Abstract
Background
The 2005 Emergency Cardiac Care guidelines for basic life support (BLS) recommend a compression to ventilation ratio of 30:2. The effect of the additional exertion required to deliver more chest compressions may present a considerable physical burden on the provider.
Objective
To compare cardiopulmonary resuscitation (CPR) performance and perceived exertion during compression to ventilation ratios of 15:2 and 30:2 with real-time feedback during two-rescuer CPR.
Methods
Eighteen BLS-certified healthcare providers each performed five minutes of chest compressions on a manikin with compression to ventilation ratios of 15:2 or 30:2 on two separate sessions. Heart rate, capillary lactate, and OMNI Rate of Perceived Exertion (RPE) were recorded before and after each session. Subjects were given continuous, automated, feedback via an accelerometer that measured rate, depth, duration, and release of compressions. Compression measurements and feedback messages were recorded continuously during each five minute session. Data were analyzed using descriptive statistics and t-test to compare groups. Repeated measures ANOVA was used to compare data over the five minute epoch.
Results
After performing external chest compressions for five minutes, peak heart rate (102±24 vs. 106±27), capillary lactate (2.2±0.95 vs. 2.2±0.96), and OMNI RPE (4.3±1.2 vs. 4.6±1.1) were higher were higher than baseline, but did not differ between 15:2 and 30:2. Compression rate (102 ± 24 vs.106 ± 27) and depth (38.8±3.6 vs. 38.2±2.9) did not differ between 15:2 and 30:2 groups or at any minute. Total chest compressions delivered were higher (p<0.05) in the 30:2 group (457±43) compared to 15:2 (379±28). The average no flow time was lower (p<0.05) in the 30:2 group (22±3.03) compared to the 15:2 group (33±2.64). Number of correction prompts (48±55 vs. 64±70) did not differ significantly between the 15:2 and 30:2 groups.
Conclusions
In a cohort of healthcare providers, increasing the CPR ratio from 15:2 to 30:2 did not change physical or perceived exertion during a five-minute bout of CPR when continuous, real-time feedback is provided. The 30:2 compression to ventilation ratio resulted in more chest compressions per minute without decreasing CPR quality.
Keywords: Cardiopulmonary resuscitation, Guidelines, Compression to ventilation ratio, Manikin, Healthcare provider, Lactate
Introduction
Cardiac arrest occurs outside of the hospital in approximately 1 of every 1000 persons per year. Overall survival from cardiac arrest continues to be low, with only 6−7% of persons who collapse outside of the hospital surviving to hospital discharge. 1 Recent data have suggested that inadequate performance of CPR may hinder the success of resuscitation efforts. 2 Chest compressions are necessary to generate coronary perfusion pressure, thus increasing the likelihood of return of spontaneous circulation (ROSC) during resuscitation efforts. 3 Interrupting chest compressions results in a rapid decline of CPP. 4 The Guidelines 2005 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care increased the chest compression to ventilation ratio from 15:2 to 30:2 to minimize no flow time (NFT). 5
The quality of chest compressions is important for successful resuscitation. Inadequate rate and depth of compression as well as insufficient recoil have been implicated in poor quality CPR. 6 Another reason for ineffective chest compressions is rescuer fatigue. 7, 8 Within 1−2 minutes, the quality of chest compressions decreases. 7 Moreover, rescuers are unaware of their decrease in performance. 8 Prior studies on rescuer fatigue have been limited by not controlling the quality of chest compressions provided, and using the previous compression to ventilation ratio of 15:2. When CPR providers are held to the parameters of the new CPR guidelines, the effect of additional work on the provider and the quality of CPR is unknown.
To date, the few studies that have explored the perceived amount of work necessary to provide quality CPR under the 2005 guidelines have not provided CPR quality feedback to providers.9-13 Prior research has demonstrated that real-time feedback improves CPR quality.14,15 We hypothesize that performance of CPR using the new guidelines and with the provision of real-time feedback will increase rescuer work and require more correction prompts during a five minute bout of CPR. We compared healthcare provider CPR performance and perceived exertion during compression to ventilation ratios of 15:2 and 30:2 with real-time feedback.
