Abstract
Objectives
To compare the effect of nebulized racemic epinephrine to nebulized racemic albuterol on successful discharge from the emergency department (ED).
Methods
Children up to their 18th month of life presenting to two teaching hospital EDs with a clinical diagnosis of bronchiolitis who were ill enough to warrant treatment but did not need immediate intubation were eligible for this double-blind randomized controlled trial (RCT). Patients received either three doses of racemic albuterol or one dose of racemic epinephrine plus two saline nebulizers. Disposition was decided 2 hours after the first nebulizer. Successful discharge was defined as not requiring additional bronchodilators in the ED after study drug administration and not subsequently admitted within 72 hours. Adjusted relative risks (aRR) were estimated using the modified Poisson regression with successful discharge as the dependent variable and study drug and severity of illness as exposures. Secondary analysis was performed for patients aged less than 12 months and first presentation.
Results
The authors analyzed 703 patients; 352 patients were given albuterol and 351 epinephrine. A total of 173 in the albuterol group and 160 in the epinephrine group were successfully discharged (crude RR = 1.08, 95% confidence interval [CI] = 0.92 to 1.26). When adjusted for severity of illness, patients who received albuterol were significantly more likely than patients receiving epinephrine to be successfully discharged (aRR = 1.18, 95% CI = 1.02 to 1.36). This was also true among those with first presentation and in those less than 12 months of age.
Conclusions
In children up to the 18th month of life, ED treatment of bronchiolitis with nebulized racemic albuterol led to more successful discharges than nebulized epinephrine.
ACADEMIC EMERGENCY MEDICINE 2008; 15:305–313 © 2008 by the Society for Academic Emergency Medicine
Keywords: bronchiolitis, albuterol, epinephrine
Bronchiolitis is a common childhood disease. It is a leading cause of hospitalization worldwide and accounts for substantial morbidity and a mortality of less than 1%.1,2 Between 1980 and 1996, annual infant hospitalization rates for bronchiolitis doubled to 34 per 1,000, while rates for other lower respiratory tract diseases remained stable.3 In 2002, bronchiolitis resulted in 149,000 hospital admissions and annual costs of $543 million in the United States.4
Bronchodilator therapy in bronchiolitis is controversial. Although commonly used,5 its efficacy is not universally accepted. Small studies6–9 and systematic reviews have shown small, short-term improvement in clinical scores in outpatient use of albuterol.10 There is, however, no convincing evidence that albuterol decreases the admission rate in outpatients.10 Some,11–13 but not all,14–16 small studies suggest that epinephrine may decrease admissions in outpatients. A Cochrane review of these studies was inconclusive, however, because of the small numbers overall.17 For the largest study included in that review (comparing racemic albuterol and epinephrine in outpatients), the power to detect a change in admissions of 15% from 50% was 23%. Even if all the cases in that review had been combined in a single study, the power would have been 58%.
The inconclusive results obtained to date suggest that if there is a difference in disposition between racemic albuterol- and epinephrine-treated patients, it is modest. It seems likely that the most important factor predicting the need for admission will be the severity of the bronchiolitis. Without a severity assessment tool validated to predict the need for admission in bronchiolitis, unmeasured but uneven distribution of factors that influence disposition can confound a modest, yet important treatment effect.
The most commonly used tool for severity assessment is the respiratory distress assessment instrument (RDAI). It was originally described in an influential early study evaluating the effect of subcutaneous epinephrine in bronchiolitis.12 The RDAI produces precise scores and is reliable among different users. Although subsequently validated in asthma, it has not been validated for predicting admission in bronchiolitis.18 Despite being widely used, because the RDAI limits its assessment to the respiratory system,12 applying it to infants with bronchiolitis is problematic. By failing to incorporate age it assigns a 3-week-old infant with wheezing a low score, but assigns a high score to an 11-month “happy wheezer” with audible wheeze and chest wall retractions.12 It also does not address other clinical findings such as dehydration, which influence disposition in infants and toddlers.
Prior to undertaking this randomized controlled trial (RCT), we derived a severity-of-illness tool in bronchiolitis patients defining “admission not needed,”“length of hospital stay up to and including the median,” and “length of hospital stay greater than the median,” as ordinal outcome measures. During the derivation of this ordinal regression model, we found that age, dehydration, retraction severity, and tachycardia predicted the outcome.19 We subsequently validated this model at a different children's hospital and measured its interrater reliability at a third site.20 This ordinal regression model reflects the systemic consequences of bronchiolitis in addition to the respiratory component and measures a meaningful outcome. It is presented in Figure 1.
Figure 1.
Ordinal regression model. Reprinted, with permission, from Walsh P, Rothenberg SJ, O'Doherty S, Hoey H, Healy R. A validated clinical model to predict the need for admission and length of stay in children with acute bronchiolitis. Eur J Emerg Med. 2004; 11(5):265–72.19 HR = heart rate.
The primary objective of this study was to compare the effect of nebulized racemic albuterol to nebulized racemic epinephrine on discharge rates among children presenting to the emergency department (ED) with bronchiolitis while adjusting for severity of illness. Our secondary objectives were to determine the effect of these bronchodilators in the subgroups of infants less than 12 months of age and those presenting for the first time.
