Abstract
Objective
To evaluate the risk factors that may be responsible for the development of contralateral reherniations from ipsilateral ones after open lumbar microdiscectomy (OLM), and to compare surgical outcomes of revision OLM for contralateral reherniations with those for ipsilateral ones.
Methods
Seventeen patients who underwent revision OLM for contralateral reherniation were enrolled into Group I, and 35 patients who underwent revision OLM for ipsilateral reherniation were enrolled into Group II. Using medical charts and imaging study results, the differences in the clinical and radiological factors were evaluated between the two groups. Clinical outcomes of each group were compared between the two groups.
Results
Significant differences were found in the interval to reherniation from initial surgery (33 months for Group I and 18.6 months for Group II, p=0.009), as well as in the incidences of both protruded disc (35.3% for Group I and 8.6% for Group II, p=0.045) and mild disc degeneration (29.4% for Group I and 5.7% for Group II, p=0.031) at initial surgery. On binary multi-logistic regression analysis, significant differences were found in the interval to reherniation (p=0.027, Odds ratio=1.051) and incidence of mild disc degeneration (p=0.025, Odds ratio=12.03) between the two groups. There were no significant differences in the improvement of clinical outcomes after revision OLM between the two groups.
Conclusion
The interval to reherniation from initial surgery and the grade of disc degeneration at initial surgery were key factors that distinguished the development of contralateral reherniations from ipsilateral ones. Surgical outcomes of revision OLM were similar in both groups.
Keywords: Reherniation, Discectomy, Lumbar spine
INTRODUCTION
Recurrent disc herniation, which has been reported in 5-15% of patients after disc excision, represents a major cause of surgical failure after open lumbar microdiscectomy (OLM)4,5,23-25). In the literature, there are several conditions that have been termed" recurrent disc herniation", including ipsilateral reherniation at the same level, contralateral reherniation at the same level, or a new herniation occurring at a different level7,9,11,13,19,20,26,29). Given that scar tissue could affect the surgical results in cases of reoperation, the strict definition of recurrent disc herniation has been considered as being a disc reherniation occurring at the same level and the same side as a previously operated lumbar disc, with a pain-free interval after the primary discectomy of greater than 3 weeks to 6 months3,4,25). Unlike the case for ipsilateral reherniations, scar tissue that might hinder reoperation is not present in contralateral reherniations. However, the risk of further damage to vertebral motion segment during revision discectomy has generally been considered higher for contralateral reherniations than for ipsilateral reherniations3).
Most of previous studies regarding reherniation after OLM have focused on ipsilateral reherniations, and only a few authors have stated concerns on contralateral reherniations3,8,27). Until now, there has been no study that compared contralateral reherniations with ipsilateral ones, after successful primary discectomy. The aims of this study were to evaluate the clinical and radiological factors that might distinguish development of contralateral reherniations from ipsilateral ones after successful OLM, and to evaluate clinical outcomes of revision OLM for contralateral reherniations compared to those for ipsilateral ones.
MATERIALS AND METHODS
Study design
From January 2002 to December 2004, a series of 3,352 patients underwent OLM for a lumbar disc herniation at our hospital. Among them, 52 patients underwent revision OLM due to reherniation at the same level as the primary OLM during follow-up. Clinical and radiological data of these 52 patients were retrospectively reviewed at November 2007. All operations had followed a standard pattern proposed by the senior author. Seventeen patients who underwent revision OLM for contralateral reherniation were entered into Group I, and 35 patients who underwent revision OLM for ipsilateral reherniation were entered into Group II. Inclusion criteria were as follows : (1) a previous episode of OLM resulting from lumbar disc herniation, (2) recurrent radicular pain resulting after a pain-free interval longer than 4 weeks, (3) recurrent disc herniation at the same level, regardless of side, verified by radiological studies, (i.e., the presence of abnormal epidural tissue that did not enhance after contrast injection, as well as epidural fibrosis showing enhancement with gadolinium on T1 weighted magnetic resonance imaging (MRI)), and (4) failure of extensive conservative treatment for more than 6 weeks. Excluded were (1) a disc herniation occurring at a new level with respect to the primary discectomy, (2) recurrent radicular symptoms associated with segmental instability, lateral recess stenosis, foraminal stenosis, epidural fibrosis, and/or adhesive arachnoiditis, (3) a clinical history of previous spinal surgery before primary discectomy, and (4) a clinical history of the primary discectomy having been performed at other hospitals.
