Abstract
Background
Associations between major depressive disorder (MDD) and psychosocial functioning are incompletely understood across time and during continuation phase cognitive therapy (C-CT). We examined the validity of the Range of Impaired Functioning Tool (RIFT; Leon et al., 1999) as a measure of psychosocial functioning and its relations to depressive symptoms in C-CT and assessment-only control conditions.
Methods
Outpatients with recurrent MDD who responded to acute-phase cognitive therapy (A-CT) were randomized to 8 months of C-CT (n = 41) or assessment only (n = 43) and followed 16 additional months (Jarrett et al., 2001). Interviewers rated depressive symptoms and psychosocial functioning monthly. Patients completed additional self-reports.
Results
The RIFT converged appropriately with other measures of psychosocial functioning, depressive symptoms, cognitive content, and personality. About half (55%) of patients were psychosocially “well” (RIFT ≤ 8) during the first month post-A-CT. C-CT improved psychosocial functioning only transiently compared to the assessment control. Examined prospectively, depressive symptom level did not predict monthly changes in psychosocial functioning significantly, whereas psychosocial dysfunction level predicted monthly changes in depressive symptoms and relapse/recurrence.
Limitations
Findings may not generalize to other patient populations, treatments, and assessment methods. The cross-lagged correlational data structure allows only tentative conclusions about the causal effect of psychosocial functioning on depressive symptoms.
Conclusions
The RIFT is a valid measure of psychosocial functioning among responders to A-CT for depression. After such response, deteriorations in psychosocial functioning may signal imminent major depressive relapse/recurrence and provide targets for change during treatments focused on relapse/recurrence prevention.
Keywords: psychosocial functioning, depression, cognitive therapy, relapse, recurrence
Introduction
Consequences of major depressive disorder (MDD) exceed personal distress to include significant psychosocial dysfunction in domains such as work, family and social relationships, and leisure activities (Leader and Klein, 1996; Weissman et al., 1978). Unfortunately temporal and causal relations between depression and psychosocial functioning are incompletely understood. Psychosocial functioning improves during effective treatments for MDD such as acute-phase pharmacotherapy and cognitive therapy (A-CT; Hirschfeld et al., 2002; Papakostas et al., 2004). However, many responders to acute phase treatments maintain significant psychosocial dysfunction (Kennedy et al., 2007).
Poorer psychosocial functioning predicts major depressive relapse/recurrence (Leon et al., 1999; Rodriguez et al., 2005), and about half of responders to A-CT relapse/recur within two years (Vittengl et al., 2007) underscoring the importance of developing continuation treatments to reduce relapse/recurrence. Continuation CT (C-CT) reduces major depressive relapse/recurrence substantially (Vittengl et al., 2007), but associations between psychosocial functioning and depressive symptoms during this treatment are unknown. The current analyses examine associations of psychosocial functioning with depressive relapse/recurrence in the context of a randomized trial of C-CT versus assessment-only control (Jarrett et al., 2001).
Development of practical, valid measures of psychosocial functioning for follow-up evaluations facilitates research testing relations of functioning with depressive symptoms and relapse. Leon et al. (1999) derived the brief Range of Impaired Functioning Tool (RIFT) from the items on the Longitudinal Interval Follow-up Evaluation (LIFE; Keller et al., 1987) clinical interview. Correlations with depressive symptoms, global assessment of functioning (GAF) scores, and prediction of relapse and recovery 6–12 months later (Leon et al., 1999; Solomon et al., 2004) support the RIFT’s validity in patients with MDD. The current analyses expand validity data for the RIFT in patients with recurrent MDD through correlations with previously established measures of psychosocial functioning, depressive cognitive content, and personality.
Patients in the current analyses responded to A-CT, were assigned randomly to either 8 months of C-CT or assessment control, and completed 16 additional months of follow-up. We measured depression (with the LIFE) and psychosocial functioning (with the RIFT) monthly post-A-CT. First, we hypothesized that the RIFT converges appropriately with other measures of psychosocial functioning, depressive cognitive content, and personality. Second, we expected that higher depressive symptoms and poorer psychosocial functioning correlate concurrently. Finally, we tested whether current psychosocial functioning predicts later depression, or vice versa, and the effect of C-CT on this risk, but we did not make directional hypotheses.
Method
Participants
Jarrett et al. (2001) detailed patient recruitment, inclusion, and exclusion. Participants were adult outpatients meeting criteria for DSM-IV nonpsychotic, recurrent MDD with clear inter-episode recovery (≥ 2 months of at least nearly normal functioning; American Psychiatric Association, 1994) and scoring ≥ 16 on the 17-item Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960). Eligible patients consenting to A-CT (N = 156) had a mean age of 41.2 years (SD = 11.0) and level of education of 15.4 years (SD = 2.8); 74.4% were women; and 7.7% were African American, 4.5% Hispanic, 1.3% Native American, and 86.5% Caucasian.