Methods
Study Design
We conducted a two-site double-blind RCT comparing nebulized racemic albuterol to nebulized racemic epinephrine. Both sites had institutional review board (IRB) approval for the study.
Study Setting and Population
The primary site was a county hospital ED with 53,000 attendances annually (23% children), serving a mixed urban, rural, and suburban population. The secondary site was a community teaching ED with an annual census of 80,000 (20% children). Both hospitals have university affiliations and emergency medicine residencies. The secondary site also has a pediatric residency program. Recruitment occurred from November 1, 2003, to May 1, 2006, and from November 1, 2004, to May 1, 2006, at the primary and secondary sites, respectively.
We defined bronchiolitis operationally as clinical evidence of lower airway obstruction (physical findings of wheezing and chest wall retractions) following an upper respiratory tract infection21 in children up to the 18th month of life. There was no lower age limit. The adopted upper age cutoff represented a midpoint between the ranges of accepted age limit (12 or 24 months) for defining bronchiolitis.4,18,21–23 We excluded children with bronchiolitis who required no treatment, those with illness so severe as to require immediate intubation, and those who received bronchodilators in the ED prior to screening. In our attempt to have broad inclusion criteria, we did not exclude patients with a history of prior episodes of wheezing, lung disease, or other comorbidity. Diagnosis was made by an attending physician or midlevel provider.
All patients with a diagnosis of bronchiolitis judged by the attending physician or physician assistant to require treatment were eligible to be enrolled. The treating physician screened and enrolled patients as they presented to the ED. Signed informed consent was obtained from a parent of all children enrolled.
Research assistants (RAs) assisted study investigators at the primary site. All clinicians and RAs received regular training reinforcement in study procedures throughout each bronchiolitis season. At the secondary site, patients were screened and enrolled on a convenience basis when a study attending physician or research nurse was available.
Study Protocol
Patients were randomized in blocks of 50 to receive either three consecutive doses of nebulized racemic albuterol or a single dose of nebulized racemic epinephrine followed by two nebulized saline treatments. The large block size reduced the risk of allocation bias and physicians being able to guess the identity of the drug. Randomization was performed using a computer-generated random number series and was stratified per site. The pharmacist had sole access to this list and the codes were secured until the study was complete.
The dose of racemic albuterol given was 0.625 mg for infants weighing less than 5 kg and 1.25 mg for those weighing 5 kg or more. The dose of racemic epinephrine was 11.25 mg (0.5 mL of 2.25% solution) regardless of weight. The hospital pharmacist prepared all of the drug packets. Each were identical and presented in sequentially numbered light-protective polythene packets containing three syringes with 0.5 mL of a clear liquid, three 2.5-mL saline vials, a study label, and a package insert with instructions to the user.
All patients received 2.5 mL of nebulized saline during the consent process prior to randomization. Both saline mist and study drugs were delivered using an oxygen-driven VixOne small-volume nebulizer (Westmed, Inc., Tucson, AZ) at 20-minute intervals. A flow rate of 7 L/min was used with wall-mounted oxygen switches and between 6 and 8 L/min with cylinder oxygen. Patients received either three nebulized racemic albuterol doses or one nebulized racemic epinephrine dose, followed by two saline nebulizers.
Data were collected prospectively using standardized forms to document history and physical exam. Data collected included age, history of prematurity, medical history including previous episodes of wheezing, use of albuterol or prednisone before arrival, and any family history of asthma. A nurse recorded the vital signs, including oxygen saturation, at triage, and a physician recorded physical examination findings. When available, RAs scribed the data form and assisted with the consent process.
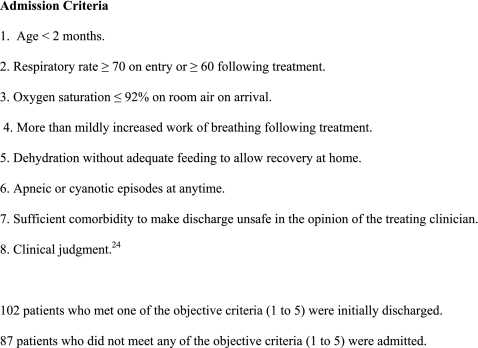
Two hours following the administration of the first dose of the study drug, the treating physician could discharge, admit, or give additional bronchodilators. Patients in this last group were classified as having a prolonged ED stay. Admission criteria are given in Figure 2, although physicians could override these criteria using clinical judgment.24 Viral antigen testing, steroid use, and discharge medications were ordered according to the treating physician's preference.
Figure 2.
Admission criteria.
Outcome Measurements
The primary outcome was “successful discharge,” defined as discharge following study drug administration, not requiring additional bronchodilators in the ED and not resulting in admission within 72 hours of discharge. Patients who were classified as having a prolonged ED stay were counted as admissions. Reattendance within 72 hours (at a clinic, doctor's office, or ED) that did not result in a hospital admission was considered a successful discharge. This outcome was chosen to ensure that the discharge was appropriate and not just temporarily deferred. We verified any further medical contact by reviewing hospital records, telephone follow-up, and checking county coroner's records to verify vital status where follow-up was unsuccessful.
