Abstract
Objective
The authors reviewed clinical and radiological outcomes in patients with three column injury of the cervical spine who had undergone posterior cervical fixation using Nitinol shape memory alloy loop in the anterior-posterior combined approach.
Materials
Nine patients were surgically treated with anterior cervical fusion using an iliac bone graft and dynamic plate-screw system, and the posterior cervical fixation using Nitinol shape memory loop (Davydov™) at the same time. A retrospective review was performed. Clinical outcomes were assessed using the Frankel grading method. We reviewed the radiological parameters such as bony fusion rate, height of iliac bone graft strut, graft subsidence, cervical lordotic angle, and instrument related complication.
Results
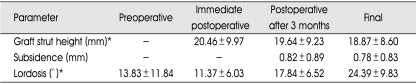
Single-level fusion was performed in five patients, and two-level fusion in four. Solid bone fusion was presented in all cases after surgery. The mean height of graft strut was significantly decreased from 20.46±9.97 mm at immediate postoperative state to 18.87±8.60 mm at the final follow-up period (p<0.05). The mean cervical lordotic angle decreased from 13.83±11.84° to 11.37±6.03° at the immediate postoperative state but then, increased to 24.39±9.83° at the final follow-up period (p<0.05). There were no instrument related complications.
Conclusion
We suggest that the posterior cervical fixation using Nitinol shape memory alloy loop may be a simple and useful method, and be one of treatment options in anterior-posterior combined approach for the patients with the three column injury of the cervical spine.
Keywords: Nitinol, Shape memory loop, Posterior cervical surgery, fracture fixation
INTRODUCTION
Three column injury of cervical spine usually requires 360 degree fusion using anterior-posterior combined approach14). The anterior or posterior approach alone would lead to the failure in stabilizing the three column injury due to instrumentation failure14). The goal of anterior-posterior combined approach is to provide structural stability until a solid bone fusion is obtained. There are many techniques of posterior cervical fixation and fusion. In the middle to lower cervical area, various posterior cervical fixation methods such as wiring, laminar clamp, pedicle screw, and lateral mass screw have been used frequently9-12,15,16).
Recently, shape memory alloy has been used in spine surgeries7,13). The Nitinol is an alloy of nickel and titanium that belongs to a class of materials called shape memory alloys. The Nitinol implant has high elasticity and flexibility (below 10℃) or rigidity (above 30℃) according to temperature change7). The shape memory alloy loop has been applied to the thoracic and lumbar regions of the spine2,7,13). We tried to use Nitinol shape memory alloy loop in the posterior cervical fixation. The authors reviewed clinical and radiological outcomes in patients with the three column injury of the cervical spine who had undergone posterior cervical fixation using Nitinol shape memory alloy loop (Davydov™) in the anterior-posterior combined approach. The purpose of this study is to evaluate the usability of posterior cervical fixation with Nitinol shape memory alloy in the anterior-posterior combined approach.
MATERIALS AND METHODS
Patient Population
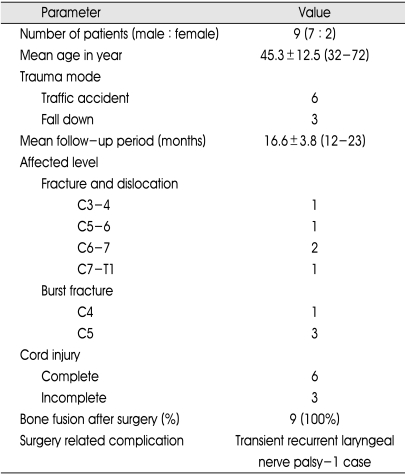
The authors reviewed retrospectively the medical records and radiological data. From January 2005 to February 2006, thirty-two patients with cervical three column injury were surgically treated at our institution. Among these, eleven patients underwent anterior cervical fusion and posterior cervical fixation with Nitinol shape memory alloy loop (Davydov™, KIMPF-DI Fixing system; CJSC KIMPF Co., Seoul, Korea). We excluded the patients who were not followed more than twelve month and had high cervical injuries (C1-2). A total of nine patients were enrolled in this study. There were 7 male and 2 female and the mean age was 45.3 years (Table 1). All nine patients had three column injury of the middle to low cervical area after trauma. We treated those patients surgically with anterior cervical fusion using iliac bone graft and dynamic plate-screw system (Atlantis™, Medtronic Sofamor Danek, Memphis, Tennessee), and posterior cervical fixation using Nitinol memory loop at the same time.
