Abstract
Effective management of human cryptosporidiosis requires efficient methods for detection and identification of the species of Cryptosporidium isolates. Identification of isolates to the species level is not routine for diagnostic assessment of cryptosporidiosis, which leads to uncertainty about the epidemiology of the Cryptosporidium species that cause human disease. We developed a rapid and reliable method for species identification of Cryptosporidium oocysts from human fecal samples using terminal restriction fragment polymorphism (T-RFLP) analysis of the 18S rRNA gene. This method generated diagnostic fragments unique to the species of interest. A panel of previously identified isolates of species was blind tested to validate the method, which determined the correct species identity in every case. The T-RFLP profiles obtained for samples spiked with known amounts of Cryptosporidium hominis and Cryptosporidium parvum oocysts generated the two expected diagnostic peaks. The detection limit for an individual species was 1% of the total DNA. This is the first application of T-RFLP to protozoa, and the method which we developed is a rapid, repeatable, and cost-effective method for species identification.
Over the last 20 years, Cryptosporidium has been identified as one of the three most common enteropathogens causing waterborne disease in both immunocompromised and immunocompetent individuals (19). Human cryptosporidiosis has been reported in all regions of the world, and prevalence rates range from 1 to 30% (8, 12). Ninety percent of reported cases are caused by two of the five Cryptosporidium species that can cause human disease, the anthroponotic species Cryptosporidium hominis and the zoonotic species Cryptosporidium parvum (16, 18, 28).
Understanding the dynamics of human cryptosporidiosis requires species identification, so that transmission routes and contamination sources can be identified. C. parvum and C. hominis are morphologically indistinguishable, and consequently species can be identified only by using molecular techniques. DNA sequencing is the “gold standard” for identification, but it is too time-consuming and expensive for routine diagnostics. More rapid and cost-effective methods, such as restriction fragment length polymorphism (RFLP) analysis, are often used (5, 18, 25). The efficacy of RFLP analysis depends on the availability of diagnostic restriction sites and a suitably high titer of parasites. Diagnosis of low-level or mixed infections is more difficult, and the analysis may underestimate the contribution of each species to human disease and misidentify contamination sources. Hence, there is a need to develop sensitive and discriminatory diagnostic methods for identification of Cryptosporidium species.
Terminal RFLP (T-RFLP) analysis is a fluorescence-based PCR technology that has been used to measure demographic complexity and biodiversity in bacterial communities, including communities from marine environments, soil, groundwater, gut microbiota, and feces (3, 6, 14, 15, 17, 23, 24). T-RFLP analysis relies on polymorphisms in the positions of restriction sites relative to the position of a fluorescently tagged primer. The use of a single fluorescent primer limits the analysis to the terminal restriction fragment (T-RF) in a target DNA molecule (15). Samples can be analyzed using capillary electrophoresis and an automated DNA sequencer, which allows fine-scale size resolution and quantification of T-RF abundance (7). Variation in the sizes of T-RFs of different species enables differentiation.
Because T-RFLP is fast, sensitive, and amenable to high-throughput analysis (7, 10, 24), it warrants investigation as a diagnostic tool for Cryptosporidium. This paper describes the use of T-RFLP analysis to identify Cryptosporidium species present in human fecal samples. T-RFLP analysis proved to be a reliable and reproducible alternative method for detection and identification of Cryptosporidium species.
MATERIALS AND METHODS
Parasite sources.
Seventy-two human fecal samples that were positive for Cryptosporidium were obtained from pathology laboratories in Sydney, Australia. Specimens were identified as Cryptosporidium positive by pathology companies using the Remel ProSpecT Giardia/Cryptosporidium microplate assay. Samples were stored as whole feces without preservatives at 4°C until processing, which occurred within 1 month after collection.
Oocyst purification and DNA extraction.
Fecal samples were exposed to 1,500 Ci from a 60Co source for 30 min. Cryptosporidium oocysts were purified using a sucrose flotation gradient as described by Truong and Ferrari (22). Purified oocysts, stained with the Cryptopsoridium-specific antibody CRY104 labeled with fluorescein isothiocyanate (Biotech Fronteirs, North Ryde, Australia), were examined using epifluorescence microscopy with appropriate filters for fluorescein isothiocyanate excitation (Axioscope; Zeiss, Germany) and were enumerated at a magnification of ×400 (20). Genomic DNA was extracted from purified oocysts using PrepGEM (ZyGEM Corporation Ltd., Hamilton, New Zealand) as previously described (9).