Severity of Illness
Severity-of-illness assignment20 was performed electronically after data collection was complete but before the randomization code was broken. The tool is complex (Figure 1) and at present is designed for research rather than clinical use.
Data Analysis
We calculated a sample size required to provide 90% power (with two-sided alpha level of 0.05) based on admission rates of 33% for patients treated with racemic epinephrine and 50% for racemic albuterol.11 We then rounded this simple sample estimate (n = 374) up to 500 as recommended by Long,25 anticipating logistic regression as the method of analysis. An entire bronchiolitis season was used as the minimum unit of recruitment to avoid potential bias from recruiting for part of the season. There may be differences between children who present early or late in the season.
Analyses were performed on an “intent-to-treat” basis. We analyzed only the first enrollment of patients who were enrolled more than once during the study.
We modeled severity as categorical variables rather than as an ordinal variable. We created a fourth severity category, containing patients missing one or more of the variables needed to determine illness severity. Study site of enrollment was modeled as a categorical variable. Owing to the relatively common outcome, we estimated adjusted relative risks, (aRR), using modified Poisson regression as described by Zou,26 rather than odds ratios. We present aRR with 95% confidence intervals (CIs) using successful discharge as the dependent variable and study drug, severity of illness, and study site as exposures. We also constructed other models to account for the patients with missing observations on the severity scale by using multiple imputations and by excluding these cases from the model. We also performed a Mantel-Haenszel simple stratified analysis, stratifying only for disease severity.
Cases that met admission criteria at enrollment were included in the primary analysis. It was felt that if a significant proportion of these patients improved sufficiently to be discharged posttreatment, this would be an important finding. We excluded these in a sensitivity analysis. We also excluded the prolonged ED treatment group in a sensitivity analysis. We analyzed patients with recurrent wheezing and patients over 12 months of age both by excluding them and by constructing a model with categorical variables for these and other variables of potential interest. These sensitivity analyses used a Poisson model with stepwise backward selection to examine the effect of all the primary and secondary endpoints by including the variables: patients with recurrent wheezing, prematurity, age less than 2 months, steroid use, hypoxia, and a family history of asthma.
We performed double data entry using a customized Filemaker-Pro (Filemaker-Pro, Version 6, Santa Clara, CA) database. Statistical analysis was performed using Stata 9.2 (Release 10, Statacorp, College Station, TX).
Results
A total of 721 patients were enrolled, 655 at one site and 66 at the other. Following the exclusion of those with eligibility violations or multiple enrollments, 703 were analyzed (Figure 3). The mean age of all patients enrolled was 6 months (median 4.8 months), 407 (58%) were male, and 610 (87%) were less than 12 months of age. Respiratory syncytial virus antigen was present in 313 of the 553 (57%) patients tested in the ED. The baseline characteristics are broadly similar and shown in Table 1.
Figure 3.
Consort diagram.
Table 1.
Baseline Patient Variables
| Variable | Epinephrine (n = 351) | Albuterol (n = 352) | p-Value (Univariate Testing) |
|---|---|---|---|
| Median age in months (IQR) | 4.8 (6.2) | 4.9 (6.1) | 1.00 |
| Male, N = 407 (57.9%) | 213 (60.7) | 194 (55.1) | 0.15 |
| Ex-premature (%) | 61 (17.4) | 69 (19.6) | 0.50 |
| Asthma or RAD in any member of immediate family | 70 (19.9) | 69 (19.6) | 0.93 |
| On albuterol before arrival in the ED, n (%) | 60 (17.1) | 64 (18.2) | 0.77 |
| On prednisone before arrival in the ED, n (%) | 15 (4.3) | 19 (5.4) | 0.66 |
| Temperature ≥ 38°C (%) | 129 (36.8) | 140 (39.8) | 0.62 |
| Age ≤ 2 months (%) | 76 (21.7) | 75 (21.3) | 1.00 |
| Age > 12 months (%) | 52 (14.8) | 41 (11.7) | 0.22 |
| First-time wheezing (%) | 198/280 (70.7) | 205/287 (71.4) | 0.85 |
| RSV antigen-positive (%) | 152/276 (55.1) | 161/277 (58.1) | 0.49 |
| SaO2 ≤ 92% (%) | 35/344 (10.2) | 25/342 (7.3) | 0.22 |
| SaO2 (±SD) | 97 (4) | 97 (3) | 0.63 |
| Mean temperature, °F (±SD) | 100.0 (1.7) | 99.9 (1.7) | 0.55 |
| Mean HR (±SD) | 156 (24) | 158 (23) | 0.35 |
| Mean RR (±SD) | 47 (13) | 46 (12) | 0.50 |
| Tachycardic (%) | 74/350 (21.1) | 88/352 (25.0) | 0.25 |
| Hydration status (%) | n = 342 | n = 346 | |
| Normal | 303 (88.6) | 303 (87.6) | |
| 5% dehydration | 24 (7.0) | 38 (11.0) | 0.02 |
| 10% dehydration | 14 (4.1) | 5 (1.5) | |
| 15% dehydration | 1 (0.3) | 0 (0) | |
| Increased work of breathing retraction severity (%) | n = 313 | n = 331 | |
| None | 20 (6.4) | 27 (8.2) | |
| Mild | 162 (51.8) | 161 (48.6) | 0.62 |
| Moderate | 115 (36.7) | 130 (39.3) | |
| Severe | 16 (5.1) | 13 (3.9) |
ED = emergency department; HR = heart rate; IQR = interquartile range; RAD = reactive airway disease; RR = respiratory rate; RSV = respiratory syncytial virus; SaO2 = oxygen saturation.
