prevention Trial’ [29] for more detail on the site selection process and results).
Another critical element is the identification of natural leaders (innovators called ‘community popular opinion leaders’; C-POLs), whose opinions are valued by members of the community, to be trained to deliver the prevention messages. In each of the five international sites, the ethnographic studies established that popular individuals in communities, who were considered leaders, could be identified and recruited to participate in the intervention.
Ethnographic study objectives
This ethnographic study was designed to provide the dataset that was used to: (i) describe and confirm the social and risk settings and risk behaviors; (ii) develop the assessment instruments; (iii) tailor the intervention in the eight core topic areas described below; (iv) design a process evaluation of the intervention; and (v) design an understandable informed consent process. To standardize the ethnographic study across the five sites, a protocol including templates and a basic tool set was developed by Trial investigators representing each of the five country sites, the NIMH, and the data coordinating center (DCC). The protocol ensured that the components of the study, ethnographic methods, core topic areas and associated required elements, training materials and certification requirements, and data analysis plans, were implemented consistently at all study sites.
Ethnographic methods
Ethnographic methods and their associated standards were selected through input and consensus of a broad group consisting of both US and international representatives from each of the five country study sites, the NIMH, and the DCC. The ethnography protocol specified the definitions and procedures for the methods selected: participant observation, focus groups, interviews, social mapping, and archival data. Each of these dominant qualitative methods is associated with strengths and limitations, which vary among cultural groups. Some of the relevant strengths that we considered in selecting these methods for this Trial are:
Participant observation allows for the collection of behavioral data that people may take for granted so much that they find it difficult to explain in an interview. It also provides a basis from which to question, probe and clarify interview and focus group responses that contradict previous observations.
Focus groups are generally viewed as a method with strengths in eliciting normative data, and generating broad-sweep overviews of the issues of concern to the cultural groups or subgroups represented in the focus group.
Individual interviews are considered the optimal choice for collecting data on personal histories and experiences, particularly on sensitive topics.
Social mapping provides information about the names and relative locations of settings where members of the populations socialize and where conversations might be initiated. This information could be used to characterize risk and to develop realistic role play scenarios for each selected venue.
Archival or secondary document review provides insights into both basic facts about a cultural groups (e.g. age, sex, level of education), as well as information on a number of basic categories considered important by those who collect and maintain data on the group (e.g. who is considered to be a member of a household, what is considered as ‘income’).
Standards developed for each of the specified methods included: (i) the number and sampling of participants; (ii) the mode of data collection; (iii) the type of data collection instrument used; (iv) the number of data collectors present for each type of data collection activity; (v) the duration of each type of data collection activity; and (vi) the type of informed consent administered with the activity.
These data collection standards enabled comparable implementation of the ethnographic study across the five country sites. The data entry system included space for the researcher to indicate any variation from standard operating methods. Therefore, even though a focus group ideally included six to eight individuals, if fewer people attended, it was still possible to conduct the session and note the deviation in the number of participants. The data system also documented relevant information associated with the management of each source of data, such as the time when each task was performed and who conducted data translation, transcription, and coding.
Although standards were adopted for the specified methods, a method that may be a good choice in one cultural context may not elicit as much useful data in another, and, in any case, a researcher must always be alert to the fact that respondents are not always truthful and that simply asking questions may bias the response away from the truth [13]. For example, in many cultural contexts, sensitive information regarding individual sexual behavior is best collected using in-depth individual interviews with respondents, whereas information regarding sexual norms or mores is better gathered using focus groups, that is, holding group discussions among target group individuals or key informants and stakeholders. The ethnographic study was thus designed to include a core set of methods, but individual sites chose the appropriate methods to elicit specific elements of required information and each site’s ethnographic data collection plan specified the methods intended for use with different participant populations, focusing on different topics. For example, in focus group discussions in India, it was found that participants were reluctant to discuss sexual practices that were personal, but had lively discussions regarding sexual practices and mores when presented with scenarios or local stories describing characters in the community and their sexual practices [30]. Because different methods are associated with different strengths in different cultures, qualitative methods are often triangulated, a strategy in which data obtained from multiple sources and multiple methods on a similar topic are compared across methods. That practice was encouraged during this Trial. The standard methods agreed upon by the five study sites for the collection of data are described in greater detail below.
Participant observation
In the initial fieldwork, participant observation was used to describe where people congregated socially and how they behaved in social groups in different venues. Participant observation was an effective method for initially identifying the natural leaders in a group (the C-POL) who were later recruited and trained to deliver prevention messages to their friends and neighbors.
Behaviors of interest included how people reacted to each other, how they treated each other, which individuals seemed to be in charge or the center of attention, which individuals were greeted with respect, admiration or liking, and what happened when different members of the group left the venue. For example, when an individual entered a hair salon in Lima, and most of the people suspended what they were doing and focused on what that person was saying, and that person also knew the names of the people in the salon, that person was identified as a potential C-POL. In China, a person in the market stalls was identified as a potential C-POL when he or she walked around and visited with people in other stalls and seemed to have a lot of people dropping by his or her stall.
Participant observation was also useful for identifying opportunities for informal social interaction, one of Kelly’s core elements of the popular opinion leader intervention [8]. Using participant observation in Russia, study teams identified the specific times of day and places that students would meet informally. This confirmed that opportunities existed for C-POLs to deliver HIV/STD prevention messages to fellow students during implementation of the intervention.
