Abstract
Purpose:
To document the status of pediatric eye care in India.
Materials and Methods:
A list of institutions providing eye care was compiled from various sources, including government officials, professional bodies of ophthalmologists, and national and international non-governmental organizations (NGO) working in the field of eye care in India. A questionnaire on eye care services was sent to all known eye care institutions in the country. Workshops and regional meetings were organized to maximize response. Validity of data was ensured by observational visits to 10% of the institutions who responded.
Results:
Out of 1204 institutions contacted, 668 (55.5%) responded to the questionnaire. Of these, 192 (28.7%) reported that they provided pediatric eye care services. A higher proportion (48.3%) of NGO hospitals reported separate pediatric ophthalmology units compared to other providers (P< 0.001). Eighty per cent of advanced care eye hospitals had dedicated outpatient, and 40% had dedicated inpatient facilities for children (P< 0.001). The advanced eye care hospitals attended to a larger number of pediatric clients (P < 0.001), and performed more pediatric eye surgeries compared to secondary and tertiary care hospitals (P < 0.001). Eighty- three per cent of advanced care centers and 72.4% of NGO hospitals had an anesthesiologist for pediatric eye service. Refractive error was the commonest reason for seeking service. The commonest surgical procedure was pediatric cataract surgery followed by squint surgery.
Conclusion:
Pediatric eye care services are not adequate in India.
Keywords: Childhood blindness, eye care infrastructure, pediatric eye care
Control of childhood blindness is one of the priorities identified for achieving the goals of Vision 2020 - the program launched by the World Health Organization (WHO) for the elimination of avoidable blindness.1 This is considered a priority because ″blind-years″ (number of years that a blind person lives after going blind) due to childhood blindness are second only to cataract and because half the blindness in children is avoidable (treatable/preventable).1-4
The prevalence of childhood blindness varies according to the socioeconomic development of the country and the mortality rate of those under five years of age.1,5 Four to five per cent of all blindness in the world is due to childhood blindness.6 Very few studies have been done in India to estimate the prevalence of childhood blindness but available evidence suggests that one out of every 1000 children is blind.7-9
India is home to 407 million children below the age of 16 years. This accounts for 40% of the Indian population.10 The needs of visually impaired children are different from adults both in terms of diagnosis and treatment.1 Therefore, there is a need to develop specific skills for providing eye care to children. The need relates both to the infrastructure and the available human resources. Pediatric ophthalmology is not yet well established as a separate subspecialty in India, though there are 200,000 blind children in India.11
Pediatric eye care needs synergy at all levels of eye care. Primary, secondary and tertiary levels need to rise to the challenge if avoidable blindness in children is to be eliminated. Developing a pediatric eye care team and augmenting their skills is essential. It has generally been stated that there are few trained or pediatric oriented ophthalmic personnel in the country.12 The present study was undertaken to document the status of pediatric eye care in India, so as to enable policy planners and program managers to address the problem of childhood blindness more effectively.
Materials and Methods
A study to document the available human resources and infrastructure for specialty eye care in India was conducted over an 18-month period in 2004-05. The study used a mix of approaches to triangulate and validate the data from different sources. A specially designed questionnaire schedule was developed and piloted at six institutions across the country - two Government, two Non-Governmental (NGO) and two private practitioners. A Technical advisory group constituted for the study and including representatives from the Government of India, ORBIS International and the three WHO collaborating centers for control of blindness in India (Aravind Eye Care System, L.V. Prasad Eye Institute and Dr. R.P. Centre for Ophthalmic Sciences) finalized the questionnaire schedule based on the feedback from the pilot survey.
A questionnaire on general eye care services was sent to all known eye care institutions in the country. Those which responded stating that they provided specialty services were then asked to provide more specific information relating to pediatric eye care. All questionnaires were administered in English.
The questionnaire was mailed to all known hospitals and clinics in the country. A list of addresses was first prepared with inputs from different sources, including the national program for control of blindness, state program officers, professional bodies of ophthalmologists, and national and international non- governmental organizations working in the field of eye care.
All questionnaires were sent by courier or by speed post to ensure that the maximal number of questionnaires could be delivered. Reminders were sent by post or telephone over a period of six months to maximize response.