There were 352 patients in the racemic albuterol group and 351 patients in the racemic epinephrine group. Figure 4 shows the age distribution of patients by treatment group. Patient flow to their ultimate disposition is shown in Figure 5. Bronchiolitis was classified as mild, moderate, and severe in 175, 419, and 47 children, respectively. The racemic albuterol group had significantly more (p = 0.007) moderately ill, but fewer mildly ill, patients compared to the racemic epinephrine group. Table 2 depicts the drug assignment and disposition of each severity-of-illness category. Patients were successfully discharged in 333 of 703 (47.4%) cases. Successful discharge decreased directly with severity of illness: moderate (aRR = 0.49, 95% CI = 0.42 to 0.57) and severe (aRR = 0.20, 95% CI = 0.10 to 0.39), compared with mild disease. The proportion of those successfully discharged in each treatment arm for each severity-of-illness category is shown in Figure 6.
Figure 4.
Age distribution of the study patients.
Figure 5.
Numbers successfully discharged and admitted. ED = emergency department.
Table 2.
Severity-of-illness and Outcomes Classification for Each Treatment Group
| Severity of Illness (Total N = 352) | Epinephrine with Data, n = 310 (Total N = 351) | Albuterol with Data, n = 331 |
|---|---|---|
| Successful discharge | 160 (45.6) | 173 (49.2) |
| Admitted | 191 (54.2) | 179 (50.9) |
| Met admission criteria at any time | 181 (51.6) | 186 (52.8) |
| Met admission criteria at any time but successfully discharged | 43/181 (23.8) | 50/186 (26.9) |
| Met admission criteria on entry | 96/321 (29.9) | 91/337 (27.0) |
| Discharged despite meeting admission criteria on entry | 22/96 (22.9) | 21/91 (23.1) |
| Discharged on albuterol | 104/138 (75.4) | 112/139 (80.6) |
| Mild | 97/310 (31.0) | 78/331 (23.6) |
| Successfully discharged | 66/97 (68.0) | 63/78 (80.8) |
| Moderate | 193/310 (62.3) | 228/331 (68.8) |
| Successfully discharged | 63/192 (32.8) | 93/227 (41.0) |
| Severe | 21/310 (6.8) | 26/331 (7.9) |
| Successfully discharged | 2/21 (16.7) | 5/26 (19.2) |
| Missing data | 41/351 (11.7) | 21/352 (6.0) |
| Successfully discharged | 29/41 (70.7) | 12/21 (57.1) |
Figure 6.
Summary of results. Successful discharge by severity of illness. Alb = albuterol; Epi = epinephrine.
Admission rates at the primary site were 52% (331/640) and at the secondary site were 62% (39/63). There were marginally significantly fewer discharges in the secondary site (aRR = 0.76, 95% CI = 0.56 to 1.03). While discharge rates and outpatient treatment failures were higher at the primary site, the use of clinical judgment rather than other admission criteria, other patient characteristics, and steroid use were similar at both sites. Thirty-seven had a second ED visit within 3 days. Six were readmitted within 3 days of initial ED discharge in the racemic albuterol group and 10 patients in the racemic epinephrine group, all from the primary site. Forty-nine of 177 (27.7%) patients who met admission criteria at entry from the primary site were discharged, while all of those who met admission criteria at entry were admitted from the secondary site. Our primary outcome results include adjustment for site.
Crude analysis (not adjusting for severity of illness) showed no difference between groups (RR 1.08, 95% CI = 0.92 to 1.26). After stratification by severity of illness, patients who received racemic albuterol were significantly more likely than patients receiving racemic epinephrine to be successfully discharged (aRR = 1.18, 95% CI = 1.02 to 1.36). This result was the same using Poisson regression and Mantel-Haenszel stratified analysis. Excluding those in the “prolonged ED treatment” group did not change the treatment results (aRR = 1.16, 95% CI = 1.01 to 1.33) in Poisson regression. Racemic albuterol's advantage did not change in the sensitivity analysis controlling for potential confounders age less than 12 months, prematurity, hypoxia, and history of prior wheezing (aRR 1.18, 95% CI = 1.02 to 1.37) (Table 3).
Table 3.