Identification of Cryptosporidium species by PCR-RFLP analysis.
Amplification of the 18S rRNA gene was performed using a previously described nested PCR (27). The primary and secondary reaction mixtures contained 6 mM MgCl2, 200 μM deoxynucleoside triphosphates, 200 nM of each primer, 1 U of Red Hot Taq (ABgene, Surrey, United Kingdom), and 2 μl of DNA template. After an initial denaturation at 94°C for 3 min, a total of 35 cycles, each consisting of 94°C for 45 s, 56°C for 45 s, and 72°C for 1 min, were performed, followed by a final extension step of 72°C for 7 min. The secondary PCR mixture (total volume, 50 μl) contained 1 μl of the primary PCR product. The cycling conditions for the secondary reactions were identical to those used for the primary PCR. All PCRs were performed with a negative control containing only PCR water and a positive control containing C. parvum DNA. Reactions were performed with Eppendorf Mastercycler Personal instruments (Eppendorf, North Ryde, Australia), and products were resolved by electrophoresis on 1.5% (wt/vol) agarose gels using Tris-borate-EDTA. Secondary product fragments that were the correct size (832 to 835 bp depending on the species) were purified using a QIAquick PCR purification kit (Qiagen, Melbourne, Australia) by following manufacturer's instructions for the spin protocol.
RFLP analysis was performed using a previously described protocol with restriction enzyme VspI (10 U/μl; New England BioLabs) (27). DNA fragments were separated on 3.5% (wt/vol) agarose gels at 100 V for 50 min. The RFLP patterns of C. hominis and C. parvum were visualized under UV light after the preparations were stained with ethidium bromide (0.5 μg/ml) for 30 min.
Optimization of the T-RFLP protocol.
The T-RFLP protocol was optimized using six C. hominis isolates and six C. parvum isolates. Two loci of the 12 isolates, the 18S rRNA gene locus and the glycoprotein 60 locus, had previously been characterized to confirm the identities of the species. The 18S rRNA gene sequences of these isolates were used to determine the lengths of the expected T-RFs.
C. hominis and C. parvum were assessed independently to ensure that there was efficient amplification of both species. Optimization of the reaction for each species was accomplished by comparing four blunt end Taq polymerases, Pfu Turbo (Stratagene, La Jolla, CA) Accuzyme (Bioline, London, United Kingdom), Accutaq (Sigma-Aldrich, Australia), and Sahara (Bioline, United Kingdom), using two final concentrations of MgCl2 (4 and 6 mM). For fluorescence analysis the forward primer of the secondary reaction was fluorescently labeled at the 5′ end with 6-carboxyfluorescein (Proligo, Lismore, Australia).
T-RFLP nested PCR.
The constituents used for primary and secondary reactions were identical to those described above except that Red Hot Taq was replaced by Accutaq (1 U) and dimethyl sulfoxide was added at a final concentration of 2%. The cycling conditions were initial denaturation at 94°C for 3 min, followed by 35 cycles, each consisting of 94°C for 45 s, 56°C for 45 s, and 68°C for 1 min, and then a final extension at 68°C for 7 min. For secondary PCRs that generated the expected products, the products were purified and subjected to restriction digestion with VspI. The amount of DNA in the restriction digest used for T-RFLP analysis was 10-fold less than the amount used for RFLP analysis due to the sensitivity of capillary electrophoresis.
Samples were analyzed at the Macquarie University DNA sequencing facility. Prior to capillary electrophoresis, 10 μl of HiDi/Standards master mixture comprising 9.9 μl of formamide and 0.1 μl of the internal DNA standard LIZ500 (Applied Biosystems) was added to 1 μl of template, and this was followed by denaturation at 95°C for 5 min. The fluorescence of the T-RFs was detected using an ABI Prism 3130x1 genetic analyzer (Applied Biosystems) in Genescan mode (8.5 kV; 40-s injection; 60°C for 100 min) with a G5 filter. T-RF sizes were determined using GeneScan software, version 4.0 (Applied Biosystems).