In addition to the mailed questionnaires, the research team organized workshops and regional meetings to improve the response rate. Workshops were organized in Chandigarh, Jaipur, Chennai, Lucknow, Bangalore and Pune when the initial response was not adequate and a large number of institutions could be invited to a common location. These were organized to reinforce the importance of this study before the health authorities, and to motivate them to direct their officials to have these forms filled. A core group was constituted to collect information from the states in addition to the efforts made by the central data collection team. Information collected was validated by ensuring that randomly selected 10% of the responding institutions were visited by a team of dedicated eye care personnel. The observers were drawn from a number of leading eye care institutions in the country. Seventy-one institutions were visited. The information submitted by them was verified by the observers.
Only hospitals providing inpatient services were considered for analysis as it was felt that such facilities were necessary for pediatric eye care. All data was entered into a specially designed database developed in Microsoft Access. Analysis was done using Stata 9.0.
The following definitions were used in the study:
Secondary care hospital: District level/ Sub-district level hospitals where one or more ophthalmologists were available either fulltime or part-time. Services provided include refraction services, treatment and surgery for cataract. Examples of such hospitals were district hospitals, small NGO/private hospitals, community health centers (if an ophthalmologist was available), medical colleges teaching only undergraduate MBBS students with minimal ophthalmic services.
Tertiary care hospital: Hospitals at the regional/state/ zonal/district level where comprehensive eye services were provided. All diagnostic and surgical services were available so that they provided care to patients referred from the secondary level. Additional diagnostic support and surgical services for cataract, glaucoma, squint, ocular trauma etc., were available along with emergency services, but there were no fully developed specialty services. Examples include large NGO/ private hospitals, medical colleges with postgraduate ophthalmic courses (MD/MS/DNB/DO).
Advanced care hospitals: Large hospitals providing subspecialty eye services in addition to normal services offered at a tertiary care center, including low-vision services.
Teaching hospital: Hospitals/ Institutions which provided postgraduate fellowship training in ophthalmology.
Specialty trained ophthalmologists: Ophthalmologists who underwent at least six months fellowship or similar dedicated training in pediatric eye care.
Specialty oriented ophthalmologists: Ophthalmologists who underwent at least four weeks training at an institution with a pediatric ophthalmology unit.
Exclusive eye hospital: Hospitals providing only ophthalmology services.
Multidiscipline /General hospitals: Hospitals providing multispecialty services (general surgery, internal medicine, pediatrics, orthopedics, obstetrics, gynecology etc.) in addition to ophthalmology services.
Public-funded hospitals: Hospitals owned/funded by public funds and including Government, University, public sector (railways, employees state corporation, steel authority etc.), autonomous bodies under the Government and defense services etc.
NGO Hospitals: Hospitals of a charitable nature working on the principle of not-for-profit.
Private institutions: Hospitals providing eye care services on commercial terms, earning a profit from the services provided.
Results
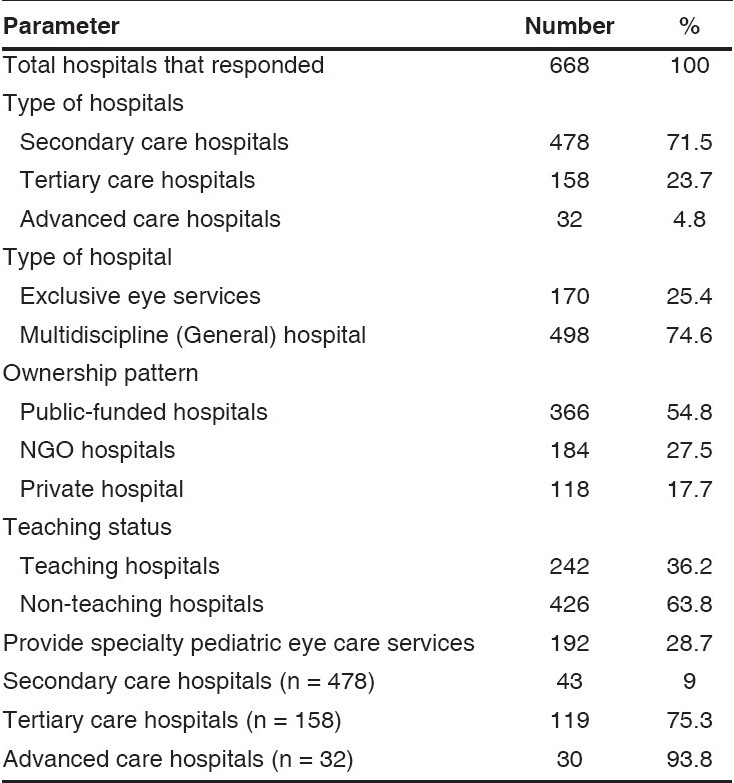
Out of a total of 1204 institutions, 668 (55.5%) responded to the questionnaire schedule across the country [Table 1]. The majority were secondary care institutions, providing multidiscipline health services. Among the 668 responding hospitals, 192 (28.7%) reported that they provided pediatric eye care services, and provided data in relation to such services. Almost all advanced care hospitals (93.8%) provided subspecialty pediatric ophthalmology services. Information on the pediatric load, services and surgical output was analyzed from the 192 hospitals providing this data.