Sensitivity Analyses to Assess the Importance of Other Variables on Probability of Successful Discharge (the Benefit of Albuterol Was Unchanged by Their Inclusion)
| Variable | aRR of Successful Discharge | 95% CI | p-Value |
|---|---|---|---|
| Albuterol | 1.18 | 1.02, 1.37 | 0.026 |
| Moderate* | 0.51 | 0.44, 0.60 | <0.001 |
| Severe* | 0.25 | 0.13, 0.49 | <0.001 |
| Not classified* | 0.88 | 0.72, 1.08 | 0.216 |
| Secondary site | 0.84 | 0.63, 1.14 | 0.262 |
| Age < 12 months | 0.98 | 0.81, 1.18 | 0.805 |
| Ex-premature | 0.71 | 0.56, 0.89 | 0.003 |
| Hypoxia | 0.41 | 0.23, 0.74 | 0.003 |
| Prior wheezing | 1.36 | 1.14, 1.62 | 0.001 |
aRR = adjusted relative risk; CI = confidence interval.
Reference category is mild disease. n for this model is 686. The same results for severity of illness and drug were obtained using Mantel-Haenszel stratified analysis.
A total of 187 patients met admission criteria at entry. Some of these were successfully discharged (see Table 2). Excluding those who met admission criteria on entry had little effect on the results (aRR 1.22, 95% CI = 1.04 to 1.43). Interrater reliability of the severity assessment tool (assessed only at the primary site) was substantial (κ = 0.68).27
Incomplete Data
The data required to calculate the severity of illness were incomplete in 62 of 703 (8.8%) cases. Risk of discharge for this group was indistinguishable from the mild severity group (aRR = 0.89, 95% CI = 0.73 to 1.09). Neither excluding these cases nor using multiple imputations changed the results (analysis not shown).
Including only infants less than 12 months, using age less than 12 months as a categorical variable or excluding subjects aged less than 2 months did not change the significant advantage of racemic albuterol over racemic epinephrine. Patients with recurrent wheezing were slightly less likely to be admitted (Table 3).
Adverse Effects
Tachycardia (defined by heart rate above the 97th percentile for age) was noted before treatment in 88 of 352 (25%) in the racemic albuterol group and 74 of 351 (21%) in the racemic epinephrine group. Posttreatment tachycardia was only noted in 52 (15%) in the former and in 42 (12%) in the latter (p = 0.32). Two patients developed perioral cold-induced urticaria. This resolved rapidly, and one received promethazine. Both were in the racemic epinephrine group and had used cylinder oxygen. One death in the racemic epinephrine group was reported within 30 days.
Discussion
Our crude results did not show a difference between agents. When we adjusted for severity, we found a lower risk of admission with the use of nebulized racemic albuterol when compared to racemic epinephrine in children presenting to the ED with bronchiolitis. This was an unexpected result and contrasted with some,11,15,28 although not all,7–9,16 existing studies. However, to the best of our knowledge, our study is the largest to date examining this question. Our results held true in all subgroups: hypoxia, age less than 12 months, prematurity, and a family history of asthma do not alter the advantage of racemic albuterol over racemic epinephrine in reducing admissions. Broad inclusion criteria helped ensure adequate sample size. Unlike many smaller studies, our sample represents the breadth of bronchiolitis seen in the ED each season.
One of the ironies of bronchiolitis research is that while bronchiolitis is agreed to be common, most studies of it are small. This is in part due to difficulties in defining the condition and distinguishing it from asthma. The term asthma is itself so broad and ill-defined that at least one editorialist has called for the term to be classified as a symptom rather than a diagnosis.29 Furthermore, it is doubtful if asthma should ever be diagnosed in the age group that we studied. Our definition of bronchiolitis is consistent with the often heterogeneous28 definitions used by others.21 We have also addressed elements seen in other definitions by both subgroup and multivariate analysis and consistently obtained results favoring racemic albuterol.
Comparing pretreatment groups by the probability of admission sets a substantially higher bar than simply comparing the distribution of individual variables between treatment arms. The latter method can lead to the appearance of balance when in fact the preintervention probability of admission differs between groups. The former requires a validated tool to predict admission and an adjusted analysis in the event that groups are not balanced or much larger sample sizes to increase the probability of treatment group balance or subject pair matching at enrollment.
From a practical standpoint, implementation of subject–pair matching would require an automated system deployed across several aggressively recruiting sites that allows rapid input of patient data, classifies severity of disease, and finds a matching case. Such a solution is clearly resource-intensive. We opted for simple enrollment and subsequent adjustment for disease severity using a validated tool, which was feasible and cost-effective and minimized barriers to recruitment by treating clinicians.
Had we ignored severity of illness, or assumed equal pretreatment probability of discharge in each treatment arm, we would have erroneously concluded that there was no difference between the drugs. Our design addressed the limitation that two relatively large groups may have a similar distribution of potentially confounding variables overall in each group, but have different combinations of these confounders at the level of individual subjects.
