Abstract
Background
Data regarding the health care costs of inflammatory bowel disease (IBD) in the United States are limited.
Objectives
1) To estimate the direct costs of Crohn’s disease (CD) and ulcerative colitis (UC) in the U.S. 2) To describe the distribution of costs between inpatient, outpatient, and pharmaceutical services, and 3) To identify sociodemographic factors influencing these costs.
Methods
We extracted medical and pharmacy claims from an administrative database containing insurance claims from 87 health plans in 33 states, occurring between the years 2003–2004. We identified cases of CD and UC using an administrative definition. For each case, we selected up to 3 non-IBD controls. Claims were classified as inpatient, outpatient, or pharmaceutical according to Current Procedural Terminology or National Drug Codes. Costs were based on the paid amount of each claim. IBD-attributable costs were estimated by subtracting costs for non-IBD patients from those with IBD. Logistic regression was used to identify the sociodemographic factors affecting these costs.
Results
We identified 9,056 CD patients and 10,364 UC patients. Mean annual costs for CD and UC were $8265 and $5066 respectively. For CD, 31% of costs were attributable to hospitalization, 33% to outpatient care, and 35% to pharmaceutical claims. The corresponding distribution for UC was 38%, 35%, and 27% respectively. Costs were significantly higher for children age < 20, compared to adults, but did not vary substantially by gender or region.
Discussion
This study demonstrates a substantial economic burden of IBD and can be used to inform health policy.
Background
In 2005, U.S. healthcare spending increased by 6.9 % to almost $2 trillion1. Current data suggests that healthcare costs now account for over 16 % of the United States gross domestic product, compared to 13.7 % one decade ago2. Much of this growth has been attributed to the rising prevalence of chronic conditions3, 4, for which direct treatment costs alone are estimated to be $277 billion annually5.
Crohn’s disease (CD) and ulcerative colitis (UC), collectively known as inflammatory bowel disease (IBD), are two of the most significant chronic gastrointestinal conditions. Both are associated with high morbidity6 and decreased quality of life7, 8. The public health burden of illness is also quite substantial; between 1 and 1.5 million Americans are estimated to be affected by these conditions9–11. Yet, little is know about the economic effects of IBD treatment in the United States. Current estimates of the treatment costs of IBD do not exist, and prior estimates 12, 13 are likely to be obsolete in light of newer therapeutic modalities and changing patterns of hospitalization and surgery14. Similarly, economic analyses in the UK and other European nations are not generally applicable to the United States, given that different patterns of healthcare utilization and payment systems between countries results in marked variations in healthcare expenditures15.
Consequently, an updated estimate of the treatment costs of Crohn’s disease and ulcerative colitis in the United States is urgently needed. In addition, as with other chronic illnesses, a detailed analysis of the demographic and clinical characteristics of individual patients and their patterns of service use is also necessary to understand the key factors driving these costs.16
The aims of this study were 1) to estimate the direct costs of treatment of Crohn’s disease (CD) and ulcerative colitis (UC) in the U.S., 2) to describe the distribution of such costs between inpatient, outpatient, and pharmaceutical services, and 3) to determine whether costs of IBD treatment vary by sociodemographic factors such as age, gender, and geographic region.
Methods
Study Design and Data Source
In this cross-sectional study, we analyzed the medical, surgical, and pharmaceutical insurance claims contained in the PharMetrics Patient-Centric Database (IMS Health, Watertown, MA) for the period January 1, 2003 through December 31, 2004. This longitudinal, patient-level database has been used in previous epidemiological studies of inflammatory bowel disease11, and at the time of this study included claims from 87 health plans in 33 states. The included plans capture a geographically diverse sample of commercially insured Americans. The number of plans per major U.S. Census region (i.e., East, South, Midwest, West) ranged from 12 to 34 (mean=21.75), and the number of states included in each region ranged from 5 to 10 (mean=8.25). No one state contributed more than 41% of enrollees to a region. Prior studies have reported PharMetrics to be representative of the national commercially-insured population on a variety of demographic measures, including geographic region, age, gender, and health plan type17.