Risk factor evaluation
Using preoperative clinical charts and radiological examinations, clinical and radiological factors differentiating the development of contralateral reherniations from that of ipsilateral ones were evaluated for each group, and then compared between the two groups.
The demographic and clinical parameters evaluated were as follows : age, gender, body mass index, diabetes, smoking, and traumatic event at initial OLM. Time interval to reherniation from initial surgery was also evaluated.
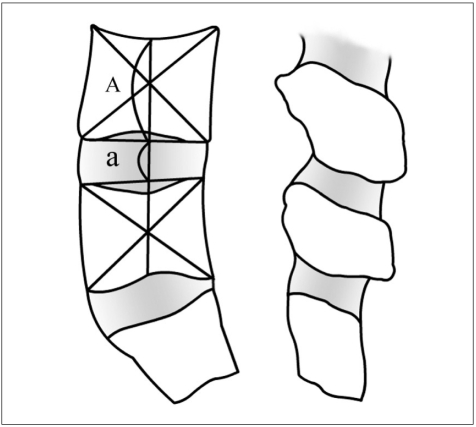
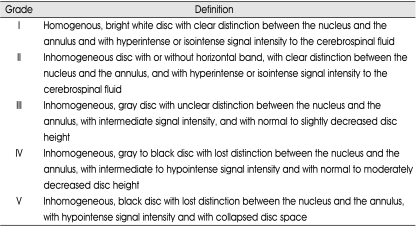
The radiological parameters included spinal level of disc herniation, extent of disc herniation, disc height ratio, presence of Modic change, and grade of disc degeneration at initial OLM. All radiological parameters were evaluated using preoperative MRI taken just before initial OLM. The disc-height ratio was measured on the T2-weighted midsagittal MRI according to Mochida's method (Fig. 1)14,16). Based on the method of Masaryk et al.15) and Modic et al.17), the extent of disc herniation was evaluated and classified as protrusion, extrusion or sequestration. A disc was considered protruded if the greatest plane, in any direction between the edges of the disc material beyond the disc, was less than the distance between the edges of the base when measured in same plane. A disc was considered extruded if, in at least in one plane, any one distance between the edges of the disc material beyond the disc space was greater than the distance between edges of the base measured in the same plane. A sequestrated disc was one in which the disc material was clearly separate from the originating disc6). Disc degeneration was divided into five grades based on findings on the MRI, as derived from the previous work of Pfirrmann et al. (Table 1)21).
Fig. 1.
Schematic drawings showing measurement of disc height ratio. Disc height ratio = (a / A).
Table 1.
Grading system of disc degeneration21)
Clinical outcome evaluation
For each group, before and after revision OLM, pain was measured by the 10-point Visual Analogue Scale (VAS) scoring (0-10), function was assessed by the Oswestry Disability Index (ODI) scoring (0-100)10) and postoperative satisfaction was evaluated using a patient's subjective satisfaction rate (0-100%)22). Clinical success was defined as : ≥2 point improvement in VAS scores, ≥25% improvement in ODI score, ≥50% patient's subjective satisfaction rate and no major complication related to the surgery22). Complications were categorized using the classification scheme described by Carreon et al.2), dividing them into major and minor complications. Major complications were those that had a negative effect on a patient's recovery, whereas minor complications were those that had not affected recovery significantly. Pre- and postoperative data were assessed using clinical charts and operative reports. All patients visited the outpatient department in June 2007 and a trained nurse collected follow-up clinical data.
Statistical analysis
Statistical analysis was done using Chi-square tests, Fisher's exact test, independent T test, and Mann-Whitney U test. The Odds ratio for significant variables was calculated by binary multi-logistic regression analysis. A p value of less than 0.05 was considered significant. The SAS (version 8.1) program was used for all statistical analysis.