Failure to address this can result in erroneous interpretation of RCTs, as has emerged when large trials were reanalyzed.30
We had anticipated this possibility in the design stage and decided a priori to apply a severity-of-illness tool in our analysis to adjust for the effect of severity of illness on the probability of discharge within this sample. Thereafter, we evaluated the additional effect of the drugs on discharge risk. We consider this methodology to be a design strength compared with previous RCTs.30
The choice of severity-of-illness tool is important. We used the National Children's Hospital (NCH) severity-of-illness tool because it has been validated with respect to need for admission. The relative complexity of this tool precluded stratification prior to enrollment. The more widely used RDAI has been reported as having almost perfect agreement (κ = 0.9) for the wheezing component and substantial agreement (κ = 0.64) for the presence of retractions component in its original description. An overall kappa was not reported.12 We and others have found worse agreement for auscultatory findings in infants,21,31 but that overall the reliability of our severity-of-illness tool (κ = 0.68) was sufficient to permit its use. Previously employed severity-of-illness or clinical scores have not been validated to predict disposition in bronchiolitis, whereas the model we used has.19
Our data show racemic albuterol leads to lower discharge rates in each severity-of-illness stratum (Figure 6), but that when these strata are combined there is no difference. The Yule-Simpson “paradox” describes just this situation, where the success of several subgroups may be reduced or even reversed when these subgroups are combined.32 The conditions required for the “paradox,” namely, the combination of an imbalance in the proportion of each subgroup receiving each intervention and a different event rate in each subgroup, are present in our data.33 This combination requires inclusion of this confounding variable in a multivariate regression analysis.34 Almost identical results were obtained using Mantel-Haenszel stratified analyses.
Another difference between our study and others is that determination of disposition was at 2 hours following the initial nebulized treatment. This reflects the widespread clinical practice of observing patients following epinephrine, rather than immediately discharging them. Our observation period ensured that disposition was not prematurely decided based on initial improvement. Studies have shown a benefit in clinical scores in the initial 15–60 minutes for infants receiving epinephrine,13,35 but overall this benefit is short-lived.17 This study, however, does not exclude a role for epinephrine. Further research is needed to address which subsequent agent should be used following inadequate response to albuterol or whether there is a synergistic effect to using both.
Limitations
The age cutoff for inclusion in this study was a compromise between the widely accepted definitions of less than 1 or 2 years of age. Reducing the upper age limit could reduce the enrollment of patients with recurrent wheezing and perhaps some of those who may subsequently develop asthma. We reanalyzed the sample population introducing age less than 12 months and first presentation as model variables. We also reanalyzed the sample after excluding patients over 12 months. In these alternative models, we continued to find results favoring racemic albuterol. Similarly, a history of recurrent wheezing or a family history of asthma did not change the treatment effects. Consequently, despite our broad inclusion criteria, our results likely hold across even the subsets of children presenting to the ED with bronchiolitis, subsets represented by some prior, more narrowly defined, but inconclusive studies.
The number of eligible patients not enrolled in the study was unknown, as the primary site IRB did not permit the collection of any information about patients either who were not enrolled due to refusal of consent or who had not been approached for consent. Anecdotal experience suggests that this number was small at the primary site. We were not able to determine the specific reason for admission, as we did not require physicians to specifically document this.
The relatively low sample size in the secondary site could be attributed to physician difference in diagnosing bronchiolitis or the availability of researchers. While it likely represents a convenience sample, the results of the secondary site paralleled those at the primary site. The numbers at the primary site, where the recruitment period was longer, were a reflection of the efforts of the investigators (who actively recruited patients from the waiting room), availability of RAs up to 16 hours a day, and widespread knowledge of the study throughout the community and the emergency medical services. At the secondary site, a research nurse was available 40 hours a week. We addressed this difference in site recruitment by including site as a variable in the model, where it approached statistical significance in its own right but did not alter albuterol's advantage.
Ideally, we would have performed stratified randomization, thereby avoiding the need for stratified or adjusted analysis. However, the severity-of-illness tool we used is complex and applying it at the randomization stage would have posed a significant barrier to recruitment. It could also introduce bias if an investigator was enrolling the patient and knew the severity score.
Potential Biases in Favor of Racemic Epinephrine
We accounted for missing data by creating a fourth severity-of-illness category, by excluding these cases, and by estimating their missing values using multiple imputation.35,36 In all cases, the treatment effects were essentially the same regardless of statistical strategy. Nonetheless, this is much less desirable than having completed data sheets. This is particularly the case as the number of incomplete data sheets was higher in the racemic epinephrine than the racemic albuterol group, potentially biasing the results. The nonsignificant aRR of the incomplete data group means that it cannot be distinguished from the mild group, potentially indicating more mild-type cases in the epinephrine group. Neither dropping these cases nor multiple imputations for these missing values changed our results. Some patients could have received more or less racemic albuterol than if we had dosed on a strictly milligram per kilogram fashion, and some may regard our doses as low. This could bias our results against albuterol.
Potential Biases in Favor of Racemic Albuterol
The last dose of active medication in the albuterol group was administered closer to the time that the disposition decision was made than in the racemic epinephrine group. This would bias the results against epinephrine assuming that racemic albuterol has an advantage over saline.
Using a single dose of racemic epinephrine, rather than three doses, reflects clinical practice. The dose of racemic epinephrine (11.25 mg regardless of weight; others have used 0.15 to 0.9 mg/kg)15,28 is comparable to that used for treating croup. This relatively high dosage minimized the potential disadvantage of using a single dose.
Potential Biases to the Null
All patients received saline mist during the consent process prior to randomization. If saline mist has a benefit, this would bias the study to the null. We used saline nebulizers following the racemic epinephrine treatment to maintain blinding. Again, any beneficial effect of saline would have biased the study to the null.