Patient Selection
All individuals in the database with continuous health plan enrollment between January 1, 2003 and December 1, 2004 were eligible for inclusion in this analysis. We identified cases of CD and UC using a previously reported definition based on administrative data 11. This definition included patients with at least 3 health care contacts, on different days, associated with an International Classification of Diseases, 9th Revision, Clinical Modification diagnosis code for CD (555.xx) or UC (556.xx), or patients with at least one claim for CD or UC and at least 1 pharmacy claim for any of the following medications: mesalamine, olsalazine, balsalazide, sulfasalazine, 6-mercaptopurine, azathioprine, infliximab, adalimumab, and enteral budesonide. For patients who had claims for both CD and UC, disease assignment was made according to the majority of the last 9 claims. For each case, we randomly selected up to 3 non-IBD controls, matched for age, gender, health plan, and geographic region.
To avoid underestimating the pharmaceutical costs, we excluded patients and controls whose health plan did not provide pharmacy coverage for at least 22 out of 24 month observation period. We also excluded patients 65 years of age or older because the managed Medicare enrollees in the PharMetrics database might not be representative of the Medicare population as a whole.
Determination of Costs
We classified each claim as inpatient, outpatient, or pharmaceutical according to Current Procedural Terminology (CPT), Healthcare Common Procedure Coding System (HCPCS), or National Drug Codes (NDC). Inpatient episodes were further categorized as “GI surgical” if 1 more claims during the period of hospitalization contained a procedure code for a gastrointestinal procedure excluding endoscopy or surgery of oral cavity and liver, biliary tract, and pancreas. (43020–43135, 43280–44346, 44500 – 45190, 45395–46505, 46700–46999, 49000–49999). Otherwise, admissions were counted as “non-GI surgical”. Outpatient claims were further categorized into the following categories: office visits, emergency department visits, endoscopic procedures, radiological procedures, laboratory/pathology, and other outpatient services based upon CPT codes.
Annual costs were based on the average amount paid by the insurer over the two years of observation. If the cost reported by the health plan was negative (0.02% of claims), the paid amount was considered as missing data and deleted from the analysis. If the amount paid was not reported by the plan (approximately 17.5 % of claims) a paid amount was imputed by multiplying the charges by the plan’s median paid to charge ratio. The disease-attributable costs in each category were estimated by subtracting the mean costs of the matched controls from those with IBD.
Statistical Analysis
All IBD-attributable costs are reported as means (with standard deviation) and medians (with interquartile ranges). Overall U.S. expenditures for Crohn’s disease and ulcerative colitis were estimated by multiplying the age, gender, and region specific mean costs for these conditions by the corresponding number of affected patients previously reported in our prevalence study11. Cost data is often not normally distributed (usually skewed to the right), and thus mean healthcare costs are typically sensitive to outlying high expenditures. Such outliers contribute to overall expenditures and disease burden, however, and were thus included in our primary analyses. To determine the extent to which these outliers influenced the results presented in this manuscript, we repeated all of our analyses after excluding patients whose total disease-attributable costs were in the top and bottom 1% of the population.
To identify the demographic factors such as patient age, geographic region, and gender that influence the direct costs of Crohn’s disease and ulcerative colitis in the United States, multivariate logistic regression was used to identify the demographic predictors of having costs in the highest quartile, compared with the lowest quartile. In these models, age, region, and gender were included as predictor variables, after controlling for insurance type (Medicaid versus commercial insurance). Age, which was assigned at the end of the observation period, was analyzed as a categorical variable (< 20, 20–39, and 40–64). In order to determine whether these results were driven by extreme values in either direction, we repeated our models after excluding outliers as above.
All statistical analyses were performed using SAS version 9.1 (Cary, NC), and the study protocol was granted exemption from review by the Institutional Review Boards at the University of North Carolina Chapel Hill and Harvard Pilgrim Health Care because it involved the use of existing, de-identified data.
Results
Study Population
Our study population included 9,056 CD patients and their 24,829 matched controls and 10,364 UC patients and their 28,160 matched controls. (Table 1) The mean age of CD and UC patients was 42 years (s.d. 13 years) and 45 years (s.d. 12 years) respectively. Fifty-six percent of CD patients and 53% of UC patients were women. Each of the 4 major U.S. census regions were adequately represented in our patient population. There were no statistically significant differences between patients and controls in each of these demographic factors.
Table 1.