RESULTS
Risk factors for contralateral reherniation
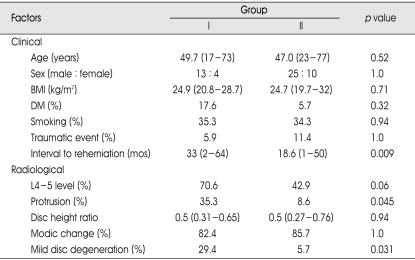
The mean age of patients at initial surgery was 49.7 years (range, 17-73 years) in Group I, and 47.0 years (range, 23-77 years) in Group II, which was not significantly different between the two groups (p=0.52). Group I consisted of 13 men and 4 women, and Group II of 25 men and 10 women. The male to female ratio was not significantly different between the two groups (p=1.0). The mean body mass index at initial surgery was 24.9 kg/m2 (range, 20.8-28.7 kg/m2) for Group I, and 24.7 kg/m2 (range, 19.7-32.0 kg/m2) for Group II, which was not significantly different between the two groups (p=0.71). Three patients (17.6%) in Group I, and two patients (5.7%) in Group II had a history of diabetes mellitus at initial surgery but the incidence was not significantly different between the two groups (p=0.32). The incidence of patients with a history of chronic smoking at initial surgery was not significantly different between the two groups (Group I : 35.3% vs. Group II : 34.3%, p=0.94). The incidence of patients with a history of traumatic event was also not significantly different between the two groups (Group I : 5.9% vs. Group II : 11.4%, p=1.0). The time interval to reherniation from the initial surgery was significantly different between the two groups (Group I : 33.0 months vs. Group II : 18.6 months, p=0.009).
Contralateral reherniation showed a trend toward a higher incidence at L4-5 spinal level (70.6%) compared with ipsilateral ones (42.9%), although this was not statistically significant (p=0.06). Considering extent of herniated disc at initial surgery, the incidence of protrusion was significantly higher in Group I (35.3%) than Group II (8.6%) (p=0.045). The mean disc height ratio at initial surgery was not significantly different between the two groups (Group I : 0.5 (range, 0.31-0.65) vs. Group II : 0.5 (range, 0.27-0.76), p=0.94). The incidence of Modic change at initial surgery was not significantly different between the two groups (Group I : 82.4% vs. Group II : 85.7%, p=1.0). The incidence of mild disc degeneration (grade I-III by the classification of Pfirrmann et al.) at initial surgery was significantly higher in Group I (29.4%) compared with Group II (5.7%) (p=0.031) (Table 2).
Table 2.
Comparison of clinical and radiological factors between contralateral and ipsilateral reherniations
BMI : body mass index, DM : diabetes mellitus
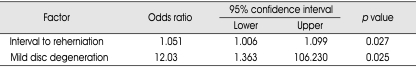
On binary multi-logistic regression analysis, time interval to reherniation (p=0.027, Odds ratio=1.051 (95% confidence interval : 1.006-1.099)) and mild disc degeneration at initial surgery (p=0.025, Odds ratio=12.03 (95% confidence interval : 1.363-106.230)) were significant factors differentiating the development of contralateral reherniations from ipsilateral ones (Table 3).
Table 3.
Results of binary multi-logistic regression analysis
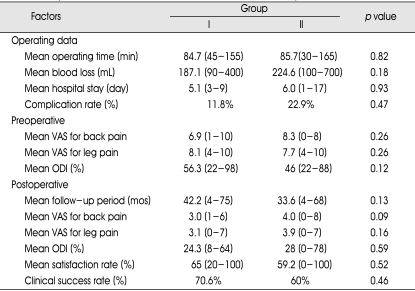
Clinical outcomes
For Group I, mean operating time was 84.7 minutes (range, 45-155 minutes), and mean estimated blood loss was 187.1 mL (range, 90-400 mL) during revision OLM. Mean hospital stay after revision OLM was 5.1 day (range, 3-9 days). Complications occurred in two patients (11.8%). Unintended durotomy happened in two patients during revision OLM, which was treated by primary suture. For Group II, mean operating time was 85.7 minutes (range, 30-165 minutes), and mean estimated blood loss was 224.6 mL (range, 100-700 mL) during revision OLM. Mean hospital stay after revision OLM was 6.0 days (range, 1-17 days). Complications occurred in eight patients (22.9%). Unintended durotomy was occurred in seven patients during revision OLM, which was treated by primary suture. Major complication occurred in one patient, which was foot drop due to nerve root injury during revision OLM and this was not recovered at the final follow-up. There was no significant difference in mean operating time, mean blood loss, mean hospital stay or complication rate between the two groups (p=0.82, p=0.18, p=0.93, and p=0.47, respectively).
