Abstract
The current recommended dietary allowance (RDA) for vitamin C, as proposed by the Food and Nutrition Board/National Research Council in 1980 and reconfirmed in 1989, is 60 mg daily for nonsmoking adult males. Levine et al. [Levine, M., Conry-Cantilena, C., Wang, Y., Welch, R. W., Washko, P. W., et al. (1996) Proc. Natl. Acad. Sci. USA 93, 3704–3709], based on a study of vitamin C pharmacokinetics in seven healthy men, have now proposed that the RDA should be increased to 200 mg daily. I have examined, in brief, the experimental and conceptual bases for this new recommendation and its implications for public health and nutrition policy and programs. Using, for illustrative purposes only, data extracted from each of two recent dietary surveys of noninstitutionalized adult males living in households in the Netherlands and the United States, it is predicted that the prevalence of intakes inadequate to meet the individual’s own requirement would be about 96% or 84%, respectively, if the criteria of adequacy used for derivation of the 200 mg RDA are accepted. Depending upon the particular average requirement value for ascorbic acid that might be derived from their data, the proposal by Levine et al. would mean a desirable increase in mean intakes in these two populations by as much about 2- to 3-fold. Hence, before an action of this kind is to be recommended, an answer must be sought to the question whether current experimental data including the criteria selected (saturation kinetics) are adequate to establish a new set of requirements for vitamin C, which then carry such profound policy implications. This will require critical assessment of all of the available evidence emerging from laboratory, clinical, and epidemiological studies to determine whether it provides a sufficient rationale for accepting criteria of vitamin C adequacy such as those proposed by Levine et al. and the requirement estimates so derived.
Keywords: requirements, dietary intakes, criterion of adequacy
According to the 1989 report of the Food and Nutrition Board/National Research Council (FNB/NRC) (1), the recommended dietary allowances (RDAs) are “the levels of intake of essential nutrients that, on the basis of scientific knowledge, are judged by the Food and Nutrition Board to be adequate to meet the known nutrient needs of practically all healthy persons.” For adult men and women, the RDA for ascorbic acid was set at 60 mg per day, which was the same figure as had been proposed in the earlier 1980 report (2). According to the latter report (2), this value of 60 mg was based upon a consideration of (i) the observed rate of the turnover and rate of depletion of an initial body ascorbic acid pool of 1500 mg; (ii) an assumed absorption of ascorbic acid of about 85% at usual intakes; and (iii) the variable loss of ascorbic acid during food preparation. The last should not have been included, because as noted above, the RDA is meant to be an actual intake level rather than a dietary content. Nevertheless, it was predicted that this intake of 60 mg daily would prevent development of signs of scurvy for at least 4 weeks on a diet lacking vitamin C. Levine et al. (3) recently reported the results of a vitamin C depletion-repletion pharmacokinetic study in seven healthy men, which had been carried out to reexamine the RDA for vitamin C. They concluded that the RDA should be increased to 200 mg daily.
The purpose of this discussion is to examine the experimental and conceptual bases of the recommendation by Levine et al. (3) and to assess the possible implications of the recommendation for public health and nutrition policy and programs. Although this paper is not intended to arrive at a judgment regarding the appropriate value for the ascorbic acid RDA, it seems important in view of the interest (4) expressed in the study by Levine et al. (3) to emphasize here a number of significant experimental and conceptual issues that were raised in or emerge from their paper and the conclusions that were drawn. The major issues are: (i) the criterion of nutritional adequacy; (ii) determination of a mean requirement of a well-defined population group and the variability in requirements among apparently similar individuals within the population; (iii) the establishment of a reference nutrient intake value, such as the RDA or an upper intake level above which a negative response might be expected; and (iv) the public health and nutrition policies that require use of nutrient requirement estimates.