Characteristics of CD and UC Patients and Controls
| CD patients | CD controls | UC patients | UC controls | |
|---|---|---|---|---|
| Mean age (s.d.) | 42 (13) | 42 (13) | 45 (12) | 45 (12) |
|
| ||||
| Age | ||||
| < 20 n (%) | 737 (8.1) | 2066 (8.3) | 488 (4.7) | 1394 (5.0) |
| 20–39 n (%) | 2755 (30.4) | 7510 (30.3) | 2661 (25.7) | 1760 (25.4) |
| 40–64 n (%) | 5564 (61.4) | 15253 (61.4) | 7215 (69.6) | 19606 (69.6) |
|
| ||||
| Gender | ||||
| Female n (%) | 5090 (56.2) | 13965 (56.2) | 5464 (52.7) | 14828 (52.7) |
| Male n (%) | 3966 (43.8) | 10864 (43.8) | 4900 (47.3) | 13332 (47.3) |
|
| ||||
| Region | ||||
| Northast n (%) | 2124 (23.5) | 5818 (23.4) | 2402 (23.2) | 6567 (23.3) |
| Midwest n (%) | 2114 (23.3) | 5903 (23.8) | 2276 (22.0) | 6339 (22.5) |
| West n (%) | 1859 (20.5) | 4930 (19.9) | 2367 (22.8) | 6190 (22.0) |
| South n (%) | 2959 (32.7) | 8178 (32.9) | 3319 (32.0) | 9064 (32.2) |
|
| ||||
| Total | 9056 | 24829 | 10364 | 28160 |
Direct Costs of Crohn’s disease and ulcerative colitis
For patients with CD, the mean total costs were $10,952 per year, compared to $2,898 for the matched controls. The mean (SD) and median (interquartile range) annual CD associated treatment costs were $8,265 (21,342) and $3,203 ($530–$9,935) per patient-year (Table 2). Pharmaceutical claims accounted for the largest proportion of direct costs (35.3%). Infliximab was the most costly medication; approximately 10% of Crohn’s disease patients had at least 2 claims for infliximab infustions. The utilization and costs of other medications is shown in Table 4. Hospitalization and outpatient services accounted for 31.4% and 33.3% respectively (Figure 1). Of the hospitalization costs, 40% were incurred during surgical hospitalizations.
Table 2.
Annual Direct Costs of CD in the United States
| Mean (SD) | Median (interquartile range) | |
|---|---|---|
| Inpatient costs | ||
| Surgical | 1,026 (7,136) | 0 (0, 0) |
| Medical | 1,567 (9,853) | 0 (0, 0) |
| Total inpatient costs | 2,593 (13,416) | 0 (0, 726) |
| Outpatient costs | ||
| Emergency Department | 97 (647) | 0 (−25, 73) |
| Office | 319 (773) | 175 (−49, 512) |
| GI Endoscopy | 266 (456) | 120 (0, 434) |
| Lab, Pathology | 318 (961) | 158 (6, 419) |
| Radiology | 272 (1,085) | 53 (−71, 399) |
| Other outpatient services | 1,480 (10,767) | 197 (−200, 1,322) |
| Total outpatient costs | 2,753 (12,078) | 1,157 (−31, 3,276) |
| Outpatient Medication costs | 2,919 (6,298) | 1,014 (83, 3,005) |
| Overall Total Cost | 8,265 (21,342) | 3,203 (530, 9,935) |
Costs reported in $USD per patient-year, determined during the period between January 1, 2003 and December 31, 2004
Table 4.
Costs and Utilization of Inflammatory Bowel Disease Mediations in the United States
| Crohn’s Disease | Ulcerative Colitis | |||
|---|---|---|---|---|
| Medication Category | Mean annual costs (SD) | Proportion (%)of patients with at least 2 claims | Mean annual costs (SD) | Proportion of patients with at least 2 claims |
| Oral steroids | 4 (18) | 14 | 4 (17) | 12 |
| Oral salicylates | 495 (768) | 39 | 563 (812) | 43 |
| Rectal salicylates | 28 (169) | 7 | 145 (431) | 20 |
| Thiopurines | 194 (491) | 25 | 83 (320) | 11 |
| Methotrexate | 2 (25) | 2 | 1 (17) | 1 |
| Ileal-release budesonide | 41 (169) | 5 | 12 (101) | 1 |
| Adalimumab | 17 (385) | <1 | 12 (353) | <1 |
| Infliximab | 1523 (5133) | 10 | 92 (1248) | <1 |
| Other | 1168 (3078) | 1065 (2258) | ||
| Total | 3474 (6253) | 1977 (2987) | ||
Costs reported in $USD per patient-year, determined during the period between January 1, 2003 and December 31, 2004
Figure 1.