Procedure
Jarrett et al. (2001) described study phases in detail. Patients received 20 individual sessions of A-CT (Beck et al., l979) from five experienced therapists in a 12–14 week protocol. The goal of A-CT is to teach patients to reduce depressive symptoms by identifying thoughts connected with negative affect, testing the validity of the thoughts using logical and empirical methods, generating alternatives when data do not support the negative thoughts’ validity, and problem-solving when they do. Consenting responders (no MDD and HRSD ≤ 9) to A-CT were randomized to C-CT (Jarrett, 1989; Jarrett et al., 2008; n = 41) or an assessment-only control condition (n = 43). The C-CT protocol consisted of 10 sessions (60–90 minutes each) over 8 months provided by the patient’s A-CT therapist. The goal of C-CT is to prevent major depressive relapse/recurrence by reducing residual symptoms of depression, improving skills learned in A-CT, enhancing behavioral and cognitive strengths, and improving coping with adversity in part by decreasing the probability of stressful events and anticipating risks for relapse/recurrence. Patients in the assessment-only condition attended 10 evaluation visits on the same schedule as C-CT patients. Jarrett et al. (2001) reported relapse rates of 31% (control) versus 10% (C-CT) during the experimental phase. All randomized patients were eligible and 74 entered the follow-up phase consisting of 10 assessments scheduled over 16 months (ending 24 months post A-CT). Pharmacotherapy was not provided during any study phase. Patient fatigue and attrition produced some missing data in study measures.
Measures
LIFE
The LIFE (Keller et al., 1987) assesses depressive symptoms and psychosocial functioning retrospectively. Experienced independent evaluators conducted this semi-structured interview at 4, 8, 12, 16, 20, and 24 months post-A-CT, at study exit, and when patients, therapists, or follow-up evaluators suspected major depressive relapse/recurrence. Weekly psychiatric status ratings (PSR) of DSM-IV MDD (on a 1–6 scale) were used to define relapse/recurrence events as ≥ 2 weeks of meeting diagnostic criteria (scores ≥ 5). Weekly PSRs were averaged to form monthly estimates of depressive symptoms for comparison with other measures, and evaluators provided monthly GAF estimates on a 0–100 scale (American Psychiatric Association, 1994). Psychosocial functioning also was scored monthly using the RIFT (Leon et al., 1999). The RIFT measures functioning at work (employment, household activities, school) and in interpersonal relationships (spouse, children, other relatives, friends), overall satisfaction with functioning, and fulfillment in recreational activities. Items are rated 1 (no impairment) to 5 (severe impairment), and the item score for functioning at work and in relationships is the highest level of dysfunction among sampled domains. The total RIFT score is the sum of the 4 items, and higher scores reflect greater dysfunction. In the current sample, alpha internal consistency was high for the monthly depressive symptom composite (Mdn = .97, range .86–.99) and moderate for the RIFT (Mdn = .74, range .68–.83).
Attributional Style Questionnaire (ASQ)
On the ASQ (Peterson et al., 1982), patients generate causes for negative and positive hypothetical situations and rate the extent to which causes reflects internal, global, and stable factors. Ratings for negative and positive situations are averaged (18 items each) to form failure (ASQ-F) and success (ASQ-S) composites (Peterson and Seligman, 1984). Correlations with self-report measures of depressive symptoms and self-concept support the validity of the ASQ (Tennen et al., 1987). The current report uses 18 assessments from 1–24 months post-A-CT; alpha internal consistency was high (ASQ-F Mdn = .87, range = .84–.90; ASQ-S Mdn = .87, range = .83–.89).
Dysfunctional Attitudes Scale (DAS)
The DAS (Form A; Weissman, 1979) measures attitudes hypothesized to relate to depression with 40 self-report items. In past research, the DAS’s validity has been demonstrated by correlations with both measures of depressive symptoms and of negative cognitive content (e.g., Dobson and Breiter, 1983; Haeffel et al., 2005; Ilardi and Craighead, 1999). The current report uses 18 assessments from 1–24 months post-A-CT; alpha internal consistency was very high (Mdn = .95, range .94–.96).
Self-Efficacy Scale (SEF)
The SEF (Sherer et al., 1982) consists of 23 self-report items measuring expected persistence and success in several domains. Correlations with self-esteem (Lansford et al., 2005) and interpersonal competency (Sherer et al., 1982) support the SEF’s validity. The current report uses 3 assessments (randomization, 8 and 24 months post-A-CT); alpha internal consistency for the total score was high (.92 at each assessment).