Criteria of Nutritional Adequacy
A recent World Health Organization/Food and Agriculture Organization/International Atomic Energy Agency (WHO/FAO/IAEA) committee (5) has defined a requirement as “. . . the lowest continuing level of nutrient intake that, at a specified efficiency of utilization, will maintain the defined level of nutriture in the individual.” Thus, the requirement value for any nutrient will be determined by the choice of the criterion used to establish the defined level of nutriture. The committee (5) also recognized that requirements varied among otherwise similar individuals and so it is also necessary to deal with distributions of requirements for each selected criterion of adequacy. There are existing conventions for selection of single points to represent those distributions. Thus, in the case of iron, for example, an earlier FAO/WHO committee (6) considered three distinct requirement estimates based on different criteria of adequacy. For menstruating women consuming a high-availability diet (about 22.5% absorption), the median requirements were estimated to be 5.6 mg per day to prevent anemia, 8.3 mg per day to maintain a normal supply of iron to tissues and preserve all clinically detectable functions as marked by the hematopoietic function (basal requirement), and 12.5 mg per day to generate and maintain a normative level of tissue iron storage that many have deemed desirable as a “reserve” (normative requirement).
At the same time, that committee (6) estimated the 95th centiles of individual requirements as 10, 16, and 24 mg per day for the requirement to prevent anemia, basal requirement, and normative requirement, respectively. However, while the FAO/WHO committee (6) presented the basis of derivation of the normative requirements, it did not publish specific, numeric estimates for this dietary reference intake value. In its judgment, the figures were too high to be achieved by normal diets and so it did not wish to be seen as promoting iron supplementation or fortification that would not be expected a priori to carry any functional or defined health benefit for general populations. The important points to note are that the committee took account of three dimensions in reaching its final judgments regarding recommended levels of intake: (i) level of requirement (criteria), (ii) variability of requirement, and (iii) implications of its recommendations when viewed in relation to existing patterns of dietary iron intake. In that same report (6), folic acid requirements were estimated at the basal and normative levels. For adult women, the estimated mean requirements were 50 (basal) and 135 (normative) μg per day. The inferred estimate of the mean requirements for vitamin A in adult women would be approximately 195 (basal) and 360 (normative) retinol equivalents (1 μg all-trans retinol) per day (6). Further, comparisons of this kind for various nutrients are given elsewhere (7).
The foregoing is relevant to the determination of the requirement and recommended intake for ascorbic acid, since the study by Levine et al. (3) included an examination of the relationship between intakes of vitamin C, ranging from 30 to 2500 mg daily, and measurements of the concentration of the vitamin in plasma, neutrophils, monocytes, and lymphocytes, bioavailability (determined from oral and intravenous administration of vitamin C), and urinary excretion of ascorbic acid, urate, and oxalate. A 100 mg daily intake level resulted in saturation levels of ascorbic acid in the cells, whereas a plateau plasma vitamin C level that was close to maximum was achieved at an intake of 200 mg daily and utilization was found to be complete for a single 200 mg dose but proportional utilization declined thereafter. Thus, depending upon the criterion of nutritional adequacy chosen, these data could be taken to indicate an apparent, mean requirement for ascorbic acid of 100 mg daily if based on saturation of neutrophil ascorbic acid levels or 200 mg if the criterion was the intake level at which the efficiency of utilization began to decline or was sufficient to promote a plasma concentration of vitamin C that is near to maximal and above the Km of the membrane, sodium-dependent ascorbic acid transporter (3). Further, some concerns might be raised about the sequential dosing protocol used by Levine et al. (3) and whether this experimental design might have biased the outcome. Results from the recent 13C-ascorbic acid compartment tracer model study by Bluck et al. (8) suggest that intakes of ascorbic acid below those found by Levine et al. (3) would be sufficient to insure mass balance of ascorbic acid at the cellular level.