For Group I, mean follow-up duration after revision OLM was 42.2 months (range, 4-75 months). The mean preoperative VAS score for back pain was 6.9 (range 1-10) and improved after surgery to 3.0 (range 1-6) (p<0.001). The mean preoperative VAS score for leg pain was 8.1 (range, 4-10) and improved after surgery to 3.1 (range, 0-7) (p<0.001). The mean preoperative ODI score was 56.3% (range, 22-98%) and improved after surgery to 24.3% (range, 8-64%) (p<0.001). The mean subjective satisfaction rate at the last follow-up evaluation was 65% (range 20-100%). Clinical success was seen in 12 of 17 patients (70.6%). For Group II, mean follow-up duration after revision OLM was 33.6 months (range, 4-68 months). The mean preoperative VAS score for back pain was 8.3 (range, 0-8) and improved after surgery to 4.0 (range, 0-8) (p<0.001). The mean preoperative VAS score for leg pain was 7.7 (range, 4-10) and improved after surgery to 3.9 (range, 0-7) (p<0.001). The mean preoperative ODI score was 46.0% (range, 22-88%) and improved after surgery to 28.0% (range 0-78%) (p<0.001). The mean subjective satisfaction rate at the last follow-up evaluation was 59.2% (range, 0-100%). Clinical success was seen in 21 of 35 patients (60%). There was no significant difference of mean follow-up time between the two groups (p=0.13). There was no significant difference in the preoperative VAS scores for back pain, leg pain, and ODI scores between the two groups (p=0.26, p=0.26, and p=0.12, respectively). There was no significant difference in the postoperative VAS scores for back pain, leg pain, ODI scores, satisfaction rate, and clinical success rate between the two groups (p=0.09, p=0.16, p=0.59, p=0.52, and p=0.46, respectively) (Table 4).
Table 4.
Comparison of clinical outcomes between contralateral and ipsilateral reherniations
VAS : visual analogue scale, ODI : Oswestry Disability Index
DISCUSSION
Although there have been many studies on ipsilateral reherniation, the literature on the contralateral reherniation after OLM is sparse3,18). The incidence of contralateral reherniation has been reported to be lower than that of ipsilateral reherniation. O'Sullivan et al.18) reported that, of 76 patients who needed reoperation after disc excision, 21% had contralateral reherniation and 44% had ipsilateral reherniation. Cinotti et al.3) reported that, of 50 patients with recurrent disc herniation operated on during 6.6 years, 34% had contralateral reherniation and 56% had ipsilateral reherniation. The results of the present study correspond well with previous studies; of 52 patients who underwent revision OLM due to reherniation at the same level as primary OLM, 17 patients (32.7%) had contralateral reherniation and 35 patients (67.3%) had ipsilateral reherniation.
Suggested risk factors for reherniation after OLM are all associated with ipsilateral reherniation. Young age, male gender, smoking, and traumatic event were suggested as clinical factors linked with ipsilateral reherniation, though this idea is still controversial25,26). Considering radiological risk factors for ipsilateral reherniation, Yorimitsu et al.29) reported that preserved disc height at initial surgery was correlated with ipsilateral reherniation. Cinotti et al.4) reported that severe disc degeneration was related with ipsilateral reherniation. In contrast, Dora et al.6) reported that minor disc degeneration was a risk factor for ipsilateral reherniation. Carragee et al.1) found that an extruded fragment with massive posterior annular loss had the highest prevalence of ipsilateral reherniation. Until now, the relationship between risk factors and the development of contralateral reherniation after OLM has not been investigated.