Materials and Methods
Subjects
The University of Pittsburgh Institutional Review Board approved this study and each subject provided informed consent. All subjects were BLS-certified healthcare providers. Subjects included physicians, paramedics and emergency medical technicians.
Protocol and Data collection
This was a prospective, randomized, cross-over study examining external chest compression performance and physical exertion of the provider during two-rescuer CPR. Subjects performed five minutes of chest compressions on a manikin with compression to ventilation ratios of 15:2 or 30:2 on two separate sessions. An investigator provided ventilations with a bag-valve mask device. Following the completion of CPR subjects rested quietly in the lab for five minutes.
Participants performed external chest compressions for five minutes on a CPR manikin (Laerdal Resusci Anne, Stavanger, Norway) placed on the floor. The manikin chest recoil spring was replaced with a stiffer prototype provided by Laerdal to impart more realistic chest compliance. Participants counted the number of compressions out loud. While performing compressions, subjects were given continuous, automated, feedback for rate, depth, duration, and release of compressions.
Feedback was provided by a Philips HeartStart MRx Monitor/Defibrillator (Philips Electronics, New York, NY) with Q-CPR feedback technology (Laerdal, Stavanger, Norway) based on measurements recorded by the Q-CPR Compression Sensor placed on the manikin's chest and connected to the monitor. Correction prompts included “incomplete release,” “release pressure,” “compress deeper,” “increase duration,” “press faster,” and “press slower.” The feedback prompts served to optimize compression rate at 100 compressions per minute and a depth of 38−51 mm.5 Compression measurements and feedback messages were recorded continuously during each five minute session for later download and analysis. After a minimum rest period of one hour, subjects performed external chest compressions for five minutes in the alternate condition.
Prior to performing CPR, a CardioSport heart rate monitor (Polar Electro Oy, Sweden) was secured around the subject's chest. Heart rate was recorded at baseline, the completion of CPR, and five minutes following CPR completion. Capillary blood lactate was drawn from the fingertip using a lancet (Becton Dickinson, Franklin Lakes, NJ), Lactate Plus test strip and meter (Nova Biomedical, Waltham, MA) with aseptic technique at baseline and five minutes following CPR completion. This time epoch was chosen to allow time for intramuscular lactate to enter the blood stream.16 The subject rated perceived exertion using the OMNI Run-Walk RPE scale, a scale of perceived effort anchored by 0 ‘extremely easy’ to 10 ‘extremely hard’.17 The scale was explained to the subject by an investigator prior to beginning the study. OMNI RPE measurements were obtained prior to CPR, immediately following the completion of CPR, and five minutes after CPR completion.
Statistical Analysis
Data were analyzed using descriptive statistics and t-test to compare groups. A sample size of 18 was targeted to detect a 1.5 absolute difference in the OMNI RPE between the study groups with a power of 0.90. This sample size would also allow us to detect a doubling of venous lactate between the baseline measurement and the post-CPR measurement. The unpaired Student's t-test was used to compare performance variables and correction prompts between the 15:2 and 30:2 compression to ventilation groups. Repeated measures ANOVA was used to analyze performance variables during each minute of the study. Analyses were considered significant when alpha ≤ 0.05.
Results
Eighteen CPR-certified healthcare providers completed the study. Demographics are shown in Table 1. All subjects were experienced CPR providers with a mean of 11.1 ± 6.79 years of experience (range: 1 to 24 years).
Table 1.
Subject Demographics
| Mean (SD) | Minimum | Maximum | |
|---|---|---|---|
| Age (yr) | 31.1 (8.0) | 21 | 57 |
| Height (in) | 69.7 (3.55) | 64 | 76 |
| Weight (lb) | 176.28 (30.62) | 130 | 240 |
| BMI | 25.46 (3.59) | 21.3 | 32.5 |
| Years of CPR training | 11 (6.79) | 1 | 24 |
| Gender (% male) | 78 |
Physiology and Perceived Exertion
After five minutes of compressions, heart rate, lactate, and OMNI RPE were increased but these outcomes did not differ between the 15:2 and 30:2 groups (Table 2).