Levine et al. (9, 10) had earlier made an argument for estimating requirements based on “in situ kinetics.” They hypothesized that ideal cell function is equivalent to a state of maximal rates of synthesis and, with reference to the specific intracellular functions of ascorbic acid, it was implied that this is achieved by maintaining plasma and intracellular concentrations of ascorbic acid at levels that would require intakes of vitamin C much higher than the current 60 mg RDA level. The validity of their proposition that an optimum vitamin C concentration would be that at which Vmax for a particular reaction was reached remains unproven (10). Most enzyme systems operate at rates far below their Vmax, where substrate availability in healthy organisms is not the limiting factor, and a specific rationale for choosing, in the present case, a value of 200 mg daily was not presented by Levine and his colleagues (3). However, as noted below, it becomes extremely important to make a sound and scientifically established case for the choice of the criterion of nutritional adequacy because of the potentially major impact of the recommendation on nutrition policy. This point concerning the importance of the target level of nutritional status has been emphasized well by Beaton (7). In sum, before a measure or indicator such as a tissue saturation level of vitamin C is accepted as a basis for estimating an average nutrient requirement, it is necessary to establish that there is a direct link between that indicator and an observed health benefit to the individual.
Mean Requirement and Variability
To establish a dietary allowance for a nutrient, such as an RDA, it has been the practice to estimate both the average of individual requirements for the nutrient in a given population/age or physiological group and the variability in the requirement among individuals within the group. For example, in setting the RDA for protein, the FNB/NRC (1) took the average requirement for adults to be 0.6 g protein per kg of body weight per day and accepted a coefficient of variation of 12.5% to account for the requirement differences among individuals. Thus, the RDA was set at 2 SDs above the average requirement, or 0.75 g protein per kg per day. However, for most essential nutrients there are insufficient data to establish precisely the extent of this variation or even whether it is normally distributed. The 60 mg daily RDA proposed by FNB/NRC (1) for ascorbic acid was considered to provide an adequate margin of safety but the variance in the vitamin C requirement among individuals was not stated specifically in the 1989 report. It would be reasonable, however, to assume that the coefficient of variation for the requirement was about 15%, using the variation in basal energy needs and in protein requirements (11) as rough guides. This would mean, therefore, that the 1989 FNB/NRC unspecified average ascorbic acid requirement was assumed to be about 46 mg daily, yielding an RDA close to 60 mg daily [46+ (2 × 6.9)].
A New Average Requirement or RDA for Ascorbic Acid
Given the design of the studies by Levine et al. (3), the 200 mg value proposed might be seen as an estimate of the average requirement to meet the criterion specified above rather then as an RDA (average + allowance for variability of requirement) in terms of previous FNB practice. I shall consider the consequences of both assumptions in the analysis that follows. In addition, for illustrative purposes, I will also use a value of 100 mg daily as being either an average requirement value or an RDA, in this same context. This 100 mg intake level was chosen for comparison here in the analysis because, as noted above, it promoted maximum intracellular vitamin C concentrations in circulating immune cells. This choice, however, should not be taken to imply that it has a functional significance—it merely helps to illustrate a number of points below. Finally, in keeping with the observed variation in many biological systems, it is assumed that a coefficient of variance of 15% can be taken as a reasonable estimate of the variation in ascorbic acid requirement among individuals, such as for the seven subjects as studied by Levine et al. (3). It follows, therefore, that there are four requirement (mg ascorbic acid daily) models that might be derived from Levine et al. (3), in addition to the one that emerges from the 1989 RDA report (1); these are summarized in Table 1. Thus, there is an apparent 4-fold range in average requirement estimates for ascorbic acid depending upon the criterion of adequacy used for this purpose. One way of comparing these different requirement distributions is to apply them to a representative sample of a large population and determine what would be the implied nutritional situation of that population.
Table 1.
Five possible models of ascorbic acid requirements
| Source (ref.) | Mean requirement, mg per day | SD of requirement, mg per day | RDA*, mg per day | Criteria used for nutritional adequacy |
|---|---|---|---|---|
| 1989 FNB/NRC (1) | 46 | 7 | 60 | Depletion rate and turnover at |
| a pool size of 1500 mg; 85% | ||||
| absorption at usual intake. | ||||
| Levine et al. (3) | ||||
| Model 1 | 77 | 11.5 | 100 | Monocyte and lymphocyte |
| Model 2 | 100 | 15 | 130 | maximum ascorbic acid |
| concentration. | ||||
| Model 3 | 154 | 23 | 200 | Bioavailability; plasma |
| ascorbic acid concentration; | ||||
| Model 4 | 200 | 30 | 260 | considerations of vitamin C |
| function. |
RDA taken to be the mean requirement + 2 SD of requirement.