“Proportional costs of outpatient, inpatient, and pharmaceutical health care services delivered to patients with Crohn’s disease in the United States”
For UC, the mean total costs for patients were $7,948 per year, compared to $2,715 for the matched controls. The mean (SD) and median (interquartile range) annual UC associated treatment costs were $5,066 (17,928) and $1,963 ($68–$5,278) per patient-year (Table 3). Hospitalization accounted for the largest proportion of direct costs (37.6%). Pharmaceutical and outpatient services accounted for 27.5% and 34.9% respectively. Oral and rectal aminosalicylates accounted for the highest proportion of UC medication costs. At least 2 claims for these agents were observed in 43% and 20% of UC patients respectively (Table 4). Similar to Crohn’s disease, 42% of the hospitalization costs were incurred during surgical hospitalizations.
Table 3.
Annual Direct Costs of UC in the United States
| Mean (SD) | Median (interquartile range) | |
|---|---|---|
| Inpatient costs | ||
| Surgical | 807 (7,255) | 0 (0, 0) |
| Medical | 1,099 (9,062) | 0 (0, 0) |
| Total inpatient costs | 1,906 (12,674) | 0 (0, 0) |
| Outpatient costs | ||
| Emergency Department | 44 (569) | 0 (−31, 19) |
| Office | 244 (709) | 130 (−81, 424) |
| GI Endoscopy | 306 (463) | 204 (0, 471) |
| Lab, Pathology | 283 (708) | 150 (5, 390) |
| Radiology | 165 (1,105) | 0 (−118, 226) |
| Other outpatient services | 727 (7,785) | 58 (−313, 801) |
| Total outpatient costs | 1,768 (8,827) | 782 (−202, 2,373) |
| Outpatient medication costs | 1,393 (3,115) | 696 (1, 2,008) |
| Overall Total Cost | 5,066 (17,928) | 1,963 (68, 5,278) |
Costs reported in $USD per patient-year, determined during the period between January 1, 2003 and December 31, 2004
Based on this cost data and prevalence data recently reported by our group11(436,000 Americans with CD; 512,000 with UC), we estimate the annual disease-attributable direct costs of IBD in the United States to be $6.3 billion ($3.6 billion for CD, $2.7 billion for UC).
After removing extreme outliers (patients in the top and bottom 1% of costs), the mean (SD) annual treatment costs for CD and UC were $7,189 ($11,778) and $4,186 ($8,975) respectively. The extrapolated treatment costs of IBD in the U.S. would be $3.1 billion for CD and $2.1 billion for UC)
Demographic factors related to health care costs
Total disease-attributable costs of Crohn’s disease varied significantly by age group. In unadjusted analyses, the mean costs for Crohn’s disease in children (age less than 20) were $9,555, compared to $8,094 for adults aged 20–39 and $8,179 for adults aged 40–64 (Figure 3). After adjusting for the effects of geographic region, gender, and insurance type, adults were significantly less likely than children to have costs in the highest quartile versus the lowest quartile [OR, 0.52; 95 % CI 0.40–0.68 for adults aged 20–39 compared to children; OR, 0.40; 95 % CI 0.31–0.52) for adults aged 40–64 compared to children] (Table 5). The effects of geographic region and gender were not statistically significant. To determine the type of service(s) responsible for the higher costs of pediatric CD compared to adult CD, we also modeled inpatient, outpatient, and pharmaceutical costs. As with total costs, the costs of inpatient and outpatient services were considerably less in adults compared to children; differences in pharmaceutical costs were not as substantial (data not shown). This suggests that differences in CD-associated costs between children and adults are driven largely by ambulatory and inpatient services, rather than pharmaceutical services.
Figure 3.
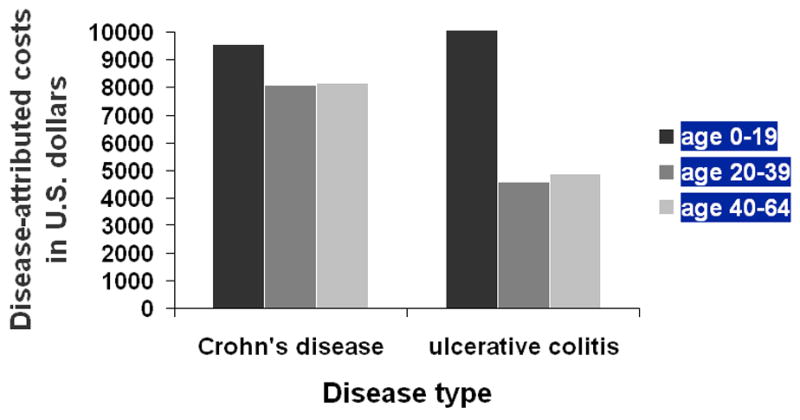
“Comparison of inflammatory bowel disease treatment costs between U.S. children and adults.” Mean costs of CD and UC in a sample of commercially insured individuals in the United States, broken down by age group. Odds ratios denote the odds of a patient having costs in the highest quartile,compared to the lowest quartile after adjusting for gender, geographical region, and insurance insurance status (Medicaid versus commercial) using logistic regression.