Interviews
Open-ended, in-depth, or rapid assessment interviews were used to collect important data on the core topic areas. Key informants, gatekeepers, stakeholders, and potential target group members were asked some of the sample questions presented in Tables 1–8. Interviewers were able to tailor their questions to the interviewee; this approach thus yielded important information that would not have been elicited using close-ended questions. Key informants and stakeholders provided information not necessarily known to target group individuals, For example, in China, the ethnographers learned that doctors experienced an upsurge in patients in the STD clinics after International AIDS Day, indicating that the community’s awareness of STD or HIV was enhanced during certain events that resulted in additional health-seeking behavior by target group individuals (see Table 1 for example questions). In Zimbabwe, target group members interviewed in open-ended interviews, revealed that, although the traditional lines of communication about sexual issues were via paternal aunts and uncles, most young adults currently learn about sex and sexual practices through discussions with their friends and peers (see Table 3 for example questions). Therefore, because conversations about sex now occurred more often among friends and peers, a C-POL approach was likely to be feasible if peers rather than aunts and uncles were trained in Zimbabwe. In addition to collecting information that would help tailor the intervention and assessment, interviews with gatekeepers and stakeholders determined the best methods to engage their support for the study and intervention. Study sites wanted to ensure that these key community members would not obstruct implementation of the intervention in the communities.
Table 1.
Core topic area: sexual health data.
| Required elements |
| STD knowledge, attitudes, beliefs |
| HIV knowledge, attitudes, beliefs |
| Health-seeking behavior |
| Sample questions: STD knowledge, attitudes, beliefs |
| Please name all the STDs that you know of (ask questions below for each STD). |
| What are the different names for these STDs? |
| What are the symptoms/manifestations of each of these? |
| How are STDs transmitted? (Probe: Can STDs be transmitted through casual contact, e.g. touching, sharing food, kissing)? |
| Are some people more vulnerable than others to STDs? |
| Why? |
| How are STDs treated? |
| Are there things that people can do to treat their own STDs? |
| Are there any STDs that are incurable? |
| Do/how do STDs differ for men and women, in terms of symptoms, transmission, prevention, etc.? |
| In this community, is there a stigma attached to having or being treated for an STD? |
| How does one prevent getting STDs in the first place? (Probe for condom use, partner reduction, substance use-related gender, etc. issues) |
| Sample questions: HIV knowledge, attitudes, beliefs |
| What are the symptoms/manifestations of HIV/AIDS? |
| What terms are used to refer to HIV/AIDS? |
| How is HIV/AIDS transmitted? |
| Does having another STD affect your likelihood of acquiring HIV/AIDS? |
| How does one prevent getting AIDS in the first place? (Probe for condom use, partner reduction, substance use-related gender, etc. issues) |
| Does/how does AIDS differ for men and women, in terms of symptoms, transmission, prevention, etc.? |
| In this community, is there a stigma attached to having or being treated for HIV/AIDS? |
| Do you know anyone who has AIDS? |
| Sample questions: Health-seeking behavior for STDs |
| What STD symptoms lead people to seek care? |
| What providers are associated with STDs or reproductive tract infection care giving? |
| What are the factors associated with provider choice? |
| What are the barriers to seeking care (social, political, access, and gender-specific)? |
| What are the patterns of resort (self-treatment, self-medication, friends)? |
| Sample questions: Health-seeking behavior for HIV |
| How is HIV/AIDS treated (treatment-related questions)? |
| What can cure AIDS? |
| What symptoms lead people to seek care? |
| What providers are associated with HIV care giving? |
| What are the barriers to seeking care (social, political, access, and gender-specific)? |
| What are the patterns of resort (self-treatment, self-medication, friends)? |
| What are the factors associated with provider choice? |
STD, Sexually transmitted disease.
Table 8.
Core topic area: population profile.
| Required elements |
| (Note: This information will be provided primarily from secondary sources. The last section, on perspectives, may come from data collected from members of the community, including gatekeepers, stakeholders, key informants, and others) |
| Country and community-level sociodemographic data |
| Country-level HIV/AIDS and STD data |
| Healthcare service delivery system |
| Status of traditional and western medicine |
| Perspectives on HIV/AIDS and STDs |
| Sample questions: Country and community-level sociodemographic data elements |
| Population size by age and gender |
| Life expectancy |
| Literacy/education levels |
| Age of marriage |
| Age of sexual debut |
| Sample questions: Country-level HIV/AIDS and STD data |
| Sentinel data on HIV prevalence and STD prevalence |
| Age and gender distribution of reported AIDS cases |
| STD incidence |
| STD modes of transmission |
| Geographical distribution of HIV/AIDS infection |
| Sample questions: Community-level data |
| (Provide any of the above data that are available on city, village, and/or venue populations. Include available data on ethnic groups in venues, and specify groups) |
| Healthcare service delivery system |
| Status of traditional and western medicine |
| Percentage/relative share of public and private sources for healthcare |
| Physicians and nurses per capita |
| Structure of delivery system (level of centralization/decentralization) |
| Government per capita expenditure on healthcare |
| AIDS care costs (e.g. government health budget) |
| Perspectives on HIV/AIDS and STD (with additional emphasis on all ethnic groups within venues) |
| Sociocultural context |
| What social and cultural issues are known to have an effect on HIV/AIDS and STD transmission (e.g. circumcision, wife inheritance, dry sex)? |
| Political context |
| What has been the political response to HIV/AIDS in the country? STD? |
| Popular opinion: What has been the history of popular opinion about HIV/AIDS and STD? |
| Policy issues |
| What government policies address issues of HIV/AIDS and STD? What are the policies regulating access to contraceptives, including condoms? |
| Economic issues |
| What are seen as the economic costs of HIV/AIDS and STD? Are economic issues thought to influence risk behaviors? |
| Religious context |
| What are the dominant religious groups in the venues? What have these groups’ responses to HIV/AIDS and STD been? What is their position on condom use, sex education/family life education? |
STD, Sexually transmitted disease.