Table 1.
Demographic and clinical results summary
Surgical technique7)
First, we applied Gardner tong to patient's head for reduction of misaligned cervical spine. After reduction, we performed anterior cervical fusion using autologous iliac bone graft and dynamic plate-screw system with usual manners in supine position. Then, the patient's position was changed to a prone position. A midline linear incision and exposure was made from the upper lamina to the lower lamina of the affected level. A very minimal skeleonization of the lamina and spinous processes were performed. Template measuring instruments were used to calculate the exact size of the Nitinol memory loop. After selection of the proper fixating loop, it was lifted by forceps and cooled in sterilized physiological saline at 5 to 15℃ for at least 30 seconds. The memory loop could be deformed easily and then, it was placed on the lamina arch of the vertebra. After the installation of the memory loop, the implant was irrigated with sterile physiological saline heated to between 35 and 45℃. The memory loop regained its initial form and rigidity. After confirmation of the firm fixation, the wound was closed layer by layer.
We could not correct misaligned cervical spine using retraction of Gardner tong in one case. Therefore, we initially performed intra-operative reduction and applied memory loop using posterior approach. After posterior approach, we operated anteriorly.
Review of clinical and radiological data
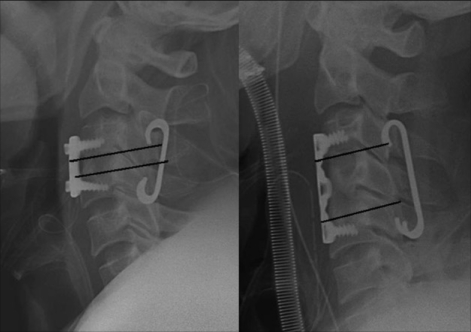
A retrospective review was carried out for the nine enrolled patients. Clinical outcomes were assessed and classified using the Frankel grading method. We also retrospectively reviewed the radiological parameters such as bony fusion rate, height of iliac bone graft strut, graft subsidence, cervical lordotic angle, and instrument related complication. Height of iliac bone graft strut was measured immediately after the operation, then 3 months after the operation and at the final follow-up period using lateral cervical X-ray (Fig. 1). The subsidence of graft strut was calculated 3 months after operation and at the final follow-up period. Cervical lordotic angle was measured by drawing lines tangent to the 2 most posterior points of the vertebral body seen on the lateral view (Fig. 2)5). We compared the means of height of iliac bone graft strut at the immediate postoperative state, 3 month after operation and at the final follow-up period. Also the mean of cervical lordotic angle was compared at the preoperative state, the immediate postoperative state, 3 month after operation, and at the final follow-up period.
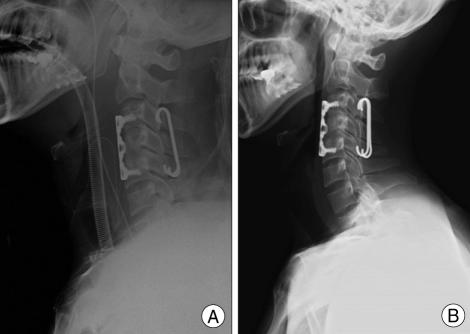
Fig. 1.
Measurement of height of graft strut on neutral cervical lateral X-ray.
Fig. 2.