Racemic albuterol was prescribed equally among those discharged from each treatment arm. This would be expected to narrow the differences in unscheduled admissions between treatment groups following discharge and increase the likelihood of a Type 2 error.
We would have liked to control for discharge medications, but to achieve this would have required unanimous agreement from all the EPs, pediatricians, and family physicians serving the study site and would likely have prevented the study from proceeding. We found discharge medications to be similar between groups.
Conclusions
In children up to the 18th month of life presenting to the ED with a clinical diagnosis of bronchiolitis, racemic albuterol, rather than racemic epinephrine, should be the initial agent chosen, as doing so modestly increases the rate of successful discharge.
Acknowledgments
The authors acknowledge the assistance of the following: Valarie Cortez (Kern Medical Center, Bakersfield College) for data collection and data entry; Thomas Purcell, MD (Kern Medical Center), for database design; Chris Steffensen, PharmD (Advocate Christ Medical Center), for study implementation; Rolla Sweis, PharmD (Advocate Christ Medical Center), for study implementation; Sam Kuan MB, BCh, BAO, and Jonathon Wasserberger, MD, for help with the manuscript; and Peter Tseng (UCLA) and Tiago Pereira (Federal University of São Paulo) for help with statistical analysis.
References
- 1.Leung AK, Kellner JD, Davies HD. Respiratory syncytial virus bronchiolitis. J Natl Med Assoc. 2005;97(12):1708–13. [PMC free article] [PubMed] [Google Scholar]
- 2.Shay DK, Holman RC, Roosevelt GE, Clarke MJ, Anderson LJ. Bronchiolitis-associated mortality and estimates of respiratory syncytial virus-associated deaths among US children, 1979–1997. J Infect Dis. 2001;183(1):16–22. doi: 10.1086/317655. [DOI] [PubMed] [Google Scholar]
- 3.Lowther SA, Shay DK, Holman RC, Clarke MJ, Kaufman SF, Anderson LJ. Bronchiolitis-associated hospitalizations among American Indian and Alaska Native children. Pediatr Infect Dis J. 2000;19(1):11–7. doi: 10.1097/00006454-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Pelletier AJ, Mansbach JM, Camargo CA., Jr Direct Medical Costs of Bronchiolitis Hospitalizations in the United States. Pediatrics. 2006;118(6):2418–23. doi: 10.1542/peds.2006-1193. [DOI] [PubMed] [Google Scholar]
- 5.Plint AC, Johnson DW, Wiebe N, et al. Practice variation among pediatric emergency departments in the treatment of bronchiolitis. Acad Emerg Med. 2004;11:353–60. doi: 10.1197/j.aem.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Schuh S, Canny G, Reisman JJ, et al. Nebulized albuterol in acute bronchiolitis. J Pediatr. 1990;117(4):633–7. doi: 10.1016/s0022-3476(05)80706-1. [DOI] [PubMed] [Google Scholar]
- 7.Can D, Inan G, Yendur G, Oral R, Gunay I. Salbutamol or mist in acute bronchiolitis. Acta Paediatr Jpn. 1998;40(3):252–5. doi: 10.1111/j.1442-200x.1998.tb01922.x. [DOI] [PubMed] [Google Scholar]
- 8.Klassen TP, Rowe PC, Sutcliffe T, Ropp LJ, McDowell IW, Li MM. Randomized trial of salbutamol in acute bronchiolitis. J Pediatr. 1991;118(5):807–11. doi: 10.1016/s0022-3476(05)80051-4. [DOI] [PubMed] [Google Scholar]
- 9.Schweich PJ, Hurt TL, Walkley EI, Mullen N, Archibald LF. The use of nebulized albuterol in wheezing infants. Pediatr Emerg Care. 1992;8(4):184–8. doi: 10.1097/00006565-199208000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Gadomski AM, Bhasale AL. Bronchodilators for bronchiolitis. Cochrane Database Syst Rev. 2006;3 doi: 10.1002/14651858.CD001266.pub2. CD001266. [DOI] [PubMed] [Google Scholar]
- 11.Menon K, Sutcliffe T, Klassen TP. A randomized trial comparing the efficacy of epinephrine with salbutamol in the treatment of acute bronchiolitis. J Pediatr. 1995;126(6):1004–7. doi: 10.1016/s0022-3476(95)70234-2. [DOI] [PubMed] [Google Scholar]
- 12.Lowell DI, Lister G, Von Koss H, McCarthy P. Wheezing in Infants: the response to epinephrine. Pediatrics. 1987;79(6):939–45. [PubMed] [Google Scholar]
- 13.Ray MS, Singh V. Comparison of nebulized adrenaline versus salbutamol in wheeze associated respiratory tract infection in infants. Indian Pediatr. 2002;39(1):12–22. [PubMed] [Google Scholar]
- 14.Ralston S, Hartenberger C, Anaya T, Qualls C, Kelly HW. Randomized, placebo-controlled trial of albuterol and epinephrine at equipotent beta-2 agonist doses in acute bronchiolitis. Pediatr Pulmonol. 2005;40(4):292–9. doi: 10.1002/ppul.20260. [DOI] [PubMed] [Google Scholar]