Table 3.
Core topic area: healthcare delivery and beliefs.
| Required elements |
| Sexual health information sources |
| Prevention and care services for STD/RTI, HIV |
| Access to condoms and STD information |
| Sample questions: Sexual health information sources |
| Where have you received your information about STD and AIDS? (Probe for IEC, governmental, community/NGO, or school-based programmes and mass media, social groups, religious, educational, marital/relational, familial, and other sources) |
| Do you feel that this information is accurate? Understandable? Sufficient? |
| What groups of people tend to rely on this source? (Probe for types of groups) |
| Are there any individuals who people tend to rely on for this kind of information? (Add to probe list for subsequent interviews) |
| Sample questions: Prevention and care services for STD/RTI |
| Who provides STD services (doctors, quacks, pharmacists)? |
| What is the system of referrals for STD/RTI at these facilities? |
| What is the availability of diagnostics for STD/RTI? |
| Are education and counseling services (including partner notification) available? |
| Are these facilities accessible (cost, hours of operation, location, privacy)? |
| Are condoms and/or STD medications available at these facilities? |
| What is the quality of care and treatment in these facilities? |
| Sample questions: Access to condoms and STD information |
| Who is supposed to have access to condoms? STD information (age restrictions)? |
| Is the cost of condoms acceptable? |
| Are condoms and STD information available at convenient hours? |
| Is the location of condoms and STD information good? |
| Is privacy an issue for people who seek condoms or STD information? |
IEC, information, education, and counseling services; NGO, non-governmental organization; RTI, reproductive tract infection; STD, sexually transmitted disease.
Focus groups
In each international site, focus groups were convened on specific topics, such as health behaviors, social groups, normative sexual practices and meanings, and C-POL characteristics. The groups were composed of six to eight members of the target population, and the discussion was guided by facilitators using probes that emerged from participant observation or interview data. This was an extremely potent technique for reaching consensus on a variety of topics. For example, not only was there consensus within focus groups at one site, but there was consensus across the five sites about many of the characteristics that contribute to someone being a natural leader and therefore a good C-POL. All sites agreed that natural leaders were respectful of traditions, yet open and good communicators. In addition, the ability to ‘keep secrets’, or ensure confidentiality during the discussion of sensitive issues, was seen as an important C-POL characteristic (see Table 5 for example questions).
Table 5.
Core topic area: community popular opinion leader characteristics.
| Required elements |
| Individual-level C-POL characteristics |
| Group-level characteristics |
| Group-level C-POL characteristics |
| Sample questions: Individual-level C-POL characteristics |
| (Ask questions for each name from C-POL probe list constructed from responses to questions in the social group core topic area) |
| Let’s talk a while about (name). |
| When you wish to discuss something with (name), do you go to her or him directly? |
| How do you get hold of (name) when you wish to discuss something? |
| Can most people go to (name) and talk to him or her directly? (Probe: Or do they need to go through someone else?) |
| Do you think many people consult with him or her? |
| Do you think (name) knows and talks with many people? |
| Sample questions: Group-level characteristics |
| (Ask questions for each group from group probe list) |
| We have talked about different groups of people, and some of the people who belong to these groups. |
| Who do you think are the most important members of (group name)? |
| Does (group name) have any relationship with (other group name)? What type? |
| Can someone in (group name) interact with someone in (other group name)? What type of interaction? |
| If someone is a member of (group name) and they want to get advice from (other group name), what do they have to do? |
| Do members of these groups tend to know one another and interact with one another? To what extent/frequency and on what topics? |
| Sample questions: C-POL characteristics |
| (Ask about each person from C-POL probe list) |
| What are (name)’s attitudes toward the (group name)? |
| How long has she or he been a member of (group name)? |
| How long has she or he lived in this community? |
| Do you know how she or he became a leader in this group? Please explain. |
| Is she or he knowledgeable about STD, HIV/AIDS? What are her or his beliefs about STD, HIV/AIDS? |
| If someone wanted to get a message out to people about how they might protect themselves from STD, HIV and AIDS, do you think she or he would be willing to help? |
| Is it easy for people to contact her or him? How do they go about it? |
| What does she or he do for a living? |
| How could I contact her or him? |
C-POL, Community popular opinion leader; STD, sexually transmitted disease.
Social mapping
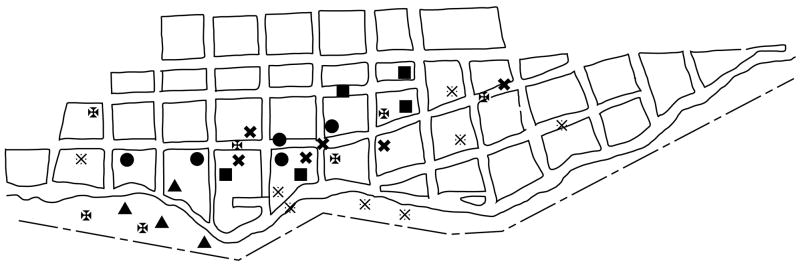
Social mapping permitted examination of the social dynamics in the communities and the identification of suitable venues in which to conduct the study. Ethnography team members conducted social mapping by observation, as well as through discussion during focus groups and individual interviews. Locations in the community where people were observed to congregate or where they used services or initiated risky behaviors were indicated on a map by different symbols (e.g. bars, ball fields, coffee houses, cafes, markets, stores, clinics, hair salons). Locations were confirmed in study sites through interview or focus group data. Such knowledge was important because this intervention requires the selection of venues with ample opportunities for informal conversations. These opportunities permit diffusion of the HIV/STD prevention messages delivered by the C-POL. Figure 1, a social map from Peru, shows different social settings (such as restaurants, sports fields, or other areas of congregation), sites that provide services (such as soup kitchens), and sites where risk behaviors occur (such as areas of prostitution). Such maps were used during intervention implementation to identify places to recruit C-POLs, conduct C-POL training, and place posters designed to stimulate conversations. In addition, social maps served as guides for process evaluation teams to conduct participant observation as part of the process evaluation, after the intervention had begun, to ensure that the C-POLs were having conversations, and to gauge community members’ reactions to the intervention and C-POL.