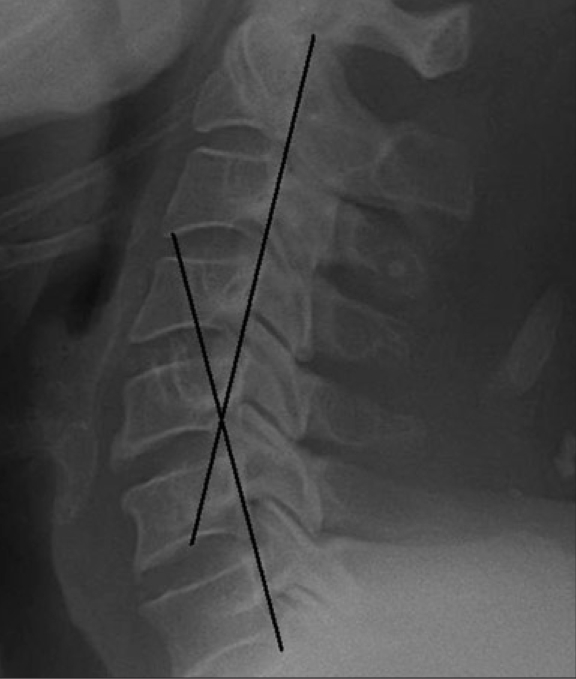
Measurement of cervical lordotic angle on lateral X-ray.
Statistical analysis was performed using the Wilcoxon signed rank test. p-value below 0.05 was considered significant.
RESULTS
The mean follow-up duration was 16.6±3.8 months (12-23 months). There were five patients with fracture/dislocation and four patients with bursting fracture (Table 1). Single-level fusion was performed in four patients and twolevel fusion in five. Six patients had complete cord injury and 3 patients had incomplete cord injury (Table 1). Before surgery, three patients were classified as Frankel type D and six as Frankel type A. After surgery, All Frankel type D patients were improved to Frankel type E, but all Frankel type A patients did not improved. The radiographically documented solid bone fusion, with evidence of solid bridging bone and no instability on flexion-extension X-ray films1), was presented in all cases. The mean height of iliac bone graft strut was 20.46±9.97 mm at the immediate postoperative state, 19.64±9.23 mm 3 months later and 18.87±8.60 at the final follow-up period. The mean height of graft strut was significantly decreased postoperatively (Table 2, P<0.05). The subsidence of graft strut occurred in all cases and the means of subsidence were 0.82±0.89 mm 3 months after operation and 0.78±0.83 mm at the final follow-up period (Table 2). The mean cervical lordotic angle was decreased from 13.83±11.84° preoperatively to 11.37±6.03° at the immediate postoperative state. However, the mean cervical lordotic angle was increased to 17.84±6.52° 3 months after surgery and 24.39±9.83° at the final follow-up period. The cervical lordotic angle was significantly improved 3 months after surgery and at the final follow-up period than preoperative and immediate postoperative conditions (p<0.05)(Table 2). Transient recurrent laryngeal nerve palsy was presented in one case. However, there were no instrument related complications, such as loosening, fracture, or dislodgement of instruments.
Table 2.
Radiologic results. The mean height of graft strut was significantly decreased postoperatively. The subsidence of graft strut occurred. The cervical lordotic angle was significantly improved 3 months after surgery and at the final follow-up period than preoperative and immediate postoperative conditions
*P<0.05, Wilcoxon signed rank test.
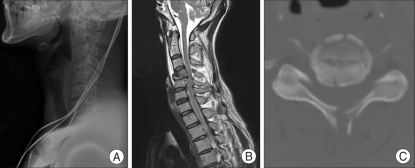
Case illustration (Fig. 3, 4)
Fig. 3.
Imaging studies of a patient with left arm monoparesis after trauma. A : Plain cervical lateral X-ray of C4 vertebral body fracture. B and C : Magnetic resonance image and computed tomography show C4 vertebral body fracture with three column injury.
Fig. 4.
A : Immediate postoperative lateral radiographs. B : Sixteen months later, lateral radiographs showing solid bone fusion and improvement of cervical lordotic angle.
A 31-year-old male patient presented with left arm monoparesis (G4/5) after traffic accident. Magnetic resonance imaging (MRI), computed tomography (CT) and initial X-ray showed a C4 vertebral body fracture with three column injury (Fig. 3). We performed a single stage anteriorposterior cervical decompression and stabilization. We did C4 corpectomy, iliac bone graft and dynamic cervical plate fixation in a supine position and then installed a Nitinol memory loop on C3 upper and C5 lower lamina in a prone position. After operation, the left arm monoparesis was improved (G4+/5). Solid bone fusion was presented on cervical lateral X-ray, which was taken at 16 months after the operation. Cervical lordotic angle was also improved (Fig. 4B).
