Abstract
Many approaches for crowded mandibular anterior teeth are currently employed: distal movement of posterior teeth, lateral movement of canines, labial movement of incisors, interproximal enamel reduction, removal of premolars, removal of one or two incisors, and various combinations of the above. Selecting the best treatment is often difficult, and all guidelines do not apply to every case. Treatment by extraction of one single mandibular incisor is not popular in the orthodontic profession despite the apparent advantages of the extraction in the region of crowding. A case report is presented one mandibular incisor extraction treatment of a 16 year-old female with a Class I malocclusion that shows a significant mandibular arch length deficiency and mandibular tooth-size excess. In this case, the degree of mandibular anterior dental crowding, existing mandibular tooth-size excess, and the dental midline discrepancy were indicated the extraction of one mandibular incisor.
Keywords: Mandibular incisor extraction, Bolton discrepancy
INTRODUCTION
One of the most critical decisions in treatment planning is whether to extract teeth. The orthodontic pendulum has swung from a predominantly non-extraction philosophy in the early 1900s, toward a more extraction-oriented therapy in the middle of the century, and now back toward a non-extraction emphasis.1
Several approaches for crowded mandibular anterior teeth are currently employed: distal movement of posterior teeth, lateral movement of canines, labial movement of incisors, interproximal enamel reduction, removal of premolars, removal of one or two incisors, and various combinations of the above. Selecting the best treatment is often difficult, and all guidelines do not apply to every case.2
Treatment by extraction of one single mandibular incisor is not popular in the orthodontic profession despite the apparent advantages of the extraction in the region of crowding.3,4 Objections to this extraction option have been based on case reports or subjective clinical opinions after observing less desirable outcomes in treated Class I and Class II malocclusions.1,2,5,6 Unwanted side-effects have been increases of overbite and overjet beyond acceptable limits, space reopening, partly unsatisfactory posterior occlusion, recurrence of crowding in the remaining three incisors, and unaesthetic loss of the interdental papillae in the mandibular anterior region.1,2,5–8
Kokich and Shapiro5 stated that if lower incisor extraction is performed without careful planning, the resulting occlusal discrepancy often cannot be resolved satisfactorily. They argued that with careful case selection, single incisor extraction may allow the clinicians to use simple treatment mechanics and achieve good results. A careful and realistic diagnostic setup was considered to be an important aid in determining tooth size discrepancies, and whether or not the occlusal result would be acceptable and consistent with the treatment objectives.
Several authors5,6,9–11 have emphasized that case where a tooth-size discrepancy (measurable mandibular Bolton excess) exists, for example with upper peg shaped laterals or missing upper lateral incisors may represent good indications for extraction of one mandibular incisor. Some authors have remarked that cases with Class III tendency could be another indication for incisor extraction, because some collapse of the lower arch may be acceptable or even desirable in such instances.8,12
Whenever single lower incisor extraction treatment is contemplated, a full diagnostic setup should be made. Tooth-size formulas are not consistently accurate in predicting a final occlusion; a full setup is the best way to be sure the occlusal results, including overbite and overjet, will be acceptable.1
According to Owen,1 patients who are suitable for single lower incisor extractions usually fit the following diagnostic pattern: Class I molar relationship, moderately crowded lower incisors, mild or no crowding in the upper arch, acceptable soft-tissue profile, minimal to moderate overbite and overjet, no or minimal growth potential, and missing lateral incisors or peg shaped laterals.
The aim of this case report was to assess the treatment outcome and changes in dentofacial structures especially mandibular incisor position after extraction of one single lower incisor.
HISTORY AND DIAGNOSIS
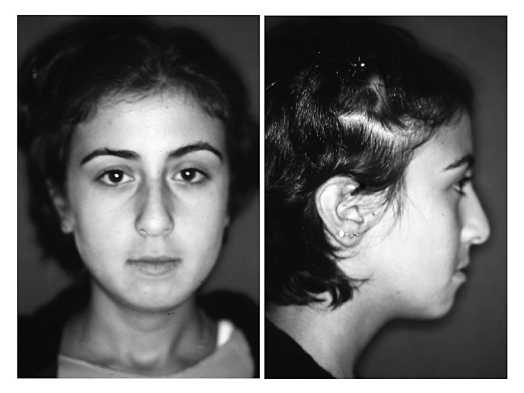
A 15-year-old Caucasian female came to the Department of Orthodontics, Ondokuz Mayis University Faculty of Dentistry for orthodontic treatment with the chief complaint of upper and lower crowding. She was in the permanent dentition and had a symmetric face with a convex profile (Figure 1). She had no important dental and medical history, and no growth potential.