Table 5.
Independent Effects of Demographic Factors on the Cost of Inflammatory Bowel Disease in the United States
| Variable | Crohn’s Disease odds ratio(95% CI)* | Ulcerative Colitis odds ration (95% CI) * |
|---|---|---|
| Age | ||
| < 20 | reference | reference |
| 20–39 | 0.52 (0.40–0.68) | 0.30 (0.21–0.42) |
| 40–64 | 0.40 (0.31–0.52) | 0.24 (0.17–0.34) |
|
| ||
| Region | ||
| Northeast | 0.89 (0.74–1.06) | 1.3 (1.15–1.58) |
| South | 0.94 (0.80–1.11) | 1.03 (0.88–1.19) |
| Midwest | 0.96 (0.80–1.13) | 1.12 (0.95–1.31) |
| West | reference | reference |
|
| ||
| Gender | ||
| Male | reference | reference |
| Female | 1.04 (0.92–1.17) | 1.06 (0.95–1.19) |
Odds Ratios and 95% confidence intervals derived from multivariate logistic regression comparing costs in the highest quartile to those in the lowest quartile. In these models, age, region, and gender were included as predictor variables, after controlling for insurance type (Medicaid versus commercial insurance). Age, assigned at the end of the observation period, was analyzed as a categorical variable (2–19, 20–39, and 40–64).
As with Crohn’s disease, treatment costs for ulcerative colitis were also less in adults compared to children. In unadjusted analyses, the mean costs for UC in children (age less than 20) were $10,063, compared to $4,610 for adults aged 20–39 and $4897 for adults aged 40–64 (Figure 3). In our adjusted models, adults were significantly less likely than children to have costs in the highest quartile versus the lowest quartile [OR, 0.30; 95 % CI 0.21–0.43 for adults aged 20–39 compared to children; OR, 0.24; 95 % CI 0.17–0.34) for adults aged 40–64 compared to children] (Table 4). Regional differences were statistically significant, but the magnitude of the differences was small. No gender differences were observed. Similar to CD, the UC-associated costs of inpatient and outpatient services were also much greater for children than the other age groups; however, pharmaceutical costs did not differ by age group (data not shown).
After repeating our models after excluding outliers as above, we again found that age, but not region or gender, was significantly associated with total costs for both CD and UC.
Discussion
This study provides an updated estimate of the treatment costs of Crohn’s disease and ulcerative colitis in the United States, a necessary step in understanding the overall burden of inflammatory bowel disease in this country. In our sample of nearly 20,000 U.S. children and adults with inflammatory bowel disease, we found that the mean treatment costs for CD were $8265 per year, and for UC were $5066 per year. As in many illnesses, a disproportionate amount of the overall societal costs resulted from the individuals with the highest resource utilization as indicated by the differences in the mean and median costs presented here. Healthcare expenditures for both conditions were significantly greater in children, compared to adults, but did not vary substantially by gender or geographical region. Based on data, we extrapolate that the total IBD associated treatment costs in the United States are $6.3 billion ($3.6 billion for CD, $2.7 billion for UC).