MDL of T-RFLP analysis.
To determine the minimum detection limit (MDL) of T-RFLP analysis, purified C. hominis and C. parvum oocysts were used to prepare suspensions with known numbers of oocysts of each species. Oocysts were immunolabeled with CRY104 as described above and sorted onto polycarbonate membranes using a FACSCalibur-sort flow cytometer (BD Biosciences, Sydney, Australia). C. hominis and C. parvum oocyst suspensions were prepared in triplicate and contained 1, 10, 100, and 1,000 oocysts. To confirm numbers of oocysts, membranes containing 1 or 10 oocysts were examined using epifluorescence microscopy as described above. DNA extraction and T-RFLP analysis were then conducted as previously described.
Mixed-infection detection.
Mixed-species suspensions were used to determine the sensitivity of T-RFLP analysis for detection of mixed infections. Purified oocysts of C. hominis and C. parvum were immunolabeled and sorted using a fluorescence-activated cell sorter as described above. Triplicate samples containing 500 oocysts were prepared using the following ratios of C. hominis to C. parvum: 1:99, 5:95, 10:90, 25:75, 50:50, 75:25, 90:10, 95:5, and 99:1. DNA was extracted using prepGEM, and amplification for T-RFLP analysis was performed as described above. For comparison, RFLP analysis was performed with mixed-species suspensions as described by Xiao et al. (27).
RESULTS
Identification of Cryptosporidium species.
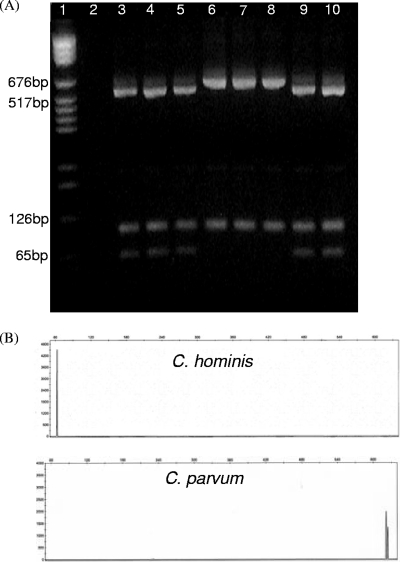
Amplification of the 18S rRNA gene was successful for 71 of the 72 isolates analyzed. Digestion of secondary PCR products with VspI enabled differentiation of C. hominis isolates and C. parvum isolates. Analysis of C. hominis isolates revealed 69- and 530-bp fragments, and analysis of C. parvum isolates revealed a single 627-bp fragment (Fig. 1A). The digestion profiles identified 38 of the 71 isolates as C. hominis (53%) and 33 of the 71 isolates as C. parvum (46%).
FIG. 1.
Species identification of Cryptosporidium isolates by RFLP (A) and T-RFLP (B) analyses of the 18S rRNA gene with VspI. C. hominis isolates (lanes 3 to 5, 9, and 10) produced three fragments but were identified by the presence of the 69- and 530-bp fragments, whereas C. parvum isolates (lanes 6 to 8) were identified by a 627-bp fragment. T-RFLP analysis was used to identify C. hominis by a 64-bp peak and C. parvum by a 624-bp peak.
Species identification by T-RFLP analysis.
The T-RFLP protocol was optimized by using six C. hominis isolates and six C. parvum isolates. The 18S rRNA gene sequences of these isolates were used to determine the lengths of the expected T-RFs. For C. hominis the predicted length was 69 bp, and for C. parvum the predicted length was 627 bp. Reactions were optimized for Taq polymerase and MgCl2 concentration, and the results showed that the fluorescently tagged primer did not alter the PCR conditions (data not shown). The optimal Taq polymerase and MgCl2 concentration that produced smooth tight peaks for both species were Accutaq and 6 mM, and these conditions were used for subsequent T-RFLP analyses. Purification of the fluorescently labeled PCR products also facilitated clean GeneScan outputs, and PCR cleaning was included in the optimized protocol.