Table 2.
Physiologic variables and perceived exertion. Values are mean (SD).
| 15:2 Pre | 15:2 Post | 30:2 Pre | 20:2 Post | |
|---|---|---|---|---|
| HR (beats / min)) | 77 (14) | 102 (24) | 76 (14) | 106 (27) |
| Lactate (mmol/L) | 1.4 (0.44) | 2.2 (0.95) | 1.4 (0.51) | 2.2 (0.96) |
| OMNI | 0.11 (0.5) | 4.3 (1.2) | 0.22 (0.7) | 4.6 (1.1) |
Compressions
Compression data are shown in Table 3. Rate and depth of compression did not differ significantly between the 15:2 and 30:2 groups or during any minute of CPR. Number of compressions with incomplete release did not differ between the 15:2 and 30:2 groups. Percentage of compressions with adequate depth was not different between the two groups. Total number of compressions was higher with 30:2 compared to 15:2. The overall NFT was lower in the 30:2 group compared to the 15:2 group.
Table 3.
Compressions and correction prompts. Values are mean (SD).
| 15:2 (SD) | 30:2 (SD) | |
|---|---|---|
| Rate (per minute) | 105 (8.4) | 109 (10) |
| Depth (mm) | 38.8 (3.6) | 38.2 (2.9) |
| Adequate depth (%) | 63 (37) | 56 (36) |
| Incomplete release | 33 (55) | 47 (69) |
| Correction prompts | 48 (55) | 64 (70) |
| Total compressions | 379 (28) | 457 (43) * |
| Total no flow time (%) | 33 (2.7) | 22 (3.0) * |
p<0.05 compared to 15:2 group
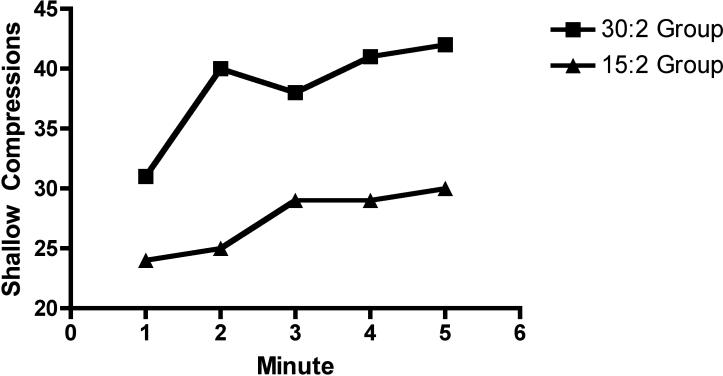
When analyzing by minute, the NFT was significantly lower in the 30:2 group (p<0.001; Figure 1). The 30:2 group received more compressions per minute but more compressions were too shallow (p=0.007, p=0.02; Figure 1). Compression depth was not different between groups (p>0.05). None of the measurements significantly differed over time.
Figure 1.
A. No flow time (%) by group. (p<0.001 for comparison between groups)
B. Compressions per minute by group. (p=0.007 between groups)
C. Shallow compressions per minute by group. (p=0.02 between groups)
D. Compression depth (mm) by group.
Correction Prompts
The number of correction prompts provided during CPR did not differ between the 15:2 and 30:2 groups or during any minute of CPR (Table 3).
Discussion
The results of this study demonstrate that in healthcare providers performing external chest compressions, a compression to ventilation ratio of 30:2 leads to a greater total number of compressions over five minutes and a lower proportion of time without chest compressions when real-time feedback is provided. We also noted a lower NFT in the 30:2 group. This supports prior research. 9-12 Moreover, with the provision of real-time feedback, the number of correct compressions and compression rate and depth did not differ between the two groups in our study. However, the 30:2 group did note more compressions that were deemed too shallow. Given the overall increase in compressions, the clinical effect of this finding is unclear. Overall, our data refute the hypothesis that increasing the rate of compressions to ventilations increases rescuer work and decreases CPR quality.