Fig. 1. Example social map of venue in Peru.
Leisure places: ■ Sports field,
 Group kitchen, ● Game playing, ◈ Restaurant/beer hall; Risky places, ▲ Prostitution, ✠ Hang out for delinquents, ✖ Hang out for drug users.
Group kitchen, ● Game playing, ◈ Restaurant/beer hall; Risky places, ▲ Prostitution, ✠ Hang out for delinquents, ✖ Hang out for drug users.
Archival data
In all study sites, archival data showing basic community demographics were collected. These data often came from official sources such as census data or, in the case of Russia, technical college enrollment data. These data included typical demographic information for the target communities, such as numbers of households, families, men and women, education, and socioeconomic status. In addition, STD and HIV data were collected from national or local health entities, such as ministries of health or from local clinics in study areas. These data were used to describe the community context.
Sampling
Sampling of participants for focus groups and individual interviews ranged from purposive, to snowball, to random. For example, the identification and recruitment of community stakeholders, or key informants, was done through a community entrée process conducted at each site, and included interviewing individuals from whom permissions were required, as well as selection through observations conducted by study ethnographers. Individuals selected for focus groups were largely selected purposively to include representatives of the target aged group, as well as community stakeholders. Individuals selected for in-depth or rapid assessment interviews were chosen purposively through observation, or snowball sampling dependent on previous interviewees’ input, as well as randomly in one case (Zimbabwe). Details on the selection and numbers of participants included in the ethnographic phase by country and method are provided in ‘Formative study conducted in five countries to adapt the community popular opinion leader’ [31] in this volume.
Assessment instruments
To collect data on sexual risk behaviors and social groups, the ethnography workgroup developed eight core topic areas. Each international site was required to develop site-specific data collection guides that covered the eight core topic areas and their required elements. The data collection guides were designed to be appropriate for the intended population. For example, interviews administered to community members in the venues had a different tone, and possibly a different set of questions, than those administered to stakeholders. These data collection guides provided instructions to the field staff, specific questions to be posed, and probes to elicit additional information. At each site, trained ethnographers collected data about the core topic areas and required elements using methods selected from among those described above.
Core topic areas and required elements
To elicit the data required to develop an assessment instrument and adapt the intervention, Trial researchers developed eight core topic areas, each with three or more required data elements to be collected at all sites. Core topic areas and required elements were agreed upon by consensus among ethnographers from all sites. For the core topic area on sexual health data, STD and HIV knowledge attitudes and beliefs, and health-seeking behavior were required elements. For sexual practices and meanings, dominant sexual practices, and sexual communication and condom use were required. With healthcare delivery and belief questions, sexual health information sources, and medical services, as well as condom access were required. For social groups, the types and characteristics of community and personal groups were required. C-POL characteristics were designed to obtain information about personal and group-level characteristics. When exploring appropriate reimbursement for the time required for study activities, the teams asked about reimbursement for study activities, as well as the appropriate amount and type of reimbursement and delivery format. When focusing on prevention messages, ethnographers were required to ask about behavior change experiences, including information sources and message types that encourage behavior change. In addition, archival data were used to describe population profiles. These core topic areas and their associated required elements and sample questions appear in the tables. Each international site was required to collect ethnographic data on each of the core topic areas and their required elements using one of more of the methods listed previously to ensure culturally appropriate data collection for their site and target population(s).
Training and certification
To ensure systematic and rigorous collection of ethnographic data, a one-week, centralized train-the-trainers workshop was conducted. A participatory learning approach was used in the training, with didactic presentations, role plays, and group critiques. Training materials were developed in English (the central ethnography training manual is available from study researchers on request), and the central training was conducted in English. Each site sent two to four staff members for this central training. During the course of the training, these staff members were provisionally certified to conduct in-country training of their ethnographic field staff. The trainers then returned to their individual country sites, developed translations of the training materials, and conducted on-site training of local ethnography staff. To ensure staffing quality standards were uniform, staff from the Trial’s DCC conducted a site visit, during which locally trained staff were individually questioned about the study design, standards adopted for each data collection method, and the process and content of informed consent. Copies of their initial (in most cases, feasibility) data were reviewed. Trained individuals who met the criteria were certified as competent to collect data, whereas those who did not demonstrate a satisfactory understanding of the protocol were retrained or reassigned to other project activities.
Data analysis plans
The creation of core topic areas and associated required elements facilitated the development of a basic hierarchical coding system. Hierarchical approaches to data coding and analysis are appropriate for the basic content and summary analysis that was required for the study. The use of topic areas also facilitated access to the data by members of the other working groups, because the set of required elements and illustrative questions for each topic provided a standard format for results at each site. To ensure some standardization and quality of data analysis among sites, an analysis plan requiring specific steps was developed at each site. These steps included basic data management, translation and transcription details, coding, and an assessment of intercoder agreement. The plan also specified who would conduct each step, the resources needed, and a timeline for the completion of all analyses.