Figure 1.
Pretreatment facial photographs.
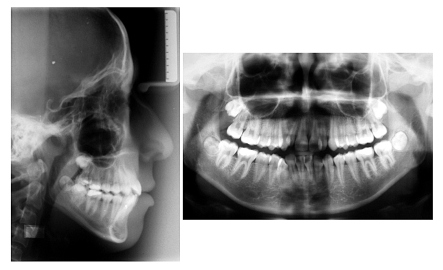
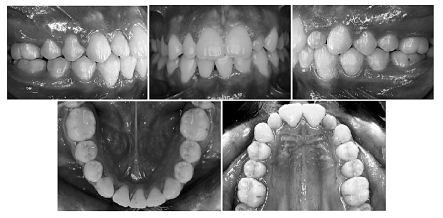
Intraoral examination showed that there was present mild crowding in the upper arch and severe crowding in anterior region of the lower arch. In occlusion, she had a 1 mm over-bite and a 2.5 mm over-jet. There was Class I molar relationship on the left side and Class II tendency on the right side. Her maxillary midline was shifted 1 mm to the right, and the mandibular midline was shifted 2 mm to the left. No mandibular shift was detected on closure. Upper lateral incisors were peg shaped and left lateral incisor was in cross-bite. The arch length deficiencies were 3 mm in the maxillary arch and 8 mm in the mandibular arch. A Bolton analysis showed 8.5 mm mandibular excess in total and 5.7 mm mandibular anterior excess (Figure 2).
Figure 2.
Pretreatment intraoral photographs.
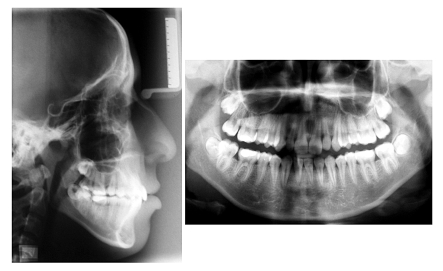
Radiographic examination revealed that all the permanent teeth were present or developing. Cephalometric evaluation showed that she had a skeletal Class I relationship with high angle pattern and lower lip was slightly protrusive to the “E” line. The maxilla and the mandible were both retrognathic relative to the cranium (Figure 3) (Table 1).
Figure 3.
Pretreatment cephalometric and panoramic radiographs.
Table 1.
Pretreatment and posttreatment cephalometric measurements.
| Pretreatment | Posttreatment | |
|---|---|---|
| Skeletal analysis | ||
| S-N-A (°) | 75.9 | 75.3 |
| S-N-B (°) | 73.4 | 73.1 |
| A-N-B (°) | 2.5 | 2.2 |
| S-N/Go-Me (°) | 46.6 | 46.0 |
| ANS-PNS/Go-Me (°) | 36.5 | 35.5 |
| Posterior/Anterior ratio (%) | 59.8 | 59.9 |
| N-Me (mm) | 125.9 | 127.4 |
| S-Go (mm) | 75.3 | 76.3 |
| Wits appraisal | −1.8 | −1.0 |
| Dental analysis | ||
| Upper incisor to N-A (mm) | 5.6 | 5.4 |
| Upper incisor to N-A (°) | 28.6 | 27.6 |
| Upper incisor to ANS-PNS (°) | 115.1 | 114.0 |
| Upper incisor to A-Pg (mm) | 7.7 | 7.3 |
| Lower incisor to N-B (mm) | 5.2 | 5.3 |
| Lower incisor to N-B (°) | 27.3 | 25.6 |
| Lower incisor to A-Pg (mm) | 4.3 | 3.8 |
| IMPA (°) | 87.4 | 86.5 |
| Interincisal angle (°) | 121.5 | 124.0 |
| Overjet (mm) | 2.5 | 3.0 |
| Overbite (mm) | 1.0 | 3.0 |
| Soft tissue analysis | ||
| Lower lip to E-line (mm) | 2.1 | 2.2 |
| Nasolabial angle (°) | 100.6 | 98.2 |
| Holdaway H angle (°) | 3.8 | 5.4 |
TREATMENT OBJECTIVES
The goals of orthodontic treatment for the patient were to (1) eliminate the dental crowding in the lower and upper arch; (2) correct the maxillary dental midline discrepancy; (3) establish a Class I molar and canine relationship, (4) maintain the overjet and improve the overbite; (5) provide for a more regular alignment of the maxillary and mandibular teeth for aesthetics, function and hygiene; (6) maintain the acceptable facial balance and muscle tone; and (7) compensate for the relative excess mandibular tooth mass with the removal of one mandibular incisor.