DISCUSSION
There were many posterior cervical fixation techniques such as spinous process wiring, interlaminar clamp, lateral mass screw fixation and cervical pedicle screw fixation. Recently, lateral mass screw system has been frequently used in posterior middle to lower cervical operation. Many reports have presented the good clinical outcomes and various aspects of lateral mass screw system8,11). However, there have been several limitations of lateral mass screw such as hardware loosening, vertebral artery injury and iatrogenic damage of nerve root6,8,9). Spinous process wiring technique is an easy and simple method but its strength is relatively weak and occasionally result in fracture of wire and fusion failure6). Interlaminar clamp or laminar hook instrument has been also used. One of the limitations of the clamp or hook system is indentation of the cervical thecal sac4). Ideal posterior cervical instrumentation needs to have short operation time, easy surgical technique, low incidence of device related complications and to provide structural stability until a solid bone fusion.
Nitinol is a shape memory alloy of nickel and titanium. It is flexible at below 10℃ and regains rigidity and its original shape at above 30℃. Several spinal surgeons have tried to apply this to lumbar or thoracic spinal surgery based on these characteristics2). Nitinol has high fatigue strength, moderate impact resistance and large forces that can be produced due to the shape memory effect. Kim et al.7) have reported the usefulness of a Nitinol memory loop in surgical treatment for lumbar disc disorder. They used Nitinol memory loop as the posterior column supporter or posterior tension bands in lumbar spine surgery. Nitinol memory loop can be easily applied in spine surgery because of heat-dependent plasticity, small muscle dissection (require only small exposure of laminar area), less bleeding and short operation time7).
We tried to apply Nitinol memory loop in posterior cervical fixation as a posterior column supporter. We were able to easily apply Nitinol memory loop at posterior middle to lower cervical spine and reduce operation time and bleeding. In the present study, Nitinol memory loop played a good role as the posterior column supporter. There were no instrument-related complications such as loop loosening and pullout. However, we believe that there are several limitations of Nitinol memory loop in cases with multi-level laminar fractures, post-laminectomy kyphosis and patients who need only posterior cervical fixation and fusion. In the above cases, we prefer a lateral mass screw system.
Although it has been reported that the cervical laminar hooks do not affect the dura and there is no evidence of spinal cord compression in cadaveric study,4) we believe that Nitinol memory loop and laminar hooks should be avoided at stenotic levels due to possibility of dura compression and further cadaveric and radiological studies of Nitinol memory loop should be required to verify its safety. In our cases, the subsidence of graft strut has occurred. Dynamic cervical plate and screw system could lead to the subsidence of graft strut3), therefore, we speculate that the subsidence of graft strut in our cases was the effect of the dynamic cervical plate system rather than of the memory loop system. However, the memory loop system did not have the resistance of the spinal axial load as in the laminar hook system. This was one of the weak points of the memory loop that could contribute to the subsidence of graft strut. Despite the subsidence, the solid bone fusions were achieved in all cases. Memory loop system is not a rigid fixation system such as the lateral mass screw and rod systems. It has elasticity and its stiffness may be weaker than lateral mass screw and rod systems. However, we believe that the elasticity of memory loop may contribute to improvement of lordotic curvature of cervical spine. In all of our cases, cervical lordotic curvatures were improved (Table 2).
Though this study showed good results using Nitinol memory loop, the small number of patients was the limitation of this study. With more number of cases with longer follow-up period, the usability and limitations of Nitinol memory loop will be investigated more precisely.
CONCLUSION
For the patients with the three column injury of the cervical spine, an anterior-posterior combined approach is known as one of the surgical tools to provide good solid fusion and fixation. We suggest that the posterior cervical fixation using Nitinol shape memory alloy loop may be a simple and useful method, and be one of treatment options in anterior-posterior combined approach for the patients with the three column injury of the cervical spine.