The software used for data analysis varied among sites. Study sites chose software already available to them for the content analyses. Individual sites had quality control measures in place. Coders were trained extensively, using consensus to build coding validity. After coding of all interviews and focus group transcripts was conducted, subsamples were selected for double-coding. Coding discrepancies were resolved via consensus. In study sites where transcripts were translated, a subsample was selected for back-translation to verify meanings. The translation of summary results was required by all teams, but detailed coding in English for all sites was not. Study site needs for coded data were allowed to drive the level of coding and analysis. For example, data analysis needed within each site was more detailed than that needed across sites. For example, the risky behaviors of married men in India, Zimbabwe, and Peru were a major factor in HIV/STD transmission, but the Russian site had very few married men, thus study teams in the former list of countries had more detailed coding associated with these behaviors than Russia.
Data for cross-site comparisons were reported in English in summary format organized by core topic area and by required element within the core topic. The summaries were based on the individual site’s content analysis and were organized into matrices according to basic variables across sites. Each site used the software that the site researchers knew best, thus minimizing costs, time, and training needs for data analysis.
This standardized yet flexible approach resulted in the production of summary reports for cross-site comparisons, organized by core topic areas, and more detailed reports for use at each site. These reports constitute rich data repositories that have been accessed to answer questions emerging from different project activities.
Transcripts and coding structures were kept as part of the study record, such that summary data can be traced back to the coded data and further to the original data source (for example, transcription) as needed. Organizing the data in this way has enhanced the integration of ethnographic data within the Trial to meet the needs of the assessment and intervention workgroups, and help identify the process evaluation objectives. Details regarding the process evaluation are presented in ‘Methodological overview of a five-country community-level HIV/sexually transmitted disease prevention trial’ in this issue [32]. The ethnographic study was designed to inform different aspects of the Trial, but the data also have value as a source of information for health planners in the five countries.
Use of ethnographic data to inform design and procedures of the Trial
This section describes in more detail how the ethnographic studies in the five countries provided input that described behavioral outcomes, social groups in the target communities, and C-POLs, and drove adaptation of the intervention and facilitated the selection of venues. In addition, this section describes how ethnographic data impacted on the methods of data collection and assessment of the intervention via the process evaluation. Ethnographic data were integrated into the Trial protocols and procedures through interactions of study members from different Trial workgroups.
Ethnographic data used for selection of behavioral outcomes and tailoring the intervention
Behavioral outcomes for the Trial were selected on the basis of ethnographic data on sexual practices and risks at all five international study sites. Consistent findings across all sites showed that both women and men highlighted the role of sex inequities driving intracouple dynamics and sexual practices. Although none of the local cultures at the study sites condoned premarital or extramarital sex, double standards were documented in all study sites except Russia. Extramarital and premarital sex are tolerated among men, but not among women. The sex inequities documented mean that women are particularly vulnerable to STDs, including HIV, for several reasons. Attitudes toward condoms were consistently negative in all study sites, particularly for steady or marital relationships. Sex inequities also provide women limited opportunities for negotiation about expectations of monogamy or the use of condoms in a relationship. In all countries, women reported often being pressured or coerced to have sex. In some countries, particularly India, sexual and physical violence against women was common. The consistency of the ethnographic results on sexual practices identified the main behavioral outcome for the Trial: unprotected sexual acts with non-spousal partners.
Another need for ethnographic data emerged when epidemiological study data indicated that some venues did not have sufficient HIV/STD-related behavioral or biological risk to assess this behavior change intervention in those locations with a feasible sample size [28]. For those sites, ethnographers worked with the site’s study team to identify new venues where higher levels of risk existed. They were able to provide information because they had been collecting data on risk behavior, not only in the venues identified for probable inclusion in the Trial, but also in the larger community within which these venues were located. See ‘Selection of populations represented in the NIMH Collaborative HIV/STD Prevention Trial’ [29] for additional information on venue selection across the five international sites.
Ethnographic data were also used when adapting the intervention, including the selection of C-POLs and adaptation of the intervention training sessions by tailoring the training manual and curriculum. Cross-site ethnographic data established the following characteristics of an ideal C-POL: respectable, credible, life/sexual experience, trustworthy, empathetic, well-spoken, and self-confident. Ethnographic data also showed that, in all study sites, C-POLs could be identified and recruited to an HIV/STD prevention intervention. When tailoring the intervention manual and curriculum, ethnographic data helped to identify appropriate language for use in the manuals, helped with the choice of an intervention logo in each study site, identified social venues for the selection of C-POLs, and allowed the selection of C-POLs in intervention communities through participant observation and nomination. Ethnographic data allowed for site-specific tailoring in the selection of additional risk behaviors on which to focus prevention messages. Although all study sites focused on condom use with non-spousal partners, and on messages related to drinking and sexual risk, only some sites chose to include messages encouraging monogamy. Ethnographic data were also used to develop site-specific C-POL training, including examples of ways to initiate conversations and examples of C-POL conversations to promote targeted behaviors. Feedback from the ethnographic team showed that people at some study sites had lower levels of knowledge about HIV and STD, thus allowing tailoring of intervention C-POL training modules to include more information about HIV and STDs. Therefore, in Russia and India, an additional fifth training module included information about HIV and STDs, whereas four intervention training sessions were shown to be sufficient in China, Zimbabwe, and Peru.
