Abstract
The aim of the study was to assess agreement between two commercially available applanation tonometers for the measurement of intraocular pressure (IOP). Forty subjects underwent IOP measurement on two accurately calibrated Goldmann type applanation tonometers (Zeiss AT 030 (GATZ) and Inami L-5110(GATI)). The order of examination was randomized and observers were masked to the IOP recorded. The mean of two consecutive readings, from a randomly selected eye for each subject, was used for analysis. Agreement was assessed using the Altman and Bland plot. The mean (SD) IOP readings on GATZ was 15.32 (±6.80) mm Hg and on GATI was 13.52 (±5.65) mm Hg (p<0.001, 95% CI of the difference: -2.48 to -1.11). The 95% limits of agreement on the Altman and Bland plot were:-2.47 to 6.16 mm Hg). There was significant inter-instrument variability between the two accurately calibrated Goldmann type applanation tonometers studied.
Keywords: Agreement, Goldmann applanation tonometer, intraocular pressure
Intraocular pressure (IOP) measurements are essential in the diagnosis and follow-up of glaucoma. While there are a number of methods for measuring IOP, applanation tonometry is probably the most widely used technique and is considered the current gold standard for IOP measurement. Goldmann type applanation tonometers made by different manufacturers are available commercially.
Studies on factors affecting IOP measurements such as central corneal thickness and keratometric readings have focused on the subject-related parameters.1 However, while there are reports comparing different instruments used for measuring IOP, a literature search did not show any published work on agreement on IOP measurements between different Goldmann type applanation tonometers.2-5 The literature search was performed in the Medline database using the key words Goldmann applanation tonometry with the Boolean operand ″AND″, and the terms agreement and comparison independently. When this did not yield any articles that met the criteria all abstracts with the key words ″Goldmann applanation tonometry″ were reviewed.
Once the instruments are calibrated as per the manufacturer′s instructions we assume that the readings between devices are comparable. A significant difference in IOP measurement between instruments has diagnostic and therapeutic implications. We studied agreement in IOP measurements using two commercially available Goldmann type applanation tonometers.
Materials and Methods
Sample size was calculated to measure a difference of greater than 2 mm of Hg between the two instruments with an estimated standard deviation of 4 mm, for 80% power and a Type 1 error of 5%. We needed 34 patients to measure this difference and recruited 40 consecutive adult subjects attending a glaucoma prevalence study for the trial.
All subjects who could undergo visual acuity measurement, refraction, slit-lamp examination and applanation tension measurement were eligible. Corneal pathology including astigmatism of 2 diopter (D) or greater, inability to measure IOP or history of allergy to proparacaine or fluorescein were reasons for exclusion. An informed consent was obtained from all participants prior to enrollment.
Intraocular pressure was measured by one of two examiners, using the Zeiss AT 030 (GATZ) (Carl Zeiss, Jena, Germany) and the InamiL-5110 (GATI) (Inami and Co., Tokyo, Japan) Goldmann type applanation tonometers.
At the start of the day the instruments were calibrated as per the manufacturer′s instructions and were used for examination only if they were accurately calibrated.
To minimize the influence of any IOP-lowering effect induced by applanation tonometry on the results, the sequence of measurements was randomized. Applanation tonometry was performed first on one randomly selected instrument followed immediately after by measurement on the second instrument. The IOP was measured after anesthetizing the cornea with sterile 0.5% proparacain eye drops (Paracain, Sunways, Mumbai, India) and staining the tear film with fluorescein strips. The tonometer was set to the zero mark prior to the start of the examination. Measurements on both instruments for a subject were performed by a single observer who was blinded to the actual readings, which were read and recorded by the second examiner who then reset the applanation tonometer to the zero mark. The IOP was measured two consecutive times for each eye on each instrument, and the mean of the two readings was used for analysis; if there was a difference of greater than 2 mm of Hg between the readings, a third measurement was taken and the median of three readings was taken. By convention, the right eye was examined first for every patient. The IOP was measured on the second instrument, placed in the same examination room, almost immediately after completing recording on the first instrument.
Measurements from one eye were randomly selected for analysis. Intraocular pressure was compared using the paired ′t′ test and agreement was assessed by the Altman and Bland plot.6
Results
Forty eyes (40 subjects, mean age: 53.3 SD ± 7.9 years, 22 males, 18 females) were included. Mean IOP (SD) on GATZ was 15.32 (±6.80) mm Hg (Range:9 mm Hg - 36 mm Hg) and on GATI 13.52 (±5.65) mm Hg (Range:7mm Hg - 30mm Hg) (p<0.001, 95% CI of the difference: -2.48 to -1.11). The coefficient of correlation for the two instruments was 0.95 (p=0.001). The Bland and Altman plot [Figure 1] revealed a tendency for higher IOP recordings on the GATZ (95% limits of agreement:-2.47 to 6.16 mm Hg).
Figure 1.