It has been previously established that prolonged time spent without chest compressions for ventilations, pulse checks, and other procedures results in a large fraction of time during resuscitation without chest compressions. 4, 6 The goal of the AHA guideline change to increase the compression to ventilation ratio emphasizes the importance of compressions, and to decrease time without chest compressions. This study, along with our prior clinical work demonstrates that increasing the compression to ventilation ratio in the prehospital setting improves the delivery of compressions, and improves return of spontaneous circulation (ROSC). 10
Importantly, peak heart rate, capillary lactate, and OMNI RPE did not differ between the 15:2 and 30:2 ratios. Prior studies have evaluated the effect of various CPR bouts on heart rate and perceived fatigue as measured on a Likert, visual analog scale (VAS), or Borg RPE. 9,11,13 Deschilder and Bridgewater describe an increase in perceived exertion by subjects as measured with the VAS and Borg scales, respectively. 11,13 One potential reason for the difference between their results and ours may be that Bridgewater examined a time period of ten minutes and concluded that the length of the fitness test should be reduced. 13 Deschilder also detected a small difference in perceived exertion. 11 However, both groups had adequate mean depth of compression, suggesting that increased effort by the providers may not be clinically relevant. Heart rate and lactate were not monitored in that study.
Distinctly different from prior studies, the subjects in our study were given real-time continuous feedback with correction prompts based on their specific compression performance. The purpose of the feedback was to encourage subjects to perform correct compressions varying only the compression to ventilation ratio. Previous studies have shown that real-time feedback during CPR performance improves the delivery of ventilations and chest compressions and have led to the development of therapeutic devices that deliver CPR performance prompts.14,15 Bridgewater provided intermittent feedback to subjects regarding their compressions per minute, but did not provide continuous correction prompts related to depth, rate or recoil. 13 Odegaard did not provide feedback to their lay person subjects. 12
There are several limitations to this study. First, we used healthcare providers as subjects and did not evaluate the lay rescuer population. This is relevant to our system, for most victims of cardiac arrest do not receive bystander CPR. 10 However, a lay rescuer may be less fit and suffer significant physical strain when performing a higher compression to ventilation ratio. Second, we did not evaluate heart rate, lactate, or exertion continuously during each five minute bout of compressions. We utilized a two-rescuer model where the subject provided compressions and ventilations were done by an investigator with the bag-valve-mask. This may have led to a more optimal setting for the subject to concentrate on chest compressions. We have previously noted that rescuers perform CPR less efficiently as more tasks are given to them. 18 Finally, this was a simulated resuscitation and may not represent the austere environment faced by many prehospital rescuers.
Conclusions
Increasing the compression to ventilation ratio from 15:2 to 30:2 did not change rescuer effort or perceived exertion in a cohort of healthcare providers during a five-minute bout of CPR when continuous feedback is provided. The 30:2 compression to ventilation ratio produced more chest compressions per minute and less time without chest compressions without decreasing CPR quality.
Supplementary Material
Acknowledgments
Laerdal medical (Stavanger, Norway) provided the prototype manikin for this study. Dr. Rittenberger is supported by Grant Number 1 KL2 RR024154-02 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Dr. Rittenberger is also supported by an unrestricted grant from the National Association of EMS Physicians/Zoll EMS Resuscitation Research Fellowship.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors have no conflict of interest to report.