Table 1.
Characteristics of responded institutions
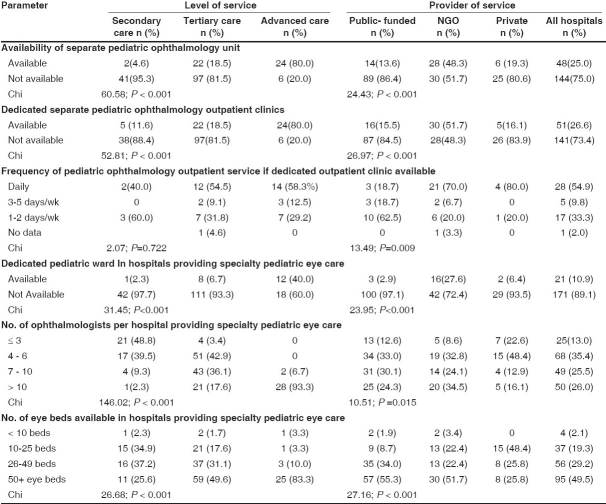
Among the 192 responding hospitals, a quarter reported that they had a separate pediatric ophthalmology unit to provide subspecialty services [Table 2]. A significantly larger number of advanced care hospitals reported a separate unit compared to secondary care institutions (X2 - 60.5880; p < 0.001). A significantly higher proportion of NGO hospitals reported separate pediatric ophthalmology units compared to the other providers (X2 - 24.4344; p < 0.001).
Table 2.
Profile of hospitals providing pediatric eye care services
Dedicated pediatric outpatient clinics were significantly more common in advanced care hospitals compared to secondary hospitals (X2 - 52.8110; p < 0.001) [Table 2]. These differences were also significant by provider of services with a higher proportion of NGO hospitals reporting the same (X2 - 29.9765; P < 0.001). The frequency of running the dedicated outpatient clinics did not vary by level of service. However, it was associated with the provider, with 75% of NGO hospitals reporting a daily clinic, as against lower frequencies by other providers (X2 - 24.1714; P < 0.01). Inpatient facilities for children were also significantly higher in advanced hospitals (X2 - 31.4560; P < 0.001), and among NGO hospitals (X2 - 23.9532; P < 0.001).
Perusal of beds per hospital also revealed that differences were significant by level of service (X2 -26.6819; P < 0.001) and by provider (X2 - 27.1692; P < 0.001), with advanced care hospitals having the highest bed per hospital rate.
Overall, the secondary and tertiary care hospitals catered to less pediatric clients on a working day, compared to advanced care hospitals. These differences were statistically significant (X2 - 27.8330; P < 0.001), when missing data was ignored [Table 3]. The differences were not significant by provider (X2 -3.1472; P=0.790). The morbidity profile was analyzed using the median new consultations for different conditions in a year. Refractive errors were the commonest condition for seeking attention at a hospital irrespective of the level of service and provider.
Table 3.