TREATMENT ALTERNATIVES
Considering all aspects of the case in detail, during the treatment-planning interview, two treatment options were presented to the patient. The first involved extraction of one single mandibular incisor and restoration of the peg shaped maxillary lateral incisors after the orthodontic treatment. This would allow easy resolving of the lower crowding and improvement of the overbite. The second option involved extraction of the all first premolar and restoration of the peg shaped maxillary lateral incisors. The patient chose the first option.
TREATMENT PROGRESS
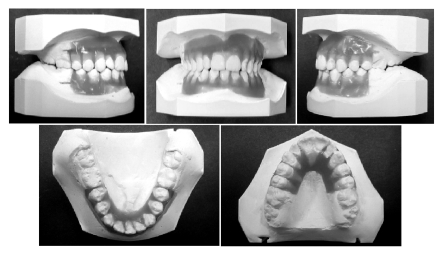
First of all, a diagnostic wax set-up was constructed with the extraction of the lower right lateral incisor for evaluation of the treatment outcomes (Figure 4). It showed that overjet, overbite and posterior occlusion would be acceptable.
Figure 4.
Diagnostic wax set-up models.
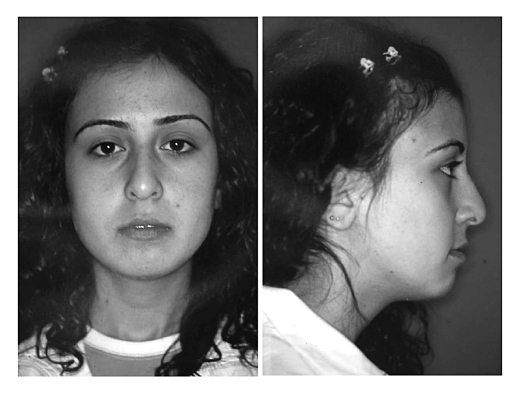
The mandibular right lateral incisor was extracted, and treatment started with a fixed appliance in the lower and upper arches (Straight Wire 0.022”, Roth Setup). Initial levelling was accomplished with the use of nickel titanium archwires over 4 months. After initial levelling, a compressed coil spring was applied to open space for upper left lateral incisor with .018-inch stainless steel archwire. After the opening of space, double arch (.012-inch NiTi) was placed to correct the cross bite of upper left lateral incisor. In the lower arch, segments of elastomeric chain were used at the onset of treatment to close the extraction space. Compensating bends were placed in the lower archwire to prevent excessive crown tipping at the extraction site. After 9 months (from the time of placing full appliances) all teeth were aligned and the extraction space was closed. For the remaining 7 months, .019x.025-inch rectangular stainless steel wires were used for torque corrections, paralleling the roots, and detailing the occlusion. After satisfactory interdigitation was achieved, the fixed appliances were removed, and maxillary removable retainer and mandibular fixed lingual retainer were placed (Figures 5, 6 and 7).
Figure 5.
Posttreatment facial photographs.
Figure 6.
Posttreatment intraoral photographs.
Figure 7.
Posttreatment cephalometric and panoramic radiographs.
The active orthodontic treatment time was 16 months. After debonding procedures, peg shaped maxillary lateral incisors were restored with composite resin (Figure 8).
Figure 8.
Intraoral photographs after restoration of upper lateral incisors.
RESULTS AND DISCUSSION
The Class I molar and canine relationship were established with satisfactory interdigitation of posterior teeth. The overjet was maintained, and the overbite was improved. The upper and lower arch length deficiencies was eliminated and the tooth-size discrepancy was managed successfully. The mandibular dental midline was become the center of the remaining lower central incisor. The dentition and the periodontal tissues remained healthy during treatment. Unaesthetic loss of the inter-dental papillae between the lower central incisors was occurred as an unwanted side-effect.