- 15.Mull CC, Scarfone RJ, Ferri LR, et al. A randomized trial of nebulized epinephrine vs albuterol in the emergency department treatment of bronchiolitis. Arch Pediatr Adolesc Med. 2004;158(2):113–8. doi: 10.1001/archpedi.158.2.113. [DOI] [PubMed] [Google Scholar]
- 16.Hariprakash S, Alexander J, Carroll W, et al. Randomized controlled trial of nebulized adrenaline in acute bronchiolitis. Pediatr Allergy Immunol. 2003;14(2):134–9. doi: 10.1034/j.1399-3038.2003.00014.x. [DOI] [PubMed] [Google Scholar]
- 17.Hartling L, Wiebe N, Russell K, Patel H, Klassen TP. Epinephrine for bronchiolitis. Cochrane Database Syst Rev. 2004;1 doi: 10.1002/14651858.CD003123.pub2. CD003123. [DOI] [PubMed] [Google Scholar]
- 18.Subcommittee on Diagnosis and Management of Bronchiolitis Diagnosis and management of bronchiolitis. Pediatrics. 2006;118(4):1774–93. doi: 10.1542/peds.2006-2223. [DOI] [PubMed] [Google Scholar]
- 19.Walsh P, Rothenberg SJ, O’Doherty S, Hoey H, Healy R. A validated clinical model to predict the need for admission and length of stay in children with acute bronchiolitis. Eur J Emerg Med. 2004;11(5):265–72. doi: 10.1097/00063110-200410000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Walsh P, Gonzales A, Satar A, Rothenberg SJ. The interrater reliability of a validated bronchiolitis severity assessment tool. Pediatr Emerg Care. 2006;22(5):316–20. doi: 10.1097/01.pec.0000215136.44286.8f. [DOI] [PubMed] [Google Scholar]
- 21.Kuppermann N, Bank DE, Walton EA, Senac MO, Jr, McCaslin I. Risks for bacteremia and urinary tract infections in young febrile children with bronchiolitis. Arch Pediatr Adolesc Med. 1997;151(12):1207–14. doi: 10.1001/archpedi.1997.02170490033006. [DOI] [PubMed] [Google Scholar]
- 22.Corneli HM, Zorc JJ, Majahan P, et al. A multicenter, randomized, controlled trial of dexamethasone for bronchiolitis. N Engl J Med. 2007;357(4):331–9. doi: 10.1056/NEJMoa071255. [DOI] [PubMed] [Google Scholar]
- 23.McConnochie KM, Roghmann KJ. Bronchiolitis as a possible cause of wheezing in childhood: new evidence. Pediatrics. 1984;74(1):1–10. [PubMed] [Google Scholar]
- 24.Ruddy RM, Gittleman M. Updates in Pediatric Emergencies. Atlanta, GA: American Healthcare Consultants; 1999. The wheezing infant. [Google Scholar]
- 25.Long JS. Regression Models for Categorical and Limited Dependent Variables. 1st ed. Thousand Oaks, CA: Sage Publications; 1997. [Google Scholar]
- 26.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 27.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 28.Patel H, Platt RW, Pekeles GS, Ducharme FM. A randomized, controlled trial of the effectiveness of nebulized therapy with epinephrine compared with albuterol and saline in infants hospitalized for acute viral bronchiolitis. J Pediatr. 2002;141(6):818–24. doi: 10.1067/mpd.2002.129844. [DOI] [PubMed] [Google Scholar]
- 29.Anonymous A plea to abandon asthma as a disease concept. Lancet. 2006;368(9537):705. doi: 10.1016/S0140-6736(06)69257-X. [DOI] [PubMed] [Google Scholar]
- 30.Kent D, Hayword R. When averages hide individual differences in clinical trials. Am Sci Online. 2007 (January February 2007). Available at: http://www.americanscientist.org/template/AssetDetail/assetid/54440. Accessed Dec 13, 2007. [Google Scholar]
- 31.Wang EE, Law BJ, Stephens D, et al. Study of interobserver reliability in clinical assessment of RSV lower respiratory illness: a Pediatric Investigators Collaborative Network for Infections in Canada (PICNIC) study. Pediatr Pulmonol. 1996;22(1):23–7. doi: 10.1002/(SICI)1099-0496(199607)22:1<23::AID-PPUL4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 32.Simpson EH. The interpretation of interaction in contingency tables. J Roy Stat Soc. 1951;13:238–41. [Google Scholar]
- 33.Perera R. Statistics and death from meningococcal disease in children. BMJ. 2006;332(7553):1297–8. doi: 10.1136/bmj.332.7553.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Julious SA, Mullee MA. Confounding and Simpson's paradox. Br Med J. 1994;309(6967):1480–1. doi: 10.1136/bmj.309.6967.1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goldstein R. Patterns of missing data. Stata Technical Bull. 1996;32:12–3. [Google Scholar]
- 36.Goldstein R. Patterns of missing data update. Stata Technical Bull. 1996;32:2. [Google Scholar]