References
- 1.Nichol G, Stiell IG, Laupacis A, Pham B, DeMaio VJ, Wells GA. A cumulative meta-analysis of the effectiveness of defibrillator-capable emergency medical services for victims of out-of-hospital cardiac arrest. Ann Emerg Med. 1999;24:517–25. [PubMed] [Google Scholar]
- 2.Wik L, Kramer-Johansen J, Myklebust H, et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293:299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- 3.Paradis NA, Martin GB, Rivers EP, et al. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA. 1990;263:1106–13. [PubMed] [Google Scholar]
- 4.Berg RA, Hilwig RW, Ewy GA, Kern KB. Precountershock cardiopulmonary resuscitation improves initial response to defibrillation from prolonged ventricular fibrillation: a randomized, controlled swine study. Crit Care Med. 2004;32:1352–7. doi: 10.1097/01.ccm.0000127780.01362.e5. [DOI] [PubMed] [Google Scholar]
- 5.ECC committee, subcommittees and task forces of the American Heart Association American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiac care. Circulation. 2005;2005;112(Suppl):IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 6.Kramer-Johansen J, Edelson D, Abella B, Becker L, Wik L, Steen P. Pauses in chest compression and inappropriate shocks: A comparison of manual and semi-automatic defibrillation attempts. Resuscitation. 73(2):212–220. doi: 10.1016/j.resuscitation.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Hightower D, Thomas SH, Stone CK, Dunn K, March JA. Decay in Quality of Closed-Chest Compressions Over Time. Annals of Emergency Medicine. 1995 September;26(3):300–303. doi: 10.1016/s0196-0644(95)70076-5. [DOI] [PubMed] [Google Scholar]
- 8.Ochoa FJ, Ramalle-Gomara E, Lisa V, Saralegui I. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation. 1998;37:149–152. doi: 10.1016/s0300-9572(98)00057-4. [DOI] [PubMed] [Google Scholar]
- 9.Yannopoulos D, Aufderheide T, Gabrielli A, et al. Clinical and hemodynamic comparison of 15:2 and 30:2 compression-to-ventilation ratios for cardiopulmonary resuscitation. Crit Care Med. 2006;34:1444–9. doi: 10.1097/01.CCM.0000216705.83305.99. [DOI] [PubMed] [Google Scholar]
- 10.Hostler DP, Rittenberger JC, Roth R, Callaway CW. Increased chest compression to ventilation ratio improves delivery of CPR. Resuscitation. 2007;74:446–52. doi: 10.1016/j.resuscitation.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 11.Deschilder K, De Vos R, Stockman W. The effect on quality of chest compressions and exhaustion of a compression-ventilation ratio of 30:2 versus15:2 during cardiopulmonary resuscitation—A randomized trial. Resuscitation. 2007;74:113–18. doi: 10.1016/j.resuscitation.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Odegaard S, Saether E, Steen PA, Wik L. Quality of lay person CPR performance with compression:ventilation ratios 15:2, 30:2 or continuous chest compressions without ventilations on manikins. Resuscitation. 2006;71:335–40. doi: 10.1016/j.resuscitation.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 13.Bridgewater F, Zeitz C, Field J, Inglis A, Poulish K. The Impact of the ILCOR 2005 CPR guidelines on a physical fitness assessment: A comparison of old and new protocols. Resuscitation. 2007. doi:10.1016/j.resuscitation.2007.08.011. [DOI] [PubMed]
- 14.Wik L, Thowsen J, Steen PA. An automated voice advisory manikin system for training basic life support without an instructor. A novel approach to CPR training. Resuscitation. 2001;50:167–172. doi: 10.1016/s0300-9572(01)00331-8. [DOI] [PubMed] [Google Scholar]
- 15.Hostler D, Wang H, Parrish K, Platt TE, Guimond G. The effect of a voice assist manikin (VAM) system on CPR quality among prehospital providers. Prehosp Emerg Care. 2005;9:53–60. doi: 10.1080/10903120590891660. [DOI] [PubMed] [Google Scholar]
- 16.Stainsby WN, Brooks GA. Control of lactic acid metabolism in contracting muscles and during exercise. In: Pandolf KB, Holloszy JO, editors. Exercise and sport sciences reviews. Williams and Wilkins; Baltimore: 1990. pp. 29–63. [PubMed] [Google Scholar]
- 17.Utter AC, Robertson RJ, Green JM, Suminski RR, McAnulty SR, Nieman DC. Validation of the Adult OMNI Scale of perceived exertion for walking/running exercise. Med Sci Sports Exerc. 2004;36(10):1776–80. doi: 10.1249/01.mss.0000142310.97274.94. [DOI] [PubMed] [Google Scholar]
- 18.Rittenberger JC, Guimond G, Platt TE, Hostler D. Quality of BLS decreases with increasing resuscitation complexity. Resuscitation. 2006;68:365–9. doi: 10.1016/j.resuscitation.2005.07.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.