Relationship Between Proposed RDA and Diet Intakes in a Healthy Population
To undertake this practical examination of the implications of the recommendations by Levine et al. (3), I present assessments of the implied prevalence of intakes too low to be expected to meet the individual’s need for ascorbic acid. These assessments are based on intakes reported for adult men, 20–50 years old, as reported in the First National Intake Survey in the Netherlands (12) and in the 1994 data of the current U.S. Department of Agriculture Continuing Study of Food Intake by Individuals (13). Repeated 24-hr dietary recall methods were used in both surveys. Both surveys used stratified random sampling procedures to identify representative samples of households from which the subjects were selected. Given recent concern about possible bias to underestimation in reported intakes (14–16), a check was made for such bias in both data sets. For each individual, reported (2-day average) energy intake was divided by the basal metabolic rate calculated using FAO/WHO/UNU equations (11). The mean ratio for Dutch men was 1.58 and for U.S. men was 1.48. The value seen for the Netherlands was about what would be expected in an industrialized country setting with modest-to-light levels of physical activity. These checks suggest that the Dutch data set did not suffer major underreporting bias. The U.S. data may suffer some degree of such bias but it does not appear to be as great as had been suggested for earlier data sets. It was concluded that assessments could proceed usefully for both data sets (14–16). As a first step in analysis of the ascorbic acid intake data, the distribution of reported intakes for each population was converted to an estimated distribution of usual intakes using the approach developed at Iowa State University (17). The adjusted distributions are portrayed in Fig. 1. It should be noted that as a result of this analysis and in comparison to the original distributions of 2-day means, the distributions were narrowed, but remained broad and definitely skewed.
Figure 1.
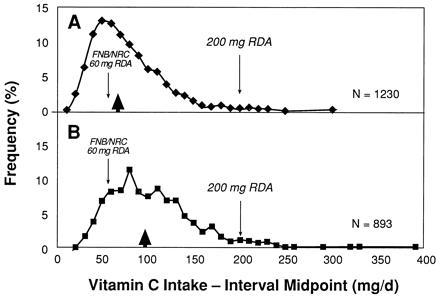
Histograms of estimated distributions of usual intakes of vitamin C (mg per day) among adult men 20–50 years of age living in the Netherlands (A) or in the United States (B). Median intakes are marked by the arrowheads. Data were taken from ref. 12 and from the most recent U.S. Department of Agriculture Continuing Study of Food Intake by Individuals (CSFII-1994) (13). Reported intake data were adjusted by the method developed at Iowa State University (17) to estimate the distributions of usual intakes. Intake intervals were set at 10 mg per day and they have been joined for presentation purposes. The 60 mg RDA recommended by FNB/NRC and the 200 mg RDA proposed by Levine et al. (3) are shown within each distribution.
A summary of the univariate statistics for usual ascorbic acid intakes in the two adjusted data sets is given in Table 2. Neither data set includes ascorbic acid that may have been ingested from pharmaceutical preparations. That would impact heavily in an examination of possible excessive intakes but it does not impact in a serious way on the examples of the dietary and food implications of varying requirement estimates presented below.
Table 2.