Ethnographic data used for study design and assessment methods
In addition, ethnographic data provided information for a better design of the informed consent process, to select the final mode of data collection, and to flow into the process evaluation. An early, important decision facing the Trial was the possible use of audio computer-assisted self-interviewing (ACASI) as the mode of data collection [33]. An ACASI feasibility study was designed and implemented to compare ACASI with computer-assisted personal interviewing [34]. At the end of the study interviews, the ethnographers conducted exit interviews with study participants, using structured open and close-ended interview guides to probe for respondent comfort with and preference for the two interview modes. These cross-site data were analysed, summarized, and provided input when deciding which interview mode to use for the Trial. Similarly, when concerns arose about developing an informed consent process that was comprehensible in the five sites, the ethnography teams added questions to the exit interviews to assess comprehension of the informed consent process. Sites were able to use data from these exit interviews to improve their informed consent process.
Ethnographic methods were also used to implement the process evaluation that monitored implementation of the intervention. Observational data were collected regarding the logos and HIV/STD prevention messages displayed in communities, and whether or not C-POLs wore articles of clothing with the intervention logo, which were provided to them as part of the intervention to stimulate questions. In addition, process evaluation team members at some sites conducted brief intercept interviews to assess exposure to the intervention among community members and exposure to prevention messages, from both the identified C-POL and additional non-governmental or governmental agencies conducting HIV/AIDS or STD prevention programmes.
In conclusion, this study used a focused ethnography approach to collect data that were important in the overall design of the Trial and specifically in the design of the intervention and the assessment. Although the core topic areas, required elements, and specification of the methods to be used were standard across sites, each site was encouraged to tailor the data collection guides to meet the cultural characteristics of the local study population [35]. The ethnographic study used an iterative approach for data collection and analysis, which was well suited to collect data on the core topic areas and to respond to the emerging needs of the steering committee and other Trial workgroups for information needed to address issues related to the study design.
Lessons learned
An integrated, qualitative–quantitative approach is key to the successful adaptation of an intervention, especially when tailoring an intervention such as the C-POL model to new contexts. The rapid ethnographic approach described in this paper worked well, as results across the five country sites arrived at similar, yet distinctive, findings that allowed the local adaptation of the intervention. Data collected on sexual practices via the ethnography study were validated with epidemiological studies using quantitative computer-assisted methods for data collection (see ‘Sexually transmitted disease and HIV prevalence and risk factors in concentrated and generalized HIVepidemic settings’ in this issue [28]). Methods used in the ethnographic study to identify characteristics of popular opinion leaders, and popular individuals were later used by the intervention teams in all study sites to identify and recruit C-POLs.
When introducing the C-POL intervention in new areas, it will be necessary to train local non-governmental and governmental health and community workers to use this rapid ethnographic approach, which can help focus intervention adaptation by identifying which communities, social groups, messages, and C-POLs are best suited for the intervention. This article presents a prototypical approach for identifying the domains in which the rapid collection of ethnographic data are needed to adapt the C-POL model to different contexts. Ethnographic data collected during a formative phase will feed into the adaptation of the intervention, and can also be used in designing evaluations of the C-POL intervention implementation.
Table 2.
Core topic area: sexual practices and meanings.
| Required elements |
| Dominant sexual practices |
| Condom use |
| Sexual communication and negotiation |
| Sample questions: Dominant sexual practices |
| What are the different types of sexual practices? |
| What terminology, safer/riskier sex practices, partner definitions, disease definitions are used? |
| Describe the types of sexual and safer/riskier sex practices that men and women like. |
| Describe same-gender and opposite-gender perceptions of and attitudes towards same-gender sex. |
| How do different types of relationships influence sexual and safer/riskier sex practices? |
| What are the differences across different types of relationships (e.g. committed versus non-committed versus commercial; same versus opposite gender) |
| Sexual initiation |
| At what age do young men and women (in this venue) have their first sexual experience? |
| Are the first sexual experiences usually with a person of the same or different age? (Comment: Need to be sensitive to potential differences between normative perceptions and personal experiences) |
| Sample questions: Condom use |
| Barriers and facilitators of condom use (probe for desire for children, religious factors). |
| What are the plusses and minuses (advantages or disadvantages) of condom use? Advantages and disadvantages of condom use with different types of partners? Probe: What about how the feel of condoms influences use (dislike condom feel, smell, etc.)? |
| How does condom use vary with different types of relationships (spouse, casual partner, sex worker)? |
| What makes it easier or harder to use condoms? |
| Probe: What factors during sexual activity influence condom use (substance use, heat of the moment)? |
| Probe: What access issues influence condom use (cost, location of supply, hours of operation, privacy)? |
| What are the sociocultural influences on condom use (e.g., religious, educational, media, marital/relational, familial)? |
| Who supports or does not support (or encourages or discourages) condom use? |
| Sample questions: Sexual communication and negotiation |
| Probe for sexual and safer/riskier sex communication and negotiation patterns: |
| Gender, ethnic, or group differences |
| Sex and conflict resolution patterns |
| Sexual coercion and violence |
Table 4.