Social Adjustment Scale—Self Report (SAS-SR)
The SAS-SR (Weissman and Bothwell, 1976) measures functioning in important social domains with 56 self-report items. Patients complete sections reflecting their social roles (e.g., some omit marital and parenting). Higher values reflect poorer adjustment. In support of its validity, the SAS-SR has correlated with clinical ratings and been sensitive to change in psychopathology (Weissman and Bothwell, 1976; Weissmann et al., 1978). The current report uses 18 assessments from 1–24 months post-A-CT; alpha internal consistency for the total score was high (Mdn = .83, range = .79–.90).
Inventory of Interpersonal Problems (IIP)
The IIP (Horowitz et al., 1988) includes 127 self-report items to measure the extent to which particular behaviors, thoughts, and feelings have caused problems in personal relationships. Higher values indicate greater problems. Horowitz et al. (1988) reported moderate correlations with psychiatric symptoms, and decreases in IIP scores with psychotherapy. The current report makes use of 18 assessments from 1–24 months post-ACT; alpha internal consistency for the total score was very high (Mdn = .98, range = .98–.99).
Dyadic Adjustment Scale (DYS)
The DYS (Spanier, 1976) measures positive adjustment and satisfaction in marital and similarly committed dyads with 32 self-report items. Higher total scores represent better overall relationship quality. Spanier (1976) reported evidence supporting both content and criterion-related validity. The current report makes use of 18 assessments from 1–24 months post-A-CT; alpha internal consistency for the total score was very high (Mdn = .96, range = .95–.98).
Schedule for Nonadaptive and Adaptive Personality (SNAP)
The SNAP (Clark, 1993) assesses 15 dimensions of personality functioning relevant to personality disorder with 375 true-false self-report items. Studies support the scales’ validity in relation to interview measures of personality disorder (Clark, 1993; Clark et al., in press) and many external variables, including psychosocial functioning (Morey et al., 2007). We analyzed the three temperament dimensions (positive and negative temperament, disinhibition) reflecting the higher order factor structure of the instrument, plus scales showing relations to depression (detachment, dependency, mistrust, self-harm; Clark et al., 2003) and social-interpersonal relevance (aggression, manipulativeness). The current report uses 3 assessments (randomization, 8 and 24 months post-A-CT); alpha internal consistency for selected scales was moderate to very high (Mdn = .82, range .66–.93).
Results
Validity of RIFT Psychosocial Functioning Scores in Recurrent Major Depressive Disorder
We tested the concurrent validity of RIFT scores for patients with recurrent depression who responded to A-CT through correlations with other measures of psychosocial functioning, depressive cognitive content, selected personality trait dimensions, and depressive symptoms. Because data were collected longitudinally, we were able to estimate both between- and within-patient (predictors centered within patients) correlations using multilevel models. Between-patient correlations help answer such questions as, “Do patients with higher depressive symptoms have higher RIFT scores than patients with lower depressive symptoms?” Within-patient correlations help answer such questions as, “Will a patient’s increase in detachment parallel an increase in that patient’s RIFT score?”
In support of the convergent validity of the RIFT, poorer psychosocial functioning on the GAF, SAS-SR, IIP, and DYS predicted higher RIFT scores both between and within patients (see Table 1). With the exception of moderate negative correlations with the SEF, relations between RIFT scores and depressive cognitive content were weaker, although statistically significant for the ASQ-F (between patients only) and the DAS (between and within patients). Among the selected personality-trait scales, higher negative temperament and associated dimensions (dependency and self-harm), as well lower positive temperament and an associated dimension (higher detachment), predicted higher RIFT scores both between and within patients, with the exception of a non-significant between-patients correlation for dependency. However, RIFT scores did not relate significantly to mistrust, manipulativeness, aggression, or disinhibition (ps > .05). Finally, higher depressive symptoms (monthly average LIFE-PSR scores) predicted higher RIFT scores both between and within patients.
Table 1.