A statistical summary of usual intakes of vitamin C in populations of adult Dutch and U.S. men
| Statistic | Dutch | U.S. |
|---|---|---|
| Number | 1230 | 893 |
| Intake, mg per day | ||
| Mean | 75.6 | 104.4 |
| SD | 37.0 | 47.2 |
| Median | 68.0 | 96.7 |
| Centiles | ||
| 1st | 20.1 | 30.4 |
| 5th | 29.8 | 43.3 |
| 10th | 36.0 | 51.9 |
| 25th | 49.0 | 70.7 |
| 75th | 95.2 | 128.8 |
| 90th | 123.5 | 168.0 |
| 95th | 142.8 | 192.5 |
| 99th | 197.9 | 238.5 |
The five requirement models shown in Table 1 were then applied to the estimated distribution of usual intakes that are described in Table 2 and portrayed in Fig. 1. This was first done using the full probability approach described in the National Academy of Sciences report on nutrient adequacy (18). The exercise was then repeated using the much simpler approach identified, but not promoted, in that report, namely, estimation of the proportion of individuals with intakes below the average requirement. Both of these approaches yield empirically very similar estimates of the proportion of individuals whose usual ascorbic acid intake is below their own true (but unknown except on a probability basis) requirement. The estimated prevalences of “apparently inadequate intakes” results are shown in Table 3.
Table 3.
Estimated prevalence of inadequate intakes of vitamin C as a function of assumed requirement distribution in the Dutch and U.S. adult male populations
| Requirement distribution* | % estimated prevalence of inadequate
intakes†
|
|
|---|---|---|
| Dutch | U.S. | |
| Existing U.S. RDA (1) | 21.7 | 6.8 |
| Levine et al. (3) | ||
| Model 1 | 59.1 | 31.8 |
| Model 2 | 77.2 | 52.2 |
| Model 3 | 96.7 | 84.3 |
| Model 4 | 99.0 | 94.4 |
See Table 1 for description of requirement distributions.
Estimated as proportion of respective population group with intakes below mean requirement; full probability assessment gave similar estimates (see text).
From the analysis presented in Table 3 and in reference to the problems associated with the choice of the criterion of nutritional adequacy that were discussed above, it would appear that all of the requirement estimates, given in Table 1, could be higher than actually necessary or at least this might seem to be the case if the requirement estimates are intended to relate to maintenance of some clinically detectable function (i.e., the Basal requirement concept). However, the low-to-moderate prevalence of inadequacy, based on the current RDA of 60 mg, seems to be consistent with the fact that neither population is believed to manifest frequent signs of functional vitamin C inadequacy. If the criterion of requirement is not intended to relate to clinically detectable functions (i.e., the Normative requirement concept) but rather based, for example, on saturation kinetics, then one is faced with the difficult problem: how far should one go in recommending levels that might have some benefit in some situation for some individuals but for which there is present lack of necessary documentation linking the criterion with a functional/health outcome?
Consider, then, the public health implications of the five requirement models in Table 1. If the requirement estimates as suggested from the data of Levine et al. (3) are accepted, then it would be concluded that 59% to 99% of the population of adult Dutch men should increase their vitamin C intakes and, similarly, this would apply to from 32% to 94% of U.S. men. It is suggested that there is an implicit obligation of committees and expert groups publishing requirement estimates and recommended intakes to ask the question: “Is such an action justified from the standpoint of the public health?” If they are not convinced that such an action should follow from the recommendation, a careful reconsideration of the criteria and evidence used in establishing the recommendations is appropriate.
It is appreciated that epidemiological data have shown a mostly indirect association of vitamin C with cancers and with atherosclerosis and coronary heart disease (19–21), and Levine et al. (3) point out that the 200 mg dose of ascorbic acid might prevent formation of harmful N-nitroso compounds in the gastrointestinal tract (22) and/or produce a plasma concentration that might inhibit low density lipoprotein oxidation (23, 24). Various experts have indicated that this latter function is largely speculative at this stage in our knowledge, at least with reference to the causation and progression of atherosclerosis in the U.S. population (19, 23–25). Certainly, it is now important to determine further whether there is a sufficient data base from which to estimate specific nutrient intake levels, including ascorbic acid, that might lower risk of chronic disease. It should be pointed out, however, that the values for the necessary mean population intakes, discussed below, are concerned with requirements that are measured in terms of physiological or pharmacokinetic responses and not on the basis of any causally quantitative associations between dietary nutrient levels and chronic disease. Thus, the requirement estimates examined here do not address this latter area of ascorbic acid function and its possible role in health maintenance. I should emphasize that if substantial and quantitatively reliable evidence were at hand that a particular ascorbic acid intake level, which was higher than that currently recommended or the prevailing mean population intake, reduced the incidence of a form of cancer, for example, then this might well be the basis for a new or revised set of recommended values for the vitamin C intakes of individuals and specific population groups.