Outpatient service at hospitals providing pediatric ophthalmology services
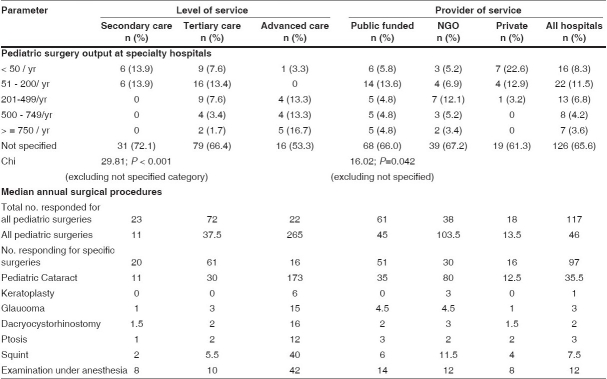
Overall, the advanced care setups performed more pediatric surgeries compared to secondary and tertiary care hospitals [Table 4]. These differences were statistically significant (X2- 29.8139; p < 0.001). Among providers, 9.6% of public-funded hospitals and 8.6% of NGO hospitals performed more than 500 pediatric surgeries a year. None of the private hospitals reported high-volume pediatric surgery and these differences were statistically significant (X2 -16.0298; p=0.042). Advanced care centers and NGO hospitals had a higher surgical output considering the median pediatric surgeries in a year. The commonest surgical procedure performed was pediatric cataract surgery followed by squint surgery. Keratoplasty was reported to be higher at NGO hospitals and advanced care centers. It was observed that the private sector was accessed quite often by clients for pediatric surgery, and their involvement in service delivery for children is important.
Table 4.
Surgical output at hospitals providing pediatric ophthalmology services
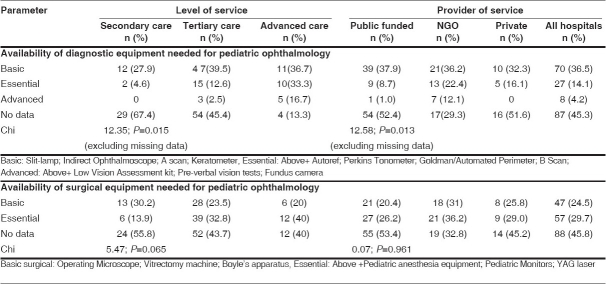
In identifying equipment required for pediatric ophthalmology, guidelines provided by WHO were considered.13 Equipment was categorized as basic, essential or advanced. A significant proportion of the secondary level, tertiary level, public-funded and private institutions did not provide complete data on equipment. It was not possible to grade the equipment available with these hospitals.
The availability of equipment is depicted in Table 5. Majority of the hospitals had access to only the basic pediatric diagnostic equipment. Differences by service level (X2-12.3537; p=0.015) and provider status (X2-12.5891; p=0.013) were however significant, excluding the non-responding hospitals. It was interesting to observe that access to pediatric surgical equipment was more ′egalitarian′, and differences by level of service (X-5.4740; p=0.065) or provider (X-0.0788; p=0.961) were not significant.
Table 5.
Equipment status at hospitals stating pediatric ophthalmology services
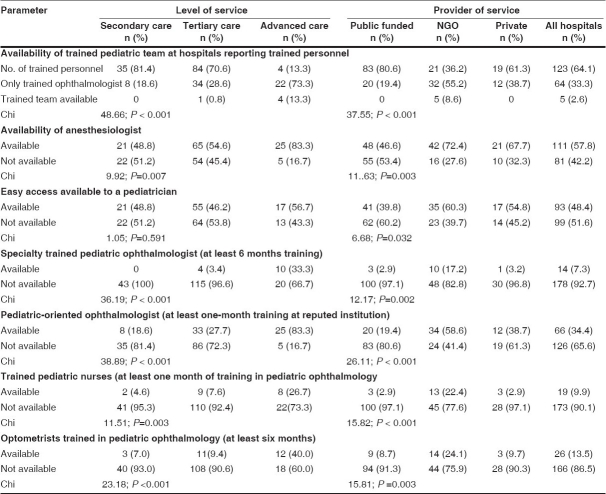
It was observed that available facilities in India afforded a training opportunity to ophthalmologists, but rarely to an entire pediatric team [Table 6]. A quarter of the advanced hospitals did not possess a pediatric specialty trained or oriented ophthalmologist, while 13.3% actually had the benefit of a fully trained team. The WHO has emphasized that a trained pediatric team encompassing skills of an ophthalmologist, optometrist, nurse and an anesthesiologist is needed for delivery of effective pediatric eye care.13
Table 6.