References
- 1.Berquist TH. Imaging of the postoperative spine. Radiol Clin North Am. 2006;44:407–418. doi: 10.1016/j.rcl.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Braun JT, Akyuz E, Udall H, Ogilvie JW, Brodke DS, Bachus KN. Three-dimensional analysis of 2 fusionless scoliosis treatments : a flexible ligament tether versus a rigid-shape memory alloy staple. Spine. 2006;31:262–268. doi: 10.1097/01.brs.0000197569.13266.fe. [DOI] [PubMed] [Google Scholar]
- 3.Brodke DS, Klimo P, Bachus KN, Braun JT, Dailey AT. Anterior cervical fixation : analysis of load-sharing and stability with use of static and dynamic plates. J Bone Joint Surg Am. 2006;88:1566–1573. doi: 10.2106/JBJS.E.00305. [DOI] [PubMed] [Google Scholar]
- 4.Fagerström T, Hedlund R, Bancel P, Robert R, Dupas B. Laminar hook instrumentation in the cervical spine. An experimental study on the relation of hooks to the spinal cord. Eur Spine J. 2001;10:340–344. doi: 10.1007/s005860100251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harrington JF, Jr, Park MC. Single level arthrodesis as treatment for midcervical fracture subluxation : a cohort study. J Spinal Disord Tech. 2007;20:42–48. doi: 10.1097/01.bsd.0000211255.05626.b0. [DOI] [PubMed] [Google Scholar]
- 6.Kandziora F, Pflugmacher R, Scholz M, Schnake K, Putzier M, Khodadadyan-Klostermann C, et al. Posterior stabilization of subaxial cervical spine trauma : indications and techniques. Injury. 2005;36(Suppl 2):B36–B43. doi: 10.1016/j.injury.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 7.Kim YS, Zhang HY, Moon BJ, Park KW, Ji KY, Lee WC, et al. Nitinol spring rod dynamic stabilization system and Nitinol memory loops in surgical treatment for lumbar disc disorders : short-term follow up. Neurosurg Focus. 2007;22:E10. [PubMed] [Google Scholar]
- 8.Kwon BK, Vaccaro AR, Grauer JN, Beiner JM. The use of rigid internal fixation in the surgical management of cervical spondylosis. Neurosurgery. 2007;60:S118–S129. doi: 10.1227/01.NEU.0000249222.57709.59. [DOI] [PubMed] [Google Scholar]
- 9.Lee DC, Yoon SH, Park HC, Park JO, Hyun DK, Park HS. Clinical and computed tomography evaluation of plate and screw on the cervical lateral mass : a modified magerl's technique. J Korean Neurosurg Soc. 2006;39:251–255. [Google Scholar]
- 10.Lee GY, Massicotte EM, Rampersaud YR. Clinical accuracy of cervicothoracic pedicle screw placement : a comparison of the "open" lamino-foraminotomy and computer-assisted techniques. J Spinal Disord Tech. 2007;20:25–32. doi: 10.1097/01.bsd.0000211239.21835.ad. [DOI] [PubMed] [Google Scholar]
- 11.Lindsey RW, Miclau T. Posterior lateral mass plate fixation of the cervical spine. J South Orthop Assoc. 2000;9:36–42. discussion 42. [PubMed] [Google Scholar]
- 12.Liu JK, Das K. Posterior fusion of the subaxial cervical spine : indications and techniques. Neurosurg Focus. 2001;10 doi: 10.3171/foc.2001.10.4.8. [DOI] [PubMed] [Google Scholar]
- 13.Sanders JO, Sanders AE, More R, Ashman RB. A preliminary investigation of shape memory alloys in the surgical correction of scoliosis. Spine. 1993;18:1640–1646. doi: 10.1097/00007632-199309000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Schultz KD, McLaughlin MR, Haid RW, Comey CH, Rodts GE, Alexander J. Single-stage anterior-posterior decompression and stabilization for complex cervical spine disorders. J Neurosurg. 2000;93:214–221. doi: 10.3171/spi.2000.93.2.0214. [DOI] [PubMed] [Google Scholar]
- 15.Tankson C, Chutkan NB. Posterior cervical instrumentation. Orthopedics. 2006;29:695–700. doi: 10.3928/01477447-20060801-12. quiz 701-702. [DOI] [PubMed] [Google Scholar]
- 16.Toohey JS, Stromberg L, Neidre A, Ramsey M, Fogel GR. Treatment of cervical pseudarthrosis after Smith-Robinson procedure with Halifax clamp fixation. J Surg Orthop Adv. 2006;15:201–202. [PubMed] [Google Scholar]