No recent studies have reported the direct costs of IBD in the United States. Therefore, this cost analysis represents an important contribution to the existing literature describing the burden of these gastrointestinal conditions. Comparisons between this study and older cost estimates of IBD in the U.S. are limited due to varying methodologies, but can be useful to illustrate gross changes in health care utilization and costs over time. For example, based on an analysis of 1988–1989 data, Hay estimated the average annual medical costs of Crohn’s diseae and ulcerative colitis in the U.S. as $6561 and $1488 respectively12. Using the medical Consumer Price Index (CPI) to inflate these costs to 2004 amounts, this would equal $13,844 for CD and $3140 for UC. Using data from 1994–1995, Feagan et al estimated the annual cost of care for Crohn’s disease was $12,41713. Inflated to 2004 dollars, this figure would equal $18,750. Notably, the proportion of all CD costs that was attributable to hospitalization decreased from roughly 55%, as reported in these earlier studies, to 31.4% as observed here. Conversely, outpatient pharmaceutical costs increased from approximately 4% of total expenditures in prior studies to 35.3% of total expenditures in this current study. In dollar amounts, the medication costs for CD (adjusted to 2004 dollars) were $844–1416 in the Hay study (2 different cost methods used) and $670 in the Feagan study, compared to $2919 in this present study. Therefore, it appears that a shifting pattern of resource utilization may be emerging, particularly for Crohn’s disease, with increasing pharmaceutical expenditures offsetting some of the costs of hospitalization and surgery.
Although resource utilization is expected to vary between countries due to differences in practice patterns and methods of healthcare financing, the cost data presented here is surprisingly similar to that reported in other Western countries. For example, Bassi et al reported the 6 month direct costs of CD and UC in the United Kingdom (based on 2004 data) as £1652 and £1256 respectively18. Using January 2004 exchange rates and annualizing over a 1 year period, this would equal approximately $6000 USD for CD and $4600 USD for UC. Odes et al recently reported the mean annual costs of CD and UC among 8 European countries and Israel as €2548 and €1524 respectively (or $3200 USD for CD and $1900 USD for UC, based on January 2004 exchange rates), with nearly 4 fold variation in total IBD costs between countries15. Similar to our study, these recent European studies also found that a relatively high proportion of costs were attributable to pharmaceuticals (nearly 25% of total costs for CD and UC combined). Although the cost data presented in this U.S. study can not be directly compared to that reported in these prior European studies due to the different methods used as well as possible differences in the study populations (e.g. ratio of incident to prevalent cases, etc), it appears that while total expenditures for IBD are somewhat higher in the United States than in other countries, the profile of spending is quite similar.
The most striking finding in our study was the significantly increased costs incurred by children with IBD, compared to adults. Several factors might explain this difference. First, it is likely that the pediatric population includes a higher proportion of incident cases than the adult population, and medical costs are known to be higher in the year following diagnosis compared to subsequent years. Secondly, some authors have speculated that early onset IBD is a specific subtype of IBD with greater extent and severity then adult onset IBD19, 20. To the extent that this is true, the higher costs incurred by children with IBD are to be expected. Finally, there may be differences in practice patterns between pediatric and adult gastroenterologists, including the frequency of scheduled office visits and the threshold for hospital admission. Indeed, this study demonstrated that the excess costs in pediatric patients were driven largely by the ambulatory and inpatient services, rather than pharmaceutical costs.
The strengths of this study include both the size and diversity of the study population. By drawing from a large number of health plans of varying size, type, and location, we believe that the cost data presented here are broadly generalized to the commercially insured population of the United States. Another strength of this study was that costs were determined by the actual amounts paid by health plans, rather than deriving costs by multiplying units of resource use by unit costs 18,15.
An inherent limitation to using administrative data for epidemiological studies is the lack of clinical detail, resulting in the possibility misclassification of our included patients. We used a stringent case definition that required either multiple IBD-related health contacts or IBD-specific pharmaceutical claims to establish a diagnosis of CD or UC. Similar administrative definitions have been previously reported by our group11 and others21, 22. Although we feel reasonably confident that the cases included in this analysis are actual cases, this study would not have identified milder cases that did not seek medical attention or utilize health care services. Similarly, the use of claims data dose not allow precise determination of which medical services used by patients identified as having IBD were used specifically to treat IBD versus other co-morbid conditions. Therefore, in our analysis we matched IBD patients with non-IBD patients of similar age, gender, region, and health plan and estimated disease-associated costs (including total pharmaceutical costs) in the IBD patients after subtracting the costs of the non-IBD controls. A third limitation is that this study was a non-random sample of the US population, and thus might not fully represent the geographic, ethnic, and socioeconomic distribution of the overall population. For example, this analysis was limited to individuals with two years of continuous health plan enrollment and at least 22 months of pharmacy benefits. These strict enrollment criteria help ensure complete utilization data for included individuals, though may limit generalizability. In addition, our analysis included a small number of Medicaid patients analyzed (1% of included patients), and the exclusion of uninsured individuals and those receiving Medicare. To the extent that Medicaid and Medicare reimbursements are lower than those from commercial payors, the direct costs reported here may overestimate total US costs. Nevertheless, we believe that the robust sample size, diversity of patients and health plans, and the precise cost data used in the analysis outweigh these limitations. Finally, our study did not estimate indirect costs, for example transportation costs, out-of-pocket costs, or productivity costs due to missed work for patients or parents. Such indirect costs, which represented approximately 20% of direct costs in the British study, further contribute to the economic burden of illness.