The pathogenic mechanism of contralateral reherniation has been considered as being different from that of ipsilateral reherniation. Jacchia et al.12) hypothesized that incomplete removal of the disc on the contralateral side during primary discectomy might cause protrusion through the external annulus on the contralateral side, which was damaged during primary discectomy. Cinotti et al.3) showed controversial results; of 16 patients with contralateral reherniation, annulotomy was extended on central posterior annulus only in three patients during primary discectomy, whereas limited annulotomy was performed on 13 patients during primary discectomy. According to the results of the present study, the interval to reherniation from initial surgery and the grade of disc degeneration at initial surgery were key factors distinguishing the development of contralateral reherniations from ipsilateral ones. Patients with contralateral reherniation showed significantly longer mean time-interval to reherniation compared with patients with ipsilateral reherniation (33 vs. 18.6 month). The risk for the development of contralateral reherniation increased 5.1 percent per month after initial OLM, when compared with ipsilateral reherniation (p=0.027, Odds ratio=1.051 (95% confidence interval : 1.006-1.099)). Annulus on the contralateral side, which was healthier and stronger than annulus on the ipsilateral side at the time of primary OLM, might weaken as time progresses, which could result in later occurrence of contralateral reherniation than ipsilateral reherniation. Another risk factor differentiating development of contralateral reherniation from ipsilateral reherniation would be mild disc degeneration at initial OLM. Patients with mild disc degeneration (grade I-III by the classification of Pfirrmann et al.) at initial OLM has a 12.03 fold increased risk for the development of contralateral reherniation, compared with ipsilateral reherniation (p=0.025, Odds ratio=12.03 (95% confidence interval : 1.363-106.230)), although the pathogenic mechanism still remains to be clarified. Therefore, to prevent contralateral reherniation, more vigorous removal of disc in the contralateral side is recommended during primary discectomy, especially for patients with mild disc degeneration. Unlike to this, the amount of removed disc in the ipsilateral side seems important to prevent ipsilateral reherniation because of significantly shorter time-interval to reherniation after primary discectomy compared with contralateral reherniation. Further prospective study measuring the amount of removed disc during primary discectomy might reveal the relationship between amount of removed disc and incidence of ipsilateral reherniation.
One of the concerns about revision OLM for ipsilateral reherniation is the increased risk of surgical complications due to scar tissue. Unlike ipsilateral reherniation, the risk of surgical complications has generally been considered low in contralateral reherniation owing to lack of scar tissue formation. In the present study, the surgical complication rate of contralateral reherniation was lower than that of ipsilateral reherniation, as expected. Major complication (foot drop) occurred in one patient in the ipsilateral reherniation group. However, the difference in complication rate was not statistically significant between the two groups (11.8% for Group I vs. 22.9% for Group II, p=0.47).
For ipsilateral reherniation, revision open discectomy is the most commonly performed surgical treatment, while spinal fusion is generally preserved for ipsilateral reherniation with instability25,26,28). On the other hand, spinal fusion has been considered necessary for contralateral reherniation because of the possibility of unsatisfactory results, which might result from additional damage of vertebral motion segment during revision surgery3). To the best of our knowledge, there has been only one study specifically focusing on the surgical outcomes of contralateral reherniation. Cinotti et al.3) compared 16 patients with contralateral reherniation, who underwent revision discectomy, to 50 patients who underwent open discectomy and showed no recurrent pain. Clinical results of reoperation for contralateral reherniation were favorable and comparable to those of primary discectomy; thus, they concluded that fusion was not necessary for contralateral reherniation. In the present study, the clinical outcomes of revision OLM for contralateral reherniation were compared with those for ipsilateral reherniation. Back pain, leg pain, and functional status were significantly improved after revision OLM in both groups, and the levels of improvement were comparable between the two groups.