Core topic area: social groups.
| Required elements |
| Types of personal groups |
| Types of community groups |
| Characteristics of personal and community groups |
| Sample questions: Types of personal groups |
| What are the personal social groups to which individuals belong? (Probe for each type from list below) |
| Kin, work, school |
| Casual relationships, friendships |
| Sexual relationships, exchange |
| Any other? |
| Sample questions: Types of community groups |
| What are the community groups to which individuals belong? (Probe for each type from list below) |
| Organizations |
| Institutions |
| Meeting or gathering places |
| Any other? |
| What community groups exist in the venue? How many are they? |
| Formal/structured: |
| Places of worship, clubs, bars |
| Schools, places of work |
| Informal/unstructured: |
| Sports fields |
| Local hangouts |
| Any other? |
| Sample questions: Specific characteristics of each type of group (personal and community) |
| How many people are in the group? |
| What are the boundaries of the group? |
| How does someone become a member of this group (for each type listed)? |
| What kinds of characteristics must a person have to be a member of the group? |
| How stable is the membership of the group? |
| What topics are discussed within the group? |
| Health? |
| Sex? |
| HIV/AIDS/STD? |
| Condoms? |
| Intravenous drug/substance abuse? |
| (From the above responses, create group probe list for subsequent interviews) |
| Whose opinions about the above topics are most valued? (Note: Use names to create C-POL probe list for subsequent interviews) |
| What is the name given to different spheres of influence? |
| What makes him or her be someone that people respect and look to for advice? |
| Overall, what are some of the characteristics of the people who tend to have leadership roles? |
| Is there anyone else that you can think of whom you haven’t already mentioned that you feel is someone who is influential in this community, knows a lot of people and who would be a good person to get messages out to others in the community? |
C-POL, Community popular opinion leader; STD, sexually transmitted disease.
Table 6.
Core topic area: appropriate reimbursements.
| Required elements |
| Reimbursement experiences |
| Appropriate amount and type of reimbursement |
| Reimbursement delivery format |
| Sample questions |
| What is done in this community to show that something is appreciated? |
| Have there been any projects or studies conducted in this area in which people were asked to answer questions in an interview or meeting? If so, did they provide something to the people who answered questions to show their appreciation? |
| What would be considered an appropriate sign of appreciation when someone helps by answering questions? |
| Would it be better to offer money or a gift? What amount or type? |
| Who should provide the reimbursement and how should it be given? |
Table 7.
Core topic area: prevention messages.
| Required elements |
| Behavior change experiences |
| Information sources for behavior change |
| Message types for behavior change |
| Sample questions: Behavior change experiences |
| When was the last time that you tried to change something you do in order to improve your health? |
| What did you do (stop smoking, drink less, change diet, etc.)? |
| What helped you to make the decision to change? |
| How do you think others could improve their health? |
| Sample questions: Information sources for behavior change |
| Who should provide information on how to improve your health? |
| Who should provide information on how to prevent STD? |
| Sample questions: Message types for behavior change |
| What types of messages do people think are the most believable? |
STD, Sexually transmitted disease.
References
- 1.Kelly J. Community-level interventions are needed to prevent new HIV infections. Am J Public Health. 1999;89:299–301. doi: 10.2105/ajph.89.3.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelly J, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, et al. Randomized, controlled, community-level HIV prevention intervention for sexual risk behavior among homosexual men in U.S. cities. Lancet. 1997;350:1500–1505. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- 3.Rogers EM. Diffusion of innovations. 4. New York: Free Press; 1995. [Google Scholar]
- 4.Rogers EM, Shoemaker FF. Communication of innovations: a cross-cultural approach. New York: Free Press; 1971. [Google Scholar]
- 5.Kelly JA, St Lawrence JS, Diaz YE, Stevenson LY, Hauth AC, Brasfield TL, et al. HIV risk behavior reduction following intervention with key opinion leaders of a population: an experimental analysis. Am J Public Health. 1991;81:168–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.St Lawrence JS, Brasfield TL, Diaz YE, Jefferson KW, Reynolds MT, Leonard MO. Three-year follow-up of an HIV risk-reduction intervention that used popular peers [Research letter] Am J Public Health. 1994;84:2027–2028. doi: 10.2105/ajph.84.12.2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sikkema KJ, Kelly JA, Winett RA, Solomon LJ, Cargill VA, Roffman RA, et al. Outcomes of a randomized community-level HIV prevention intervention for women living in 18 low-income housing developments. Am J Public Health. 2000;90:57–63. doi: 10.2105/ajph.90.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelly JA. Popular opinion leaders and HIV prevention peer education: resolving discrepant findings, and implications for the development of effective community programmes. AIDS Care. 2004;16:139–150. doi: 10.1080/09540120410001640986. [DOI] [PubMed] [Google Scholar]
- 9.NIMH Collaborative HIV/STD Prevention Trial Group. The community popular opinion leader HIV prevention programme: conceptual basis and intervention procedures. AIDS. 2007;21(Suppl 2):S59–S68. doi: 10.1097/01.aids.0000266458.49138.fa. [DOI] [PubMed] [Google Scholar]