Status of human resources for pediatric ophthalmology
There were significant differences based on the level of service (X2-9.9283; p=0.007) as well as providers (X2 -11.6306; p=0.003) in the availability of an anesthesiologist [Table 6]. Advanced centers and NGO providers had better availability in this regard. Access to a pediatrician was similar across different hospitals. The differences by level of service were not significant (X2-1.0508; p=0.591), though it was statistically significant by providers of services (X2-6.6873; p=0.032). Significant differences were also observed both for the level of service as well as the provider of service in relation to specialty trained ophthalmologists, specialty oriented ophthalmologists, ophthalmic nurses and optometrists. Uniformly, advanced centers and NGO hospitals had access to trained human resources for pediatric ophthalmology.
Discussion
A child becomes bilaterally blind every minute, primarily within developing nations. Of the 1.5 million blind children in the world, 1.3 million live in Asia and Africa, and 75% of all causes are preventable or curable.5,14 It is estimated that 200,000 of these children are in India.11,12 The needs of these children need to be addressed so as to be able to achieve the goals of Vision 2020.
India is a country in transition, and needs to address preventable and treatable causes of childhood blindness at the same time. Studies among schools for the blind children in India observed pattern of causes of visual loss to be intermediate between those seen in industrialized countries and in the poorest developing countries of the world.15 Corneal causes, globe abnormalities, cataract and retinal causes have been highlighted as important causes in the Indian context.4,15-18 Recent studies in the country suggest that there is a declining trend in relation to corneal blindness.17,18 This would therefore mean that curative services will need to be augmented and appropriate skills provided to eye care professionals.
In many countries, a child with congenital glaucoma will be referred to a glaucoma specialist; congenital cataract will be managed by an anterior segment surgeon; ocular plastic problems by an oculo-plastic surgeon; squint patients will be seen by a strabismologist.19 Even where pediatric ophthalmology is offered as a subspecialty service, in countries like Germany, such services do not include cataract, glaucoma, orbital surgery, laser for retinopathy of prematurity (ROP) etc.20 Therefore, children will not be provided services from one source, but would need to go to different ophthalmologists or hospitals for treatment. This is not conducive to an efficient pediatric eye care program.
There has been no formal training for pediatric ophthalmology till recently, although pediatric ophthalmology departments are now being set up in tertiary care eye hospitals. However, strabismology has been recognized as a distinct subspecialty in India for decades and many tertiary eye hospitals established a strabismus department as early as 1960.12 Such departments do not cater only to children but provide services across all age groups. Only recently have institutions like Aravind Eye Care System, Sankara Netralaya and L.V. Prasad Eye Institute, which have been labeled as pediatric ophthalmology learning and training centers, have formalized fellowship programs in pediatric ophthalmology. More ophthalmologists are now opting for pediatric ophthalmology fellowship training.12
Not only in India, but in many countries, pediatric ophthalmology fellowships are of recent origin. In countries like Israel, Chile, Philippines , France, Italy, Japan and Sweden, along with many other countries, there is no formal fellowship program in pediatric ophthalmology.20,27 Even in countries where formal fellowship programs exist, they are of variable duration ranging from a couple of months to two years.28-33
Though pediatric ophthalmology is now developing as a distinct subspecialty in India, the clinical load may not warrant a situation in most hospitals of specialty ophthalmologists working only in pediatric ophthalmology. To attract ophthalmologists to take up pediatric ophthalmology, it would be necessary to allow them to also attend to ophthalmic problems in other age groups to generate adequate professionally satisfying workloads. In countries like Singapore, pediatric ophthalmologists also maintain their general practices.29 In fact many general ophthalmologists provide pediatric eye care services even without a formal training in many countries.21,23-28,30,33-35
Though a significant number of hospitals in the country have either specialty trained or oriented ophthalmologists, they are usually not supported by a trained pediatric team, as was observed in the present study. The subspecialty needs a team approach to be successful and identifying modalities of training a composite team of ophthalmologists, optometrists, nurses, anesthesiologist and counselors needs to be addressed. The WHO also strongly recommends the team approach.13
The present study was the first ever study in the Indian subcontinent to collect information on the status of pediatric eye care services. To gather information, the questionnaire used in this study ran into 17 pages, which was indeed a limitation. It would have required substantial time from the respondents, and could have been a reason for the response rate of 55.5%.