In conclusion, this study presents a contemporary estimate of the treatment costs of IBD in the United States, and as such represents an important step in understanding the care for persons with these conditions. Indeed, Crohn’s disease and ulcerative colitis are costly medical conditions, both at the level of the individual patient and in aggregate. This findings can 1) inform IBD-related health policy, including the planning of appropriate clinical services and allocating research funding commensurate with the overall disease burden, 2) identify risk factors for increased costs (i.e. children) for which to target more effective treatments 3) support IBD advocacy work, and 4) help put into perspective the cost of emerging therapeutics and facilitate future economic studies of IBD care.
Figure 2.
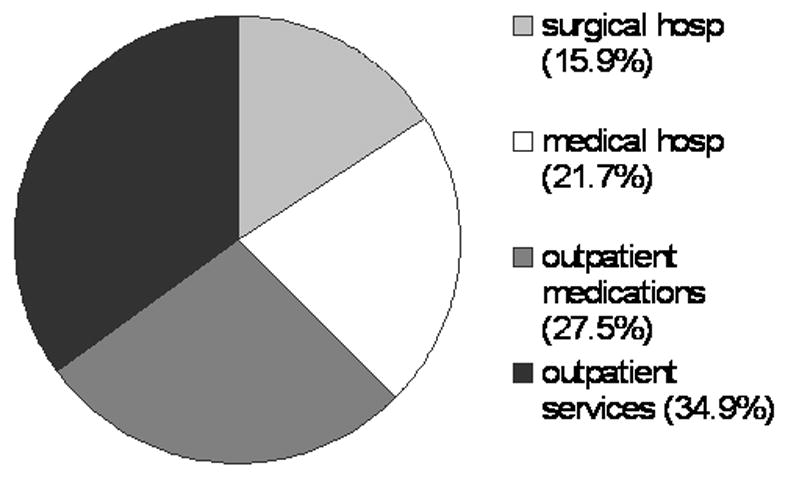
“Proportional costs of outpatient, inpatient, and pharmaceutical health care services delivered to patients with ulcerative colitis in the United States”
Acknowledgments
Study Support: Dr. Kappelman was supported in part by the National Center for Research Resources (NCRR) Grant 1K12 RR023248-04 and the National Institute for Diabetes and Digestive and Kidney Diseases Grant 5P30 DK034987.
Footnotes
Conflict of Interest: No authors have a conflict of interest to disclose
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Catlin A, Cowan C, Heffler S, Washington B. National health spending in 2005: the slowdown continues. Health Aff (Millwood) 2007;26:142–53. doi: 10.1377/hlthaff.26.1.142. [DOI] [PubMed] [Google Scholar]
- 2.Thorpe KE. Factors accounting for the rise in health-care spending in the United States: the role of rising disease prevalence and treatment intensity. Public Health. 2006;120:1002–7. doi: 10.1016/j.puhe.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Thorpe KE. The rise in health care spending and what to do about it. Health Aff (Millwood) 2005;24:1436–45. doi: 10.1377/hlthaff.24.6.1436. [DOI] [PubMed] [Google Scholar]
- 4.Thorpe KE, Florence CS, Howard DH, Joski P. The rising prevalence of treated disease: effects on private health insurance spending. Health Aff (Millwood) 2005:W5-317–W5-25. doi: 10.1377/hlthaff.w5.317. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 5.DeVol R, Bedroussian A, Charuworn A, Chatterjee A. An Unhealthy America: The Economic Burden of Chronic Disease. Milken Institute; 2007. [Google Scholar]
- 6.Longobardi T, Jacobs P, Bernstein CN. Work losses related to inflammatory bowel disease in the United States: results from the National Health Interview Survey. Am J Gastroenterol. 2003;98:1064–72. doi: 10.1111/j.1572-0241.2003.07285.x. [DOI] [PubMed] [Google Scholar]
- 7.Cohen RD. The quality of life in patients with Crohn’s disease. Aliment Pharmacol Ther. 2002;16:1603–9. doi: 10.1046/j.1365-2036.2002.01323.x. [DOI] [PubMed] [Google Scholar]
- 8.McLeod RS, Churchill DN, Lock AM, Vanderburgh S, Cohen Z. Quality of life of patients with ulcerative colitis preoperatively and postoperatively. Gastroenterology. 1991;101:1307–13. doi: 10.1016/0016-5085(91)90081-u. [DOI] [PubMed] [Google Scholar]
- 9.Loftus EV., Jr Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504–17. doi: 10.1053/j.gastro.2004.01.063. [DOI] [PubMed] [Google Scholar]