Validity Estimates of Range of Impaired Functioning (RIFT) Scores
| Between Patients | Within Patients | |||||
|---|---|---|---|---|---|---|
| Predictor of RIFT | k | n | Beta (SE) | r | Beta (SE) | r |
| Measures of Psychosocial Functioning | ||||||
| Global Assessment of Functioning | 24 | 78 | −0.271* (0.016) | −.65 | −0.177* (0.006) | −.36 |
| Social Adjustment Scale-SR | 18 | 78 | 6.172* (0.553) | .59 | 1.708* (0.230) | .11 |
| Inventory Interpersonal Problems | 18 | 78 | 1.806* (0.437) | .29 | 0.989* (0.252) | .07 |
| Dyadic Adjustment Scale | 18 | 51 | −0.061* (0.011) | −.46 | −0.043* (0.007) | −.14 |
| Measures of Depressive Cognitive Content | ||||||
| ASQ-Failure Composite | 18 | 78 | 0.863* (0.280) | .22 | 0.092 (0.103) | .01 |
| ASQ-Success Composite | 18 | 78 | −0.458 (0.305) | −.11 | −0.206 (0.106) | −.03 |
| Dysfuctional Attitudes Scale | 18 | 78 | 0.026* (0.007) | .26 | 0.012* (0.003) | .06 |
| Self-Efficacy Scale | 3 | 77 | −0.071* (0.019) | −.33 | −0.114* (0.029) | −.18 |
| Selected Scales from the Schedule for Nonadaptive and Adaptive Personality | ||||||
| Negative Temperament | 3 | 76 | 0.116* (0.043) | .26 | 0.175* (0.046) | .18 |
| Dependency | 3 | 76 | 0.178 (0.094) | .19 | 0.233* (0.107) | .10 |
| Self-harm | 3 | 76 | 0.341* (0.116) | .28 | 0.335* (0.101) | .16 |
| Positive Temperament | 3 | 76 | −0.214* (0.051) | −.38 | −0.210* (0.059) | −.17 |
| Detachment | 3 | 76 | 0.237* (0.080) | .28 | 0.210* (0.101) | .10 |
| Measure of Depressive Symptoms | ||||||
| Psychiatric Status Rating | 24 | 78 | 2.612* (0.271) | .53 | 0.804* (0.053) | .22 |
Note. k = number of assessments covering 24 months post-acute phase cognitive therapy. n = number of patients. SR = self-report. ASQ = Attributional Style Questionnaire.
p < .05.
Level of Psychosocial Functioning After A-CT
During the first month of the experimental phase, the average RIFT score among responders to A-CT (M = 8.68, SD = 2.92) was slightly outside the “well” range (≤ 8) suggested by Judd et al. (2005). About half (55%; SE = 6%) of the A-CT responders could be classified as well during the first month of the experimental phase.
We tested the effect of C-CT versus assessment control on RIFT scores during the 8-month experimental phase. In a multilevel model, the main effects of treatment group, F(1,76) = 0.71, p = .40, and assessment month, F(7,512) = 0.79, p = .60, were not significant, but the interaction of treatment group and assessment month was significant, F(7,512) = 2.48, p = .02. A parallel model computed over the full 24 months of follow-up yielded no significant effects of treatment group, F(1,76) = 0.71, p = .40, assessment month, F(23,1557) = 0.99, p = .48, or their interaction, F(1,1557) = 1.19, p = .24. Examination of least-squares estimated means revealed that the C-CT group (M = 8.21, SE = 0.49) had significantly lower (less impaired) RIFT scores (p < .05) than the assessment-only group (M = 9.64, SE = 0.50) only at month 6 (about 0.5 SD difference between groups). Averaged over 24 months, estimated RIFT scores for the C-CT and assessment-only control groups were 8.52 (SE = 0.33) and 8.91 (SE = 0.33), respectively (about 0.1 SD difference between groups), and the estimated proportions of psychosocially well patients (RIFT ≤ 8) each month were 55% (SE = 5%) and 48% (SE = 5%), respectively.
RIFT scores varied more substantially between patients who did and did not experience a major depressive relapse/recurrence at some point over the 24 months post-A-CT. In a multilevel model, the main effect of relapse/recurrence status was significant, F(1,76) = 25.91, p < .01, whereas neither the main effect of month, F(23,1557) = 1.07, p = .37, nor its interaction with relapse/recurrence status, F(23,1557) = 1.23, p = .21, were significant. Averaging over the 24 months of assessment, estimated RIFT scores for the groups with and without relapse/recurrence were 10.01 (SE = 0.33) and 7.80 (SE = 0.28), respectively (about 0.8 SD difference between groups), and the estimated proportions of psychosocially “well” patients (RIFT ≤ 8) were 35% (SE = 5%) and 63% (SE = 4%), respectively.