The T-RFLP results differentiated C. hominis and C. parvum based on the fluorescently labeled 5′ T-RFs. C. hominis isolates generated a 64-bp T-RF, and C. parvum isolates generated a 624-bp T-RF (Fig. 1B). A second T-RF with an estimated size of 621 bp was detected in the profiles of all C. parvum isolates. The intensity of the second peak was consistently less than the intensity of the 624-bp T-RF peak.
Comparison of T-RFLP analysis to RFLP analysis produced consistent results, and the organisms in each sample were identified as the same species by both methods (see File S1 in the supplemental material). One sample, isolate 24, which did not produce a visible RFLP product when it was resolved using gel electrophoresis, was identified as C. parvum by T-RFLP analysis. Eight isolates were not identified by T-RFLP analysis after 6 months of storage.
MDL for T-RFLP analysis.
The MDL for T-RFLP analysis was higher than the MDL for RFLP analysis. For C. parvum, RFLP analysis was able to resolve DNA from a single oocyst, but for C. hominis RFLP products were observed in only one of the three samples containing DNA from a single oocyst (Table 1; see also File S2 in the supplemental material). Despite using 10-fold less DNA template than RFLP analysis, T-RFLP analysis detected the expected T-RF for all three C. hominis samples which contained DNA from a single oocyst (see File S3 in the supplemental material).
TABLE 1.
Detection of C. hominis and C. parvum in samples with known numbers of oocysts
| No. of oocysts in sample | No. of samples in which C. parvum was detected (n = 3)
|
No. of samples in which C. hominis was detected (n = 3)
|
||
|---|---|---|---|---|
| RFLP | T-RFLP | RFLP | T-RFLP | |
| 1 | 3 | 3 | 1 | 3 |
| 10 | 3 | 3 | 3 | 3 |
| 100 | 3 | 3 | 3 | 3 |
| 1,000 | 3 | 3 | 3 | 3 |
Mixed-infection detection.
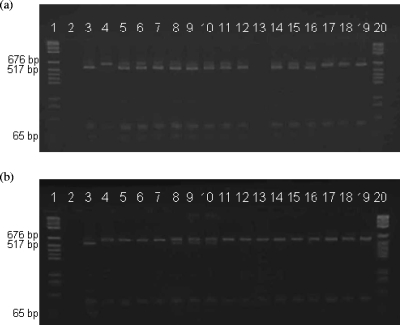
For all ratios tested C. parvum DNA was detected by RFLP analysis (Fig. 2) and T-RFLP analysis (Table 2). C. hominis DNA was not detected by RFLP or T-RFLP analysis when its contribution of DNA was equal to or less than that of C. parvum. The sensitivity of T-RFLP analysis enabled detection of C. hominis DNA in the suspension containing equal amounts of C. hominis and C. parvum (see File S4 in the supplemental material).
FIG. 2.
Detection of C. hominis and C. parvum at different ratios in mixed populations. (a) Analysis of mixed-species suspensions identified C. parvum DNA at all C. parvum/C. hominis ratios. Lane 1, molecular weight marker; lane 2, negative control; lane 3, C. hominis control; lane 4, C. parvum control; lanes 5 to 7, 1:99 ratio; lanes 8 to 10, 5:95 ratio; lanes 11 to 13, 10:90 ratio; lanes 14 to 16, 25:75 ratio; lanes 17 to 19, 50:50 ratio. (b) C. hominis DNA could not be detected by RFLP analysis at the majority of the ratios. The only exception was sporadic amplification in the samples containing C. hominis and C. parvum at a ratio of 5:95 (lanes 8 to 10).
TABLE 2.
Detection of C. hominis and C. parvum when different ratios in mixed populations were used
| C. hominis/C. parvum ratio | No. of samples in which species were detected (n = 3)
|
||
|---|---|---|---|
| Only C. hominis | Only C. parvum | Both species | |
| 0.1:9.9 | 0 | 3 | 0 |
| 0.5:9.5 | 0 | 0 | 3 |
| 1:9 | 0 | 2 | 1 |
| 2.5:7.5 | 0 | 1 | 2 |
| 5:5 | 0 | 2 | 1 |
| 7.5:2.5 | 0 | 0 | 3 |
| 9:1 | 0 | 0 | 2 |
| 9.5:0.5 | 0 | 0 | 3 |
| 9.9:0.1 | 0 | 0 | 3 |
Repeatability of T-RFLP analysis.