- 10.Farmer P. AIDS – talk and the constitution of cultural models. Soc Sci Med. 1994;38:801–809. doi: 10.1016/0277-9536(94)90152-x. [DOI] [PubMed] [Google Scholar]
- 11.Herdt G, Boxer A. Ethnographic issues in the study of AIDS. J Sex Res. 1991;28:171–187. [Google Scholar]
- 12.Pequegnat W, Page JB, Strauss A, Amaro H, Goldstein P, Fritz RB, et al. Qualitative inquiry: an underutilized approach in AIDS research. In: Pequegnat W, Stover E, editors. How to write a successful research grant. New York: Plenum; 1995. pp. 97–111. [Google Scholar]
- 13.Schensul JJ, LeCompte MD, editors. Ethnographer’s toolkit. Lanham, MD: AltaMira Press; 1999. [Google Scholar]
- 14.Bentley ME, Pelto GH, Straus WL, Schumann DA, Adegbola C, de la Pena E, et al. Rapid ethnographic assessment: application in a diarrhea management program. Soc Sci Med. 1988;27:107–116. doi: 10.1016/0277-9536(88)90168-2. [DOI] [PubMed] [Google Scholar]
- 15.Chambers R. Shortcut and participatory methods for gaining social information for projects. In: Cernea M, editor. Putting people first: sociological variables in rural development. New York: Oxford University Press for the World Bank; 1991. pp. 515–537. [Google Scholar]
- 16.Gittelsohn JP, Pelto PJ, Bentley ME, Bhattacharyya K, Jensen JL. Rapid assessment procedures(rap) – ethnographic methods to investigate women’s health. International Nutrition Foundation; Boston: 1998. [Google Scholar]
- 17.Herman E, Bentley ME. Manuals for ethnographic data collection: experience and issues. Soc Sci Med. 1992;35:1369–1378. doi: 10.1016/0277-9536(92)90040-w. [DOI] [PubMed] [Google Scholar]
- 18.Handwerker WP. Quick ethnography: a guide to rapid multi-method research. Lanham, MD: AltaMira Press; 2001. [Google Scholar]
- 19.Pelto PJ, Pelto GH. Studying knowledge, culture, and behavior in applied medical anthropology. Med Anthropol Q. 1997;11:147–163. doi: 10.1525/maq.1997.11.2.147. [DOI] [PubMed] [Google Scholar]
- 20.Scrimshaw SC, Hurtado E. Rapid assessment procedures for nutrition and primary health care: anthropological approaches to improving programme effectiveness. Reference Series. Vol. 11. Los Angeles, CA: UCLA Latin American Center; 1987. [Google Scholar]
- 21.Tashima N, Crain C, O’Reilly K, Elifson KW. The Community Identification (CID) process: a discovery model. Qual Health Res. 1996;6:23–48. [Google Scholar]
- 22.Corneli AL, Piwoz E, Bentley ME, Moses A, Nkhoma JR, Tohill BC, et al. Involving communities in the design of clinical trial protocols: the BAN Study in Lilongwe, Malawi. Contemp Clin Trials. 2007;28:59–67. doi: 10.1016/j.cct.2006.08.003. e-pub ahead of press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bernard HR. Social research methods: qualitative and quantitative approaches. Thousand Oaks, CA: Sage Publications, Inc; 1999. [Google Scholar]
- 24.Schensul JJ. Organizing community research partnerships in the struggle against AIDS. Health Educ Behav. 1999;26:266–283. doi: 10.1177/109019819902600209. [DOI] [PubMed] [Google Scholar]
- 25.Trotter RT. Ethnographic research methods for applied medical anthropology. In: Hill CE, editor. Training manual in applied medical anthropology, American Anthropological Association special publication no. 27. Arlington, VA: American Anthropological Association; 1991. [Google Scholar]
- 26.Trotter RT. Anthropological midrange theories in mental health research: selected theory, methods, and systematic approaches to at-risk populations. Ethos. 1997;25:259–274. [Google Scholar]
- 27.Ulin P, Robinson E, Tolley E, McNeill E, editors. Qualitative methods: a field guide for applied research in sexual and reproductive health. Research Triangle Park, NC: Family Health International; 2002. [Google Scholar]
- 28.NIMH Collaborative HIV/STD Prevention Trial Group. Sexually transmitted disease and HIV prevalence and risk factors in concentrated and generalized HIV epidemic settings. AIDS. 2007;21(Suppl 2):S81–S90. doi: 10.1097/01.aids.0000266460.56762.84. [DOI] [PubMed] [Google Scholar]
- 29.NIMH Collaborative HIV/STD Prevention Trial Group. Selection of populations represented in the NIMH Collaborative HIV/STD Prevention Trial. AIDS. 2007;21(Suppl 2):S19–S28. doi: 10.1097/01.aids.0000266454.26268.90. [DOI] [PubMed] [Google Scholar]
- 30.Sivaram S, Lakshmi CS, Go V, Srikrishnan AK, Celentano DD, Solomon S, Bentley ME. Telling stories: narrative scenarios to assess sexual norms for an HIV prevention study in Chennai, India. In: Verma RK, Pelto PJ, Schensul SL, Joshi A, editors. Sexuality in the time of AIDS: contemporary perspectives from the communities in India. New Delhi: Sage Publications; 2004. [Google Scholar]
- 31.NIMH Collaborative HIV/STD Prevention Trial Group. Formative study conducted in five countries to adapt the community popular opinion leader intervention. AIDS. 2007;21(Suppl 2):S91–S98. doi: 10.1097/01.aids.0000266461.33891.d0. [DOI] [PubMed] [Google Scholar]
- 32.NIMH Collaborative HIV/STD Prevention Trial Group. Methodological overview of a five-country community-level HIV/sexually transmitted disease prevention trial. AIDS. 2007;21(Suppl 2):S3–S18. doi: 10.1097/01.aids.0000266453.18644.27. [DOI] [PubMed] [Google Scholar]
- 33.Strader L. Development of a multilingual survey instrument in audio computer-assisted self-interviewing (ACASI). Presented at the Annual Meeting of the American Public Health Association; Atlanta, Georgia. 2001. [Abstract 28287] [Google Scholar]
- 34.NIMH Collaborative HIV/STD Prevention Trial Group. The feasibility of audio computer-assisted self-interviewing in international settings. AIDS. 2007;21(Suppl 2):S49–S58. doi: 10.1097/01.aids.0000266457.11020.f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Needle R, Trotter R, Goosby E, Bates C, Von Zinkernagel D. Methodologically sound rapid assessment and response: providing timely data for policy development on drug use interventions and HIV prevention. Int J Drug Policy. 2000;11:19–23. [Google Scholar]