- 10.Loftus EV., Jr The burden of inflammatory bowel disease in the United States: a moving target? Clin Gastroenterol Hepatol. 2007;5:1383–4. doi: 10.1016/j.cgh.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 11.Kappelman MD, Rifas-Shiman SL, Kleinman K, et al. The prevalence and geographic distribution of Crohn’s disease and ulcerative colitis in the United States. Clin Gastroenterol Hepatol. 2007;5:1424–9. doi: 10.1016/j.cgh.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 12.Hay JW, Hay AR. Inflammatory bowel disease: costs-of-illness. J Clin Gastroenterol. 1992;14:309–17. doi: 10.1097/00004836-199206000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Feagan BG, Vreeland MG, Larson LR, Bala MV. Annual cost of care for Crohn’s disease: a payor perspective. Am J Gastroenterol. 2000;95:1955–60. doi: 10.1111/j.1572-0241.2000.02261.x. [DOI] [PubMed] [Google Scholar]
- 14.Lichtenstein GR, Yan S, Bala M, Blank M, Sands BE. Infliximab maintenance treatment reduces hospitalizations, surgeries, and procedures in fistulizing Crohn’s disease. Gastroenterology. 2005;128:862–9. doi: 10.1053/j.gastro.2005.01.048. [DOI] [PubMed] [Google Scholar]
- 15.Odes S, Vardi H, Friger M, et al. Cost analysis and cost determinants in a European inflammatory bowel disease inception cohort with 10 years of follow-up evaluation. Gastroenterology. 2006;131:719–28. doi: 10.1053/j.gastro.2006.05.052. [DOI] [PubMed] [Google Scholar]
- 16.Druss BG, Marcus SC, Olfson M, Tanielian T, Elinson L, Pincus HA. Comparing the national economic burden of five chronic conditions. Health Aff (Millwood) 2001;20:233–41. doi: 10.1377/hlthaff.20.6.233. [DOI] [PubMed] [Google Scholar]
- 17.Stempel DA, Mauskopf J, McLaughlin T, Yazdani C, Stanford RH. Comparison of asthma costs in patients starting fluticasone propionate compared to patients starting montelukast. Respir Med. 2001;95:227–34. doi: 10.1053/rmed.2000.1027. [DOI] [PubMed] [Google Scholar]
- 18.Bassi A, Dodd S, Williamson P, Bodger K. Cost of illness of inflammatory bowel disease in the UK: a single centre retrospective study. Gut. 2004;53:1471–8. doi: 10.1136/gut.2004.041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hait E, Bousvaros A, Grand R. Pediatric inflammatory bowel disease: what children can teach adults. Inflamm Bowel Dis. 2005;11:519–27. doi: 10.1097/01.mib.0000166932.66853.fd. [DOI] [PubMed] [Google Scholar]
- 20.Haller CA, Markowitz J. IBD in children: lessons for adults. Curr Gastroenterol Rep. 2007;9:528–32. doi: 10.1007/s11894-007-0070-8. [DOI] [PubMed] [Google Scholar]
- 21.Herrinton LJ, Liu L, Lafata JE, et al. Estimation of the period prevalence of inflammatory bowel disease among nine health plans using computerized diagnoses and outpatient pharmacy dispensings. Inflamm Bowel Dis. 2007;13:451–61. doi: 10.1002/ibd.20021. [DOI] [PubMed] [Google Scholar]
- 22.Bernstein CN, Blanchard JF, Rawsthorne P, Wajda A. Epidemiology of Crohn’s disease and ulcerative colitis in a central Canadian province: a population-based study. Am J Epidemiol. 1999;149:916–24. doi: 10.1093/oxfordjournals.aje.a009735. [DOI] [PubMed] [Google Scholar]