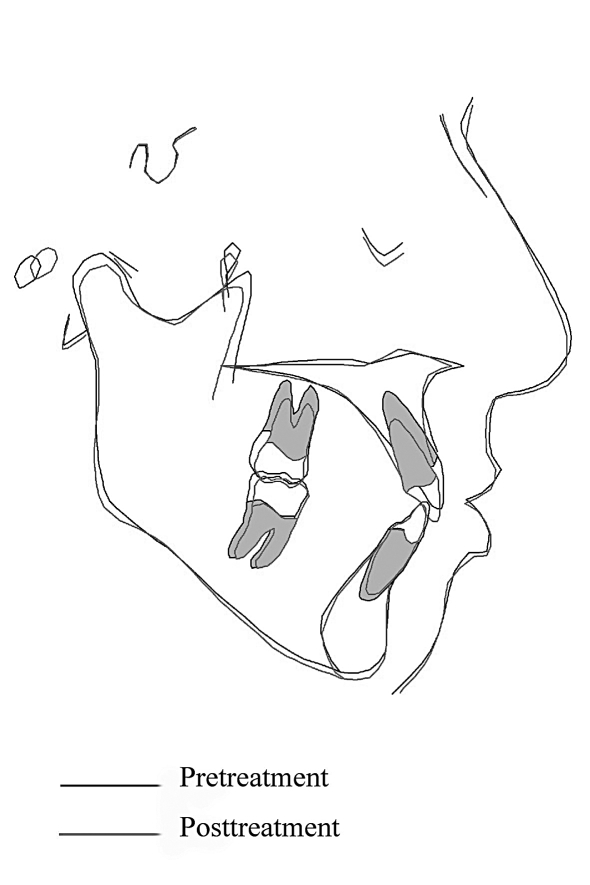
Posttreatment radiographs showed that minimal root resorption had occurred during treatment and that root parallelism was satisfactory. Cephalometric evaluation revealed that no significant changes were occurred except the increasing of the overbite. The lower and the upper incisors were retroclined slightly, and the interincisal angle was decreased (Table 1) (Figure 9).
Figure 9.
Superimposition of pretreatment and posttreatment cephalometric tracings.
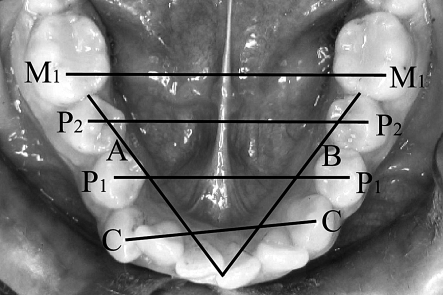
Lower cast analysis (Figure 10) showed that there was no change in the arch length, the inter-canine width was decreased, and interpremolar and intermolar widths were increased (Table 2).
Figure 10.
Measurement technique for cast analysis. (A+B: arch length, C-C: intercanine width, P1-P1: width between the first premolars, P2-P2: width between the second premolars, M1-M1: intermolar width)
Table 2.
Measurements evaluated on the lower casts.
| Before Treatment (mm) | After Wax Set-up (mm) | After Treatment (mm) | |
|---|---|---|---|
| Arch Length | 63,74 | 63,80 | 63,48 |
| Intercanine Width | 26,10 | 23,96 | 25,20 |
| P1-P1 Width | 32,12 | 33,54 | 35,10 |
| P2-P2 Width | 37,66 | 38,58 | 40,52 |
| Intermolar Width | 43,40 | 43,66 | 44,42 |
A class I malocclusion with a significant mandibular tooth-size excess can frequently be treated by extracting one mandibular incisor in the literature.5,8,13 A mandibular tooth-size excess greater than 1.6 mm, as determined by the Bolton analysis14, is considered significant and can typically be handled in 1 of 3 ways: interproximal reduction, extraction, or restoration. Extraction of one mandibular incisor is generally done in patients with Bolton discrepancies greater than 2.0 mm. The decision to extract should be supported by initial records, diagnostic wax set-up, and clinical experience. Additional information, such as Bolton analysis, shape of maxillary incisor crowns, and amount of interproximal enamel is also important.15
Reidel13 has suggested that in patients with severely crowded mandibular arches, the removal of one or more mandibular incisor(s) is the only logical alternative which may allow for increased stability of the mandibular anterior region without continuous retention.16 In this case, we believed that treatment results would be stable because of the fact that intercanine width was decreased, and the lower incisors were not protruded.