Reducing a “Population Risk” of Inadequate Intakes to Meet Physiological Needs
From the foregoing analysis of predicted prevalence of intakes that are inadequate to meet the physiological/pharmacokinetic criteria of nutritional adequacy defined above, it is now worth considering what population mean vitamin C intake level would be needed to lower the population risk of inadequacy of intake to a level of 5% or even 1%. Thus, if it can be assumed that the shape of the intake distribution remains unchanged, to achieve a population risk of inadequate intakes as low as 5% then the 5th centile of intake would have to approximate the determined mean requirement. Similarly, for a 1% risk, the 1st centile of intake would have to approximate the mean requirement.
In the estimated distribution of usual intakes described above (Table 2), the 5th centile for the Dutch population was 45.8 mg below the average intake; it follows, then, that the intake distribution would have to shift upward by this amount (mean intake = 46 + 45.8) to about 92 mg per day to achieve a population risk of 5% if average requirement was taken to be 46 mg per day. The population mean intake would have to be 246 mg if the average requirement were taken as 200 mg per day. Similar calculations can be made for a 1% population risk; here, separation between 1st centile and mean intake was 55.5 mg per day for the Dutch men. These estimates, together with comparable ones for the U.S. population, are also summarized in Table 4.
Table 4.
Predicted population mean intakes to achieve defined population risk levels—A portrayal of possible policy implications
| Average nutrient requirement as derived from postulated RDAs, mg per day | Necessary group mean intake, mg per day
|
|||
|---|---|---|---|---|
| For population risk = 5%
|
For population
risk = 1%
|
|||
| Dutch | U.S. | Dutch | U.S. | |
| 1989 FNB/NRC, 46 | 92 | 107 | 101 | 120 |
| Model 1, 77 | 123 | 138 | 132 | 151 |
| Model 2, 100 | 146 | 161 | 155 | 174 |
| Model 3, 154 | 200 | 215 | 209 | 228 |
| Model 4, 200 | 246 | 261 | 255 | 274 |
Existing group mean intakes are 75.6 mg per day and 104 mg per day for Dutch and U.S. adult male populations, respectively.
Therefore, if one of the five separate requirement estimates used above were adopted as a matter of public health policy, it would necessitate, depending upon the population, increasing existing intakes by a modest amount, of approximately a quarter above usual intakes up to an approximate 3-fold rise above these intakes. These represent significant and even profound changes from current dietary practice by the population as a whole. Increasing the intake of ascorbic acid to the level recommended by Levine et al. (3) is feasible on an individual basis but at the entire population level this matter is far more complex. Depending upon food choices, it is possible to obtain about 200 mg ascorbic acid with four or five servings of fruits and vegetables, although relatively few American adults actually consume this number of servings (26). Because, at least for the U.S., approximately 38% of the ascorbic acid in the food supply is provided by citrus fruits, 16% by potatoes, and 30% from other vegetables (1), it must to be appreciated that a desirable 2-fold increase in the level of ascorbic in the diet, for example, would have both significant structural and, possibly, economic implications for the pattern of agriculture and the qualitative character of the U.S. food production and processing system. Indeed, if common food sources of vitamin C were insufficient, in terms of supply and use, to provide for the necessary intakes of ascorbic acid, then pharmaceutical supplements would have to be recommended for the population as a means of assuring adequate levels of intake. In this context, some have also cautioned that intakes at the higher end of the levels shown in Table 4 may have untoward effects (27), although there is a great deal of uncertainty about how high an intake of ascorbic acid would have to be to cause significant harm.