The WHO suggests that there should be one pediatric ophthalmology service center for every 10 million population, where at least one specialty trained or oriented ophthalmologist should be available.13 There were 69 such centers for a population of 1.1 billion, translating to 0.63 pediatric ophthalmology service units per 10 million population. Many of these hospitals do not have a full complement of diagnostic and surgical equipment, infrastructure and supportive human resources to provide vibrant pediatric ophthalmology services. The available centers are also not homogenously distributed across the country. Better ratios were observed in the southern and western part of India as against a complete lack of services in the North and East, where only a few centers were functional. Pediatric eye care services are inadequate in India and investment of time and money, and a professional and political commitment is required to support the establishment of need-based pediatric centers.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Gilbert CE, Foster A. Childhood blindness in the context of vision 2020: The right to sight. Bull WHO. 2001;79:227–32. [PMC free article] [PubMed] [Google Scholar]
- 2.Dandona L, Gilbert CE, Rahi JS, Rao GN. Planning to reduce childhood blindness in India. Indian J Ophthalmol. 1998;46:117–22. [PubMed] [Google Scholar]
- 3.Gilbert CE, Canovas R, Hagan M, Rao S, Foster A. Causes of childhood blindness: Results from West Africa, South India and Chile. Eye. 1993;7:184–8. doi: 10.1038/eye.1993.39. [DOI] [PubMed] [Google Scholar]
- 4.Hornby SJ, Adolph S, Gothwal VK, Gilbert CE, Dandona L, Foster A. Evaluation of children in six blind schools of Andhra Pradesh. Indian J Ophthalmol. 2000;48:195–200. [PubMed] [Google Scholar]
- 5.Wilson ME, Pandey SK, Thakur J. Pediatric cataract blindness in the developing world: Surgical techniques and intraocular lenses in the new millennium. Br J Ophthalmol. 2003;87:14–9. doi: 10.1136/bjo.87.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Resnikoff S, Pascolini D, Etyaale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull WHO. 2004;82:844–51. [PMC free article] [PubMed] [Google Scholar]
- 7.Dandona R, Dandona L. Childhood blindness in India: A population based perspective. Br J Ophthalmol. 2003;87:263–5. doi: 10.1136/bjo.87.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murthy GV, Gupta SK, Ellwein LB, Munoz SR, Pokharel GP, Sanga L, et al. Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci. 2002;43:623–31. [PubMed] [Google Scholar]
- 9.Dandona R, Dandona L, Srinivas M, Sahare P, Narsaiah S, Munoz SR, et al. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002;43:615–22. [PubMed] [Google Scholar]
- 10.Office of the Registrar General and Census Commissioner, India. Population projections for India and States 2001-2026 (Revised December 2006) New Delhi: Registrar General and Census Commission, Govt. of India; 2006. [Google Scholar]
- 11.Nirmalan PK, Sheeladevi S, Tamilselvi V, Victor AC, Vijayalakshmi P, Rahmathullah L. Perceptions of eye diseases and eye care needs among parents in rural South India: The Kariapatti Pediatric Eye Evaluation Project (KPEEP) Indian J Ophthalmol. 2004;52:163–7. [PubMed] [Google Scholar]
- 12.Vijaylakshmi P, Nirmalan P, Kothari MT. Pediatric ophthalmology and strabismus in India. J AAPOS. 2004;8:18–9. doi: 10.1016/j.jaapos.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. A five-year project for the prevention of childhood blindness: Report of a WHO Consultation. Geneva: WHO; 2002. WHO/PBL/ 02.88. [Google Scholar]
- 14.Steinkuller PG, Du L, Gilbert C, Foster A, Collins ML, Coats DK. Childhood blindness. J AAPOS. 1999;3:26–32. doi: 10.1016/s1091-8531(99)70091-1. [DOI] [PubMed] [Google Scholar]