The ability to consistently identify Cryptosporidium species by T-RFLP analysis was determined by performing a blind screen analysis using 20 alphabetically coded samples. Amplification was successful for 19 of the 20 isolates analyzed. Fourteen isolates contained a 64-bp T-RF and were identified as C. hominis, and the remaining five isolates were identified as C. parvum due to detection of the 624-bp T-RF (see File S5 in the supplemental material). T-RFLP analysis identified all blind screen isolates as members of the correct species.
DISCUSSION
This study developed and evaluated T-RFLP analysis for identification of Cryptosporidium species and was the first study to apply this methodology to protozoa. Routine laboratory diagnosis of Cryptosporidium oocysts does not discriminate between Cryptosporidium species (2, 11). Species identification, a basic requirement for epidemiological research, is commonly performed using PCR-RFLP analysis or DNA sequencing (4, 27). Although PCR-RFLP analysis is capable of detection and identification of species, it requires relatively high parasite loads for interpretation of restriction fragments resolved using agarose gel electrophoresis. Consequently, low-level infections elude diagnosis, and important species information required for effective management of the disease is lost. T-RFLP analysis was shown to be a rapid, sensitive, and nonsubjective alternative method for identification of Cryptosporidium species.
Although five Cryptosporidium species are known to cause disease in humans (16, 18, 28), this study was performed to develop T-RFLP analysis of the 18S rRNA genes to differentiate C. hominis and C. parvum. T-RFLP analysis unambiguously differentiated between C. hominis and C. parvum isolates and identified the C. hominis-specific peak at 64 bp and the C. parvum-specific peak at 624 bp. Due to the heterogeneity in the 18S rRNA genes of C. parvum isolates, the electropherograms for these isolates had a second minor peak at 621 bp, which was attributed to the second, type B copy of the 18S rRNA gene (13). The mobilities calculated by the GeneScan software were approximately the same as the mobilities expected for the two species, 69 bp for C. hominis and 627 bp for C. parvum. To maintain accurate species identification and to correct for run variation, a panel of reference controls should be included in each analysis run. The reliability and reproducibility of T-RFLP analysis for identification of Cryptosporidium species is high, and the T-RFs for all samples were consistent with previous sample identifications. The DNA extraction method used in this study is new (9), and no stability data have been reported yet. It is possible that the failure to reamplify the DNA of eight isolates was due to degradation over the 6 months of storage. The DNA stability after extraction with PrepGEM needs to be evaluated if this method is to be used for preparation of Cryptosporidium libraries.
Mixed infections are not commonly detected in cases of human cryptosporidiosis. It has been proposed that when C. hominis and C. parvum simultaneously infect the same host, C. parvum displaces C. hominis and becomes the predominant parasite (1). Mixed-species analyses in this study indicated that preferential amplification of C. parvum DNA occurs regardless of its relative contribution to the DNA pool. Both RFLP and T-RFLP analyses failed to consistently detect C. hominis DNA when its contribution to the DNA pool was equal to or less than that of C. parvum. Similar results were obtained in a previous study which used different nested primer sets (21), and this suggests that mixed infections may occur more frequently than has been recorded. The limitations of selective amplification by PCR mean that previous studies of human cryptosporidiosis have overlooked the contribution of C. hominis and other pathogenic species to human disease. This would have limited the identification of all possible disease sources.
Accurate identification of all species causing human cryptosporidiosis should increase our understanding of both the disease dynamics and the sources of infection. Here, C. hominis and C. parvum were the only species used, but altering the restriction enzyme would allow T-RFLP analysis to be used for identification of other Cryptosporidium species of concern to human health, such as Cryptosporidium meleagridis, Cryptosporidium canis, and Cryptosporidium muris, which can be differentiated using SspI (26).