CONCLUSIONS
One single mandibular incisor extraction can be an effective treatment choice for the appropriate malocclusion with a Bolton discrepancy. However, several factors must be considered before making the final treatment decision. In addition, evaluation of a diagnostic wax set-up will allow the orthodontist to predict the success of the proposed treatment plan.
References
- 1.Owen AH. Single lower incisor extractions. J Clin Orthod. 1993;27:153–160. [PubMed] [Google Scholar]
- 2.Valinoti JR. Mandibular incisor extraction therapy. Am J Orthod Dentofac Orthop. 1994;105:107–116. doi: 10.1016/S0889-5406(94)70106-7. [DOI] [PubMed] [Google Scholar]
- 3.Gottlieb E, Nelson AH, Vogels DS. JCO study of orthodontic diagnosis and treatment procedures. Part I: Results and trends. J Clin Orthod. 1996;30:615–629. [PubMed] [Google Scholar]
- 4.Travess H, Harry DR, Sandy J. Orthodontics. Part 8: Extraction in orthodontics. Br Dent J. 2004;196:195–203. doi: 10.1038/sj.bdj.4810979. [DOI] [PubMed] [Google Scholar]
- 5.Kokich VG, Shapiro PA. Lower incisor extraction in orthodontic treatment: four clinical reports. Angle Orthod. 1984;54:139–153. doi: 10.1043/0003-3219(1984)054<0139:LIEIOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Klein DJ. The mandibular central incisor, an extraction option. Am J Orthod Dentofac Orthop. 1997;111:253–259. doi: 10.1016/s0889-5406(97)70182-3. [DOI] [PubMed] [Google Scholar]
- 7.Dacre JT. The long term effects of one lower incisor extraction. Eur J Orthod. 1985;53:706–713. doi: 10.1093/ejo/7.2.136. [DOI] [PubMed] [Google Scholar]
- 8.Canut JA. Mandibular incisor extraction: indications and long-term evaluation. Eur J Orthod. 1996;18:485–489. doi: 10.1093/ejo/18.5.485. [DOI] [PubMed] [Google Scholar]
- 9.Pauls HJ. Mandibular incisor extraction: case report. J Orofac Orthop. 1999;60:435–443. doi: 10.1007/BF01388196. [DOI] [PubMed] [Google Scholar]
- 10.Grob DJ. Extraction of a mandibular incisor in a Class I malocclusion. Am J Orthod Dentofac Orthop. 1995;108:533–541. doi: 10.1016/s0889-5406(95)70054-4. [DOI] [PubMed] [Google Scholar]
- 11.Hinkle F. Incisor extraction case report. Am J Orthod Dentofac Orthop. 1987;92:94–97. doi: 10.1016/0889-5406(87)90363-5. [DOI] [PubMed] [Google Scholar]
- 12.FærØvig E, Zachrisson BU. Effect of mandibular incisor extraction on anterior occlusion in adults with Class III malocclusion and reduced overbite. Am J Orthod Dentofac Orthop. 1999;115:113–124. doi: 10.1016/s0889-5406(99)70337-9. [DOI] [PubMed] [Google Scholar]
- 13.Riedel RA, Little RM, Bui TD. Mandibular incisor extraction: postretention evaluation of stability and relapse. Angle Orthod. 1992;62:103–116. doi: 10.1043/0003-3219(1992)062<0103:MIEPEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Bolton WA. Disharmony in tooth size and its relation to analysis and treatment of malocclusion. Angle Orthod. 1958;28:113–130. [Google Scholar]
- 15.Kokich VO. Treatment of a Class I malocclusion with a carious mandibular incisor and no Bolton discrepancy. Am J Orthod Dentofac Orthop. 2000;118:107–113. doi: 10.1067/mod.2000.108562. [DOI] [PubMed] [Google Scholar]
- 16.Blake M, Bibby K. Retention and stability: A review of the literature. Am J Orthod Dentofac Orthop. 1998;114:299–306. doi: 10.1016/s0889-5406(98)70212-4. [DOI] [PubMed] [Google Scholar]