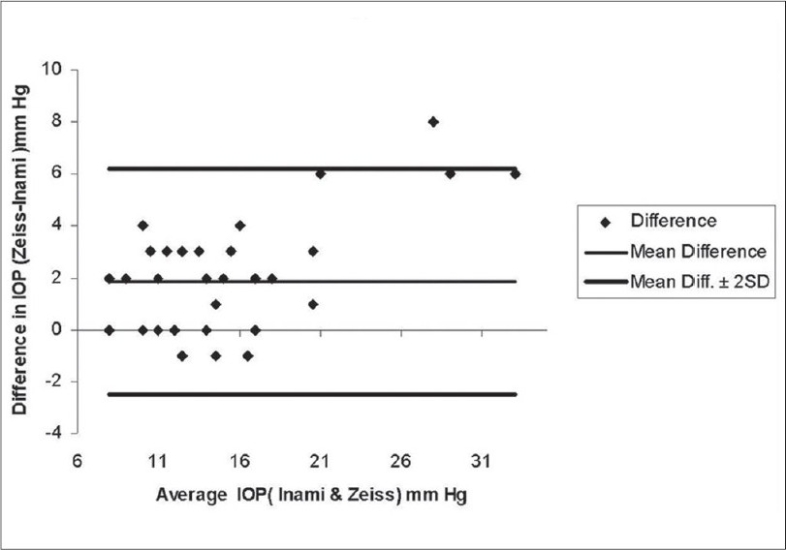
Altman and Bland plot displaying the difference in IOP measurements plotted against the mean IOP measurements
Discussion
Intraocular pressure readings are essential in the diagnosis and management of glaucoma. The absolute level of IOP may not be as important to glaucoma diagnosis as was once thought, however, the trend of IOP measurements is relevant in the management of glaucoma patients.
There are various factors that could affect IOP measurements. We attempted to minimize their influence on the study results. In order to avoid an observer bias, two observers were used for the study - however, the same observer made IOP measurements on both instruments for a single patient. To minimize the effect of a possible transient lowering of IOP following applanation tonometry, on the results, we randomly allocated the order of IOP measurement by either machine. The IOPs on the second instrument were measured within a few minutes of the measurement on the first machine to minimize any temporal variation in IOP.
The significant variation in IOP recordings between both instruments is surprising. Lower IOP readings were consistently recorded on the Inami AT. In 70% of subjects IOP differences were within the clinically acceptable range of 2 mm. With both instruments calibrated accurately as per the manufacturer′s recommendations better agreement between the instruments would be expected. Since manometric measurements were not made in any of our subjects it is difficult to comment on which instrument was giving erroneous results.
The clinical implications of this variation on disease diagnosis are considerable since both instruments are widely used in Asia. It could result in potential misdiagnosis of normal tension glaucoma (NTG) or primary open angle glaucoma (POAG). Follow-up may not be affected as significantly as long as all measurements are made on a single instrument by a single observer keeping other factors such as calibration and the time of measurement constant. However, with increasing cross-referrals and the use of multiple instruments in various clinics the possibility of lack of agreement between devices has to be kept in mind. Therapeutic and surgical decisions can be significantly affected by this lack of agreement.
We have compared applanation readings between only two instruments. With the large number of similar applanation tonometers available, agreement between other commercially available devices needs to be assessed. In this study all devices were calibrated correctly as per the manufacturer′s instructions. If this was indeed the case there should not have been a significant difference between devices and certainly not a difference of the magnitude that was found. Perhaps, the manufacturers need to reassess the calibration procedures for these devices.
In conclusion, we demonstrate yet another variable in IOP measurements, the effect of which could be minimized by performing baseline and follow-up IOP measurements on a single instrument. Additionally, therapeutic decisions should be made keeping in mind the possibility of an inter-instrument variability.
References
- 1.Whitacre MM, Stein R. Sources of error with use of Goldmann-type tonometers. Surv Ophthalmol. 1993;38:1–30. doi: 10.1016/0039-6257(93)90053-a. [DOI] [PubMed] [Google Scholar]
- 2.Morledge-Hampton SJ, Kwon RO, Krishna R, Debry PW, Willoughby TL. Comparison of proview phosphene tonometry with Goldmann applanation tonometry. Can J Ophthalmol. 2006;41:722–6. doi: 10.3129/i06-065. [DOI] [PubMed] [Google Scholar]
- 3.Herdener S, Hafizovic D, Pache M, Lautebach S, Funk J. Dynamic contour tonometry (DCT) versus Goldmann applanation tonometry (GAT): A comparison of agreement and reproducibility. Graefes Arch Clin Exp Ophthalmol. 2007;245:1027–30. doi: 10.1007/s00417-006-0449-5. [DOI] [PubMed] [Google Scholar]
- 4.Abraham LM, Epasinghe NC, Selva D, Casson R. Comparison of the ICare (R) rebound tonometer with the Goldmann applanation tonometer by experienced and inexperienced tonometrists. Eye. 2008;22:503–6. doi: 10.1038/sj.eye.6702669. [DOI] [PubMed] [Google Scholar]
- 5.Gupta V, Sony P, Agarwal HC, Sihota R, Sharma A. Inter- instrument agreement and influence of central corneal thickness on measurements with Goldmann, pneumotonometer and noncontact tonometer in glaucomatous eyes. Indian J Ophthalmol. 2006;54:261–5. doi: 10.4103/0301-4738.27952. [DOI] [PubMed] [Google Scholar]
- 6.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]