The use of T-RFLP analysis in epidemiological studies should provide rapid, reproducible, and accurate identification of Cryptosporidium species in infections. The MDL and the sensitivity of T-RFLP analysis to a single oocyst should improve prevalence estimates. The methodology developed in this study will be used in an ongoing investigation of human cryptosporidiosis in New South Wales, Australia.
Supplementary Material
Acknowledgments
This work was performed with financial assistance from the Environmental Biotechnology CRC.
We thank Jeremy McAnulty and Jennie Musto of the NSW Health Communicable Disease Branch for their assistance with sample collection. We especially acknowledge Douglas Hanley Moir, SDS Pathology and Symbion in North Ryde and the Westmead, Australia, John Hunter, St. Vincents, Blacktown, Gosford, Australia, David Campbell, and the Wollongong and Seals hospitals for providing human fecal samples.
Footnotes
Published ahead of print on 31 October 2008.
Supplemental material for this article may be found at http://aem.asm.org/.
REFERENCES
- 1.Akiyoshi, D. E., S. Mor, and S. Tzipori. 2003. Rapid displacement of Cryptosporidium parvum type 1 by type 2 in mixed infections in piglets. Infect. Immun. 71:5765-5771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baveja, U. K. 1998. Acid fast staining versus ELISA for detection of Cryptosporidium in stool. J. Commun. Dis. 30:241-244. [PubMed] [Google Scholar]
- 3.Bruce, K. D. 1997. Analysis of mer gene subclasses within bacterial communities in soils and sediments resolved by fluorescent-PCR-restriction fragment length polymorphism profiling. Appl. Environ. Microbiol. 63:4914-4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chalmers, R., C. Jacson, K. Elwin, S. Hadfield, and P. Hunter. 2007. Investigation of genetic variation within Cryptosporidium hominis for epidemiological purposes. National Public Health Service for Wales, Cardiff, Wales, United Kingdom.
- 5.Cohen, S., F. Dalle, A. Galay, M. Palma, A. Bonnin, and H. Ward. 2006. Identification of Cpgp40/15 type Ib as the predominant allele in isolates of Cryptosporidium spp. from waterborne outbreak of gastroenteritis in South Burgundy, France. J. Clin. Microbiol. 44:589-591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunbar, J., L. O. Ticknor, and C. R. Kuske. 2000. Assessment of microbial diversity in four southwestern United States soils by 16S rRNA gene terminal restriction fragment analysis. Appl. Environ. Microbiol. 66:2943-2950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunbar, J., L. O. Ticknor, and C. R. Kuske. 2001. Phylogenetic specificity and reproducibility and new method for analysis of terminal restriction fragment profiles of 16S rRNA genes from bacterial communities. Appl. Environ. Microbiol. 67:190-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fayer, R., and B. Ungar. 1986. Cryptosporidium spp. and cryptosporidiosis. Microbiol. Rev. 50:458-483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferrari, B. C., M. L. Power, and P. L. Bergquist. 2007. Closed-tube DNA extraction using a thermostable proteinase is highly sensitive, capable of single parasite detection. Biotechnol. Lett. 29:1831-1837. [DOI] [PubMed] [Google Scholar]
- 10.Fogarty, L., and M. Voytek. 2005. Comparison of Bacteroides-Prevotella 16S rRNA genetic markers for fecal samples from different animal species. Appl. Environ. Microbiol. 71:5999-6007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kehl, K. S., H. Cicirello, and P. L. Havens. 1995. Comparison of four different methods for detection of Cryptosporidium species. J. Clin. Microbiol. 33:416-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laubach, H., C. Bentley, E. Ginter, J. Spalter, and L. Jensen. 2004. A study of risk factors associated with the prevalence of Cryptosporidium in villages around Lake Atitlan, Guatemala. Braz. J. Infect. Dis. 8:319-323. [DOI] [PubMed] [Google Scholar]