Temporal Relations Between Psychosocial Functioning and Depression
We computed cross-lagged multilevel models to test possible causal relations between psychosocial functioning and depressive symptoms. Table 2 shows results from the 24-month experimental plus follow-up phases (results for the 8-month experimental phase were similar and are not shown). Not surprisingly, monthly psychosocial functioning (RIFT) and depressive symptoms (PSR) were predicted by patients’ average scores on these measures over the time period studied. After accounting for the prior month’s psychosocial functioning, prior depressive symptoms did not predict current psychosocial functioning. In contrast, after accounting for the prior month’s depressive symptoms, prior psychosocial functioning predicted current depressive symptoms. In other words, patients with greater psychosocial dysfunction in a given month experience greater depressive symptoms during the next month. This pattern of results is consistent with psychosocial dysfunction influencing later depressive symptoms. Treatment group assignment did not moderate these effects significantly.
Table 2.
Prediction of Monthly Depressive Symptoms and Psychosocial Functioning
| Outcome: Psychosocial Functioning | Outcome: Depressive Symptoms | |||
|---|---|---|---|---|
| Predictor | Beta (SE) | r | Beta (SE) | r |
| Between Patients Effects | ||||
| Mean Psychosocial Dysfunction | 0.999* (0.024) | .78 | 0.003 (0.013) | .01 |
| Mean Depressive Symptoms | 0.040 (0.093) | .01 | 1.020* (0.052) | .59 |
| Treatment Group | −0.005 (0.087) | .00 | −0.004 (0.048) | .00 |
| Within Patients Effects | ||||
| Prior Month Psychosocial Dysfunction | 0.568* (0.023) | .35 | 0.075* (0.011) | .13 |
| Prior Month Depressive Symptoms | −0.026 (0.051) | −.01 | 0.363* (0.024) | .29 |
| Group X Prior Depressive Symptoms | 0.059 (0.092) | .01 | ||
| Group X Prior Psychosocial Dysfunction | −0.022 (0.020) | −.02 | ||
Note. N = 78 participants measured monthly for 24 months. Psychosocial functioning was measured with the Range of Impaired Functioning Tool and depressive symptoms were Psychiatric Status Ratings from the Longitudinal Interval Follow-up Evaluation.
Treatment Group coded CCT = +0.5, control = −0.5. --- = not included in model.
p < .05, two-tailed.
Parallel to the multilevel model using continuous PSR scores, we computed a time-lagged Cox regression model predicting time-to-relapse/recurrence. For the 24-month experimental plus follow-up phases, depressive symptoms in the month before the event (relapse/recurrence or study exit; beta = 0.491, SE = 0.209, p = .02) and RIFT scores in the month before the event (beta = 0.258, SE = 0.068, p < .01) predicted relapse/recurrence, but effects of treatment group (beta = −0.486, SE = 1.382, p = .73) and the interaction of prior-month RIFT scores and treatment group (beta = 0.041, SE = 0.118, p = .73) were not significant. The hazard ratio for psychosocial functioning (1.29) indicated that, for each 1-point increase on the RIFT, the odds of relapse/recurrence during the next month increased by 29%.
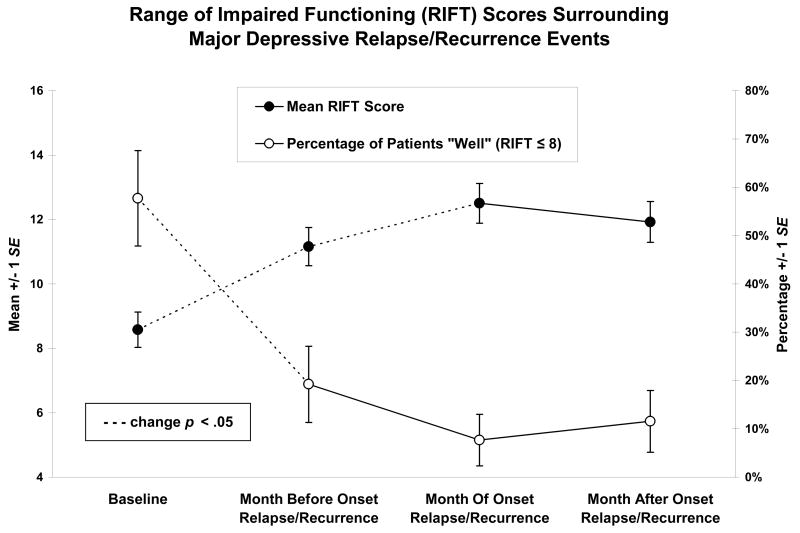
To illustrate, we identified those patients (n = 26) who relapsed/recurred between months 3-23 and had RIFT scores available at baseline (month 1 post-A-CT) and for the months before, during, and after the onset of the relapse/recurrence. As shown in Figure 1, from baseline to the month before relapse/recurrence, the average RIFT score increased significantly (about 2.6 RIFT points or 0.9 SD; t(25) = −3.97, p < .01), and the percentage of patients scoring in the “well” range (RIFT ≤ 8) decreased significantly (from 58% to 19%; McNemar χ2(1) = 10.00, p < .01).