- 15.Rahi JS, Sripathi S, Gilbert CE, Foster A. The importance of prenatal factors in childhood blindness in India. Dev Med Child Neurol. 1997;39:449–55. doi: 10.1111/j.1469-8749.1997.tb07464.x. [DOI] [PubMed] [Google Scholar]
- 16.Rahi JS, Sripathi S, Gilbert CE, Foster A. Childhood blindness in India: Causes in 1318 blind school students in nine states. Eye. 1995;9:545–50. doi: 10.1038/eye.1995.137. [DOI] [PubMed] [Google Scholar]
- 17.Gogate P, Deshpande M, Sudrik S, Taras S, Kishore H, Gilbert C. Changing pattern of childhood blindness in Maharashtra, India. Br J Ophthalmol. 2007;91:8–12. doi: 10.1136/bjo.2006.094433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Titiyal JS, Pal N, Murthy GV, Gupta SK, Tandon R, Vajpayee RB, et al. Causes and temporal trends of blindness and severe visual impairment in children in schools for the blind in North India. Br J Ophthalmol. 2003;87:941–5. doi: 10.1136/bjo.87.8.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alvarez MG. Pediatric ophthalmology and strabismus in Brazil. J AAPOS. 2005;9:205–6. doi: 10.1016/j.jaapos.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Lorenz B, Lenk-Schaefer M. Paediatric ophthalmology in Germany. J AAPOS. 2006;10:1–3. doi: 10.1016/j.jaapos.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 21.Spierer A. Paediatric ophthalmology in Israel. J AAPOS. 2003;7:231–2. doi: 10.1016/s1091-8531(03)00143-5. [DOI] [PubMed] [Google Scholar]
- 22.Katz X. Paediatric ophthalmology and strabismus in Chile. J AAPOS. 2004;8:121–2. doi: 10.1016/j.jaapos.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 23.Santiago Alvina PD. Paediatric ophthalmology in the Philippines. J AAPOS. 2005;9:103–5. doi: 10.1016/j.jaapos.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 24.Speilmann AC. Pediatric ophthalmology and strabismus in France. J AAPOS. 2003;7:156–7. doi: 10.1016/s1091-8531(03)00059-4. [DOI] [PubMed] [Google Scholar]
- 25.Nucci P. Pediatric ophthalmology and strabismus in Italy. J AAPOS. 2004;8:220–1. doi: 10.1016/j.jaapos.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 26.Sato M, Watanabe Y. Current status of pediatric ophthalmology and strabismus in Japan. J AAPOS. 2004;8:297–8. doi: 10.1016/j.jaapos.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 27.Stromland K. Pediatric ophthalmology and strabismus in Sweden. J AAPOS. 2003;7:374–5. doi: 10.1016/s1091-8531(03)00172-1. [DOI] [PubMed] [Google Scholar]
- 28.Ramirez Ortis MA. Paediatric ophthalmology and strabismus in Mexico. J AAPOS. 2005;9:303–5. doi: 10.1016/j.jaapos.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 29.Ling Y. Paediatric ophthalmology in Singapore. J AAPOS. 2007;11:3–4. doi: 10.1016/j.jaapos.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 30.Filous A. Pediatric ophthalmology in the Czech Republic. J AAPOS. 2005;9:1–2. doi: 10.1016/j.jaapos.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 31.Eltoukhi EL. The development of pediatric ophthalmology and strabismus in Egypt. J AAPOS. 2003;7:309–10. doi: 10.1016/s1091-8531(03)00171-x. [DOI] [PubMed] [Google Scholar]
- 32.Khan AO, Al-MesferS Pediatric ophthalmology and strabismus in the Kingdom of Saudi Arabia. J AAPOS. 2004;8:513–4. doi: 10.1016/j.jaapos.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 33.Murray AD. Pediatric ophthalmology in South Africa. J AAPOS. 2005;9:404–5. doi: 10.1016/j.jaapos.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 34.O′Keefe M. Paediatric ophthalmology in Ireland. J AAPOS. 2004;8:407–8. doi: 10.1016/S1091853104000151. [DOI] [PubMed] [Google Scholar]
- 35.Kowal L. Pediatric ophthalmology in Australia. J AAPOS. 2003;7:311–3. doi: 10.1016/s1091-8531(03)00184-8. [DOI] [PubMed] [Google Scholar]