- 13.Le Blancq, S. M., N. V. Khramtsov, F. Zamani, S. J. Upton, and T. W. Wu. 1997. Ribosomal RNA gene organization in Cryptosporidium parvum. Mol. Biochem. Parasitol. 90:463-478. [DOI] [PubMed] [Google Scholar]
- 14.Liu, W., T. Marsh, H. Cheng, and L. Forney. 1997. Characterization of microbial diversity by determining terminal restriction fragment length polymorphisms of genes encoding 16S rRNA. Appl. Environ. Microbiol. 63:4516-4522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marsh, T. 1999. Terminal restriction fragment length polymorphism (T-RFLP): an emerging method for characterising diversity among homologous populations of amplification products. Curr. Opin. Microbiol. 2:323-327. [DOI] [PubMed] [Google Scholar]
- 16.Misic, Z., and N. Abe. 2007. Subtype analysis of Cryptosporidium parvum isolates from calves on farms around Belgrade, Serbia and Montenegro, using the 60 kDa glycoprotein gene sequences. Parasitology 134:351-358. [DOI] [PubMed] [Google Scholar]
- 17.Moeseneder, M. M., J. M. Arrieta, G. Muyzer, C. Winter, and G. J. Herndl. 1999. Optimization of terminal-restriction fragment length polymorphism analysis for complex marine bacterioplankton communities and comparison with denaturing gradient gel electrophoresis. Appl. Environ. Microbiol. 65:3518-3525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morgan-Ryan, U., A. Fall, L. Ward, N. Hijjawi, I. Sulaiman, F. Fayer, R. Thompson, M. Olson, A. Lal, and L. Xiao. 2002. Cryptosporidium hominis n. sp. (Apicomplexa: Cryptosporidiidae) from Homo sapiens. J. Eukaryot. Microbiol. 49:433-440. [DOI] [PubMed] [Google Scholar]
- 19.Petri, W. 2005. Treatment of giardiasis. Curr. Treatment Options Gastroenterol. 8:13-17. [DOI] [PubMed] [Google Scholar]
- 20.Power, M. L., S. R. Shanker, N. C. Sangster, and D. A. Veal. 2003. Evaluation of a combined immunomagnetic separation/flow cytometry technique for epidemiological investigations of Cryptosporidium in domestic and Australian native animals. Vet. Parasitol. 112:21-31. [DOI] [PubMed] [Google Scholar]
- 21.Reed, C., G. D. Sturbaum, P. J. Hoover, and C. R. Sterling. 2002. Cryptosporidium parvum mixed genotypes detected by PCR-restriction fragment length polymorphism analysis. Appl. Environ. Microbiol. 68:427-429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Truong, Q., and B. C. Ferrari. 2006. Quantitative and qualitative comparisons of Cryptosporidium faecal purification procedures for the isolation of oocysts suitable for proteomic analysis. Int. J. Parasitol. 36:811-819. [DOI] [PubMed] [Google Scholar]
- 23.van der Maarel, M., R. R. Artz, R. Haanstra, and L. J. Forney. 1998. Association of marine archaea with the digestive tracts of two marine fish species. Appl. Environ. Microbiol. 64:2894-2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang, M., S. Ahrne, M. Antonsson, and G. Molin. 2004. T-RFLP combined with principal component analysis and 16S rRNA gene sequencing: an effective strategy for comparison of fecal microbiota in infants of different ages. J. Microbiol. Methods 59:53-69. [DOI] [PubMed] [Google Scholar]
- 25.Xiao, L., J. Alderisio, J. Limor, M. Royer, and A. Lal. 2000. Identification of species and sources of Cryptosporidium oocysts in storm waters with a small-subunit rRNA-based diagnostic and genotyping tool. Appl. Environ. Microbiol. 66:5492-5498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xiao, L., L. Escalante, C. Yang, I. Sulaiman, A. Escalante, R. Montali, R. Fayer, and A. Lal. 1999. Phylogenetic analysis of Cryptosporidium parasites based on the small-subunit rRNA gene locus. Appl. Environ. Microbiol. 65:1578-1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xiao, L., U. Morgan, J. Limor, A. Escalante, M. Arrowood, R. Shulaw, R. Thompson, F. R., and A. Lal. 1999. Genetic diversity within Cryptosporidium parvum and related Cryptosporidium species. Appl. Environ. Microbiol. 65:3386-3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xiao, L., and U. Ryan. 2004. Cryptosporidiosis: an update in molecular epidemiology. Curr. Opin. Infect. Dis. 17:483-490. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.