Based on the results of the present study, revision OLM seems to be a good treatment option for patients with reherniation after primary discectomy, regardless of the side of reherniation. However, mean satisfaction rates and clinical success rates were relatively low in both groups, which still suggest the necessity of spinal fusion for patients showing poor clinical outcomes. Future studies concerning risk factors for poor clinical outcomes after revision OLM might elucidate more effective surgical strategies treating reherniations.
To our knowledge, this is the first study to evaluate the risk factors differentiating development of contralateral reherniation from that of ipsilateral reherniation. It is also the first to compare surgical outcomes of revision OLM for contralateral reherniation with those for ipsilateral reherniation. However, the retrospective study design and relatively small number of patients included should be considered when interpreting the results of the present study.
CONCLUSION
The interval to reherniation from initial surgery and the grade of degeneration at initial surgery were key factors that distinguished the development of contralateral reherniations from ipsilateral ones. To prevent contralateral reherniation, more vigorous removal of disc in the contralateral side is recommended during primary discectomy, especially for patients with mild disc degeneration. Though revision OLM seems to be a good treatment option for patients with reherniation after primary discectomy, regardless of the side of reherniation, relatively low clinical success rates still suggest the necessity of spinal fusion for patients showing poor clinical outcomes.
Acknowledgements
This study was supported by a grant from the Wooridul Spine Foundation.
References
- 1.Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica : the effects of fragment type and annular competence. J Bone Joint Surg Am. 2003;85:102–108. [PubMed] [Google Scholar]
- 2.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85:2089–2092. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Cinotti G, Gumina S, Giannicola G, Postacchini F. Contralateral recurrent lumbar disc herniation : results of discectomy compared with those in primary herniation. Spine. 1999;24:800–806. doi: 10.1097/00007632-199904150-00012. [DOI] [PubMed] [Google Scholar]
- 4.Cinotti G, Roysam GS, Eisenstein SM, Postacchini F. Ipsilateral recurrent lumbar disc herniation. A prospective, controlled study. J Bone Joint Surg Br. 1998;80:825–832. doi: 10.1302/0301-620x.80b5.8540. [DOI] [PubMed] [Google Scholar]
- 5.Dai LY, Zhou Q, Yao WF, Shen L. Recurrent lumbar disc herniation after discectomy : outcome of repeat discectomy. Surg Neurol. 2005;64:226–231. doi: 10.1016/j.surneu.2004.11.003. discussion 231. [DOI] [PubMed] [Google Scholar]
- 6.Dora C, Schmid MR, Elfering A, Zanetti M, Hodler J, Boos N. Lumbar disk herniations : do MR imaging findings predict recurrence after surgical diskectomy? Radiology. 2005;235:562–567. doi: 10.1148/radiol.2352040624. [DOI] [PubMed] [Google Scholar]
- 7.Ebeling U, Kalbarcyk H, Reulen HJ. Microsurgical reoperation following lumbar disc surgery : timing, surgical findings, and outcome in 92 patients. J Neurosurg. 1989;70:397–404. doi: 10.3171/jns.1989.70.3.0397. [DOI] [PubMed] [Google Scholar]
- 8.Epstein JA, Lavine LS, Epstein BS. Recurrent herniation of the lumbar intervertebral disk. Clin Orthop Relat Res. 1967;52:169–178. doi: 10.1097/00003086-196700520-00013. [DOI] [PubMed] [Google Scholar]
- 9.Erbayraktar S, Acar F, Tekinsoy B, Acar U, Güner EM. Outcome analysis of reoperations after lumbar discectomies : a report of 22 patients. Kobe J Med Sci. 2002;48:33–41. [PubMed] [Google Scholar]