Figure 1.
Discussion
Psychosocial Dysfunction after A-CT
Because half of A-CT responders relapse within 2 years without continuation treatment (Vittengl et al., 2007), and psychosocial dysfunction is a risk factor for relapse/recurrence (Leon et al., 1999; Solomon et al., 2004), better understanding of the nature of psychosocial dysfunction in this population may facilitate improvement of preventive techniques. In the current sample, about half (55%) of patients were “well” on the RIFT during the first month post-A-CT. C-CT’s reduction of psychosocial dysfunction was small overall, whereas more frequent therapy sessions during A-CT are associated with large gains in psychosocial functioning (Vittengl et al., 2004). Perhaps it is necessary to increase the frequency of sessions during C-CT and/or to test different patterns of fading (i.e., shorter intervals between) sessions to achieve greater psychosocial improvement.
Convergence of Psychosocial Dysfunction with Cognitive Content and Personality
Our data expand validity information for the RIFT and support the instrument’s use as a brief measure sensitive to both individual differences and changes within patients over time. The RIFT’s substantial convergence with conceptually related measures of psychosocial functioning (GAS, SAS-SR, IIP, DYS) and with depressive symptoms (monthly average PSR and categorical relapse/recurrence) support the measures’ validity in patients with recurrent MDD who respond to A-CT. Moreover, the RIFT correlated significantly with depressive cognitive content (ASQ-F, DAS, SEF) and personality trait dimensions (e.g., negative temperament, self-harm, low positive temperament, detachment).
Temporal Relations Between Psychosocial Functioning and Depression
We found that A-CT responders’ depressive symptoms did not predict monthly changes in psychosocial dysfunction (controlling prior-month dysfunction) significantly, whereas psychosocial dysfunction predicted monthly changes in depressive symptoms and relapse/recurrence (controlling prior-month symptoms). Similarly, many patients left the RIFT’s “well” range before they relapsed/recurred. Previous research indicates that higher RIFT scores predict major depressive relapse/recurrence 6–12 months later (Leon et al., 1999; Solomon et al., 2004). The current analyses additionally suggest that psychosocial dysfunction is a risk factor above-and-beyond current depressive symptoms for relapse/recurrence during the next month.
Relations between psychosocial functioning and depression may be different post-A-CT among responders than during A-CT among acutely depressed patients. During A-CT, depressive symptom change is earlier, greater, and accounts for a large proportion of the change in psychosocial functioning (Hirschfeld et al., 2002; Vittengl et al., 2004). Post-A-CT, we found that depressive symptoms did not predict subsequent psychosocial dysfunction, whereas psychosocial dysfunction predicted subsequent depressive symptoms and relapse/recurrence. We speculate that psychosocial functioning and depressive symptoms are reciprocally influential but differ in their resistance to change. Psychosocial functioning may be a larger system (e.g., involves multiple people, social roles, environments) that changes more slowly than intra-individual experiences of depressive symptoms. As acutely depressed patients improve during ACT, rapid decreases in depressive symptoms may facilitate slower improvements in psychosocial functioning as the social environment begins to notice and “trust” (i.e., perceive as lasting) improvements in the patient’s functioning. Improvements accrued in patients’ psychosocial systems during A-CT may then help protect responders from subsequent increases depressive symptoms post-A-CT. Additional research is needed to test this hypothetical mechanism.
Limitations
Aspects of the study’s sample, design, and assessment limit our conclusions. First, patients had carefully diagnosed recurrent MDD and responded to A-CT, so generalization of our findings to other patient populations requires additional research. Second, depressive symptoms and psychosocial dysfunction were assessed longitudinally but retrospectively every 4 months (Keller et al., 1987). It is possible that patients’ states when assessed influenced their description of prior symptoms and functioning. Third, monthly psychosocial dysfunction scores may obscure time-lagged associations with depressive symptoms at shorter intervals (e.g., weekly or daily). More frequent assessment might allow more sensitive hypothesis tests, albeit with increased costs for patients and researchers. Finally, effects of psychosocial functioning on depressive symptoms in this study’s causal models should be viewed as tentative because of the correlational structure of the dataset.