Application of the probability approach to individuals used here for estimating the proportion of the population at risk of “inadequate” intakes from dietary survey data has been criticized as being premature, in part, because of the gross errors that are involved in accurately estimating usual food intake of individuals and in estimating the precise nature of requirement distributions (28). Many of the criticisms of the probability assessment are fully justified when discussing its application to a particular individual (7). Fortunately, however, many of the criticisms, except those relating to possible overall bias in underestimation of total food intake (14–16), are greatly diminished when group rather than individual assessments are performed (7, 29, 30) after adjustment of observed intakes to estimate the distribution of usual intakes (16). Hence, it seems to me that it is highly instructive to apply this approach in the present context, where the major concern is for the rationale and choice of a nutrient requirement estimate, especially when considered in relation to two population groups in which a functional or clinically significant ascorbic acid inadequacy has not been shown to be a current major public health problem. It is also worth stressing, once again, that my purpose here is not to attempt to assess nutritional status from dietary data but rather to underscore the importance of carefully documenting the link between the criteria of adequacy used to establish requirements and measurable functional outcomes or health benefits for the populations concerned.
The above considerations need to be taken into account in assessing the appropriateness of the recommendation by Levine et al. (3). Only in this way can a sound judgment be reached on the RDA for ascorbic acid for use by healthy policy makers and for the design of effective national nutrition programs. Regardless of what policy decisions are made, it is essential that the requirement values provided for this purpose are based on rigorous scientific evidence and critical thought.
Acknowledgments
The analysis of the dietary survey data was undertaken with the considerable assistance of Dr. George H. Beaton, to whom I am deeply grateful and also for his valuable comments on earlier drafts of this paper. I also appreciate the permission I was granted to use the data obtained from the First National Food Intake Survey, conducted in the Netherlands during the period April 1987 to March 1988.
Footnotes
Abbreviations: RDA, recommended dietary allowance; FNB/NRC, Food and Nutrition Board/National Research Council; WHO/FAO/IAEA, World Health Organization/Food and Agriculture Organization/International Atomic Energy Agency.
References
- 1.FNB/NRC. Recommended Dietary Allowances. Tenth Revised Edition; Food and Nutrition Board. Washington, DC: Natl. Acad. Press; 1989. [Google Scholar]
- 2.FNB/NRC. Recommended Dietary Allowances. Ninth Revised Edition; Food and Nutrition Board. Washington, DC: Natl. Acad. Press; 1980. [Google Scholar]
- 3.Levine M, Conry-Cantilena C, Wang Y, Welch R W, Washko P W, Dhariwal K P, Park J B, Lazarev A, Graumlich J F, King J, Cantilena L R. Proc Natl Acad Sci USA. 1996;93:3704–3709. doi: 10.1073/pnas.93.8.3704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brody, J. E. New York Times April 16, 1996, pp. C1 and C3.
- 5.WHO. Trace Elements in Human Nutrition and Health. Geneva: W.H.O.; 1996. pp. 1–343. [Google Scholar]
- 6.FAO/WHO (1988) Requirements for Vitamin A, Iron, Folate and Vitamin B12: Report of a Joint FAO/WHO Expert Consultation, FAO Food and Nutrition Series No. 23 (Food Agric. Org. U.N., Rome), pp. 1–107.