- 10.Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 11.Herron L. Recurrent lumbar disc herniation : results of repeat laminectomy and discectomy. J Spinal Disord. 1994;7:161–166. doi: 10.1097/00002517-199407020-00010. [DOI] [PubMed] [Google Scholar]
- 12.Jacchia GE, Bardelli M, Barile L, D'arienzo M, Innocenti M. Casistica, risultati e cause di insuccessi di ernie discali operate. Ital J Orthop Traumatol. 1980;6:5–23. [Google Scholar]
- 13.Le H, Sandhu FA, Fessler RG. Clinical outcomes after minimal-access surgery for recurrent lumbar disc herniation. Neurosurg Focus. 2003;15:E12. doi: 10.3171/foc.2003.15.3.12. [DOI] [PubMed] [Google Scholar]
- 14.Lee SH, Chung SE, Ahn Y, Kim TH, Park JY, Shin SW. Comparative radiologic evaluation of percutaneous endoscopic lumbar discectomy and open microdiscectomy. Mt Sinai J Med. 2006;73:795–801. [PubMed] [Google Scholar]
- 15.Masaryk TJ, Ross JS, Modic MT, Boumphrey F, Bohlman H, Wilber G. High resolution MR imaging of sequestrated lumbar intervertebral disks. Am J Roentgenol. 1988;150:1155–1162. doi: 10.2214/ajr.150.5.1155. [DOI] [PubMed] [Google Scholar]
- 16.Mochida J, Nishimura K, Nomura T. Appropriate procedure of posterior herniotomy and percutaneous nucleotomy in lumbar disc herniation. Rinsho Seikei Geka. 1994;29:423–430. [Google Scholar]
- 17.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease : assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166:193–199. doi: 10.1148/radiology.166.1.3336678. [DOI] [PubMed] [Google Scholar]
- 18.O'Sullivan MG, Connolly AF, Buckley TF. Recurrent lumbar disc protrusion. Br J Neurosurg. 1990;4:319–326. doi: 10.3109/02688699008992741. [DOI] [PubMed] [Google Scholar]
- 19.Ozgen S, Naderi S, Ozek MM, Pamir MN. Findings and outcome of revision lumbar disc surgery. J Spinal Disord. 1999;12:287–292. [PubMed] [Google Scholar]
- 20.Papadopoulos EC, Girardi FP, Sandhu HS, Sama AA, Parvataneni HK, O'Leary PF, et al. Outcome of revision discectomies following recurrent lumbar disc herniation. Spine. 2006;31:1473–1476. doi: 10.1097/01.brs.0000219872.43318.7a. [DOI] [PubMed] [Google Scholar]
- 21.Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001;26:1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 22.Shim CS, Lee SH, Shin HD, Kang HS, Choi WC, Jung B, et al. CHARITE versus ProDisc : a comparative study of a minimum 3-year follow-up. Spine. 2007;32:1012–1018. doi: 10.1097/01.brs.0000260795.57798.a0. [DOI] [PubMed] [Google Scholar]
- 23.Silvers HR, Lewis PJ, Asch HL, Clabeaux DE. Lumbar diskectomy for recurrent disk herniation. J Spinal Disord. 1994;7:408–419. [PubMed] [Google Scholar]
- 24.Spengler DM. Lumbar discectomy : results of a limited disc excision and selective foraminotomy. Spine. 1982;7:604–607. [PubMed] [Google Scholar]
- 25.Suk KS, Lee HM, Moon SH, Kim NH. Recurrent lumbar disc herniation : results of operative management. Spine. 2001;26:672–676. doi: 10.1097/00007632-200103150-00024. [DOI] [PubMed] [Google Scholar]
- 26.Swartz KR, Trost GR. Recurrent lumbar disc herniation. Neurosurg Focus. 2003;15:E10. doi: 10.3171/foc.2003.15.3.10. [DOI] [PubMed] [Google Scholar]
- 27.Torma T. Post-operative recurrence of lumbar disc herniation. Acta Chir Scand. 1952;103:213–221. [PubMed] [Google Scholar]
- 28.Tsai CH, Hsu HC, Chen YJ, Lin CJ, Chen HT. Recurrent lumbar disc herniation after discectomy : clinical result of repeated discectomy and analysis of factors affecting surgical outcome. Mid Taiwan J Med. 2007;12:125–132. [Google Scholar]
- 29.Yorimitsu E, Chiba K, Toyama Y, Hirabayashi K. Long-term outcomes of standard discectomy for lumbar disc herniation : a follow-up study of more than 10 years. Spine. 2001;26:652–657. doi: 10.1097/00007632-200103150-00019. [DOI] [PubMed] [Google Scholar]