Clinical Implications
After response to A-CT for unipolar depression, roughly 40–50% of patients continue to experience psychosocial dysfunction. The current formulation of C-CT (10 sessions spread over 8 months) may not improve psychosocial functioning beyond gains made during A-CT among responders. Our results suggest that deteriorations in psychosocial functioning post-A-CT often foreshadow subsequent increases in depressive symptoms and relapse/recurrence. Clinicians may want to assess patients with recurrent MDD to identify specific areas of psychosocial deterioration (e.g., decline in work performance, increase in marital conflict, cessation of leisure activities) preceding prior major depressive episodes. Such areas provide excellent targets to use during stress-inoculation procedures important in relapse prevention. Monitoring identified areas of psychosocial functioning may inform patients and clinicians about the need for treatment to prevent or shorten subsequent major depressive episodes (e.g., increasing the frequency of C-CT sessions and/or initiating pharmacotherapy).
Acknowledgments
The clinical trial was conducted at the University of Texas Southwestern Medical Center as Dallas, Department of Psychiatry, in the Psychosocial Research and Depression Clinic directed by Dr. Jarrett and was supported in part by grants MH-38238 and MH-01571 from the National Institute of Mental Health, Bethesda, MD (Dr. Jarrett). Gratitude is expressed to our colleagues who contributed to this research and have been named previously. We appreciate the administrative support of Eric J. Nestler, MD, PhD (The Lou and Ellen McGinley Distinguished Chair in Psychiatric Research), Department of Psychiatry, The University of Texas Southwestern Medical Center at Dallas.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jeffrey R. Vittengl, Department of Psychology, Truman State University
Lee Anna Clark, Department of Psychology, University of Iowa.
Robin B. Jarrett, Department of Psychiatry, The University of Texas Southwestern Medical Center at Dallas
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders DSM-IV. 4. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. Guilford Press; New York, NY: 1979. [Google Scholar]
- Clark LA. Schedule for Nonadaptive and Adaptive Personality (SNAP) University of Minnesota Press; Minneapolis, MN: 1993. [Google Scholar]
- Clark LA, Simms LJ, Wu KD, Casillas A. (SNAP-2): Manual for Administration, Scoring, and Interpretation. 2. University of Minnesota Press; Minneapolis, MN: Schedule for Nonadapative and Adaptive Personality. in press. [Google Scholar]
- Clark LA, Vittengl JR, Kraft D, Jarrett RB. Separate personality traits from states to predict future depression. J Personal Disord. 2003;17:152–172. doi: 10.1521/pedi.17.2.152.23990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobson KS, Breiter HJ. Cognitive assessment of depression: Reliability and validity of three measures. J Abnorm Psychol. 1983;92:107–109. doi: 10.1037//0021-843x.92.1.107. [DOI] [PubMed] [Google Scholar]
- Haeffel GJ, Abramson LY, Voelz ZR, Metalsky GI, Halberstadt L, Dykman BM, Donovan P, Hogan ME, Hankin BL, Alloy LB. Negative cognitive styles, dysfunctional attitudes, and the remitted depression paradigm: A search for the elusive cognitive vulnerability to depression factor among remitted depressives. Emotion. 2005;5:343–348. doi: 10.1037/1528-3542.5.3.343. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschfeld RMA, Dunner DL, Keitner G, Klein DN, Koran LM, Kornstein SG, Markowitz JC, Miller I, Nemeroff CB, Ninan PT, Rush AJ, Schatzberg AF, Thase ME, Trivedi MH, Borian FE, Crits-Christoph P, Keller MB. Does psychosocial functioning improve independent of depressive symptoms? A comparison of nefazodone, psychotherapy, and their combination. Biol Psychiatry. 2002;51:123–133. doi: 10.1016/s0006-3223(01)01291-4. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureño G, Villaseñor VS. Inventory of interpersonal problems: Psychometric properties and clinical applications. J Consult Clin Psychol. 1988;56:885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- Ilardi SS, Craighead WE. The relationship between personality pathology and dysfunctional cognitions in previously depressed adults. J Abnorm Psychol. 1999;108:51–57. doi: 10.1037//0021-843x.108.1.51. [DOI] [PubMed] [Google Scholar]
- Jarrett RB. Cognitive therapy for recurrent unipolar depressive disorder: The continuation/maintenance phase. University of Texas Southwestern Medical Center; Dallas, TX: 1989. Unpublished manuscript. [Google Scholar]