- 7.Beaton G H. In: Modern Nutrition in Health and Disease. 8th Ed. Shils M E, Olson J A, Shike M, editors. Vol. 2. Philadelphia: Lea & Febiger; 1993. pp. 1491–1505. [Google Scholar]
- 8.Bluck L J C, Issard A P, Bates C J. J Mass Spectrom. 1996;31:741–748. doi: 10.1002/(SICI)1096-9888(199607)31:7<741::AID-JMS352>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 9.Levine, M., Dhariwal, K. R., Washko, P. W., Welch, R. W. & Wang, Y. (1993) Asia Pac. J. Clin. Nutr. 2, Suppl. 1, S5–S13. [PubMed]
- 10.Levine, M., Dhariwal, K. R., Welch, R. W., Wang, Y. & Park, J. B. (1995) Am. J. Clin. Nutr. 62, Suppl., 1347S–1356S. [DOI] [PubMed]
- 11.FAO/WHO/UNU. Energy and Protein Requirements. Report of a Joint FAO/WHO/UNU Expert Consultation. Geneva: W.H.O.; 1985. Technical Report Series No. 7241206. [PubMed] [Google Scholar]
- 12.Hushof K F A M, von Staveren W A. Food Policy. 1991;16:257–260. [Google Scholar]
- 13.Agriculture Research Service. Continuing Study of Food Intake by Individuals 1994–96. Washington, DC: U. S. Department of Agriculture; 1996. 1994 data distribution on CD-ROMreleased January1996. [Google Scholar]
- 14.Dwyer J T. In: Modern Nutrition in Health and Disease. 8th Ed. Shils M E, Olson J A, Shike M, editors. Vol. 1. Philadelphia: Lea & Febiger; 1993. pp. 842–860. [Google Scholar]
- 15.Shoeller D A. Nutr Rev. 1990;48:373–379. doi: 10.1111/j.1753-4887.1990.tb02882.x. [DOI] [PubMed] [Google Scholar]
- 16.Mertz W, Tsui J C, Judd J T, Reiser S, Hallfrisch J, Morris E R, Steele P C, Lashley E. Am J Clin Nutr. 1991;54:291–295. doi: 10.1093/ajcn/54.2.291. [DOI] [PubMed] [Google Scholar]
- 17.Nasser, S. M., Carriquiry, A. L., Dodd, K. W. & Fuller, S. M. (1996) J. Am. Stat. Assoc., in press.
- 18.FNB/NRC. Nutrient Adequacy: Assessment Using Food Consumption Surveys. Washington, DC: Natl. Acad. Press; 1986. pp. 1–146. pages. [PubMed] [Google Scholar]
- 19.FNB/NRC. Diet and Health. Washington, DC: Natl. Acad. Press; 1989. pp. 1–749. [Google Scholar]
- 20.Gutteridge J M C, Halliwell B. Antioxidants in Nutrition, Health and Disease. Oxford: Oxford Univ. Press; 1994. pp. 1–143. [Google Scholar]
- 21.Gershoff S N. Nutr Rev. 1993;51:313–326. doi: 10.1111/j.1753-4887.1993.tb03757.x. [DOI] [PubMed] [Google Scholar]
- 22.Tannenbaum S K, Mergens W. Ann NY Acad Sci. 1980;355:267–279. doi: 10.1111/j.1749-6632.1980.tb21345.x. [DOI] [PubMed] [Google Scholar]
- 23.Steinberg D. N Engl J Med. 1993;20:1487–1489. doi: 10.1056/NEJM199305203282012. [DOI] [PubMed] [Google Scholar]
- 24.Kushi L H, Folson A R, Prineas R J, Mink P J, Yu Y, Bostick R M. N Engl J Med. 1996;334:1156–1162. doi: 10.1056/NEJM199605023341803. [DOI] [PubMed] [Google Scholar]
- 25.Greenberg E R, Sporn M B. N Engl J Med. 1996;334:1189–1190. doi: 10.1056/NEJM199605023341810. [DOI] [PubMed] [Google Scholar]
- 26.Krebs-Smith S M, Cook A, Subar A F, Cleveland M S, Friday J. Am J Public Health. 1995;85:1623–1629. doi: 10.2105/ajph.85.12.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Herbert V, Shaw S, Jayatilleki E. J Nutr. 1996;126:1213S–1220S. doi: 10.1093/jn/126.7.1902b. [DOI] [PubMed] [Google Scholar]
- 28.Hegsted D M. Nutrient Adequacy. Washington, DC: Natl. Acad. Press; 1986. pp. 104–109. [Google Scholar]
- 29.Beaton, G. H., Burema, J. & Ritenbaugh, C. (1996) Am. J. Clin. Nutr., in press. [DOI] [PubMed]
- 30.Beaton G H. J Nutr. 1996;126:2320S–2328S. doi: 10.1093/jn/126.suppl_9.2320S. [DOI] [PubMed] [Google Scholar]