- Jarrett RB, Kraft D, Doyle J, Foster BM, Eaves GG, Silver PC. Preventing recurrent depression using cognitive therapy with and without a continuation phase: A randomized clinical trial. Arch Gen Psychiatry. 2001;58:381–388. doi: 10.1001/archpsyc.58.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrett RB, Vittengl JR, Clark LA. Preventing recurrent depression. In: Whisman MA, editor. Adapting cognitive therapy for depression: Managing complexity and comorbidity. Guilford; New York, NY: 2008. pp. 132–156. [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, Endicott J, Leon AC, Solomon DA, Coryell W, Maser JD, Keller MB. Psychosocial disability in the course of bipolar I and II disorders: A prospective, comparative, longitudinal study. Arch Gen Psychiatry. 2005;62:1322–1330. doi: 10.1001/archpsyc.62.12.1322. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kennedy N, Foy K, Sherazi R, McDonough M, McKeon P. Long-term social functioning after depression treated by psychiatrists: A review. Bipolar Disord. 2007;9:25–37. doi: 10.1111/j.1399-5618.2007.00326.x. [DOI] [PubMed] [Google Scholar]
- Lansford JE, Antonucci TC, Akiyama H, Takahashi K. A quantitative and qualitative approach to social relationships and well-being in the United States and Japan. J Comp Fam Stud. 2005;36:1–22. [Google Scholar]
- Leader JB, Klein DN. Social adjustment in dysthymia, double depression and episodic major depression. J Affect Disord. 1996;37:91–101. doi: 10.1016/0165-0327(95)00076-3. [DOI] [PubMed] [Google Scholar]
- Leon AC, Solomon DA, Mueller TI, Turvey CL, Endicott J, Keller MB. The Range of Impaired Functioning Tool (LIFE-RIFT): A brief measure of functional impairment. Psychol Med. 1999;29:869–878. doi: 10.1017/s0033291799008570. [DOI] [PubMed] [Google Scholar]
- Morey LC, Hopwood CJ, Gunderson JG, Skodol AE, Shea MT, Yen S, Stout RL, Zanarini MC, Grilo CM, Sanislow CA, McGlashan TH. Comparison of alternative models for personality disorders. Psychol Med. 2007;37:983–994. doi: 10.1017/S0033291706009482. [DOI] [PubMed] [Google Scholar]
- Papakostas GI, Petersen T, Denninger JW, Tossani E, Pava JA, Alpert JE, Nierenberg AA, Fava M. Psychosocial functioning during the treatment of major depressive disorder with fluoxetine. J Clin Psychopharmacol. 2004;24:507–511. doi: 10.1097/01.jcp.0000138761.85363.d5. [DOI] [PubMed] [Google Scholar]
- Peterson C, Seligman ME. Causal explanations as a risk factor for depression: Theory and evidence. Psychol Rev. 1984;91:347–374. [PubMed] [Google Scholar]
- Peterson C, Semmel A, von Baeyer C, Abramson LT, Metalsky GI, Seligman MEP. The Attributional Style Questionnaire. Cognit Ther Res. 1982;6:287–300. [Google Scholar]
- Rodriguez BF, Bruce SE, Pagano ME, Keller MB. Relationships among psychosocial functioning, diagnostic comorbidity, and the recurrence of generalized anxiety disorder, panic disorder, and major depression. J Anxiety Disord. 2005;19:752–766. doi: 10.1016/j.janxdis.2004.10.002. [DOI] [PubMed] [Google Scholar]
- Sherer M, Maddux J, Mercandante B, et al. The Self-Efficacy Scale: Construction and validation. Psychol Rep. 1982;51:663–671. [Google Scholar]
- Solomon DA, Leon AC, Endicott J, Mueller TI, Coryell W, Shea MT, Keller MB. Psychosocial impairment and recurrence in major depression. Compr Psychiatry. 2004;45:423–430. doi: 10.1016/j.comppsych.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38:15–28. [Google Scholar]
- Tennen H, Herzberger S, Nelson HF. Depressive attributional style: The role of self-esteem. J Pers. 1987;55:631–660. doi: 10.1111/j.1467-6494.1987.tb00456.x. [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Jarrett RB. Improvement in social-interpersonal functioning after cognitive therapy for recurrent depression. Psychol Med. 2004;34:643–658. doi: 10.1017/S0033291703001478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Dunn TW, Jarrett RB. Reducing relapse and recurrence in unipolar depression: A comparative meta-analysis of cognitive-behavioral therapy's effects. J Consult Clin Psychol. 2007;73:475–488. doi: 10.1037/0022-006X.75.3.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman AN. The Dysfunctional Attitudes Scale: A validation study. (Doctoral dissertation, University of Pennsylvania) Diss Abstr Int. 1979;40:1389B–1390B. [Google Scholar]
- Weissman MM, Bothwell S. Assessment of social-adjustment by patient self-report. Arch Gen Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Prusoff BA, Thompson Harding PS, Myers JK. Social adjustment by self-report in a community sample and in psychiatric outpatients. J Nerv Ment Dis. 1978;166:317–326. doi: 10.1097/00005053-197805000-00002. [DOI] [PubMed] [Google Scholar]